Professional Documents
Culture Documents
Fluids & Electrolyte New
Uploaded by
Maria VisitacionOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fluids & Electrolyte New
Uploaded by
Maria VisitacionCopyright:
Available Formats
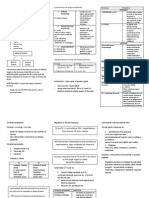
TOPICS/SUBJECTS
1. FLUIDS
2. ELECTROLYTES
3. ABG
FLUIDS
Grace O. Galapia-Magno, RN, MAN
Coverage of Discussion
1. Regulator
2. Compartments
3. Percentage
4. Movements
5. Types
6. Intake and Output
7. Edema
8. Hypervolemia
9. Hypovolemia
What is the most important regulator
of water?
A. Hypothalamus
B. Pituitary Gland
C. ADH
D. ANP
E. Aldosterone
F. Renin
G. Colon
H. Heart
I. Kidneys
J. Baroreceptors
ADH on work.
ADH stops urine
ADH Antidiuretic Hormone
blood volume
ADH
urine output
blood volume
blood volume
ADH
urine output
blood volume
Drill
1. What triggers a ADH?
a. FVE
b. FVD
2. What will be the concentration of urine if
ADH is high?
a. Diluted
b. Concentrated
Man can live 30 45 days without food
But only 10 14 days without water
Compartment of Fluids.
1. Extracellular Fluids
2. Intracellular Fluids
Transcellular Fluid
60% of Body Weight is Water
Fluid Compartments:
1. ICF Intracellular Fluid =40%
2. ECF Extracellular Fluid =20%
IVF Intravascular Fluid = 5%
Arterial Fluid = 2%
Venous Fluid = 3%
ITF interstitial fluid = 15%
3. Transcellular Fluid
Pleural Fluid
Peritoneal Fluid
Pericardial Fluid
CSF
Synovial Fluid
Drill
Compute the distibution of water to an adult
weighing 90 kg.
1. ICF?
2. ECF?
3. IVF?
1. Arterial Fluid?
2. Venous Fluid?
4. ITF?
Fluids move
thru ACTIVE or PASSIVE transport
mechanism?
2 Transport Mechanisms
1. Active: solutes from low to high (PISO)
2. Passive: solutes and solvent
Osmosis: solvent
Diffusion: solutes (gas exchange)
Ultrafiltration: solutes and solvent (Dialysis)
Drill
1. Movement of solvent from low to high
concentration?
A. Osmosis
B. Diffusion
C. Active
Drill
2. Movement of solute from low to high
concentration?
A. Osmosis
B. Diffusion
C. Active
3 Types of Fluids
1. Isotonic: 0.9% NaCl,LR(Same Osmotic Pressure)
Raise blood volume
2. Hypotonic: 0.45% NaCl, D5W
Hydrate cells
3. Hypertonic: 10%, 20%, 50% Dextrose in
Water, D5LR, Mannitol
Pull water from the cells
Composition of Fluids
Saline solution water & electrolyte
Dextrose solution water or saline & calories
Lactated ringers water & electrolyte(Na,K,Cl -,Ca++
Balance Isotonic varies, water & electrolyte some
electrolyte( Na,K,Mg++,Cl-,HCO3,gluconate)
Whole blood & blood component
Plasma Expander albumin, dextran, plasma protein
Drill
1. What IV fluid is indicated to client with
Stroke?
2. What IV fluid will be given in severe burn
injury?
3. What IV fluid will be prepared to a CHF client?
4. What IV fluid is best during DKA?
5. What IV fluid is a substitute for TPN solution?
IV Fluids Safety
Macrodrip
Microdrip
Soluset
IV Infusion Pump
Drill
1. 1000 mL D5LR to run in 10 hours, DF 20
How many cc/hr?
How many gtts/min?
2. 1000 mL D5LR, 120cc/hr, DF 15
How many hours to consume?
How many gtts/min?
IV Fluid Computation
TVI/cchr = duration in hr
TVI/duration in hr = cc/hour
Cchr/1 = gtts/min (60 DF)
Cchr/3 = gtts/min (20 DF)
Cchr/4 = gtts/min (15 DF)
Cchr/5 = gtts/min (12 DF)
Cchr/6 = gtts/min (10 DF)
Intake and Output
2.6
kg
2.6
kg
The following are typical 24-hour values for an adult.
Intake 2,600 ml/24h
1,500 ml oral fluids
800 ml in food
300 ml in oxidation of food
Output 2,600 ml/24h
1,500 ml urine
200 ml in stool
500 ml through the skin
400 ml through respiration
What is essential and non essential
intake/output?
Drill
Colostomy Irrigation
350 mL irrigation
150 mL drainage
1. How many mL is the
intake?
2. How many mL is the
output?
3. When do you tally I and
O sheet?
4. Can you delegate I and
O to NA?
5. When is the best time
to weigh your patient?
6. Give an example of
patient that would
require I and O
monitoring?
Osmolality
Refers to the concentration of a solution.
Hypoosmolality Hyperosmolality
Drill
1. In FVD what plasma
osmolality may be
observed?
A. Hyperosmolality
B. Hypoosmolality
2. In Polycythemia Vera
what plasma
osmolality may be
observed?
A. Hyperosmolality
B. Hypoosmolality
3. In CRF what plasma
osmolality may be
observed?
A. Hyperosmolality
B. Hypoosmolality
4. In the 2
nd
stage of ARF
what plasma
osmolality may be
observed?
A. Hyperosmolality
B. Hypoosmolality
29
Causes of EDEMA FORMATION:
1.
Ex: CHF, CRF
2.
Ex: proteinuria, negative nitrogen
balance
3. Lymphatic Obstruction
Ex: Filariasis, Hodgkins and Non
Hodgkins
4. Increased Capillary Permeability
EXTRAVASATION
leakage of a fluid out of its
container
Inflammation: movement of
white blood cells from the
capillaries to the tissues
surrounding them
Malignant cancer: metastasis
it refers to cancer cells exiting
the capillaries and entering
organs
INFILTRATION
Infiltration is the
accumulation of
substance in a tissues or
cells.
The material collected in
those tissues or cells is
also called infiltration.
Drill
1. What is a pitting edema?
2. What is a non-pitting edema?
3. Scoring of edema?
4. Generalized edema?
5. Common location of
edema?
