Professional Documents
Culture Documents
Introduction To Indonesian Code of Ethics
Uploaded by
Lady KweeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Introduction To Indonesian Code of Ethics
Uploaded by
Lady KweeCopyright:
Available Formats
Introduction to
Code of Ethics
An Interactive Lecture
Leonardi A Goenawan
What do you know about Ethics?
The Science of Human Duty
A particular system of principles & rules
concerning duty, whether true or false
Rules of practice in respect to a single
class of human actions; as, political or
social ethics; medical ethics.
According to Philosophy 1
Ethics is a major branch of philosophy,
encompassing right conduct and good life.
It is significantly broader than the
common conception of analyzing right and
wrong. A central aspect of ethics is "the
good life", the life worth living or life that
is simply satisfying, which is held by many
philosophers to be more important than
moral conduct
According to Philosophy 2
Ethics is the formal study of moral standards
and conduct. For this reason, the study of ethics
is also often called "moral philosophy."
What is good? What is evil?
How should I behave - and why?
How should I balance my needs against the needs of
others?
These are some of the questions asked in the field of
ethics, a branch of philosophy which has some of the
most immediate and obvious consequences for how
we live our lives.
Moral or Ethics ?
Ethic:
A set of moral principles;
a theory or system of moral values;
The principles of conduct governing an individual or
a group;
A guiding philosophy;
A consciousness of moral importance;
A set of moral issues or aspects (as rightness);
Ethics is usually regarded as more universal in nature.
People from all cultures share the same ethics. It
contains the idea of distinguishing what is right from
wrong, and striving to do what is right.
Moral or Ethics ?
Moral:
Relating to principles of right and wrong in behavior;
Expressing or teaching a conception of right behavior;
Conforming to a standard of right behavior;
Capable of right and wrong action;
Morality may be more local in nature, more culture
specific.
There are many cultural practices which are moral or
immoral depending where they are practiced.
Why medical ethics is important?
Physicians deal with saving humans life.
Patients want dedicated physicians they
can trust.
Physicians want to feel good about
themselves and what they do.
THE MEDICAL ECOSYSTEM
- Enlarging Circle of Influence
DOCTOR PATIENT
Disease Diagnosis Health Promotion
Disease Prevention Therapy
Medical Insurance
Managed Care
Hospital
Laboratories
Pharmaceutical
Industry
Patients Family,
Culture, Religion
Patients Work, Employer
Other Doctors
Paramedics
Clinic
Management
Public Health
Medical
Research
Medical
Students
CME,
CPD
Doctors
Employer
Doctors
Family
Doctors
Employee
Practice
Management
MDO
Medical Council
The LAW
Government
Bodies
Medical
Charities
Patient
Organisation
Alternative
Medicine
Press, Media
National Community
International Community
Natural Disasters
Political
Upheaval, War
THE PRINCIPLES IN MEDICAL
ETHICS
The Principle of Non-Maleficence
The Principle of Beneficence
The Principle of Autonomy
The Principle of Veracity
The Principle of Confidentiality (or
Fidelity)
The Principle of Social Responsibility and
Justice
The Principle of Non-
Maleficence
First do no harm
Sanctity of life
Calculated risk or risk benefit
The Principle of Beneficence
Do only that which benefits the patient
Patients welfare as the first consideration
Care consideration competence
The obligation to provide and accept
beneficial treatment
The Principle of Autonomy
Right to information and self
determination
Free and informed consent
Free will and accord - intentional
participation in treatment
Respect and dignity maintained
The right of an individual to choose
between various alternatives presented to
them
The Principle of Veracity
Truth telling
Obligation to full and honest disclosure
The Principle of Confidentiality
Based on loyalty and trust
Maintain the confidentiality of all personal,
medical and treatment information
Information to be revealed with consent and
for the benefit of the patient
Except when ethically and legally required
Disclosure should not be beyond what is
required
The Principle of Justice and
Social Responsibility
Actions are consistent, accountable and
transparent
Not to discriminate on age, sex, religion,
race, position or rank
Greater good of society
Respect of the Law
Equity and distribution of burden &
benefits
Principle of Double-Effect
The act itself must be morally good or at least
indifferent.
