Professional Documents
Culture Documents
CH 40
Uploaded by
Mehabooba Mehataf0 ratings0% found this document useful (0 votes)
27 views39 pagesch
Original Title
ch40
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentch
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
27 views39 pagesCH 40
Uploaded by
Mehabooba Mehatafch
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 39
Chapter 40
Legal I ssues, Quality Assurance,
and I nfection Control in Dental
Radiography
Copyright 2003, Elsevier Science (USA).
All rights reserved. No part of this product may be reproduced or transmitted in any
form or by any means, electronic or mechanical, including input into or storage in any
information system, without permission in writing from the publisher.
PowerPoint
presentation slides may be displayed and may be reproduced in print
form for instructional purposes only, provided a proper copyright notice appears on
the last page of each print-out.
Produced in the United States of America
ISBN 0-7216-9770-4
Copyright 2003, Elsevier Science (USA). All rights reserved.
I ntroduction
The dental assistant must be aware of the legal
responsibilities involved in taking dental radiographs.
There are both federal and state regulations that control
the use of dental x-ray equipment.
To ensure the highest quality and minimal risk to
patients in radiation exposure, a quality assurance
program is necessary.
Dental radiography procedures are not usually
considered high risk for the transmission of diseases.
However, infectious diseases present a significant
hazard in the dental office and dental professionals are
at an increased risk for acquiring such diseases.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Legal I ssues
There are three major categories of legal
considerations with which the dental assistant
should be familiar regarding the use of x-rays in
dentistry:
Federal and state regulations regarding x-ray
equipment and its use.
Licensure for individuals exposing radiographs.
Risk management for avoiding potential
lawsuits.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Federal and State Regulations
The use of dental x-ray equipment is regulated by both
federal and state regulations.
All dental x-ray machines manufactured or sold in the
United States after 1974 must meet federal regulations
which include safety specifications for minimum filtration
and accuracy of the milliamperage time and kilovoltage
settings.
Many states require x-ray machines to be registered and
charge a fee for this registration.
Most states have laws that require inspections of dental x-
ray equipment on a regular basis, for instance, every 5
years.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Licensure Requirements
The Consumer-Patient Radiation Health and Safety Act
is a federal law that requires persons who take dental
radiographs to be properly trained and certified.
It is up to the individual state to determine its own
policy regarding qualification of individuals exposing
radiographs.
X-ray certification requirements for the dental assistant
will vary from state to state.
Some states require DANB certification; other states
may require an additional examination.
Each state deals with dental radiography differently.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Risk Management
Risk management policies are designed to reduce the
likelihood of a malpractice lawsuit against the dentist.
The dental assistant has an important role in risk
management.
The dental assistant must be careful never to say
anything negative about the x-ray equipment or how it
is working.
Statements made without thinking, such as the timer
must be off, this thing never works right, or the
solutions are weak, are unnecessary and can make
the patient feel uncomfortable.
Statements made by anyone at the time of an alleged
negligent act are admissible as evidence in court.
Copyright 2003, Elsevier Science (USA). All rights reserved.
I nformed Consent
It is the dentists responsibility to discuss the need
for radiographs and treatment procedures with the
patient.
The dental assistant may participate in the process
of obtaining informed consent.
Patients must give their informed consent for
dental radiographs, as well as for other
procedures.
Copyright 2003, Elsevier Science (USA). All rights reserved.
For Valid I nformed Consent
The patient must be provided with the following
information in lay terms:
The risks and benefits of the radiographs.
The person who will be exposing the
radiographs.
The number and type of radiographs.
The consequences of not having the
radiographs.
Any alternative diagnostic aids that may
provide the same information as the
radiographs.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Liability
Under state laws, the supervising dentist is legally
responsible, or liable, for the actions of the dental
auxiliary.
This is called respondeat superior doctrine. It
means that the employer is responsible for the
actions of the employee.
However, even though dental assistants work
under the supervision of a licensed dentist, they
can also be held legally liable for their own actions.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Patient Records
It is very important to document the exposure of
dental radiographs.
The number of films exposed, as well as the quality
of the radiographs, may be an important issue in a
malpractice suit.
Radiographs that are of poor quality and are
nondiagnostic reflect against the dentist.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Documentation of Dental Radiographs
The dental record must include the following
information:
Informed consent.
The number and type of radiographs exposed.