FLUID ASSESSMENT:
FVE FVD
1. Mucus membrane
2. Skin integrity
3. Body weight
4. Jugular vein
5. BP, PAWP 6-12 mm Hg, PAP
25/15 mm Hg
6. CVP (most accurate) 0-7 mm
Hg or 5-10 cm of H2O
7. I&O
8. Pulse
9. Lung sound and heart sound
10. Urine output
11. Urine SG 1.005-1.030
12. Hematocrit 48%
13. Plasma osmolality 252-309
mOsml/L
14. LOC
FVE
CAUSE
DX
S/SX
CX
MX
IV
H20
IT
H20
IC
H20
TC
H20
Water Intoxication
3
rd
Spacing or 3
RD
FLUID SHIFT
Pleural sac = Pleural Effusion
Pericardial sac = Pericardial Effusion
Peritoneal sac = Ascites
FVD
CAUSE
DX
S/SX
CX
MX
IC
H20
IT
H20
IV
H20
Shock
tissue perfusion (H20, 02, glucose)
CHD
ANS
ER situation (CPR)
Modified T.
02 treatment (ETT-Mech Vent.)
IV line or cutdown (Intra Osseous)
Drugs:
Epinephrine
Inotropes and Vasopressors
Treat the underlying
cause
Dont be too late!
ORGANS EARLY S/SX
Reversible
LATE S/SX
Irreversible
BRAIN LOC (disorientation) Coma
HEART tachy Brady
KIDNEYS Oliguria (>30mL/H) Anuria (>10mL/H)
LUNGS tachy Brady
SKIN Pallor Cyanosis
GIT Ulceration Ulceration-bleeding
LIVER detoxification Sepsis
Drill
1. Most common type of Shock?
2. Hct level in a multiple gun shot wound patient?
3. Serum osmolality of a CRF patient?
4. Drug of choice to improve cardiac contraction in
CHF patient?
5. Severe respiratory complication in fluid overload?
6. Early sign of cerebral edema?
7. Therapeutic and diagnostic mx in pleural effusion?
Thank you
FLUID POST TEST
20 ITEMS
1. A client who is admitted with malnutrition and
anorexia secondary to chemotherapy is also
exhibiting generalized edema. The client asks the
nurse for an explanation for the edema. Which of
the following is the most appropriate response by
the nurse?
A. The fluid is an adverse reaction to chemotherapy.
B. A decrease in activity has allowed extra fluid to
accumulate in the tissues.
C. Poor nutrition has caused decreased blood protein
levels and fluid has moved from the blood vessels
into the tissues.
D. Chemotherapy has increased your blood pressure
and fluid was forced out into the tissues.
2. A client who has a recent surgery has been
vomiting and becomes dizzy while standing up
to go to the bathroom. After assisting the
client back to bed, the nurse notes that the
blood pressure is 55/30 and the pulse is 140.
The nurse hangs which of the following IV
fluids to correct this condition?
A. D5.45 NS at 50 ml/hr
B. 0.9 NS at a rate of 1,000ml/hr
C. D5W at 125 ml/hr
D. 0.45 NS at open rate.
3. The client who has undergone an exploratory
laparotomy and subsequent removal of a large
intestinal tumor has a nasogastric tube (NGT) in
place and an IV running at 150 mL/hr via an IV
pump. Which data should be reported immediately
to the health care provider?
A. The pump keeps sounding an alarm that the high
pressure has been reached.
B. Intake is 1800 mL, NGT output is 550 mL, and Foley
output 950 mL.
C. On auscultation, crackles and rales in all lung fields
are noted.
D. Client has negative pedal edema and an increasing
level of consciousness.
4. The client diagnosed with diabetes insipidus
weighed 180 pounds when the daily weight
was taken yesterday. This morning's weight is
175.6 pounds. One liter of fluid weighs
approximately 2.2 pounds. How much fluid
has the client lost (in milliliters)?
A. 500 mL
B. 1000 mL
C. 2000 mL
D. 4400 mL
5. The nurse writes the nursing problem of "fluid
volume excess" (FVE). Which intervention
should be included in the plan of care?
A. Change the IV fluid from 0.9% NS to D5W.
B. Restrict the client's sodium in the diet.
C. Monitor blood glucose levels.
D. Prepare the client for hemodialysis.
6. The client has received IV solutions for three
(3) days through a 20-gauge IV catheter
placed in the left cephalic vein. On morning
rounds the nurse notes the IV site is tender to
palpation and a red streak has formed. Which
action should the nurse implement first?
A. Start a new IV in the right hand.
B. Discontinue the intravenous line.
C. Complete an incident record.
D. Place a warm application over the
site.
7. The nurse and an unlicensed nursing assistant
are caring for a group of clients. Which
nursing intervention should the nurse perform?
A. Measure the client's output from the
indwelling catheter.
B. Record the client's vital signs
C. Instruct the client on appropriate fluid
restrictions.
D. Provide water for a client diagnosed with
diabetes insipidus.
8. A nurse is reading a physician's progress
notes in the client's record and reads that the
physician has documented "sensible fluid loss
of approximately 800 mL daily." The nurse
understands that this type of fluid loss can
occur through:
A. The skin
B. Urinary output
C. Wound drainage
D. The gastrointestinal tract
9. A nurse is assigned to care for a group of
clients. On review of the clients' medical
records, the nurse determines that which
client is at risk for deficient fluid volume?
A. A client with a colostomy
B. A client with congestive heart failure
C. A client with decreased kidney function
D. A client receiving frequent wound
irrigations
10. A nurse caring for a client who has been
receiving intravenous diuretics suspects that
the client is experiencing a deficient fluid
volume. Which assessment finding would the
nurse note in a client with this condition?
A. Lung congestion
B. Increased hematocrit
C. Increased blood pressure
D. Increased central venous pressure (CVP)
11. A nurse is assigned to care for a group of
clients. On review of the clients' medical
records, the nurse determines that which
client is at risk for excess fluid volume?
A. The client taking diuretics
B. The client with renal failure
C. The client with an ileostomy
D. The client who requires gastrointestinal
suctioning
12. The nurse is caring for a client with
congestive heart failure. On assessment, the
nurse notes that the client is dyspneic and
that crackles are audible on auscultation. The
nurse suspects excess fluid volume. What
additional signs would the nurse expect to
note in this client if excess fluid volume is
present?
