Professional Documents
Culture Documents
LAC+USC Emergency Department - Presentation of Dr. Edward Newton
Uploaded by
barbarafeder0 ratings0% found this document useful (0 votes)
1K views17 pagesCopyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
1K views17 pagesLAC+USC Emergency Department - Presentation of Dr. Edward Newton
Uploaded by
barbarafederCopyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 17
EMERGENCY MEDICINE
LAC +USC MEDICAL CENTER
Ed Newton, M.D., Chair Emergency Medicine
A DAY IN THE LIFE
• Clinical: 400 patients/day in 6 EDs; busiest
Level I Trauma Center in US
• Teaching: 54 EM residents, competitive
specialty draws top residents to the MC; med
student rotation
• Administration: planning, problem
resolution, evaluations; recruiting/retention
• Scholarly Activity: writing and editing
texts/journals; speaking at conferences
Safety Net Hospitals
• Urban, academic centers, Trauma
Centers
• Care for a disproportionate number of
uninsured, medically complex patients
with additional significant social
problems; specialty care
• Underfunded: Less able to implement
changes in structure, equipment,
personnel, information systems
SAFETY NET
• In addition Safety Net functions to:
• Train large % of health care
workers
• Prepare for and provide care in
disaster situations
• Perform disease surveillance, public
health functions
SAFETY NET
• Safety net is unraveling as more hospitals close
completely or close their EDs
• Virtually no “surge capacity” exists to accommodate
a sudden increase in the number of patients from
natural disasters; flu or other epidemics;
bioterrorism
• Increased diversions and transport times
• Only 4% of $3.8 billion Homeland Security funds for
emergency preparedness has gone to emergency
medical services (2003)
EMERGENCY DEPARTMENT
OVERCROWDING
ED OVERCROWDING
• Victims of our own success:
– always open; don’t have to take time
off work to see a physician
– can deal with any medical problem
– get immediate access to whole
diagnostic capability of the hospital
• Most of the increase in # of visits
is from insured patients
A FEW FACTS: 1993-2003
• 114 million ED visits/year (26% increase)
• Net loss of 703 hospitals; 198,000
hospital beds; 425 EDs (15%)
• 60%-79% of hospitals operating over
capacity
• 45 million uninsured, many more
underinsured (e.g. MediCal, high
deductible policies)
INCREASED DEMAND FOR
ED SERVICES
• Aging population
• Diabetes epidemic; CHF epidemic
• Increased referrals by PMD’s to ED
especially for sicker patients
• More invasive treatment options
available that can’t be provided in
an office
IMPACT OF OVERCROWDING
ON EMERGENCY MEDICINE
• Changed scope of practice of EM to
include more critical care, inpatient
care and primary care
• Increased turnover of staff, burnout
• Increased errors
• Not an ideal environment for
providing inpatient care
CAUSES OF ED
OVERCROWDING
• High levels of uninsured and
underinsured (45% in LA County) lack of
access to all but ED; failure of primary
care
• EMTALA Federal law (1986)
• Reduced inpatient bed capacity
• Hospital closures
• Nursing shortage
• Nursing ratios
The Uninsured
• Linking a national
health plan to
insurance
companies and
employment will
still leave out a
huge population
• The sickest patients
are too sick to work
EMTALA
• Annual “bad debt” per physician $12,300
• Annual “bad debt” per Emergency Physician:
$138,000 (AMA)
• Guarantees access for all patients but is an
unfunded mandate
• Has resulted in other specialists refusing to
participate in “on call” panels and rise of
specialty surgical specialty hospitals with no
ED∴ not subject to EMTALA
HOSPITAL CLOSURES:
California Data
• 79 hospital closures
1996-2006 (CHA)
