Professional Documents
Culture Documents
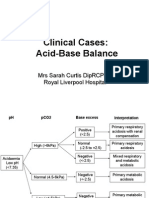
Assessment Disorders Acidbase Sarah Curtis
Uploaded by
monday125Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessment Disorders Acidbase Sarah Curtis
Uploaded by
monday125Copyright:
Available Formats
Assessment And Disorders
Of Acid-Base Balance
Mrs Sarah Curtis DipRCPath
Royal Liverpool Hospital
Aims of the lecture
Understand measurements used to
describe acid-base biochemistry
Develop a logical approach to assessment
of acid-base disorders
Apply knowledge to clinical cases
What do Blood Gas machines measure?
Derived parameters
Base excess
Standard bicarbonate
Total CO2
Anion Gap
Co-oximetry
Total Hb
O2 saturation
Oxy-Hb
CO-Hb
Met-Hb
Metabolites
Glucose
Lactate
Electrolytes
Sodium
Potassium
Chloride
Calcium
Gases
PCO2
PO2
pH
Lets take a look at the
Henderson-Hasselbalch
equation
pH = pK
a
+ Log
10
[A-]
[AH]
Where has it come from?
Panic!
Panic!
Panic!
Panic!
Panic!
Panic!
What am I supposed to do with it?
Panic!
You may previously have seen two different logs used:
Base 10 (Log
10
often just written Log)
We are only concerned with Log
10
Base e (Log
e
or Ln)
and the reverse of this, antilog, 10
x
The logarithm of 1000 to base 10 is 3
Log
10
1000 = 3
The logarithm of a number is the exponent by which another fixed
value, the base, has to be raised to produce that number.
????????
And in reverse the antilog of 3 to base 10 is 1000
Antilog 3 = 10
3
= 1000
because 1000 is 10
3
1000 = 10
3
= 101010
Enough maths, time for
some Chemistry
Acid Equilibria
Acids reversibly dissociate to release protons (H
+
)
AH
A
-
H
+
acid conjugate
base (salt)
proton
Acid Dissociation Constant
K
a
= [A
-
] x [H
+
]
[AH]
Strong acids (e.g. HCl) are more favourably dissociated: K
a
large
Weak acids (e.g. ethanol) are poorly dissociated: K
a
small
Describes the readiness with which an acid will dissociate
HCl
Cl
-
H
+
HCl Cl
-
Cl
-
Cl
-
H
+
H
+
H
+
H
+
Cl
-
EtOH
EtO
-
H
+
EtO
-
H
+
EtOH
EtOH
EtOH
EtOH
Bringing in the logarithms
We all love pH, but what does it mean?
Even for strong acids, [H
+
] is still very small
Logarithms make the numbers manageable (pre electronic calculators!)
pH = -Log
10
[H
+
]
[H+]
Blood
= 40 nmol/L
Blood pH = -Log
10
[0.00000040]
= 0.00000040 mol/L
= pH 7.0
The same trick is used for the rather less popular pK
a
pK
a
= -Log
10
[K
a
]
Deep breath
pK
a
= -Log
10
[K
a
]
Substituting for K
a
Since LogXY = LogX + LogY
pH = pK
a
+ Log
10
[A-]
[AH]
= -Log
10
[A
-
] [H
+
]
[AH]
= -Log
10
[A
-
] - Log
10
[H
+
]
[AH]
= -Log
10
[A-] + pH
[AH]
pK
a
= -Log
10
[K
a
] K
a
= [A
-
] [H
+
]
[AH]
We know:
Substituting for -Log
10
[H
+
]
Rearranging to put pH at the beginning
pH = -Log
10
[H
+
]
= -Log
10
[A
-
] x [H
+
]
[AH]
Henderson-Hasselbalch
Lets take another look at the
Henderson-Hasselbalch
equation
pH = pK
a
+ Log
10
[A
-
]
[AH]
Conjugate base (salt)
Acid
In blood there is a bicarbonate buffering system
Describes the relationship between pH and a buffering system
weak acid and its conjugate base (salt)
HCO
3
-
H
2
CO
3
+ H
+
Henderson-Hasselbalch
and the blood
pH = pK
a
+ Log
10
[HCO
3
-
]
[H
2
CO
3
]
Conjugate base (salt)
Acid
The lungs
excrete CO
2
,
increasing
the buffering
capacity
Bicarbonate buffering in
blood has a pK
a
= 6.1
H
2
O + CO
2
Carbonic
anhydrase
As H
2
CO
3
is in equilibrium with CO
2
we can replace this with PCO
2
(kPa)
multiplied by a solubility factor 0.225
HCO
3
-
H
2
CO
3
+ H
+
6.1
0.225 x PCO
2
How does this relate to laboratory
assessment of acid-base Biochemistry?