A. Weight loss
B. Flat neck and hand veins
C. An increase in blood pressure
D. A decreased central venous pressure (CVP)
13. A nurse is caring for a client with a
nasogastric tube. Nasogastric tube irrigations
are prescribed to be performed once every
shift. The client's serum electrolyte results
indicate a potassium level of 4.5 mEq/L and a
sodium level of 132 mEq/L. Based on these
laboratory findings, the nurse selects which
solution to use for the nasogastric tube
irrigation?
A. Tap water
B. Sterile water
C. Normal Saline
D. Distilled water
14. Our cells move substances across a
membrane with the use of energy through
ATP because of the ff reasons EXCEPT:
A. The substances may be too large
B.Substances may be difficult to dissolve in a fat
core
C. The substances moves downhill against a
gradient
D. The substances move uphill against a
gradient
15. The nurse is aware that ascites can be
related to a diminished plasma proteins. The
nurse administer albumin to the patient to
assist in:
A. clotting of blood
B. activation of WBC
C. formation of RBC
D. development of oncotic pressure
16. Who among the ff clients is most prone to
dehydration?
A. A 45 y/o male who had undergone
cholecystectomy
B. A 24 y/o female who is experiencing nausea
and vomiting
C. A 4 month old infant with diarrhea
D. A 17 y/o male with fever
17. Signs and symptoms of ECF volume deficit
does not include which of the ff?
A. weight loss, poor skin turgor
B. thirst, dry mouth and mucous membrane
C. oliguria, dark concentrated urine
D. decreased hematocrit, decreased specific
gravity
18. Which of the ff is the most accurate
indicator of edema?
A. skin turgor
B. serum sodium levels
C. weight gain
D. appearance of the skin in the legs
19. Edema occurs because of the ff mechanisms
EXCEPT:
A. increased venous hydrostatic pressure
B. increased aldosterone secretion
C. decreased ADH secretion
D. decreased colloidal osmotic pressure
20. Solutes move from an area o f higher
concentration to an area of lower
concentration. The process involves:
A. Diffusion
B. Osmosis
C. Filtration
D. Active transport
FLUIDS POST TEST KEY ANSWER
1. A client who is admitted with malnutrition and
anorexia secondary to chemotherapy is also
exhibiting generalized edema. The client asks the
nurse for an explanation for the edema. Which of
the following is the most appropriate response by
the nurse?
A. The fluid is an adverse reaction to chemotherapy.
B. A decrease in activity has allowed extra fluid to
accumulate in the tissues.
C. Poor nutrition has caused decreased blood protein
levels and fluid has moved from the blood vessels
into the tissues.
D. Chemotherapy has increased your blood pressure
and fluid was forced out into the tissues.
2. A client who has a recent surgery has been
vomiting and becomes dizzy while standing up
to go to the bathroom. After assisting the
client back to bed, the nurse notes that the
blood pressure is 55/30 and the pulse is 140.
The nurse hangs which of the following IV
fluids to correct this condition?
A. D5.45 NS at 50 ml/hr
B. 0.9 NS at a rate of 1,000ml/hr
C. D5W at 125 ml/hr
D. 0.45 NS at open rate.
3. The client who has undergone an exploratory
laparotomy and subsequent removal of a large
intestinal tumor has a nasogastric tube (NGT) in
place and an IV running at 150 mL/hr via an IV
pump. Which data should be reported immediately
to the health care provider?
A. The pump keeps sounding an alarm that the high
pressure has been reached.
B. Intake is 1800 mL, NGT output is 550 mL, and Foley
output 950 mL.
C. On auscultation, crackles and rales in all lung fields
are noted.
D. Client has negative pedal edema and an increasing
level of consciousness.
4. The client diagnosed with diabetes insipidus
weighed 180 pounds when the daily weight
was taken yesterday. This morning's weight is
175.6 pounds. One liter of fluid weighs
approximately 2.2 pounds. How much fluid
has the client lost (in milliliters)?
A. 500 mL
B. 1000 mL
C. 2000 mL
D. 4400 mL
5. The nurse writes the nursing problem of "fluid
volume excess" (FVE). Which intervention
should be included in the plan of care?
A. Change the IV fluid from 0.9% NS to D5W.
B. Restrict the client's sodium in the diet.
C. Monitor blood glucose levels.
D. Prepare the client for hemodialysis.
6. The client has received IV solutions for three
(3) days through a 20-gauge IV catheter
placed in the left cephalic vein. On morning
rounds the nurse notes the IV site is tender to
palpation and a red streak has formed. Which
action should the nurse implement first?
A. Start a new IV in the right hand.
B. Discontinue the intravenous line.
C. Complete an incident record.
D. Place a warm application over the
site.
7. The nurse and an unlicensed nursing assistant
are caring for a group of clients. Which
nursing intervention should the nurse perform?
A. Measure the client's output from the
indwelling catheter.
B. Record the client's vital signs
C. Instruct the client on appropriate fluid
restrictions.
D. Provide water for a client diagnosed with
diabetes insipidus.
8. A nurse is reading a physician's progress
notes in the client's record and reads that the
physician has documented "sensible fluid loss
of approximately 800 mL daily." The nurse
understands that this type of fluid loss can
occur through:
A. The skin
B. Urinary output
C. Wound drainage
D. The gastrointestinal tract
9. A nurse is assigned to care for a group of
clients. On review of the clients' medical
records, the nurse determines that which
client is at risk for deficient fluid volume?
A. A client with a colostomy
B. A client with congestive heart failure
C. A client with decreased kidney function
D. A client receiving frequent wound
irrigations
10. A nurse caring for a client who has been
receiving intravenous diuretics suspects that
the client is experiencing a deficient fluid
volume. Which assessment finding would the
nurse note in a client with this condition?
A. Lung congestion
B. Increased hematocrit
C. Increased blood pressure
D. Increased central venous pressure (CVP)
11. A nurse is assigned to care for a group of
clients. On review of the clients' medical
records, the nurse determines that which
client is at risk for excess fluid volume?
A. The client taking diuretics
B. The client with renal failure
C. The client with an ileostomy
D. The client who requires gastrointestinal
suctioning
12. The nurse is caring for a client with
congestive heart failure. On assessment, the
nurse notes that the client is dyspneic and
that crackles are audible on auscultation. The
nurse suspects excess fluid volume. What
additional signs would the nurse expect to
note in this client if excess fluid volume is
present?