The rationale for exposing the radiographs.
The diagnostic interpretation.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Ownership of Dental Radiographs
Radiographs are the property of the dentist, even
though the patient, or the patients insurance
company, paid for them.
This is because dental radiographs are a part of
the patients records.
Patients have a right to reasonable access of their
records.
Make an entry in the chart stating when and to
whom the duplicate radiographs were sent.
NEVER give or send the original radiographs to a
patient.
Copyright 2003, Elsevier Science (USA). All rights reserved.
When Patients Refuse Dental Radiographs
When this occurs, the dentist must decide whether an
accurate diagnosis can be made without radiographs
and whether treatment can be provided.
The use of dental radiographs is now the accepted
standard of care.
No document can be signed to release the dentist from
liability. Even if the patient suggests signing a release
or waiver that will release the dentist from liability, it
would be considered invalid if an injury did result.
It should be recorded in the patients record if a
patient refuses recommended radiographs.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Patient Education
As a dental assistant, you should understand and be
sensitive to the patients concern and fears about
exposure to radiation during dental radiographs.
The dental assistant is often the person that the
patient feels most comfortable with in confiding these
fears.
The dental assistant can explain to the patient just
how important radiographs are in detecting diseases
and planning treatment.
Patients can be informed of the federal and state laws
enacted for their protection.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Quality Assurance in the Dental Office
Quality assurance is a way of assuring that
everything possible is being done to produce high-
quality diagnostic radiographs.
It includes both quality control tests that
monitor dental x-ray equipment, supplies, and film
processing.
It also includes quality administration
procedures that include records of maintenance
and record-keeping logs.
Copyright 2003, Elsevier Science (USA). All rights reserved.
I nfection Control in Dental Radiography
Dental radiography presents unique infection
control problems because of the potential for
operator contamination and cross contamination to
other patients and to other members of the dental
team.
Constant movement by the operator from the oral
cavity to the exposure controls outside the
operatory to the darkroom and finally to film
mounting increases the risk of exposing others to
infectious diseases.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Radiography Operatory Preparation
The first step in preparation of the operatory is to
determine the surfaces to be covered or
disinfected with a high-level surface disinfectant.
In general, surfaces that cannot be easily cleaned
and disinfected should be protected by a barrier-
most commonly plastic or foil barriers.
Surface barriers are preferred to be on electrical
switches because of the possibility of the cleaner
and disinfectant causing an electrical short.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 40-4 Radiography operatory with barriers in place.
Fig. 40-4
Copyright 2003, Elsevier Science (USA). All rights reserved.
X-Ray Machine
The tubehead, position-indicating device (PID),
control panel, and exposure button must all be
covered or carefully disinfected.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 40-5 X-ray equipment with barriers in place.
Fig. 40-5
Copyright 2003, Elsevier Science (USA). All rights reserved.
Lead Apron
The lead apron should be considered
contaminated and wiped with a disinfectant
after each use.
Copyright 2003, Elsevier Science (USA). All rights reserved.
The Dental Chair
The back and arms of the chair, the headrest, and
the headrest adjustment controls must all be
covered or disinfected.
Once the radiography operatory is set up, the film
and film-holding devices should be prepared.
Copyright 2003, Elsevier Science (USA). All rights reserved.
The Work Area
The work area where the x-ray film and film-
holding devices are placed during exposure should
be disinfected and then a barrier should be placed.
This can be a paper sheet, paper towels, or plastic
cover.
Once the procedure is completed, the barriers
should be discarded. Surfaces not protected by
barriers should be cleaned and disinfected.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig 40-6 A, A plastic surface barrier is placed. B, After each exposure, the dental
assistant wipes the film dry using a paper towel and then places the exposed film into
a plastic bag that has been taped to the wall.
Fig. 40-6
Copyright 2003, Elsevier Science (USA). All rights reserved.
Preparation of Supplies and Equipment
Before beginning the procedure, gather all the
supplies that you might need to decrease the
chance of cross-contamination.
For example, think about the type of film-holding
devices, cotton rolls, and bitewing tabs that may
be needed if the patient has an edentulous area.
If you need some additional supplies during the
procedure, either use overgloves (food handlers
gloves) or ask someone for assistance.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Film
Dental film should be dispensed from a central area in a
disposable container, such as a paper cup or an envelope.
To minimize contamination by saliva, a clear plastic barrier
envelope may be placed over the film packet.