The agent may not positively will the bad effect
but may merely permit it. If he could attain the
good effect without the bad effect, he should do
so. The bad effect is sometimes said to be
indirectly voluntary.
The good effectmust be produced directly by
the action, not by the bad effect. Otherwise, the
agent would be using a bad means to a good
end, which is never allowed.
Principle of Double-Effect
The good effect must be sufficiently desirable to
compensate for the allowing of the bad effect. In
forming this decision many factors must be weighed and
compared, with care and prudence proportionate to the
importance of the case. Thus, an effect that benefits or
harms society generally has more weight than one that
affects only an individual; an effect sure to occur
deserves greater consideration than one that is only
probable; an effect of a moral nature has greater
importance than one that deals only with material things
St Thomas Acquinas. New Catholic Encyclopedia, vol 4, 1967 (internet edition).
What is an Ethical Dilemma?
A conflict between moral imperatives, i.e., what
is the right thing to do?
What is medically right vs. patient preference
Jehovahs Witnesses and transfusions
What is preferred by patient vs. proxy decision maker
Rights of minor vs. legal guardians
What is best for patient vs. what is best for society
Commitment laws, notification of sexual partners of patients
with HIV
How to Analyze an Ethics Case
What is being proposed?
What are the medical issues?
Risks, benefits, alternatives
Case and statutory law
Who are the stakeholders?
Patient, family, medical staff, hospital, state
Cultural and religious concerns
Are possible consultants to medical, legal, and ethical issues
When does this need to be done?
Emergency exceptions to informed consent
Why is an ethical dilemma being created?
Conflicts between decision makers, law and ethics
How can this be resolved?
Meeting(s), consultation(s)
Withdrawing vs. Withholding Care
Withdrawing care
Decision to remove an active intervention
that is already being provided to a patient
Withholding care
Decision not to provide an active
intervention to a patient
Withdrawing vs. Withholding Care
In medical ethics today, there is no distinction made
between withdrawing and withholding care.
In the past, withholding was considered ethically
superior to withdrawing.
Most recently, ethicist are espousing the position
that withdrawing is ethically superior to withholding,
since a trial of treatment gives information on its
efficacy for the particular patient.
You might also like
- Assignment-Legal and Ethical Issues in PicuDocument20 pagesAssignment-Legal and Ethical Issues in PicushahnazNo ratings yet
- Edical ThicsDocument81 pagesEdical ThicsDivyanshi KomalNo ratings yet
- 1 - Ethical IssuesDocument33 pages1 - Ethical IssuesDaniyal Azmat100% (1)
- 1 - Introduction To EthicsDocument70 pages1 - Introduction To EthicsMohammed HussienNo ratings yet
- Legal and Ethical Issues in Pediatric NursingDocument18 pagesLegal and Ethical Issues in Pediatric NursingTanvi0% (1)
- Legal and Ethical Issues in Pediatric NursingDocument18 pagesLegal and Ethical Issues in Pediatric NursingTanvi100% (4)