A. Weight loss
B. Flat neck and hand veins
C. An increase in blood pressure
D. A decreased central venous pressure (CVP)
13. A nurse is caring for a client with a
nasogastric tube. Nasogastric tube irrigations
are prescribed to be performed once every
shift. The client's serum electrolyte results
indicate a potassium level of 4.5 mEq/L and a
sodium level of 132 mEq/L. Based on these
laboratory findings, the nurse selects which
solution to use for the nasogastric tube
irrigation?
A. Tap water
B. Sterile water
C. Normal Saline
D. Distilled water
14. Our cells move substances across a
membrane with the use of energy through
ATP because of the ff reasons EXCEPT:
A. The substances may be too large
B.Substances may be difficult to dissolve in a fat
core
C. The substances moves downhill against a
gradient
D. The substances move uphill against a
gradient
15. The nurse is aware that ascites can be
related to a diminished plasma proteins. The
nurse administer albumin to the patient to
assist in:
A. clotting of blood
B. activation of WBC
C. formation of RBC
D. development of oncotic pressure
16. Who among the ff clients is most prone to
dehydration?
A. A 45 y/o male who had undergone
cholecystectomy
B. A 24 y/o female who is experiencing nausea
and vomiting
C. A 4 month old infant with diarrhea
D. A 17 y/o male with fever
17. Signs and symptoms of ECF volume deficit
does not include which of the ff?
A. weight loss, poor skin turgor
B. thirst, dry mouth and mucous membrane
C. oliguria, dark concentrated urine
D. decreased hematocrit, decreased specific
gravity
18. Which of the ff is the most accurate
indicator of edema?
A. skin turgor
B. serum sodium levels
C. weight gain
D. appearance of the skin in the legs
19. Edema occurs because of the ff mechanisms
EXCEPT:
A. increased venous hydrostatic pressure
B. increased aldosterone secretion
C. decreased ADH secretion
D. decreased colloidal osmotic pressure
20. Solutes move from an area o f higher
concentration to an area of lower
concentration. The process involves:
A. Diffusion
B. Osmosis
C. Filtration
D. Active transport
Sonny M. Moreno, RN, USRN, MAN
2012
Key Points
Water
Ionized Electrolytes
Cations and Anions
Hormones
Kidneys
Small Intestine
What is Electrolyte?
An electrolyte is any substance
containing free ions that make the
substance electrically conductive.
Functions of Electrolytes
Blood volume regulation
Maintains Plasma osmolality
Muscle relaxation
Muscle contraction
Energy formation
Bones and teeth formation
Nutrients metabolism
Nerve impulse transmission
Buffer system
Electrolytes Imbalance
Drill
1. Major IC cations?
2. Major EC cations?
3. Hormone that regulates Na?
4. Hormone that regulates Ca?
5. Hormone that regulates PO4?
6. Electrolytes imbalance during Acidosis?
Sodium
Fxn:
Maintains plasma osmolality
Important for nerve impulse
transmission (PISO)
Normal value: 135-145 mEq/L
RDA: 0.5 2.7 6.0 gm/day
Source: canned foods, cheese,
ketchup
Regulated by Aldosterone
HYPERNATREMIA
Cause: Cushings Disease,
DI and FVD
S/sx:
brain activity
Excessive thirst
Seizure
brain activity
Flushed skin
Dx: Hct, plasma osmo
135 mEq/L
Mngmt: restrict Na and
hydrate (D5W)
HYPONATREMIA
Cause: Addisons Disease,
SIADH and FVE (CRF
& CHF)
S/sx: mimics hypogly,
stroke, bells palsy
brain activity
Weakness
Abdl spasm
Cerebral edema*
Dx: Hct, plasma osmo
145 mEq/L
Mngmt: restrict H2O and
give Na oral (Sodium
Tablet ) and IV (NaCl)
Drill
1. Normal value of serum Na? 135-145 mEq/L
2. Severe complication of hyponatremia?addisons Dse
3. Hct level in hypernatremia? Increase
4. Typical manifestation of hypernatremia? restrict Na
5. IVF for hypernatremia? D5w
6. IVF that must be avoided in hyponatremia? NaCl
7. High level of aldosterone leads to what electrolytes
imbalance? Sodium
8. Best Salt substitute? KCl
Potassium
Fxn:
Inhibits cardiac excitability
Muscle relaxation
Normal value: 3.5-5.0 mEq/L
Source: banana, orange,
potato or any fresh fruits
and raw vegetables, salt
substitute (KCl)
Mainly excreted by the
kidneys
HYPERKALEMIA
Cause: RF, Addisons ,
Tissue Injuries
s/sx:
Muscle: flaccidity to
weakness
GIT: diarrhea
Heart: brady,
Arrhythmias
(peaked T wave)
Dx: 5.0 mEq/L
Mngmt: Kayexalate,
Insulin+Glucose and
DIALYSIS
Calcium Gluconate to
improve heart contraction
HYPOKALEMIA
Cause: Cushings, Diuretics,
Laxatives, Insulin
S/sx:
Muscle: spasticity to
weakness
GIT: constipation
Heart: tachy to A and
inverted T wave, U wave
appearance
Note: digoxin toxicity
Dx: 3.5. mEg/L
Mngmt: oral K, tablet
(Kalium Durule) and IV
(KCl)
Kayexalate
Sodium Polystyrene Sulfonate
Resin Exchange (K loss, Na absorption)
Oral and enema administration
Lowers serum K
Calcium Gluconate
Given to strengthen cardiac contractions
Mix with D5W only (titration)
KCl Administration
40 mEq/L:1LPNSS
10 mEq/hour (max dose)
Cardiac monitor
Agitate freq.
Drill
1. ECG pattern in hypokalemia?
2. ER situation in hyperkalemia?
3. Drug of choice in hyperkalemia to improve cardiac
output? calcium gluconate
4. Maximum concentration of IV KCl? 10 mEq/hour
5. Insulin is given during which K imbalance?
hyperkalemia
6. K imbalance during 2
nd
stage of ARF?
7. GIT disturbance in hypokalemia?constipation
8. Which electrolyte must be checked to client taking
Digitalis?
Calcium
Fxn:
muscle contraction
Helps in blood coagulation (CF
4)
Bones and teeth formation
Normal value:
4.5-5.5 mEq/L
8.5-10.5 mg/dl
RDA: 800 1200 mg/day
Source: dairy products (milk,
cheese, yogurt) and g.l.v.