pH = 6.1 + Log
10
[HCO
3
-
]
0.225 x PCO
2
Normal blood pH = 7.35-7.45
[H
+
] > 45 nmol/L = acidaemia
[H
+
] < 35 nmol/L = alkalaemia
Normal [H
+
] = 35-45 nmol/L
What is the prevailing [H
+
]?
Measured using pH electrode on blood gas machine
pH
1
st
How does this relate to laboratory
assessment of acid-base Biochemistry?
pH = 6.1 + Log
10
[HCO
3
-
]
0.225 x PCO
2
Normal blood PCO
2
= 4.7-6.0 kPa
PCO
2
> 6.0 kPa = metabolic
PCO
2
< 4.7 kPa = respiratory
2
nd
PCO
2
> 6.0 kPa = respiratory
PCO
2
< 4.7 kPa = metabolic
Alkalosis Acidosis
Is the primary disorder metabolic or respiratory?
Measured using CO
2
electrode on blood gas machine
PCO
2
How does this relate to laboratory
assessment of acid-base Biochemistry?
pH = 6.1 + Log
10
[HCO
3
-
]
0.225 x PCO
2
Normal blood standard HCO
3
-
= 22-26 mmol/L
3
rd
Is there any compensation?
Derived by blood gas machine (Van Slyke equation) using pH, PCO
2
& Hb
Normal [HCO
3
-
]
standard
= all respiratory
Abnormal [HCO
3
-
]
standard
= metabolic component
Standard bicarbonate is one corrected for respiratory contribution (normalise PCO
2
)
a - 24.4 = - (2.3 b + 7.7) (c - 7.40) + d/(1 - 0.023 b)
a = bicarbonate concentration in plasma (mmol/L)
b = haemoglobin concentration in blood (mmol/L)
c = pH of plasma at 37 C
d = base excess concentration in blood (mmol/L)
How does this relate to laboratory
assessment of acid-base Biochemistry?
pH = 6.1 + Log
10
[HCO
3
-
]
0.225 x PCO
2
Normal Total CO
2
(bicarbonate) = 22-33 mmol/L
Measured enzymatically or derived by gas machine from Henderson-Hasselbalch
Total CO
2
is approximation of bicarbonate = HCO
3
-
+ CO
2
+ H
2
CO
3
+ CO
3
-
TCO
2
= Metabolic acidosis / Respiratory alkalosis
TCO
2
= Metabolic alkalosis / Respiratory acidosis
Base Excess
CO
2
cannot be buffered by bicarbonate
Respiratory
alkalosis
relative base deficit
HPr
Pr
- H
+
Pr
-
HPr
H
+
Equilibration of CO
2
requires non-bicarbonate buffers
relative base excess
H
2
O + CO
2
Carbonic
anhydrase
HCO
3
-
H
2
CO
3
+ H
+
/ negative base excess
Derived by blood gas machine using pH, PCO
2
& Hb
Amount of strong acid/alkali needed to titrate whole blood to pH 7.4 at normal PCO
2
BE = (HCO
3
-
- 24.4 + [2.3 Hb + 7.7] [pH - 7.4]) (1 - 0.023 Hb)
Respiratory
acidosis
Anion Gap
Unmeasured Anions
Proteins
-Hydroxybutyrate
Acetoacetate
Lactate
Sulphates
Phosphates
Formate
Glycolate
Oxalate
Hippurate
Salicylate
Unmeasured Cations
Calcium
Magnesium
(Lithium)
(Cationic Igs)
Difference between sum of measured anions and cations
Anion gap = [Na
+
] + [K
+
] [Cl
-
] [HCO
3
-
]
Normal individuals have excess measured cations, hence anion gap
Increased
anion gap in
metabolic
acidosis
(HCO
3
-
)
Absent gap is rare phenomenon
Increased unmeasured cations
Hypoalbuminaemia
Bromide toxicity (spurious Cl
-
)
Nitrates
(Osmolar gap indicates uncharged species)
Disorders of Hydrogen Ion
Homeostasis
Metabolic Acidosis
pH [H+] PCO
2
HCO
3
-
PO
2
N /
Metabolic Acidosis - Causes
Increased Acid Formation
Ketoacidosis: diabetic, alcoholic, starvation
Lactic acidosis
Type A: tissue hypoxia
Type B: drugs, liver disease, IEMs
D-lactic acidosis
Poisoning: salicyate, alcohols