- Legeal & EthicalDocument6 pagesLegeal & EthicalNaro LemtorNo ratings yet
- Kaidah Dasar Bioetika & Prima FacieDocument60 pagesKaidah Dasar Bioetika & Prima FacieSamdiSutantoNo ratings yet
- Theories and Principles of Health Ethics: Vincent Z. Solidum, MAN, RNDocument33 pagesTheories and Principles of Health Ethics: Vincent Z. Solidum, MAN, RNJmarie Brillantes Popioco100% (1)
- CLinical Ethics and ProfessionalismDocument38 pagesCLinical Ethics and ProfessionalismBerhanuNo ratings yet
- Ethical Legal Issues Related To Gerontological Care HCDocument41 pagesEthical Legal Issues Related To Gerontological Care HCtamika sealyNo ratings yet
- Medical Ethics LDocument28 pagesMedical Ethics Lalmastar officeNo ratings yet
- Professional Practice in Physical TherapyDocument19 pagesProfessional Practice in Physical TherapyRizwan BashirNo ratings yet
- Nursing EthicsDocument8 pagesNursing EthicsJam AicaNo ratings yet
- Ethical Principles in Community Health NursingDocument24 pagesEthical Principles in Community Health Nursingjansanmathew33% (3)
- Health Care Ethics GuideDocument14 pagesHealth Care Ethics GuideJaz Dawn Hernandez SorianoNo ratings yet
- Kuliah Bioetik FK UnjaDocument33 pagesKuliah Bioetik FK UnjaTitia RahmaniaNo ratings yet
- KD BN Prima Facie 2013Document60 pagesKD BN Prima Facie 2013Aldo HamkaNo ratings yet
- 1.01. Bioethical PrinciplesDocument26 pages1.01. Bioethical PrinciplesAbi Tabares100% (1)
- Intro To Ethics Presentation-Brig. Maqsood 15-09-2021Document37 pagesIntro To Ethics Presentation-Brig. Maqsood 15-09-2021gdrive.r859abNo ratings yet
- Week 5 - PHI100Document30 pagesWeek 5 - PHI100jerome rarogalNo ratings yet
- Ethical TheoriesDocument35 pagesEthical TheoriesJenross De LeonNo ratings yet
- Etika Profesi Dan Hukum Kesehatan: Fikri Mourly WahyudiDocument23 pagesEtika Profesi Dan Hukum Kesehatan: Fikri Mourly WahyudiArya MuhammadNo ratings yet
- Chapter 7 Nursing EthicsDocument66 pagesChapter 7 Nursing EthicsMikee PaningbatanNo ratings yet
- NCM108 Module 1-CDocument9 pagesNCM108 Module 1-Cmirai desuNo ratings yet
- Medical Ethics-1Document50 pagesMedical Ethics-1Princewill SeiyefaNo ratings yet
- What Is Bioethics?: Key Ethical Concerns in Bioethics Often Involve Big Questions Such AsDocument10 pagesWhat Is Bioethics?: Key Ethical Concerns in Bioethics Often Involve Big Questions Such AsJonas AncianoNo ratings yet
- An Introduction To Medical Ethics: Dr. Philip S.L. Beh Email: Philipbeh@pathology - Hku.hkDocument43 pagesAn Introduction To Medical Ethics: Dr. Philip S.L. Beh Email: Philipbeh@pathology - Hku.hksatyachakrabortyNo ratings yet
- BioethicsDocument32 pagesBioethicsJireh RiveraNo ratings yet
- Activity 2Document8 pagesActivity 2Myhen Grace QuebecNo ratings yet
- Definition of Terms EthicsDocument18 pagesDefinition of Terms EthicsEliezer NuenayNo ratings yet
- Definition of Terms EthicsDocument18 pagesDefinition of Terms EthicsEliezer NuenayNo ratings yet
- 9Document40 pages9PRINCIPAL ALSNo ratings yet
- Beginning BioethicsDocument79 pagesBeginning BioethicsGilbert IskandarNo ratings yet
- Medical Ethics: Basic PrinciplesDocument18 pagesMedical Ethics: Basic PrinciplesAli KhalidNo ratings yet