• 11 recent hospital
closures in LA
County including
MLK
• California MediCal
reimbursement
ranks 50th vs all
states
NURSING SHORTAGE
• Nurse ratio are a good idea to improve
quality of care but have resulted in
additional closures of inpatient beds
• Implemented at the same time as
serious nursing shortage
• Ratios are not enforced in the ED ∴
patients accumulate in ED as “boarding
admitted patients” ED cannot accept
new critical patients
Additional Health Costs in
US
• Highest levels of
interpersonal violence of
any Western society
• High levels of drug and
alcohol addiction and
abuse
• Ability to provide very
expensive technologies
• High level of futile care at
the end of life
• Lack of investment in
preventive care
SOME SOLUTIONS
• National health plan without links to insurance
companies and employment
• Provide funding for EMTALA related care
• Increase inpatient, psychiatric and convalescent
hospital bed capacity
• Every hospital should have a surge capacity plan that
involves the whole institution
• Build up primary care capacity
• Entice more nurses into profession by increasing
wages and benefits; increase training capacity
• Mandate participation in ED call panel as a condition
for medical staff privileges
• Gun control, violence intervention and rehab programs
You might also like
- Necessity of Sadness Draft 1Document6 pagesNecessity of Sadness Draft 1api-241786723No ratings yet
- Khanh Tran EssayDocument7 pagesKhanh Tran EssayKhoa HữuNo ratings yet
- Substance Abuse & Mental HealthDocument1 pageSubstance Abuse & Mental Healthkaitlin100% (1)
- Observations of An AA MeetingDocument2 pagesObservations of An AA MeetingKaryn Ives Kerr100% (1)
- Psychiatric 3: Suicide (DR Rosales) June 8, 2011Document4 pagesPsychiatric 3: Suicide (DR Rosales) June 8, 2011Von HippoNo ratings yet
- How Narcissism Relates to Social Media UseDocument1 pageHow Narcissism Relates to Social Media UseDASTIN FAIZ PORDADINo ratings yet
- Na ReflectionDocument6 pagesNa Reflectionapi-433710976No ratings yet
- Case Study on Celiac Disease Diagnosis and Gluten-Free DietDocument4 pagesCase Study on Celiac Disease Diagnosis and Gluten-Free DietRachael OyebadeNo ratings yet
- Pre-Reflection Womens Health Paper Alyssa MatulichDocument5 pagesPre-Reflection Womens Health Paper Alyssa Matulichapi-456313554No ratings yet
- Substance Group Reflection PaperDocument4 pagesSubstance Group Reflection PaperAmberNo ratings yet
- Aa Support Group ObservationDocument6 pagesAa Support Group Observationapi-302499446100% (3)
- Counselor's Manual For Relapse Prevention With Chemically Dependent Criminal Offenders Technical Assistance Publication Series 19Document133 pagesCounselor's Manual For Relapse Prevention With Chemically Dependent Criminal Offenders Technical Assistance Publication Series 19Norma FloresNo ratings yet
- Gender Dysphoria: Agnes B. Padilla MD, DPBP, FppaDocument25 pagesGender Dysphoria: Agnes B. Padilla MD, DPBP, FppaSivaganesh Paidi100% (2)
- Argument Social Media and NarcissismDocument5 pagesArgument Social Media and NarcissismbriegondaNo ratings yet
- Response Essay of Dont Blame The Eater FinalDocument5 pagesResponse Essay of Dont Blame The Eater Finalapi-250309746No ratings yet
- Beautiful Boy by David Sheff - Discussion QuestionsDocument3 pagesBeautiful Boy by David Sheff - Discussion QuestionsHoughton Mifflin HarcourtNo ratings yet
- PARENTING STYLES GUIDE CHILD DEVELOPMENTDocument14 pagesPARENTING STYLES GUIDE CHILD DEVELOPMENTRana QaiserNo ratings yet
- Interview Paper SW 3010Document7 pagesInterview Paper SW 3010api-319252753No ratings yet
- Carl Rogers' Person-Centered Therapy and Self-ActualizationDocument2 pagesCarl Rogers' Person-Centered Therapy and Self-ActualizationChristianieAnnNo ratings yet