Inherited organic acidoses
Decreased Acid Excretion
Uraemia
Distal renal tubular acidosis (1/4)
Acid Ingestion
Strong acid
Ammonium chloride
I.V. feeding with cationic amino acids
Loss Of Base
Gastrointestinal: diarrhoea, fistula
Renal
Proximal renal tubular acidosis (2)
Acetazolamide
Ureteroenterostomy
Which of these increase the anion gap?
Metabolic Acidosis Response
Buffering
Acute H
+
resisted by bicarbonate buffering causing HCO
3
-
Tissue proteins and bone important in chronic acidosis
Respiratory Compensation
Peripheral chemoreceptors and respiratory centre stimulated hyperventiliation
Self-limiting as generates additional CO
2
lower limit for PCO
2
is 1.6 kPa
Develops rapidly but several hours to become maximal
Renal Compensation
Urine H+ excretion maximised (pH 4.2)
Glutaminase induced in chronic acidosis
Increased renal gluconeogenesis
Increased rate of regeneration of bicarbonate
Glutamine Glutamate
NH
3
H
2
O
Systemic Effects Of Acidosis
Cardiovascular
Negative inotropic effect
Arteriolar vasodilaton
Constriction of peripheral veins
Oxygen Delivery
Immediate right shift (Bohr) in oxyHb dissociation curve
Slow left shift in oxyHb dissociation curve (synthesis breakdown 2,3-BPG)
Potassium
K
+
movement from ICF to ECF causing hyperkalaemia
Decreased renal excretion
Frequently K-depleted; hypokalaemia common with correction
Bone
Decalcification with negative calcium balance
Osteodystrophy
Metabolic Acidosis - Management
Identify and treat cause
Administration of i.v. sodium bicarbonate (alkali)
Usually only given if [H
+
] > 100 nmol/L (pH 7.0)
Oral bicarbonate
CKD, RTA types 1 & 2
Rapid correction impairs O
2
delivery (until 2,3-BPG normal)
Rebound alkalosis possible
Respiratory Acidosis
pH [H+] PaCO
2
HCO
3
-
N /
Respiratory Acidosis - Causes
Defective Control Of Respiration
CNS depression
Anaesthetics
Narcotics
Severe hypoxia
CNS disease
Trauma
Stroke
Neurological disease
Spinal cord lesions
Poliomyelitis
Guillan-Barre syndrome
Motor neurone disease
Neurotoxins
Defective Respiratory Function
Mechanical
Myasthenic syndrome
Myopathies
Thoracic tumours and deformities
Pneumothorax
Pleural effusion
Airway disease
Restrictive defects
Fibrosis
Pulmonary oedema
Infiltrative tumours
Obstructive defects
Chronic bronchitis
Emphysema
Severe asthma
Laryngospasm
Impaired perfusion
Massive pulmonary embolism
Respiratory Acidosis Response
Buffering
Limited buffering by haemoglobin
Intracellular buffers important in chronic acidosis
Respiratory Compensation
PCO
2
stimulates respiratory centre but disease prevents adequate response
Renal Compensation
Maximal bicarbonate reabsorption
Almost all phosphate excreted as H
2
PO
4
-
Marked increase in urinary ammonium
Respiratory Acidosis Systemic Effects
Hypoxaemia:
Breathlessness, cyanosis, drowsiness
Hypercapnia:
Neurological, headache, papilloedema, extensor plantar responses, myoclonus
Effects of acidosis (as for metabolic)
Respiratory Acidosis Management
Treat underlying cause if possible
Maintain adequate arterial PO
2
, avoid loss of hypoxic stimulus to respiration
Avoid rapid correction as risk of alkalosis due to persistence of compensation