- The Four Bioethical PrinciplesDocument4 pagesThe Four Bioethical Principlesariansofia1031No ratings yet
- Part Four - L&MDocument18 pagesPart Four - L&MJrBong SemaneroNo ratings yet
- Intro BioethicsDocument19 pagesIntro Bioethicsaubrey justimbasteNo ratings yet
- Most Important Medical Ethics PillarDocument2 pagesMost Important Medical Ethics PillarHariniNo ratings yet
- Values of NursingDocument27 pagesValues of NursingJay-l Escuadra82% (22)
- Bioethics: Moral Philosophy and BioethicsDocument7 pagesBioethics: Moral Philosophy and BioethicsJes Cmt100% (1)
- NCM 119 Juris - Nursing EthicsDocument57 pagesNCM 119 Juris - Nursing Ethicsinno so qtNo ratings yet
- Basic Nursing Ethics: Foundations of ResponsibilitiesDocument24 pagesBasic Nursing Ethics: Foundations of ResponsibilitiesAndrea TylerNo ratings yet
- Ethical Dimension of Nursing Practice WordDocument6 pagesEthical Dimension of Nursing Practice Wordpink096No ratings yet
- Nursing EthicsDocument6 pagesNursing EthicsAliza Bea CastroNo ratings yet
- Group 2 HandoutsDocument22 pagesGroup 2 Handoutsyutanakamotoyuta29No ratings yet
- Yasir Mehmood - 29 (Phil-201)Document12 pagesYasir Mehmood - 29 (Phil-201)Yasir MehmoodNo ratings yet
- 1 - NUM1205 - An Introduction To Law and Ethics - SVDocument41 pages1 - NUM1205 - An Introduction To Law and Ethics - SVLuis Martin PunayNo ratings yet
- Grp. 3 Moral Principle and Professional EthicsDocument47 pagesGrp. 3 Moral Principle and Professional EthicsjiangNo ratings yet
- Notes in NCM 108 Health Care EthicsDocument5 pagesNotes in NCM 108 Health Care EthicsJazel May G. RicoNo ratings yet
- 1 ST SessionDocument71 pages1 ST SessionAbdelrahman SelimaNo ratings yet
- Fiel Angelo G. Mallari, RNDocument68 pagesFiel Angelo G. Mallari, RNfiel mallariNo ratings yet
- Ethical GovernanceDocument4 pagesEthical GovernanceStee Al-FradianteeNo ratings yet
- Bioethics ReportDocument25 pagesBioethics ReportReyna Rodelas100% (1)
- Bioethical PrinciplesDocument48 pagesBioethical PrinciplesAnonymous yINtpcNo ratings yet
- Medical Ethics and Case Studies Part1Document12 pagesMedical Ethics and Case Studies Part1denver cayagaNo ratings yet
- Hippocratic OathDocument5 pagesHippocratic OathMohamed ShalanNo ratings yet
- Case of The WeekDocument20 pagesCase of The WeekLady KweeNo ratings yet
- Why School Health Programs Are ImportantDocument18 pagesWhy School Health Programs Are ImportantLady Kwee100% (3)
- Contin Educ Anaesth Crit Care Pain-2011-Stotz-193Document1 pageContin Educ Anaesth Crit Care Pain-2011-Stotz-193Lady KweeNo ratings yet
- Brain Death in ImagingDocument3 pagesBrain Death in ImagingLady KweeNo ratings yet
- Digestion: Rondang R. SoegiantoDocument21 pagesDigestion: Rondang R. SoegiantoLady KweeNo ratings yet
- Moral Dev.L Kolberg - EnglishDocument10 pagesMoral Dev.L Kolberg - EnglishLady KweeNo ratings yet
- Patient PresentationsDocument7 pagesPatient PresentationsLady KweeNo ratings yet
- STUDENT PORTFOLIO FOR MEDICINE DEPARTMENTDocument2 pagesSTUDENT PORTFOLIO FOR MEDICINE DEPARTMENTLady KweeNo ratings yet
