Professional Documents
Culture Documents
Infeksi Tulang Dan Persendian
Uploaded by
Theresia Merdeka PutriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Infeksi Tulang Dan Persendian
Uploaded by
Theresia Merdeka PutriCopyright:
Available Formats
Musculoskeletal Infection
Punto Dewo
Dept. of Orthopaedics & Traumatology
Bone and Joint Infection
Osteomyelitis
Septic arthritis
How do infecting organisms enter
bones or joints
Hematogenous spread
Inoculation through wounds
Extension from adjacent infected
structures
Inoculation
through
traumatic
wounds,
operations
Extension
from adjacent
infected
structures
Hematogenous spread
Bacteremia
Sluggish circulation in metaphysis
(in children)
Foci spread subperiosteal
abscess () draining sinus
(infants) foci spread through
growth plate
Involucrum : new bone formation
encircling cortical shaft
Sequestrum : dead bone surrounded by pus
or scar tissue
Acute hematogenous osteomyelitis
Male : female = 2 : 1
> 90% monostotic
> 90% lower extremity
The child limp or refuse to walk or
refuse to use the extremity involved
Early acute : w/in 24-48 hrs, only pain
and fever
Late acute : 4-5 days after onset,
subperiosteal abscess needs
surgical drainage
Neonates
Older children
Premature infants
Evaluation of Acute Osteomyelitis
CBC, ESR, CRP
Blood culture : ident. causative
organism in 50%
Bone aspiration : for subperiost
abscess, ident. 70%
X-Ray : could be normal
Bone scan Tc 99m
MRI scan
Treatment of Acute Osteomyelitis
I.V Antibiotic started promptly
S. aureus most common infecting
agent
Gram ()ve organism in vertebrae
and immunocomp pts
Surgery for late acute (draining
abscess)
Complications
Recurrent osteomyelitis : to minimize
AB coverage for 6 weeks
Distant seeding
Septic arthritis
Pathologic fracture due to
osteonecrosis
Growth arrest due to damaged gr. pl.
Subacute Hematogenous
Oeteomyelitis
Less virulent org + effective immune
response
Less clear onset, older children ( 2-
16 y.o), equiv sex ratio
No or mild fever, mild tenderness
Lab findings inconclusive
AB for 6 weeks
Chronic Hematogenous
Osteomyelitis
Sx several weeks-months
Developed vs developing countries
Child : neglected cases
Adult : secondary
Sequestra, involucrum, draining
sinus
Needs culture from bone/deep tissue
Treatment of Chronic Osteomyelitis
Aggressive debridement
Bone grafting
Antibiotic beads (local)
Soft tissue coverage
Systemic antibiotic for 6-12 weeks
Trisna Rahardja, M, 46 yo,
Chronic osteomyelitic of the distal third
of the left tibia and fibula post ORIF
on 2008
Didik R, M, 20 yo
Chronic osteomyelitis of the right tibia fibula with bone
defect post nailing
Septic Arthritis
More common in children < 5 y.o
S. aureus, > 95% monoarticular,
hematogenous or extension from
adjecent structures
41% knee, 23% hip, 14% ankle, 12%
elbow, 4% wrist, 4% shoulder
Cartilage eroded
Clinical feature
Pain and swelling in affected joint
Malaise, fever, limp, refuse to walk,
refuse to move extremity
(pseudoparalysis)
Joints held in comfy positions
CBC, ESR, X-Ray, joint aspiration
Synovial fluid analysis :
-Turbid
-Yellow to creamy pus
-WBC > 50.000/mm3
-Glucose decreased
Treatment of Septic Arthritis
i.v antibiotic promptly
Surgical irrigation and drainage
Open or arthroscopic
complications
Joint destruction
Bony ankylosis
Soft tissue ankylosis (Tuberculosis)
Clinical Feature
X-ray of the Left lower leg
Cellulitis
Subcutaneous
Less distinctive margins
Local signs + lymhadenopathy