Metabolic Alkalosis
pH [H+] PaCO
2
HCO
3
-
K
+
N /
(not > 8kPa)
Metabolic Alkalosis - Causes
Saline-Responsive
Gastrointestinal
Vomiting
Gastric drainage
Congenital Cl-losing diarrhoea
Exogenous alkali administration
Sodium bicarbonate
Lactate
Acetate (especially if GFR)
Urinary
Poorly reabsorpable anion therapy
Diuretic administration post PCO
2
Saline-Unresponsive
Association with hypertension
Primary hyperaldosteronism
Secondary hyperaldosteronism
Not usually associated with HT
Barters syndrome
Refeeding syndrome
Severe potassium depletion
Magnesium deficiency
Excessive loss / increased generation of H
+
, exogenous alkali
Metabolic Alkalosis Response
Buffering
Release of buffered H
+
, with HCO
3
-
Respiratory Compensation
Decreased stimulation of chemoreceptors but self-limiting as PCO
2
stimulates
Hypoxic stimulus also overrides H
+
Renal Compensation
Inappropriate reabsorption of HCO
3
-
due to GFR and increased tubular function
If ECF volume associated with Cl
-
deficiency, obligatory HCO
3
-
reabsorption
Potassium deficiency contributes to persistence of alkalosis
Increased mineralocorticoid activity promotes distal tubular Na
+
Metabolic Alkalosis Systemic Effects
Generally opposite to those of acidosis
Less pronounced CV effects, poor O
2
delivery, no apparent bone effects
Potassium depletion, which sustains alkalosis
Neuromuscular hyperexcitability: parasthesia, muscle cramps, tetany, convulsions
( Binding of H
+
to albumin increases Ca
2+
binding, lowering ionised calcium)
Metabolic Alkalosis Management
Treat underlying cause
Treat factors that sustain alkalosis
Do not give saline if saline-unresponsive cause
(e.g. sodium excess)
Respiratory Alkalosis
pH [H+] PaCO
2
HCO
3
-
K
+
Phos
N /
Respiratory Alkalosis - Causes
Rate of excretion of CO
2
exceeds rate of production
Voluntary hyperventiliation
Mechanical hyperventilation
Reflex hyperventilation
Pulmonary compliance
Disease affecting chest wall
Irritative lesions of the air passages
Respiratory stimulation
Cortical influences : pain, fever, anxiety
Local disease: trauma, tumours
Toxins: salicylate, hepatic failure
Hypoxaemia: high altitude, right-to-left shunts, pulmonary disease, CO
Recovery from metabolic acidosis
Respiratory Alkalosis Response
Buffering
Release of H
+
from non-bicarbonate buffers
New steady state achieved within 6 hours
Respiratory Compensation
Inhibitory effect of PCO
2
overwhelmed by primary cause
Renal Compensation
Decreased renal generation of bicarbonate (CO
2
is substrate)
Respiratory Alkalosis Systemic Effects
Manifestations of underlying disease predominate
Acute hypocapnia decreases cerebral blood flow
Ionised calcium: perioral and peripheral parasthesia
Cardiovascular: increased heart rate, tightening of chest, angina
Mild hypokalaemia
Marked hypophosphataemia
Respiratory Alkalosis Management
Treat underlying cause
Rapid symptomatic relief by re-breathing
Sedation or prevention of hyperventilation
by mechanical hyperventilation
Mixed Acid-Base Disorders
Mixed primary disorders are quite common if you look for them
Some examples of double disorders triple etc. also occur!