- Homeboy Industries (Final)Document10 pagesHomeboy Industries (Final)Paula De GuzmanNo ratings yet
- Carl RogersDocument2 pagesCarl RogersAndrew BuckNo ratings yet
- Substance Abuse, Eating Disorders and Impulse ControlDocument14 pagesSubstance Abuse, Eating Disorders and Impulse ControlAaronAgulayNo ratings yet
- Psych Ward HistoryDocument6 pagesPsych Ward HistoryNestley TiongsonNo ratings yet
- Substance Abuse Assessment, Diagnosis, and Initial Treatment Planning For Behavioral Health CliniciansDocument28 pagesSubstance Abuse Assessment, Diagnosis, and Initial Treatment Planning For Behavioral Health Clinicianseuronetit100% (1)
- Personal Statement SW 4997Document6 pagesPersonal Statement SW 4997api-276764287No ratings yet
- LGBT Sexuality OutlineDocument11 pagesLGBT Sexuality OutlineYhan-yhan Rodriguez Khou100% (1)
- Acute Renal Failure 2Document56 pagesAcute Renal Failure 2Jeeca O. Veloso100% (1)
- A Racial WorldviewDocument4 pagesA Racial Worldviewapi-490642506No ratings yet
- Student Research Paper: Homelessness As A Scourge in Seattle City 1Document13 pagesStudent Research Paper: Homelessness As A Scourge in Seattle City 1Justine Oseko MongayoNo ratings yet
- Check List For PT ETOH Alcohol UseDocument12 pagesCheck List For PT ETOH Alcohol Usesen ANo ratings yet
- PORTFOLIO-Senitnel Event Paper FinalDocument25 pagesPORTFOLIO-Senitnel Event Paper FinalLeAnnaNo ratings yet
- Promoting Healthy Aging by Confronting AgeismDocument7 pagesPromoting Healthy Aging by Confronting AgeismJuanito MaravillasNo ratings yet
- Op-Ed Part 2Document1 pageOp-Ed Part 2api-530416054No ratings yet
- The Victim's Autopsy ReportDocument2 pagesThe Victim's Autopsy ReportShan KNo ratings yet
- N420.Alcoholics' Anonymous Journal GuideDocument4 pagesN420.Alcoholics' Anonymous Journal Guidemichael andersonNo ratings yet
- Professional Meeting Reflective Journal-2Document3 pagesProfessional Meeting Reflective Journal-2api-399086837No ratings yet
- Holistic Health Care PlanDocument9 pagesHolistic Health Care Planapi-449021066No ratings yet
- Guide To: Medi-Cal Mental Health ServicesDocument53 pagesGuide To: Medi-Cal Mental Health ServicesJRSNo ratings yet
- Quasi-Experimental and Single-Case Designs M:C 10Document5 pagesQuasi-Experimental and Single-Case Designs M:C 10Elaine Louise O. ForondaNo ratings yet
- Humantrafficking Logic ModelDocument1 pageHumantrafficking Logic Modelapi-341131818100% (1)
- Acompanado Psy 490 Psychology Reflection PaperDocument6 pagesAcompanado Psy 490 Psychology Reflection Paperapi-478101869No ratings yet
- Community Assessment PaperDocument6 pagesCommunity Assessment Paperapi-543558169No ratings yet
- HOSPICE CARE: A TEAM APPROACH TO COMPASSIONATE END-OF-LIFE CAREDocument7 pagesHOSPICE CARE: A TEAM APPROACH TO COMPASSIONATE END-OF-LIFE CAREJason SteelNo ratings yet
- Healthcare Ethics & Law: Professional ResponsibilitiesDocument45 pagesHealthcare Ethics & Law: Professional ResponsibilitiesraykantankaNo ratings yet
- Case Study 2Document7 pagesCase Study 2api-561058683No ratings yet
- Synthesis Paper 2Document9 pagesSynthesis Paper 2api-608069746No ratings yet
- How to Prevent Homelessness for SeniorsDocument10 pagesHow to Prevent Homelessness for SeniorsGeraldine Lucero100% (1)
- 5 Stages of Emotional ResponseDocument2 pages5 Stages of Emotional Responsemastermanyu100% (1)
- Elder Abuse and Neglect: Brenda Holmes MSN/Ed, RNDocument25 pagesElder Abuse and Neglect: Brenda Holmes MSN/Ed, RNSonia SinghNo ratings yet
- Conexiones Capstone Project PresentationDocument8 pagesConexiones Capstone Project Presentationapi-467632033100% (1)