- Family Portrait by Camio Pictures 2013Document12 pagesFamily Portrait by Camio Pictures 2013Lady KweeNo ratings yet
- Stress Management LAGDocument41 pagesStress Management LAGLady KweeNo ratings yet
- Family Portrait by Camio Pictures 2013Document12 pagesFamily Portrait by Camio Pictures 2013Lady KweeNo ratings yet
- CT features that predict outcomes after head injuryDocument5 pagesCT features that predict outcomes after head injuryLady KweeNo ratings yet
- Hyperosmolar HyperglycemicDocument8 pagesHyperosmolar HyperglycemicCésar Augusto Sánchez SolisNo ratings yet
- BB GastrointestinalDocument43 pagesBB GastrointestinalLady KweeNo ratings yet
- HT Autoimmune DiseasesDocument2 pagesHT Autoimmune DiseasesJoshua ObrienNo ratings yet
- Physical Examination of Cardiovascular: DR - Ira Andaningsih SPJP Cardiovascular Block 2008Document89 pagesPhysical Examination of Cardiovascular: DR - Ira Andaningsih SPJP Cardiovascular Block 2008YeniNo ratings yet
- Oncogene AEG 1 Promotes Glioma Induced Neurodegeneration by Increasing Glutamate ExcitotoxicityDocument11 pagesOncogene AEG 1 Promotes Glioma Induced Neurodegeneration by Increasing Glutamate ExcitotoxicityLady KweeNo ratings yet
- Quality of Life in Adults With Brain Tumors Current Knowledge and Future DirectionsDocument10 pagesQuality of Life in Adults With Brain Tumors Current Knowledge and Future DirectionsLady KweeNo ratings yet
- Clinical Features of Primary Brain Tumours UDocument5 pagesClinical Features of Primary Brain Tumours ULady KweeNo ratings yet
- MindMapper 2009 Help GuideDocument146 pagesMindMapper 2009 Help GuideLady KweeNo ratings yet
- Dengue Guidelines WHO 2011Document78 pagesDengue Guidelines WHO 2011Yhoga Timur LagaNo ratings yet
- Oncogene AEG 1 Promotes Glioma Induced Neurodegeneration by Increasing Glutamate ExcitotoxicityDocument11 pagesOncogene AEG 1 Promotes Glioma Induced Neurodegeneration by Increasing Glutamate ExcitotoxicityLady KweeNo ratings yet
- Facilitating Learning Teaching - Learning MethodsDocument55 pagesFacilitating Learning Teaching - Learning MethodsIeda RahmanNo ratings yet
- Facilitating Learning Teaching - Learning MethodsDocument55 pagesFacilitating Learning Teaching - Learning MethodsIeda RahmanNo ratings yet
- Problem BasedDocument3 pagesProblem BasedLady KweeNo ratings yet
- Vaughn and Baker - Teaching MethodsDocument10 pagesVaughn and Baker - Teaching MethodsLady KweeNo ratings yet
- Oncogene AEG 1 Promotes Glioma Induced Neurodegeneration by Increasing Glutamate ExcitotoxicityDocument11 pagesOncogene AEG 1 Promotes Glioma Induced Neurodegeneration by Increasing Glutamate ExcitotoxicityLady KweeNo ratings yet
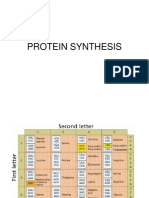
- Protein Synthesis3Document11 pagesProtein Synthesis3Lady KweeNo ratings yet
- Brain Tumor Edema Neuroscience ReviewDocument10 pagesBrain Tumor Edema Neuroscience ReviewLady KweeNo ratings yet
- Environmental Ethics-NewDocument15 pagesEnvironmental Ethics-NewGayathri Devi100% (1)
- Ethics CorruptionDocument18 pagesEthics CorruptionJaneNo ratings yet
- Aristotle's Virtue EthicsDocument12 pagesAristotle's Virtue EthicsasdasdasdasdNo ratings yet
- Business EthicsDocument21 pagesBusiness EthicsMuhd Fasyraf100% (1)