Metabolic Acidosis Metabolic Alkalosis
Respiratory Acidosis Respiratory failure
Cardiac arrest
Ethanol
Methanol
Diuretics + COPD
Vomiting + COPD
Severe K
+
depletion
Respiratory Alkalosis Salicylate
Septicaemia
Fulminant hepatic failure
Ketoacidosis + pneumonia
Vomiting + CCF
Diuretics + pneumonia
Metabolic Alkalosis Vomiting + renal failure
Diuretics + DKA
Severe vomiting in ketoacidosis
Counterbalancing Additive
Conclusions
Henderson-Hasselbalch is our friend!
Respiratory disorders are compensated by
metabolic processes
Metabolic disorders are compensated by
respiratory processes
Over-compensation does not occur
You might also like
- AbgDocument52 pagesAbgm07wwpNo ratings yet
- How To Read Arterial Blood Gas .PTDocument36 pagesHow To Read Arterial Blood Gas .PTMohd Erham bin JonohNo ratings yet
- Acid Base Balance PSN LHRDocument63 pagesAcid Base Balance PSN LHRPooran Kumar100% (2)
- Review Article: Sodium Bicarbonate Therapy in Patients With Metabolic AcidosisDocument14 pagesReview Article: Sodium Bicarbonate Therapy in Patients With Metabolic AcidosisMuhammad Arif Nur SyahidNo ratings yet
- Regulation of Acid-Base Balance: ElizabethDocument35 pagesRegulation of Acid-Base Balance: ElizabethGeorge LusanaNo ratings yet
- Complement: Kathleen Basa Kris Nicole de Guzman Jessica Mae Ong 3HmtDocument70 pagesComplement: Kathleen Basa Kris Nicole de Guzman Jessica Mae Ong 3HmtCherry Reyes-Principe100% (1)
- Concentration of Urine: Maj DR Shavana R.L RanaDocument22 pagesConcentration of Urine: Maj DR Shavana R.L RanaChandan Sah100% (1)
- Alawlaqi - Obesity FinalDocument26 pagesAlawlaqi - Obesity FinalMotea Alawlaqi100% (1)
- Acid-Base Disorders NotesDocument10 pagesAcid-Base Disorders NotesLovely100% (1)
- Acid-Base MSC CasesDocument16 pagesAcid-Base MSC Casesmonday125No ratings yet
- Acid-Base BalanceDocument28 pagesAcid-Base Balanceps4only100% (1)
- Hormonal Control of Calcium and Phosphate MetabolismDocument50 pagesHormonal Control of Calcium and Phosphate MetabolismhamidNo ratings yet
- Acid Base HomeostasisDocument11 pagesAcid Base HomeostasisOrion JohnNo ratings yet
- Arterialbloodgasanalysis ppt-2Document43 pagesArterialbloodgasanalysis ppt-2Kresna Dharma SuryanaNo ratings yet
- DR Cole Storage Disorders Hand OutDocument3 pagesDR Cole Storage Disorders Hand Outmonday125No ratings yet
- Chemical Pathology II HIV AIDSDocument33 pagesChemical Pathology II HIV AIDSSimeon AdebisiNo ratings yet
- Acid Base DisordersDocument5 pagesAcid Base DisordersjohnshenryNo ratings yet
- Acid Base TutorialDocument47 pagesAcid Base TutorialDiah Puspita Rini100% (2)
- DR Moat Paediatric BochemistryDocument62 pagesDR Moat Paediatric Bochemistrymonday125No ratings yet
- Assessment of Metabolic AcidosisDocument34 pagesAssessment of Metabolic Acidosisfatha100% (1)
- Basic Immunology: Ratna Windyaningrum Supervisor: Dr. Arif Dermawan, M.Kes., Sp. T.H.T.K.L (K)Document42 pagesBasic Immunology: Ratna Windyaningrum Supervisor: Dr. Arif Dermawan, M.Kes., Sp. T.H.T.K.L (K)Ratna Windyaningrum100% (1)
- Physiology Acid QuizDocument5 pagesPhysiology Acid QuizRavi AminNo ratings yet
- Acid Base Disorders JAPIDocument5 pagesAcid Base Disorders JAPIVitrag_Shah_1067No ratings yet