BINDS with albumin
Requires Active Vitamin D to be
absorbed from the intestines
Regulated by Parathyroid glands
Active Vitamin D
Parathyroid Glands
Parathyroid Glands
HYPERCALCEMIA
Cause:
Hyperparathyhroidism
S/sx: 5.5 mEq/L
deep bone pain,
lithiasis formation
Shortened QT interval
HYPOPHOSPHATEMIA
(low energy store)
Mngmt:
parathyroidectomy,
hydration,
prevent fracture,
reduce Ca intake,
Calcitonin
DIALYSIS
HYPOCALCEMIA
Cause: Hypoparathyhroidism
S/sx: 4.5 mEq/L
TETANY: tingling,
trousseau, chvostek and
laryngeal spasm*
Lengthened QT interval
Torsades de pointes
HYPERPHOSPHATEMIA
(wide calcification)
Mngmt:
Oral Ca, tablet Ca and IV
(Calcium Gluconate)
respiratory support for
laryngeal spasm (TT)
Tetany
Drill
1. Normal value of serum Ca? 4.5- 5.5 mEq/L
2. Danger sign of tetany?Tingling, Chvostek,
trosseau
3. Aids in Ca absorption?
4. Safety precautions in hypercalcemia?
5. Drug that will push serum Ca into the bones?
6. Early observable signs of Tetany? chvostek
7. Must on the bedside post thyroidectomy?
8. 3 targets of PTH?
HYPERPHOSPHATEMIA ( 2.6)
Cause: Excessive intake of P,
Hypoparathyroidism, High risk
(infants fed with cows milk)
S/sx: Wide-spread calcification,
Visual impairment, Decreased
mental status
Mx:
Treat the underlying cause
Restrict all forms of P
supplements
Give phosphate binding agent
(laxative) Aluminum Magnesium
or Calcium Gel, AMPHOGEL,
OSCAL
Dialysis
HYPOPHOSPHATEMIA ( 1.8)
Cause: diuretics, insulin,
malabsorption
S/sx: Low energy store (prioritize
the problem), Organ failure
Mx:
Treat the underlying cause
Increase P supplements
Oral (eggs, nuts, whole grains
and meat)
IV (KP04 maximum of 10
mEq/hour) or NaP04
Monitor respiratory status
Magnesium
Function:
Aids in nerve impulse
transmission
Plays a role for nutrients
metabolism
Positively charged ion
(cation)
Normal value: 1.5-2.6 mEq/L
Source: chocolates, dry
beans, meats, nuts,
seafoods
Regulated by
Parathormone
Hypermagnesemia
Cause: RF most
common
S/sx: 2.6 mEq/L
DTR (0, +1)
brain activity,
LOC to coma
HYPERCALCEMIA
Mngmt: laxatives,
diuretics, DIALYSIS
Hypomagnesemia
Cause: laxatives,
diuretics, alcoholism
S/sx: 1.5 mEq/L
DTR (+3, +4)
brain activity
(seizure)
HYPOCALCEMIA
Mngmt: oral Mg,
tablet Mg, MgSO4
parenteral
Chloride
Acid by nature
Found in the GIT
98-106 mEq/L
Goes with all electrolytes
Drill
1. High serum Cl leads to Acidosis or Alkalosis?
2. DTR in hypomagnesemia?
3. Drug of choice to lower serum PO4?
4. Normal serum level of PO4?
5. Hyperreflexia and DTR of 4 is a sign of
hypermagnesemia or hypomagnesemia?
Thank you
ABG
Sonny M. Moreno, RN, USRN, MAN
What is ABG?
ABG Indications?
Metabolic Disorders
DM
Vomiting and Diarrhea
Renal Failure
Shock
Respiratory Disorders
COPD
Cardiac Problems
What will happen if there is an
acid imbalance?
The Process.
1. Buffer system
2. Respiratory regulation
3. Renal regulation
Body on work
H2CO3
H + HCO3
H2CO3
H2CO3
H2O & CO2
H2O
CO
2
Kidne
ys
Lungs
ABG Collection of Specimen
Baseline v/s
Allens Test
Heparin
Site care
Allen's test
Elevate the hand and make a fist for
approximately 30 seconds.
Apply pressure over the ulnar and the radial
arteries occluding both (keep the hand
elevated).
Open the hand which will be blanched.
Release pressure on the ulnar artery and look
for perfusion of the hand (this takes under 8
seconds).
If there is any delay then it may not be safe to
perform radial artery puncture.
Handling of the specimen
Label
Bubbles free
Dont agitate
Avoid warm
Site
care?