Th/ Systemic + Local
Erysipelas
Similar to cellulitis BUT more
superficial
Well demarcated and painful plaque
Th/ Systemic + Local
Necrotizing Fasciitis
Muscle fascia
Aggressive and life threatening
Etiology : Streptococcus Group A
Requires emergent and extensive
surgical debridement
Gas Gangrene
Muscle
In grossly contaminated
traumatic wounds
Etiology :
Clostridium Perfringens
and Clostridium Welchii
Need surgical debridement
and fasciotomy
Hyperbaric chamber
therapy
You might also like
- James Arthur Say You Wont Let Go PDFDocument3 pagesJames Arthur Say You Wont Let Go PDFLim Yi Jin86% (7)
- Osteomyelitis: M.Rasoolinejad, MDDocument48 pagesOsteomyelitis: M.Rasoolinejad, MDRobert MedinaNo ratings yet
- Osteomyelitis: Mariamawit B Dbu, College of MedicineDocument34 pagesOsteomyelitis: Mariamawit B Dbu, College of MedicinedenekeNo ratings yet
- Study On Empowering Youth and Adults To Overcome Mental Health Hardships Using A Web ApplicationDocument6 pagesStudy On Empowering Youth and Adults To Overcome Mental Health Hardships Using A Web ApplicationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- OsteomyelitisDocument147 pagesOsteomyelitisAnkit Agur100% (1)
- Hematología - Williams (Tomo 1)Document1,036 pagesHematología - Williams (Tomo 1)LIliana100% (3)
- OsteomyelitisDocument11 pagesOsteomyelitisLorebell100% (7)
- MedicalDocument29 pagesMedicalZia Ur RehmanNo ratings yet
- National Health MissionDocument70 pagesNational Health Missionprabha krishnanNo ratings yet
- Common Communicable DiseasesDocument86 pagesCommon Communicable DiseasesBenj VillanuevaNo ratings yet
- Bone Infections - Acute OsteomyelitisDocument35 pagesBone Infections - Acute Osteomyelitismeto50% (4)
- OsteomyelitisDocument9 pagesOsteomyelitisTineLawrenceNo ratings yet
- Presented by Animesh Amal: Brand Plan On Salbutamol + Ambroxol + GuaifenesinDocument36 pagesPresented by Animesh Amal: Brand Plan On Salbutamol + Ambroxol + GuaifenesinAnonymous 75aETJ8ONo ratings yet
- OsteomyelitisDocument21 pagesOsteomyelitisSurgeonZak0% (1)
- Bone - Infection Tanpa AnotasiDocument75 pagesBone - Infection Tanpa AnotasirifanirdNo ratings yet
- Final HICC Manual AIIMSDocument35 pagesFinal HICC Manual AIIMSNaMakNo ratings yet
- Punto Dewo: Dept. of Orthopaedics & TraumatologyDocument37 pagesPunto Dewo: Dept. of Orthopaedics & Traumatologyamaya zifunNo ratings yet
- OsteomyelitisDocument41 pagesOsteomyelitisArumpaavai PugazhiniNo ratings yet
- Septic ArthritisDocument21 pagesSeptic ArthritisDawex IsraelNo ratings yet
- Bone and Joint InfectionDocument43 pagesBone and Joint Infectionraheeg siddigNo ratings yet
- Bone and Joint InfectionsDocument43 pagesBone and Joint InfectionsaugyeraNo ratings yet
- DR - Khaled Ata MD. Department of Orthopedic Faculty of MedicineDocument53 pagesDR - Khaled Ata MD. Department of Orthopedic Faculty of Medicineبراءة أحمد السلاماتNo ratings yet
- Infecti ON: Acute, Subacute and Chronic OsteomyelitisDocument32 pagesInfecti ON: Acute, Subacute and Chronic OsteomyelitisNardine RoslanNo ratings yet
- OsteomyelitisDocument32 pagesOsteomyelitisAndi Wija Indrawan PangerangNo ratings yet
- Review of Musculoskeletal TumorsDocument63 pagesReview of Musculoskeletal TumorsDanur AdiNo ratings yet
- Presentation 1Document120 pagesPresentation 1Khurram ChauhanNo ratings yet
- Grade 2 InfectionDocument29 pagesGrade 2 InfectionshaifNo ratings yet