- Biochemical Tests in Diabetes: DR Joe Fleming PHD MCB Frcpath Dept of Clinical Biochemistry CMC VelloreDocument43 pagesBiochemical Tests in Diabetes: DR Joe Fleming PHD MCB Frcpath Dept of Clinical Biochemistry CMC Velloremariya khanNo ratings yet
- COMPILED SCTL Adrenal Disorders PDFDocument14 pagesCOMPILED SCTL Adrenal Disorders PDFeeelie35No ratings yet
- Renal Regulation of Acid-Base BalanceDocument10 pagesRenal Regulation of Acid-Base BalanceMarianela Vásquez ArayaNo ratings yet
- Pratley New Treatments For Type 2 DiabetesDocument85 pagesPratley New Treatments For Type 2 DiabetesMia DangaNo ratings yet
- Routine and Acute Clinical ChemistryDocument2 pagesRoutine and Acute Clinical ChemistryMohamed MounirNo ratings yet
- Arterial Blood Gases - UpToDateDocument20 pagesArterial Blood Gases - UpToDateGuillermo MárquezNo ratings yet
- Asthma (For RACP Exams)Document18 pagesAsthma (For RACP Exams)Sam HuntNo ratings yet
- Bleeding Disorders: LCDR Art GeorgeDocument54 pagesBleeding Disorders: LCDR Art Georgesatya_mdsNo ratings yet
- Arterial Blood GasDocument55 pagesArterial Blood GasRathis Dasan100% (1)
- Autoimmunity PDFDocument73 pagesAutoimmunity PDFErum JanNo ratings yet
- Chronic Leukemia: Rahmawati Minhajat A. Fachruddin BenyaminDocument24 pagesChronic Leukemia: Rahmawati Minhajat A. Fachruddin BenyaminMJ Putra100% (1)
- Simulation StationDocument2 pagesSimulation Stationmonday125No ratings yet
- Beta BlockersDocument70 pagesBeta BlockersIrina Cabac-PogoreviciNo ratings yet
- Decision Algorithm For Prescribing SGLT2 Inhibitors and GLP-1 Receptor AgonistsDocument11 pagesDecision Algorithm For Prescribing SGLT2 Inhibitors and GLP-1 Receptor AgonistsNati BocciaNo ratings yet
- Lab 9++10 Pathological UrinlysisDocument38 pagesLab 9++10 Pathological UrinlysisSai SreedharNo ratings yet
- Plasma Enzyme DiagnosisDocument30 pagesPlasma Enzyme DiagnosisKayode IbitoyeNo ratings yet
- Acid Base ImbalanceDocument50 pagesAcid Base ImbalanceDian Pratiwi BurnamaNo ratings yet
- 2 Acid-Base ImbalanceDocument9 pages2 Acid-Base ImbalanceKhuzema SaeedNo ratings yet
- Introduction To Acid Base Metabolic AcidosisDocument12 pagesIntroduction To Acid Base Metabolic AcidosisKris Sharine Batalla OderoNo ratings yet
- FOCUS SAS Training Day Leeds Dr. Joanna Sheldon Protein Reference Unit, St. George'sDocument19 pagesFOCUS SAS Training Day Leeds Dr. Joanna Sheldon Protein Reference Unit, St. George'smonday125No ratings yet
- Hypernatremia From HarrisonDocument3 pagesHypernatremia From HarrisonNobel LaureateNo ratings yet
- Heat Coagulation TestDocument8 pagesHeat Coagulation TestRawan MaherNo ratings yet
- Renal Physiology For The BoardsDocument37 pagesRenal Physiology For The BoardsRainy Day100% (1)
- Chemical Pathology UnitDocument22 pagesChemical Pathology UnitLee Yann Na IbrahimNo ratings yet
- Acid Base DisordersDocument11 pagesAcid Base DisordersS100% (1)
- Introduction To Endocrinology For Clinical StudentsDocument28 pagesIntroduction To Endocrinology For Clinical StudentsOhwovoriole ToketemuNo ratings yet
- Renal PathologyDocument28 pagesRenal PathologyApril Deveras JudillaNo ratings yet
- Innate & Adaptive Immunity (DR - Soraya Rezeki, MKT)Document30 pagesInnate & Adaptive Immunity (DR - Soraya Rezeki, MKT)Dyah Wahlia100% (1)