- Nurse Involvement in End of Life DecisionDocument4 pagesNurse Involvement in End of Life Decisiontri hardaniNo ratings yet
- SW 4020 Community Analysis PaperDocument6 pagesSW 4020 Community Analysis Paperapi-242943882No ratings yet
- Gerona Scholarly Reflection 2Document9 pagesGerona Scholarly Reflection 2api-544562008No ratings yet
- Running Head: Senior Capstone Reflection 1Document7 pagesRunning Head: Senior Capstone Reflection 1Nathalee WalkerNo ratings yet
- Lateral Violence in NursingDocument5 pagesLateral Violence in NursingJea GarciaNo ratings yet
- Health Care Disparities - Stereotyping and Unconscious BiasDocument39 pagesHealth Care Disparities - Stereotyping and Unconscious BiasCherica Oñate100% (1)
- Psychological Disorder (Schizophrenia)Document31 pagesPsychological Disorder (Schizophrenia)Farah Bashir0% (1)
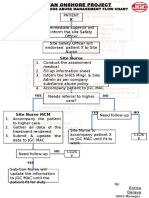
- Alcohol and Drug Abuse Flow ChartDocument1 pageAlcohol and Drug Abuse Flow Chartboen jaymeNo ratings yet
- Cns 765 Case Study FinalDocument10 pagesCns 765 Case Study Finalapi-582911813No ratings yet
- I Didn't Cause It, I Can't Change It: How Mothers of Adult Children with Co-occurring Disorders Have CopedFrom EverandI Didn't Cause It, I Can't Change It: How Mothers of Adult Children with Co-occurring Disorders Have CopedNo ratings yet
- Laurie Udesky - Sample Release Form 2Document1 pageLaurie Udesky - Sample Release Form 2barbarafederNo ratings yet
- Algis MartellDocument59 pagesAlgis MartellbarbarafederNo ratings yet
- Laurie Udesky - Sample Release Form 1Document1 pageLaurie Udesky - Sample Release Form 1barbarafederNo ratings yet
- Children's Food Environment - Behavioral IndicatorsDocument12 pagesChildren's Food Environment - Behavioral IndicatorsbarbarafederNo ratings yet
- The 7 Social Media Habits of Highly Effective Health Reporters - Laura McClureDocument9 pagesThe 7 Social Media Habits of Highly Effective Health Reporters - Laura McClurebarbarafederNo ratings yet
- Erika Franklin Fowler - Getting A Grip On StatisticsDocument61 pagesErika Franklin Fowler - Getting A Grip On Statisticsbarbarafeder100% (1)
- Children's Food Environment - State LawsDocument6 pagesChildren's Food Environment - State LawsbarbarafederNo ratings yet
- 100806guttierez ObjectionDocument15 pages100806guttierez ObjectionbarbarafederNo ratings yet
- Charles Connors Document - AntidoteDocument60 pagesCharles Connors Document - AntidotebarbarafederNo ratings yet
- Gar CIA LawsuitDocument6 pagesGar CIA LawsuitbarbarafederNo ratings yet
- Gar CIA Lawsuit Exhibits 2Document149 pagesGar CIA Lawsuit Exhibits 2barbarafederNo ratings yet
- Gar CIA Lawsuit Exhibits 1Document327 pagesGar CIA Lawsuit Exhibits 1barbarafeder100% (1)
- Health Information Technology - A GlossaryDocument1 pageHealth Information Technology - A GlossarybarbarafederNo ratings yet
- Cox DocumentDocument15 pagesCox DocumentbarbarafederNo ratings yet
- Kartell, James - Decision and Order 5-5-10Document6 pagesKartell, James - Decision and Order 5-5-10barbarafederNo ratings yet
- Ann Moss Joyner - Mapping Social InequitiesDocument68 pagesAnn Moss Joyner - Mapping Social InequitiesbarbarafederNo ratings yet
- DBB - Marom - Medical Board DocumentDocument21 pagesDBB - Marom - Medical Board DocumentbarbarafederNo ratings yet
- Health Disparities in South Los Angeles - LaVonna LewisDocument22 pagesHealth Disparities in South Los Angeles - LaVonna LewisbarbarafederNo ratings yet
- MayoTestCatalog Rochester LaboratoryReferenceEdition SortedByTestName DuplexDocument1,181 pagesMayoTestCatalog Rochester LaboratoryReferenceEdition SortedByTestName DuplexsureshNo ratings yet
- Pennington Co. Courant, January 3, 2013Document8 pagesPennington Co. Courant, January 3, 2013surfnewmediaNo ratings yet