- Ethics in Law EnforcementDocument145 pagesEthics in Law EnforcementbobNo ratings yet
- Informative Speech OutlineDocument2 pagesInformative Speech Outlineapi-264979431100% (1)
- Topics To Be Covered: Ethics and Morality Relates To "Right" and "Wrong" Conduct. While They AreDocument3 pagesTopics To Be Covered: Ethics and Morality Relates To "Right" and "Wrong" Conduct. While They AreKshitij NegiNo ratings yet
- Sociology Lesson - Deviance and CrimeDocument20 pagesSociology Lesson - Deviance and Crimerey portilloNo ratings yet
- Lect# 2 Moral Vs Non Moral StandarsDocument6 pagesLect# 2 Moral Vs Non Moral Standarsaminurrahman33367% (6)
- Moral Criticism Also Known As Christian Humanism Is A School of Thought That Focuses On Judging and Evaluating TheDocument2 pagesMoral Criticism Also Known As Christian Humanism Is A School of Thought That Focuses On Judging and Evaluating TheChippy MagalonaNo ratings yet
- Morale Development: "Ethics in Engineering" Says, "Ethics Is Also Used To Refer To The Particular Set of BeliefsDocument11 pagesMorale Development: "Ethics in Engineering" Says, "Ethics Is Also Used To Refer To The Particular Set of Beliefssiva7448163No ratings yet
- Brief Summary EthicsDocument22 pagesBrief Summary EthicsHeart AbagNo ratings yet
- Business Ethics Fundamentals MGT 3800 Chapter 6Document15 pagesBusiness Ethics Fundamentals MGT 3800 Chapter 6ramstexNo ratings yet
- Ethical Theories and Approaches PDFDocument2 pagesEthical Theories and Approaches PDFShannon100% (1)
- Ethics Week1 14 QuizzesNo MidtermPrelimFinalsDocument7 pagesEthics Week1 14 QuizzesNo MidtermPrelimFinalsGrezhel Mae Alonte100% (6)
- HippocratesDocument11 pagesHippocratesEdward BabitzkeNo ratings yet
- TOK EthicsDocument3 pagesTOK EthicsSerena Nikita CoulsonNo ratings yet
- Indian Ethos and ManagementDocument131 pagesIndian Ethos and ManagementdollyguptaNo ratings yet
- The Natural Law TheoryDocument2 pagesThe Natural Law TheoryLuke VelasquezNo ratings yet
- Sexual MoralityDocument2 pagesSexual MoralityFlorina AndreiNo ratings yet
- Lecture Note-Aristotle and Natural Law TheoryDocument6 pagesLecture Note-Aristotle and Natural Law TheoryRam Kumar YadavNo ratings yet
- Things Go Bump in The Night Case StudyDocument5 pagesThings Go Bump in The Night Case StudyShelton D'mello100% (1)
- 04-801 HOMEWORK 1 Name: NIZEYIMANA Jean Paul Andrew ID: Jnizeyim Course: Entrepreneurship For Emerging MarketsDocument2 pages04-801 HOMEWORK 1 Name: NIZEYIMANA Jean Paul Andrew ID: Jnizeyim Course: Entrepreneurship For Emerging MarketsyohanizeNo ratings yet
- ETHICSDocument83 pagesETHICSMa. Aira AntalanNo ratings yet
- Dialectical EthicsDocument2 pagesDialectical EthicsLizette100% (1)
- Concept of Ethics and MoralityDocument46 pagesConcept of Ethics and MoralityNeha VermaNo ratings yet
- Kohlbergs Stages of Moral DevelopmentDocument20 pagesKohlbergs Stages of Moral DevelopmentArunita Padhi SarangiNo ratings yet
- Group 1Document2 pagesGroup 1John Fernand RacelisNo ratings yet
- Bullying ProjectDocument9 pagesBullying Projectapi-458879520No ratings yet
- Ethical Decision Making PDFDocument3 pagesEthical Decision Making PDFabhi7840No ratings yet