- Chemical Pathology Job Description December 2011Document9 pagesChemical Pathology Job Description December 2011Chengyuan ZhangNo ratings yet
- Acid-Base Disorder CasesDocument40 pagesAcid-Base Disorder CaseslrostomeNo ratings yet
- Approach To The Child With Metabolic Acidosis - UDocument3 pagesApproach To The Child With Metabolic Acidosis - URishi Shrestha100% (1)
- 2 Renal PhysiologyDocument56 pages2 Renal PhysiologyNoraine Princess TabangcoraNo ratings yet
- Hemoglobin Structure & SynthesisDocument24 pagesHemoglobin Structure & SynthesisIMDCBiochemNo ratings yet
- Caffeine BronchodilatorDocument30 pagesCaffeine Bronchodilatormonday125No ratings yet
- Clinical Guideline For Anticoagulant Use in AdultsDocument108 pagesClinical Guideline For Anticoagulant Use in Adultsmonday125No ratings yet
- ADMA 2010 BlackboardDocument41 pagesADMA 2010 Blackboardmonday125No ratings yet
- Karen Smith Duty Biochemist ScenariosDocument43 pagesKaren Smith Duty Biochemist Scenariosmonday125100% (2)
- Pleasing Her Husband's Boss (Hot Wife and Her Cuckold 2) by Michaels DeanaDocument29 pagesPleasing Her Husband's Boss (Hot Wife and Her Cuckold 2) by Michaels Deanamonday12560% (10)
- Bible 2018Document183 pagesBible 2018monday125No ratings yet
- 2010 - Zhang - EAP For AR Review PDFDocument8 pages2010 - Zhang - EAP For AR Review PDFmonday125No ratings yet
- FRCPath OSPE 25042014Document11 pagesFRCPath OSPE 25042014monday125No ratings yet
- ST Agnes Catholic Primary SchoolDocument12 pagesST Agnes Catholic Primary Schoolmonday125No ratings yet
- Uric AcidDocument6 pagesUric Acidmonday125100% (1)
- ICP-MS Talk ACBDocument31 pagesICP-MS Talk ACBmonday125No ratings yet
- OspeDocument29 pagesOspemonday125No ratings yet
- Frances Boa Methodology QuestionDocument39 pagesFrances Boa Methodology Questionmonday125No ratings yet
- FRCPath Chemical Pathology CurriculumDocument109 pagesFRCPath Chemical Pathology Curriculummonday125No ratings yet
- FOCUS SAS Training Day Leeds Dr. Joanna Sheldon Protein Reference Unit, St. George'sDocument19 pagesFOCUS SAS Training Day Leeds Dr. Joanna Sheldon Protein Reference Unit, St. George'smonday125No ratings yet
- Critical Appraisal: DR A C J Hutchesson Chair of Examiners' Panel, Frcpath (Clinical Biochemistry)Document10 pagesCritical Appraisal: DR A C J Hutchesson Chair of Examiners' Panel, Frcpath (Clinical Biochemistry)monday125No ratings yet
- Writing An Abstract: Sally - Benton@bartshealth - Nhs.ukDocument7 pagesWriting An Abstract: Sally - Benton@bartshealth - Nhs.ukmonday125No ratings yet
- Model Albumin AnswerDocument13 pagesModel Albumin Answermonday125No ratings yet
- FRCPath Cases 1Document36 pagesFRCPath Cases 1monday125100% (1)
- Bill Bartlett - 1 1 1Document68 pagesBill Bartlett - 1 1 1monday125No ratings yet
- Master Sheet: 1. Irregular ClotDocument20 pagesMaster Sheet: 1. Irregular Clotmonday125No ratings yet
- Module 3, Lecture 3 FOCDocument9 pagesModule 3, Lecture 3 FOCSanmukh KaurNo ratings yet
- Rules, Scripts and BeanshellDocument7 pagesRules, Scripts and BeanshelltgudyktzxNo ratings yet
- 50TPD Soybean Oil Batch Type Solvent Extraction PlantDocument4 pages50TPD Soybean Oil Batch Type Solvent Extraction PlantKenan KardasNo ratings yet