ABG Interpretation
ABG Normal Values
pH 7.35-7.45
HC03 22.26 mEq/L
Pa C02 35-45 mm Hg
Pa 02 80-100 mm Hg
FI02 20%
Base Excess +/- (2 mmol/L)
7.8
5
6.5
0
NV: 7.35-7.45, 22-26, 35-45
HCO3:alkali, CO2:acid
pH = 7.40 N
HCO3 = 20
PaCO2 = 40 N
Simple Metabolic Acidosis
pH = 7.40 N
HCO3 = 28
PaCO2 = 40 N
Simple Metabolic Alkalosis
pH = 7.40 N
HCO3 = 24 N
PaCO2 = 48
Simple Respiratory Acidosis
pH = 7.40 N
HCO3 = 24 N
PaCO2 = 32
Simple Respiratory Alkalosis
NV: 7.35-7.45, 22-26, 35-45
RO-ME (to pH)*
pH = 7.33
HCO3 = 20
PaCO2 = 40 N
Metabolic Acidosis
pH = 7.47
HCO3 = 28
PaCO2 = 40 N
Metabolic Alkalosis
pH = 7.47
HCO3 = 24 N
PaCO2 = 32
Respiratory Alkalosis
pH = 7.33
HCO3 = 24 N
PaCO2 = 48
Respiratory Acidosis
NV: 7.35-7.45, 22-26, 35-45
HCO3 and CO2 both acids or alkalis (pH)*
pH = 7.33
HCO3 = 20
PaCO2 = 48
Mixed Acidosis
pH = 7.40 N
HCO3 = 28
PaCO2 = 32
Mixed Alkalosis
pH = 7.33
HCO3 = 20
PaCO2 = 48
Mixed Acidosis
pH = 7.40 N
HCO3 = 28
PaCO2 = 32
Mixed Alkalosis
NV: 7.35-7.45, 22-26, 35-45
Observe the arrows of HCO3 and CO2 (pH)*
Primary problem will follow the pH*
pH = 7.33
HCO3 = 20
PaCO2 = 32
Uncompensated Metabolic Acidosis
pH = 7.47
HCO3 = 28
PaCO2 = 48
Uncompensated Metabolic Alkalosis
pH = 7.33
HCO3 = 28
PaCO2 = 48
Uncompensated Respiratory Acidosis
pH = 7.47
HCO3 = 20
PaCO2 = 32
Uncompensated Respiratory Alkalosis
NV: 7.35-7.45, 22-26, 35-45
Observe the arrows of HCO3 and CO2 (pH)*
Primary problem, check the difference*
Fully (pH:7.40)*
Partially (pH with in normal range)*
pH = 7.40 N
HCO3 = 18
PaCO2 = 32
Compensated Metabolic Acidosis
pH = 7.35 N
HCO3 = 30
PaCO2 = 48
Compensated Metabolic Alkalosis
pH = 7.40 N
HCO3 = 28
PaCO2 = 48
Compensated Respiratory Acidosis
pH = 7.44 N
HCO3 = 20
PaCO2 = 32
Compensated Respiratory Alkalosis
Key to ABG Interpretation
pH is alkali by nature
HCO3 is alkali by nature
CO2 is acid by nature
ROME
Opposite () Mixed
Same () () Compensated or
Uncompensated
Drill 5
pH 7.40
CO2 47
HCO3 29
Fully Compensated Metabolic Alkalosis
Drill 4
pH 7.47
CO2 34
HCO3 20
Uncompensated Respiratory Alkalosis
Drill 3
pH 7.39
CO2 46
HCO3 19
Mixed Acidosis
Drill 2
pH 7.33
CO2 46
HCO3 25
Respiratory Acidosis
Drill 1
pH 7.32
CO2 33
HCO3 20
Uncompensated Metabolic Acidosis
Thank you
Four-Step Guide to ABG Analysis
1. Is the pH normal, acidotic or alkalotic?
2. Are the PaCO2 or HCO3 abnormal? Which
one appears to influence the pH?
3. If both the PaCO2 and HCO3 are abnormal,
the one which deviates most from the norm
is most likely causing an abnormal pH.
4. Check the PaO2. Is the patient hypoxic?
http://www.manuelsweb.com/abg.htm
Swearingen's handbook (1990)
To Interpret ABG
Compensation can be seen when both the
PaCO2 and HCO3 rise or fall together to
maintain a normal pH.
Uncompensated occurs when the PaCO2 and
HCO3 rise or fall together but the pH remains
abnormal.
Compensated occurs when the PaCO2 and
HCO3 rise or fall together and the pH returns
to normal.
Sample Lab results:
Simple Metabolic Acidosis
Metabolic Acidosis
Mixed Acidosis
Uncompensated Metabolic Acidosis
Compensated Metabolic Acidosis
Fully
Partially
http://www.manuelsweb.com/abg.htm
Swearingen's handbook (1990)
Once it fails!
MANIFESTATIONS
METABOLIC ACIDOSIS
Weakness
Headache
Disorientation
Deep rapid breathing
Nausea and vomiting
Coma
CAUSE: DKA, terminal CA,
RF, starvation, DIARRHEA
RESPIRATORY ACIDOSIS
Dyspnea
Irritability
Disorientation
Tachycardia
Cyanosis
Coma
CAUSE: COPD, airway
obtruction, apnea
MANIFESTATIONS
METABOLIC ALKALOSIS
Muscle hypertonicity
(tetany)
Tingling
Tremors
Shallow and slow
respiration
Dizziness, confusion
Coma
CAUSE: gastric lavage,
gastric suctioning
RESPIRATORY ALKALOSIS
Deep rapid breathing
Lightheadedness
Tingling, numbness
Tinnitus
Loss of consciousness
CAUSE: anxiety, CPR
Role of water?
- +
EC
IC
Types
of Ions
CATIONS OR POSITIVE CHARGE
1. Magnesium
2. Calcium
3. Sodium
4. Hydrogen
5. Potassium
ANIONS OR NEGATIVE CHARGE
1. Chloride
2. Bicarbonate
3. Phosphate
What regulates ionized electrolytes?
Intestine
Circulation
Kidneys
Hormones*
Hormones that regulates ionized electrolytes?
Na
K
Mg
Ca
PO4
Cl
Endogenous
Exogenous
Key Points!
Major source: food intake
Excretion: kidneys, GIT, sweat,
Easily disturbed in case of Acid
Base Imbalance
Imbalance is usually
associated with diseases:
DM
DI and SIADH
BURNS
CHF and CRF
DIARRHEA
CUSHINGS and ADDISONS
ACIDOSIS and ALKALOSIS
Also DRUGS: Laxatives, Diuretics
Which is more important in diagnosing
electrolytes imbalance?
IV
IC
URIN
E
IT
RECALL!