- Osteomyelitis Septic Arthritis Etc 2021Document48 pagesOsteomyelitis Septic Arthritis Etc 2021Mohamed Anas SayedNo ratings yet
- Orthopedic DisordersDocument15 pagesOrthopedic Disordershasanatiya41No ratings yet
- Septicarthritis 110426090729 Phpapp02Document21 pagesSepticarthritis 110426090729 Phpapp02Diana MayasariNo ratings yet
- Neonatal surgical infection managementDocument43 pagesNeonatal surgical infection managementAhmad Abu KushNo ratings yet
- Septic ArthritisDocument12 pagesSeptic ArthritisRashi JainNo ratings yet
- INFECTIONS OF THE BONEDocument88 pagesINFECTIONS OF THE BONEEunike Arianny SipayungNo ratings yet
- Bone and Joint Infection: Dr. Zainab AbdulwahabDocument89 pagesBone and Joint Infection: Dr. Zainab Abdulwahabzen.maree6No ratings yet
- OsteomyelitisDocument47 pagesOsteomyelitisArmand Al HaraaniNo ratings yet
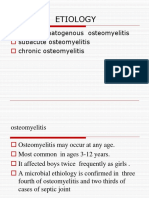
- Etiology: Acute Hematogenous Osteomyelitis Subacute Osteomyelitis Chronic OsteomyelitisDocument42 pagesEtiology: Acute Hematogenous Osteomyelitis Subacute Osteomyelitis Chronic OsteomyelitisNoe-pal DynmNo ratings yet
- 34 W11 OsteomylitisDocument32 pages34 W11 OsteomylitisAbdulelah MurshidNo ratings yet
- Osteomyelitis in Children 4911Document39 pagesOsteomyelitis in Children 4911M. Eka PutraNo ratings yet
- Osteomyelitis Causes, Symptoms, and TreatmentDocument4 pagesOsteomyelitis Causes, Symptoms, and TreatmentHidayu AliasNo ratings yet
- LARGE JOINTS IN HEALTH AND DiseaseDocument75 pagesLARGE JOINTS IN HEALTH AND DiseaseIdris Balasa IdrisNo ratings yet
- OsteomielitisDocument104 pagesOsteomielitisConstantia Rosa PattiselannoNo ratings yet
- OsteomyelitisDocument38 pagesOsteomyelitisRobel SirakNo ratings yet
- Osteomyelitis PDFDocument39 pagesOsteomyelitis PDFxxsaptxxNo ratings yet
- Child Presenting With Joint PainDocument22 pagesChild Presenting With Joint PainlagathurcNo ratings yet
- Osteomyelitis: By: Glowsy CabralDocument29 pagesOsteomyelitis: By: Glowsy CabralMaryjoy Gabriellee De La CruzNo ratings yet
- OsteomylitisDocument28 pagesOsteomylitisHiba V.ANo ratings yet
- OSTEOMYELITISDocument4 pagesOSTEOMYELITISGanah PeterNo ratings yet
- OsteomyelitisDocument22 pagesOsteomyelitisVino GalNo ratings yet
- OSTEOMYELITISDocument3 pagesOSTEOMYELITISsweetangelNo ratings yet
- 9 - Musculoskeletal InfectionsDocument61 pages9 - Musculoskeletal InfectionsTestingAccNo ratings yet
- Pa Tho Physiology of OsteomyelitisDocument4 pagesPa Tho Physiology of OsteomyelitisninasaguidNo ratings yet
- Non-Neoplastic Bone Disease GuideDocument45 pagesNon-Neoplastic Bone Disease GuideKNo ratings yet
- Osteomylities DonDocument32 pagesOsteomylities DonNatunga RonaldNo ratings yet
- General OrthopaedicsDocument50 pagesGeneral Orthopaedicsضبيان فرحانNo ratings yet
- Osteomyelitis2 200610201550Document46 pagesOsteomyelitis2 200610201550Lolo Toto100% (1)
- Infeksi Pada Tulang Dan Sendi: Wien AryanaDocument54 pagesInfeksi Pada Tulang Dan Sendi: Wien AryanaDewa ayu NarheswariNo ratings yet
- Wound Infection & OsteomyelitisDocument33 pagesWound Infection & OsteomyelitisMoiz AzizNo ratings yet
- Reey8t.b. OsteomyelitisDocument52 pagesReey8t.b. Osteomyelitiskuku93No ratings yet
- Musculoskeleta L Infection) : Ismail BastomiDocument46 pagesMusculoskeleta L Infection) : Ismail BastomiYUFFANo ratings yet
- OsteomyelitisDocument28 pagesOsteomyelitisZelalem AbrhamNo ratings yet
- Causes, Symptoms and Treatment of Septic ArthritisDocument29 pagesCauses, Symptoms and Treatment of Septic ArthritisJauharil Wafi MuhammadNo ratings yet