- Magnetism: Teacher Notes and Answers 19 MagnetismDocument3 pagesMagnetism: Teacher Notes and Answers 19 Magnetismmahsan abbas100% (1)
- Consumer Surplus:: at K Chabveka Economics NotesDocument28 pagesConsumer Surplus:: at K Chabveka Economics NotesShawn DzingayiNo ratings yet
- UK Assemblies PDFDocument284 pagesUK Assemblies PDFFernando Borges ChachaNo ratings yet
- Syllabus 3210 Fall 2012 PDFDocument4 pagesSyllabus 3210 Fall 2012 PDFRahul KarnaNo ratings yet
- Regcm 4.3 Training Session Ii Regcm4.3-Rc OutputDocument8 pagesRegcm 4.3 Training Session Ii Regcm4.3-Rc OutputShane Marie VisagaNo ratings yet
- EC303Document19 pagesEC303api-3853441No ratings yet
- 13 Years BITSAT Past PapersDocument304 pages13 Years BITSAT Past PapersEdu VsatNo ratings yet
- Chapter 1 - Distillation PDFDocument107 pagesChapter 1 - Distillation PDFFatin Natasha NazriNo ratings yet
- Electronic Devices & Practice: InstructorDocument23 pagesElectronic Devices & Practice: Instructorjavaid musaNo ratings yet
- Reflection and ShearDocument7 pagesReflection and ShearsamNo ratings yet
- Mechanical Damage and Fatigue Assessment of Dented Pipelines Using FeaDocument10 pagesMechanical Damage and Fatigue Assessment of Dented Pipelines Using FeaVitor lopesNo ratings yet
- How Can Dust Make Planets More Suitable For Life?: Authors: Associate EditorDocument4 pagesHow Can Dust Make Planets More Suitable For Life?: Authors: Associate EditorLucien GbezeNo ratings yet
- PU225 Series: Solenoid ValveDocument1 pagePU225 Series: Solenoid Valveremus popescuNo ratings yet
- Economics Solution Book PDFDocument368 pagesEconomics Solution Book PDFgoutam1235100% (3)
- Esam AliDocument23 pagesEsam AliYoussef AliNo ratings yet
- Dr. Rife and Philip Hoyland's 3.3 MHZ SweepDocument2 pagesDr. Rife and Philip Hoyland's 3.3 MHZ SweepKhalid Ibrahim100% (1)
- Tapchanger Dual Assessment Raka Levi31102011 PDFDocument12 pagesTapchanger Dual Assessment Raka Levi31102011 PDFYuri OmonteNo ratings yet
- Just in Time AlgebraDocument289 pagesJust in Time AlgebraamaiscNo ratings yet
- Chemistry Note Form 5Document9 pagesChemistry Note Form 5SofiyyahOpieNo ratings yet
- State-Of-The-Art of Battery State-Of-Charge DeterminationDocument19 pagesState-Of-The-Art of Battery State-Of-Charge Determinationyasvanthkumar sNo ratings yet
- Panasonic MINAS A5Document478 pagesPanasonic MINAS A5Vaikuntam Ramamurthy100% (1)
- TP 3017D Taman Angkasa Nuri - V01Document25 pagesTP 3017D Taman Angkasa Nuri - V01Najwa AzmanNo ratings yet
- From-To Chart ExampleDocument22 pagesFrom-To Chart Exampleajeng.saraswatiNo ratings yet
- Understanding The Relationship Between Human Behavior and Susceptibility To Cyber AttacksDocument25 pagesUnderstanding The Relationship Between Human Behavior and Susceptibility To Cyber AttacksVelibor SabanNo ratings yet
- Astm B695-04-2009Document6 pagesAstm B695-04-2009Danny TriwibowoNo ratings yet
- An Empirical Study On The Nexus Between The Emotional Intelligence of Top Managers and Their Assessment of Intellectual CapitalDocument30 pagesAn Empirical Study On The Nexus Between The Emotional Intelligence of Top Managers and Their Assessment of Intellectual Capitalmaher76No ratings yet
- Shaw, Milton C. Metal Cutting PrinciplesDocument759 pagesShaw, Milton C. Metal Cutting PrinciplesJuan Sebastian Quinche Velandia75% (4)