1. Mg 1.5-2.6 320-420mg/d
2. P 1.8-2.6 700mg/d
3. K 3.5-4.5 200-250mg/d
4. Ca 4.5-5.5 800-1200mg/d
5. Cl 98-106 750mg/d
6. Na 135-145 2,400 mg/d
7. H 7.35-7.45(pH)
8. HCO3 22-26 mEq/L
RDA NORMAL V. Functions
iNurse Hope
You might also like
- Mabes Fluid and Electrolyte ImbalancesDocument15 pagesMabes Fluid and Electrolyte ImbalancesMabesNo ratings yet
- Different Iv FluidsDocument2 pagesDifferent Iv FluidsBeverly DatuNo ratings yet
- Preeclampsia Eclampsia and Hellp SyndromeDocument24 pagesPreeclampsia Eclampsia and Hellp Syndromeapi-403416350100% (1)
- Neurologic NursingDocument10 pagesNeurologic NursingAllisson Beckers100% (1)
- Fluidsandelectrolytes 090224074347 Phpapp02Document102 pagesFluidsandelectrolytes 090224074347 Phpapp02IsaacJ22No ratings yet
- Concept Map SepsisDocument4 pagesConcept Map SepsisSavanna ChambersNo ratings yet
- Fluid Electrolytes and Acid Base BalanceDocument108 pagesFluid Electrolytes and Acid Base BalancesayednourNo ratings yet
- Hemorrhagic Cerebro Vascular DiseaseDocument37 pagesHemorrhagic Cerebro Vascular Diseasejbvaldez100% (1)
- Acute Kidney Injury (AKI) :: FeaturesDocument3 pagesAcute Kidney Injury (AKI) :: FeaturesDavid PerezNo ratings yet
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDocument42 pagesHepatobiliary Disorders: Katrina Saludar Jimenez, R. NKatrinaJimenezNo ratings yet
- AnemiaDocument35 pagesAnemiaAgus SyaifudinNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Med-Surg Nusing BulletsDocument65 pagesMed-Surg Nusing BulletsHarley C. Tan100% (1)
- Competency Appraisal Midterm ExaminationsDocument9 pagesCompetency Appraisal Midterm ExaminationsRellie Castro100% (1)
- Cardiac Conditions Cardiac Dysrhythmias: B. Sinus BradycardiaDocument5 pagesCardiac Conditions Cardiac Dysrhythmias: B. Sinus BradycardiaIrish Eunice FelixNo ratings yet
- Fluid and ElectrolytesDocument12 pagesFluid and ElectrolytesKristine Castillo100% (2)
- Insulin AdministrationDocument15 pagesInsulin Administrationmec17No ratings yet
- Alteration in Fluid and Electrolyte Status Lecture NotesDocument11 pagesAlteration in Fluid and Electrolyte Status Lecture Notes0912247251No ratings yet
- Hepatobiliary DisordersDocument2 pagesHepatobiliary DisordersFreeNursingNotes0% (1)
- Acute Rheumatic FeverDocument50 pagesAcute Rheumatic Feversunaryo lNo ratings yet
- Test Quiz Hypo Kale MiaDocument6 pagesTest Quiz Hypo Kale MiaVivian Montesena BreganzaNo ratings yet
- Assessment Renal CalculiDocument2 pagesAssessment Renal CalculiLeslie LuscombeNo ratings yet
- Antipsychotic Drugs: Conventional AntipsychoticsDocument16 pagesAntipsychotic Drugs: Conventional AntipsychoticsApple MaeNo ratings yet
- Obstetric Case Study CesarianDocument16 pagesObstetric Case Study CesarianRazan NasereddineNo ratings yet
- Pediatric Vital Sign Normal RangesDocument5 pagesPediatric Vital Sign Normal Rangestinea nigraNo ratings yet
- Fluids and ElectrolytesDocument17 pagesFluids and ElectrolytesNano BaddourNo ratings yet
- Growth and Development Growing Complex Phenomenon of A Structure or Whole GrowthDocument69 pagesGrowth and Development Growing Complex Phenomenon of A Structure or Whole GrowthYna RamiroNo ratings yet
- Nursing Skills: Blood Transfusion/ Iv TherapyDocument6 pagesNursing Skills: Blood Transfusion/ Iv TherapyVince John SevillaNo ratings yet
- Medical Surgical NursingDocument66 pagesMedical Surgical Nursing04eden100% (3)
- NCM 116: Care of Clients With Problems in Nutrition and Gastrointestinal, Metabolism and Endocrine,, Acute and ChronicDocument18 pagesNCM 116: Care of Clients With Problems in Nutrition and Gastrointestinal, Metabolism and Endocrine,, Acute and ChronicSIJINo ratings yet
- Hematologic DiseasesDocument11 pagesHematologic DiseasesPerrilyn Perey100% (2)
- Acute and Chronic PyelonephritisDocument7 pagesAcute and Chronic PyelonephritisMatthew Ryan100% (1)
- Cardiac Condition NCM 112Document10 pagesCardiac Condition NCM 112Irish Eunice FelixNo ratings yet
- Endocrine DisordersDocument16 pagesEndocrine DisordersEiffel AnchetaNo ratings yet
- Urinary System DisordersDocument120 pagesUrinary System DisordersFaith Levi Alecha Alferez100% (1)
- Endocrine DisordersDocument3 pagesEndocrine DisordersIrish OrleansNo ratings yet
- Genito Urinary NursingDocument6 pagesGenito Urinary NursingAbdallah AlwawiNo ratings yet
- Summary Notes For Studying Fluid and ElectrolytesDocument8 pagesSummary Notes For Studying Fluid and ElectrolytesCandace Mead100% (1)
- Pharmacology - Section 23 - Antibiotics 2Document5 pagesPharmacology - Section 23 - Antibiotics 2Pathalee ThalpavilaNo ratings yet
- Iv Fluids and Solutions With Nursing ResponsibilitiesDocument33 pagesIv Fluids and Solutions With Nursing ResponsibilitiesJennie JalemNo ratings yet
- Fluids Electrolytes - Acid-Base BalanceDocument11 pagesFluids Electrolytes - Acid-Base BalanceJhosita Flora Laroco100% (1)
- Antepartum PeriodDocument3 pagesAntepartum PeriodjisooNo ratings yet
- Medical Surgical Nursing - LectureDocument77 pagesMedical Surgical Nursing - LecturePink Majaila GludoNo ratings yet
- Git HandoutsDocument49 pagesGit HandoutsCharlz Zipagan100% (1)
- FBCDocument14 pagesFBCJane GarciaNo ratings yet
- 81 HematologyDocument18 pages81 HematologyLuis Perez100% (5)
- Module 4 Nursing ProcessDocument14 pagesModule 4 Nursing ProcessArjay Cuh-ingNo ratings yet
- Endocrine Med-Surg Slide Show Presentation (Nursing)Document43 pagesEndocrine Med-Surg Slide Show Presentation (Nursing)loveoverprideNo ratings yet
- Dissiminated Intravascular Coagulation PathoDocument2 pagesDissiminated Intravascular Coagulation Pathoapi-341263362No ratings yet