- Proposed Rule: Medical Benefits: Medical Care or Services Reasonable ChargesDocument4 pagesProposed Rule: Medical Benefits: Medical Care or Services Reasonable ChargesJustia.comNo ratings yet
- Donald HazzardDocument14 pagesDonald HazzardshogaibutsuNo ratings yet
- Healthcare Fraud in CanadaDocument28 pagesHealthcare Fraud in CanadaMartin McTaggartNo ratings yet
- Kdunn Pharmacy Resume 2018Document1 pageKdunn Pharmacy Resume 2018api-271763344No ratings yet
- MEDICARD PHILIPPINES, INC VS. Commissioner of Internal Revenue (GR NO. 222743) April 5, 2017Document24 pagesMEDICARD PHILIPPINES, INC VS. Commissioner of Internal Revenue (GR NO. 222743) April 5, 2017Emil BautistaNo ratings yet
- 2009 IP On Wheeled Mobility v2.0Document339 pages2009 IP On Wheeled Mobility v2.0Linda_Elsaesse_1100No ratings yet
- Writing Complaint Responses Final 26-5-10Document6 pagesWriting Complaint Responses Final 26-5-10Marc MarcoNo ratings yet
- Resume AroraDocument2 pagesResume Aroraapi-463677449No ratings yet
- AHM 250 Chapter 1Document9 pagesAHM 250 Chapter 1Paromita MukhopadhyayNo ratings yet
- A Better Way Health Care SnapshotDocument3 pagesA Better Way Health Care SnapshotStephen LoiaconiNo ratings yet
- UntitledDocument2 pagesUntitledapi-247568866No ratings yet
- ToastmasterDocument12 pagesToastmasterElfirasaniNo ratings yet
- Exercises of Task 6Document5 pagesExercises of Task 6Engel N. RosarioNo ratings yet
- Social Security, Medicare and Medicaid Work For Washington 2012Document23 pagesSocial Security, Medicare and Medicaid Work For Washington 2012SocialSecurityWorksNo ratings yet
- Pharmacology For The Primary Care Provider 4th Edition Edmunds Test BankDocument35 pagesPharmacology For The Primary Care Provider 4th Edition Edmunds Test Bankalomancyheriot.o7m4100% (24)
- Medicard v. CIRDocument22 pagesMedicard v. CIRKris CalabiaNo ratings yet
- ER Nursing Management of Orthopedic InjuriesDocument2 pagesER Nursing Management of Orthopedic InjuriesRolando Ian Maranan RNNo ratings yet
- Hospitals Care Systems of FutureDocument21 pagesHospitals Care Systems of FutureAlejandro CortésNo ratings yet
- IQ4I Research & Consultancy Published A New Report On "BioTextiles Global Market - Forecast To 2023"Document4 pagesIQ4I Research & Consultancy Published A New Report On "BioTextiles Global Market - Forecast To 2023"VinayNo ratings yet
- Chapter 14Document42 pagesChapter 14Fatma Taha MohamedNo ratings yet
- 2015-2016 Programs Dallas Dental Hygienists' SocietyDocument4 pages2015-2016 Programs Dallas Dental Hygienists' SocietyRickie LindleyNo ratings yet
- HospitalDocument40 pagesHospitalAshish DubeyNo ratings yet
- Chapter I (A Case Study in Community and Public Health Area: Barangay Kayquit Iii, Purok 3 & 4)Document3 pagesChapter I (A Case Study in Community and Public Health Area: Barangay Kayquit Iii, Purok 3 & 4)sophiasaphire100% (1)
- Careplus-Pharmacare Forteo FormDocument1 pageCareplus-Pharmacare Forteo FormclarkmNo ratings yet
- Glossary of Dental Clinical and Administrative TermsDocument38 pagesGlossary of Dental Clinical and Administrative TermsSarah TanNo ratings yet
- New Haven Public Schools 2013-14 Site Based Budget Request SummaryDocument5 pagesNew Haven Public Schools 2013-14 Site Based Budget Request SummaryHelen BennettNo ratings yet
- Ontario Jurisprudence Exam Notes - Ontario Drug Benefit Act (2/2)Document4 pagesOntario Jurisprudence Exam Notes - Ontario Drug Benefit Act (2/2)Herodotus100% (5)
- Outpatient Rooms: Listen To The Dialogue Between Nurses and Patients / Visitors in The Outpatient RoomsDocument8 pagesOutpatient Rooms: Listen To The Dialogue Between Nurses and Patients / Visitors in The Outpatient Roomssudi lestariNo ratings yet