- OsteomyelitisDocument93 pagesOsteomyelitisRyan KurniawanNo ratings yet
- Bone Infection, (Osteomyelitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandBone Infection, (Osteomyelitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Kritall APRASIALDocument7 pagesKritall APRASIALHaidar ShiddiqNo ratings yet
- CEBM - Diagnostic Study Appraisal WorksheetDocument3 pagesCEBM - Diagnostic Study Appraisal WorksheetWildan DzakiyNo ratings yet
- Anti Diabetes MellitusDocument21 pagesAnti Diabetes MellitusTheresia Merdeka PutriNo ratings yet
- Gallstone Disease and Acute CholecystitisDocument21 pagesGallstone Disease and Acute CholecystitisTheresia Merdeka PutriNo ratings yet
- Maternal Near MissDocument66 pagesMaternal Near MissdrmoraNo ratings yet
- Case Study: Lumbar Spondylosis L3/L4 Related With L4/L5 Spinal StenosisDocument22 pagesCase Study: Lumbar Spondylosis L3/L4 Related With L4/L5 Spinal StenosisJohanes Rully BagaskaNo ratings yet
- Triage Quick Reference Guide PDFDocument21 pagesTriage Quick Reference Guide PDFmesrianti_rubenNo ratings yet
- Chorioamnionitis by DR Simon ByonanuweDocument31 pagesChorioamnionitis by DR Simon ByonanuweDr Simon ByonanuweNo ratings yet
- Prof. Erica Wood - APEC PBMDocument46 pagesProf. Erica Wood - APEC PBMbudi darmantaNo ratings yet
- Materi Bahasa Inggris The Hospital TeamDocument4 pagesMateri Bahasa Inggris The Hospital TeamRiyadi MeighaNo ratings yet
- OSCE GuideDocument184 pagesOSCE GuideKesavaa VasuthavenNo ratings yet
- Austin Journal of Invitro FertilizationDocument5 pagesAustin Journal of Invitro FertilizationAustin Publishing GroupNo ratings yet
- Vacancies in The Department of Health: DirectorateDocument3 pagesVacancies in The Department of Health: DirectorategxjjsjejduNo ratings yet
- مزاولة مهنة - طب أسنان نوفمبر 2020Document5 pagesمزاولة مهنة - طب أسنان نوفمبر 2020وردة صبرNo ratings yet
- AO CMFS During COVID-19Document6 pagesAO CMFS During COVID-19โสภาพรรณวดี รวีวารNo ratings yet
- FKIK DikonversiDocument119 pagesFKIK DikonversiIera TajudinNo ratings yet
- NCP FormDocument3 pagesNCP FormJasmine diokNo ratings yet
- Post Dural Puncture HeadacheDocument7 pagesPost Dural Puncture Headachedrsaurav86623No ratings yet
- Leaky Gut Syndrome Symptoms, Diet, Tests & TreatmentDocument12 pagesLeaky Gut Syndrome Symptoms, Diet, Tests & TreatmentCarl MacCordNo ratings yet
- Migmar Tsering (Mike) S ResumeDocument3 pagesMigmar Tsering (Mike) S Resumeapi-284044370No ratings yet
- Pathogens: A 2021 Update On Syphilis: Taking Stock From Pathogenesis To VaccinesDocument14 pagesPathogens: A 2021 Update On Syphilis: Taking Stock From Pathogenesis To Vaccinesgupro tahiNo ratings yet
- How To Setup Biotrans ?Document21 pagesHow To Setup Biotrans ?Agoes TreeyantNo ratings yet
- Guidelines For 1st Quarter AY 2022-2023Document12 pagesGuidelines For 1st Quarter AY 2022-2023Zhen ChiNo ratings yet
- ESSAY&MCQDocument21 pagesESSAY&MCQBianca DwintaNo ratings yet
- God is Our Refuge in Times of TroubleDocument3 pagesGod is Our Refuge in Times of TroubleMarcelo piñaNo ratings yet
- DMSCO Log Book Vol.25 1947Document49 pagesDMSCO Log Book Vol.25 1947Des Moines University Archives and Rare Book RoomNo ratings yet
- Epidemiology & Health Information: NU1103 Tara Brookes @tarapb8Document40 pagesEpidemiology & Health Information: NU1103 Tara Brookes @tarapb8smartisaacNo ratings yet