- 90 Pharmacology and Parenteral Therapy NCLEXDocument30 pages90 Pharmacology and Parenteral Therapy NCLEXHope YanesNo ratings yet
- Fluid and Electrolytes Case StudyDocument2 pagesFluid and Electrolytes Case StudyJamie Wiebe100% (8)
- Pyschiatric Nursing SummarizeDocument39 pagesPyschiatric Nursing SummarizeKyssel Seyer100% (1)
- HIV AIDS NCLEX Questions Nursing Review QuizDocument10 pagesHIV AIDS NCLEX Questions Nursing Review QuizShella Mae UsquisaNo ratings yet
- Summary of Normal Laboratory ValuesDocument7 pagesSummary of Normal Laboratory ValuesIvan Matthew SuperioNo ratings yet
- Iv FluidsDocument11 pagesIv FluidsDianna Rose BelenNo ratings yet
- MedSurg Nursing Case Study 1Document1 pageMedSurg Nursing Case Study 1Shahab SaqibNo ratings yet
- UrinalysisDocument9 pagesUrinalysisyuppierajNo ratings yet
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Introduction To LeadershipDocument1 pageIntroduction To LeadershipMaria VisitacionNo ratings yet
- UTI IntroDocument1 pageUTI IntroMaria VisitacionNo ratings yet
- 11 Nursing Core ResponsibilityDocument2 pages11 Nursing Core ResponsibilityMaria VisitacionNo ratings yet
- Dar 5Document1 pageDar 5Maria VisitacionNo ratings yet
- Nurse'S Notes (Dar Method)Document1 pageNurse'S Notes (Dar Method)Maria VisitacionNo ratings yet
- DAR SampleDocument1 pageDAR SampleMaria VisitacionNo ratings yet
- DAR Sample 2Document1 pageDAR Sample 2Maria VisitacionNo ratings yet
- Causes: Polycythemia VeraDocument15 pagesCauses: Polycythemia VeraMaria VisitacionNo ratings yet
- BibliographyDocument12 pagesBibliographyMaria VisitacionNo ratings yet
- Brain CancerDocument29 pagesBrain CancerMaria VisitacionNo ratings yet
- Triage 1Document3 pagesTriage 1Maria VisitacionNo ratings yet
- Congenital AnomaliesDocument26 pagesCongenital AnomaliesMaria VisitacionNo ratings yet
- Leukemia ReportDocument5 pagesLeukemia ReportCrisantaCasliNo ratings yet
- Critical Thinking PowerpointDocument16 pagesCritical Thinking PowerpointMaria VisitacionNo ratings yet
- Case FormatDocument12 pagesCase FormatMaria VisitacionNo ratings yet
- Nursing Pharmacology COMPLETEDocument40 pagesNursing Pharmacology COMPLETEMonique Leonardo100% (8)
- Autsim and Vitamin DDocument4 pagesAutsim and Vitamin DNo OneNo ratings yet
- Sfsac@xmu - Edu.my: To: From: FIS1012050@. Xmu - Edu.my Subject: Concern of Final Examination Amid Covid-19Document2 pagesSfsac@xmu - Edu.my: To: From: FIS1012050@. Xmu - Edu.my Subject: Concern of Final Examination Amid Covid-19Ahmad RazaNo ratings yet
- Psilocybin For Depression and Anxiety Associated With Life-Threatening IllnessesDocument2 pagesPsilocybin For Depression and Anxiety Associated With Life-Threatening IllnessesJosé Carlos Solís SuárezNo ratings yet
- AXA-Self Declaration FormDocument1 pageAXA-Self Declaration FormtanishqNo ratings yet
- Haad QuestionDocument20 pagesHaad QuestionNimraj PatelNo ratings yet
- Antibiotics CasesDocument39 pagesAntibiotics CasesnistaneNo ratings yet
- Childhood ObesityDocument30 pagesChildhood ObesityLeetal KarkayNo ratings yet
- CombinepdfDocument177 pagesCombinepdfPrincess RonsableNo ratings yet
- Your Dynamic Profile: Wellness ReportDocument17 pagesYour Dynamic Profile: Wellness Reportvica sibueaNo ratings yet
- Raminder Nirula - High-Yield Internal Medicine (High-Yield Series) - Lippincott Williams and Wilkins (2006)Document228 pagesRaminder Nirula - High-Yield Internal Medicine (High-Yield Series) - Lippincott Williams and Wilkins (2006)Isah Mohammed100% (1)
- Klasifikasi Dan DD MigrenDocument17 pagesKlasifikasi Dan DD MigrenYosephinNo ratings yet
- Disorders of Small IntestineDocument41 pagesDisorders of Small IntestineSamuel kuriaNo ratings yet
- Risk AssessmentDocument2 pagesRisk Assessmentapi-551545059No ratings yet
- Cholinergic SyndromeDocument3 pagesCholinergic SyndromeEmman AguilarNo ratings yet
- A Vegan PowerDocument3 pagesA Vegan PowerashankarNo ratings yet
- MSM Sulphur For HealthDocument7 pagesMSM Sulphur For HealthMasterOfHotGlass100% (1)
- Adime For DiabetesDocument2 pagesAdime For Diabetesapi-383891195No ratings yet
- Dengue NS1 RDT Annex 5-6Document4 pagesDengue NS1 RDT Annex 5-6Ga B B Orlongan100% (1)
- Mechanisms of Cataract Formation: Nicholas Phelps Brown MD, FRCS, FrcophthDocument7 pagesMechanisms of Cataract Formation: Nicholas Phelps Brown MD, FRCS, FrcophthQomariah RiaNo ratings yet
- CENE Course Outline On Psychiatric NursingDocument3 pagesCENE Course Outline On Psychiatric NursingJohn Ryan BuenaventuraNo ratings yet
- Chapter 22 Nursing Management of The Postpartum Woman at RiskDocument18 pagesChapter 22 Nursing Management of The Postpartum Woman at RiskSusanna ConigliaroNo ratings yet
- Kelompok 2 H2S 97-2003 PPT ToksikDocument38 pagesKelompok 2 H2S 97-2003 PPT ToksikHerfando Maulana AlhafizhNo ratings yet
- Nutri Lec ReviewerDocument182 pagesNutri Lec ReviewerRaquel MonsalveNo ratings yet
- Family Case Study: BLK 4. Room 7, Phase 5 Brgy. Dela PazDocument9 pagesFamily Case Study: BLK 4. Room 7, Phase 5 Brgy. Dela PazShamz SitiarNo ratings yet
- Fluids and Electrolytes ImbalancesDocument7 pagesFluids and Electrolytes Imbalancessinister17No ratings yet
- A Clinal Primer On Intellectual DisabilityDocument13 pagesA Clinal Primer On Intellectual DisabilityAra AzzahraNo ratings yet
- Heart Rate Variability Biofeedback Increases Baroreflex Gain and Peak Expiratory FlowDocument17 pagesHeart Rate Variability Biofeedback Increases Baroreflex Gain and Peak Expiratory FlowLuis A Gil PantojaNo ratings yet
- QuestionsDocument6 pagesQuestionsLorvic Andrew Juanson UmaliNo ratings yet