Films that are enclosed in a clear plastic barrier packet are
available commercially.
The barrier-protected film packets are exposed and brought
to the processing area.
The barriers are contaminated and must be removed very
carefully without touching the inner packet so the packet
can be handled with bare hands.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 40-7 Protective barrier on x-ray film.
Fig. 40-7
Copyright 2003, Elsevier Science (USA). All rights reserved.
Contaminated Film Packets
The contaminated film packet is the major source
of cross-contamination during radiographic
procedures.
When the packet is removed from the patients
mouth, it is coated with saliva (or, on occasion,
contaminated with blood).
For this reason, the operator must always wear
gloves while handling contaminated film packets.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Decontamination of Film Packets
Wipe saliva from the film packet using a dry 2 x 2
inch gauze sponge or a paper towel.
Do not attempt to sterilize the film packet. Heat
sterilization will destroy the image.
Some film manufacturers permit light spraying of
the film packets with a disinfectant spray;
however, immersion of the packet in a disinfecting
solution can result in the solution seeping into the
emulsion and damaging the image.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Film-Holding Devices
Film-holding instruments and bite-blocks that are
placed in the patients mouth are semicritical items
and must be sterilized or high-level disinfected
before reuse.
The alternative is to use disposable film holders
and discard them after a single use.
Sterilized film-holding devices should remain
packaged until the patient is seated and the
patient can view the opening of the package.
Patients appreciate knowing that proper infection
control procedures are in place throughout the
office.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Miscellaneous I tems
Other miscellaneous items include cotton rolls that
can be used to stabilize film placement and paper
towels that can be used to wipe saliva from
exposed films.
A disposable container, such as a paper cup
labeled with the patients name, is also necessary
to collect the exposed films.
All miscellaneous items should be dispensed from a
central supply area.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Gloves and protective clothing must be worn while
exposing radiographs and handling the
contaminated films.
Because radiographic procedures do not involve
the aerosol produced by the dental handpiece, a
mask and glasses are optional while radiographic
films are being made.
Preparation of the Operator
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 40-8 While wearing the appropriate personal protection, the operator
places the lead apron on the patient.
Fig. 40-8
Copyright 2003, Elsevier Science (USA). All rights reserved.
I nfection Control During Exposure
After gloving, the operator should be careful not to
touch any surfaces that are not covered.
The best way to do this is to develop a sequence in
which the operator touches as few surfaces as
possible.
After each exposed film is removed from the
patients mouth, it must be wiped with a paper
towel to remove excess saliva.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Collection of Contaminated Films
Once dried, each film must be placed in a disposable
container (plastic bag or paper cup) that is labeled with
the patients name.
This container will be used to transport the films to the
darkroom.
The outside surface of this container must not be
touched by gloved hands.
To prevent film fog caused by radiation, the container
should never be placed in a room where additional
films are being exposed.
Exposed films should never be placed in the operators
laboratory or uniform pocket.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Film-Holding Devices
During exposure, film-holding devices should be
transferred from the covered work area to the
patients mouth and then back to the same area.
Contaminated instruments should never be placed
on an uncovered surface.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Management of Contaminated I tems
After Exposure
After completion of film exposure, all contaminated
items must be discarded, and any uncovered surfaces
must be disinfected.
Contaminated radiography items must be handled in
the same manner as recommended for other
contaminated dental instruments.
Contaminated items must be discarded while wearing
gloves; this includes the disposable surface coverings.
The operator should carefully unwrap all covered
surfaces; the actual surfaces that are wrapped should
not be touched by gloved hands.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Film-holding devices
While the operator is wearing gloves, the contaminated
film-holder must be removed from the treatment area
and placed in the area designated for contaminated
instruments.
Handwashing
After the removal and disposal of all contaminated
items, the gloves must be removed and the hands
washed.
Surface disinfection
Any uncovered areas that were contaminated during
exposure must be cleaned and disinfected using an EPA-
registered hospital-grade disinfectant and utility gloves.
Management of Contaminated I tems
After Exposure- contd
Copyright 2003, Elsevier Science (USA). All rights reserved.
Film Transport
The disposable container should never be touched
by gloved hands.
Only after the gloves have been removed, the
hands have been washed and dried, the patient
has been dismissed, and the area has been
cleaned and disinfected should the operator carry
the disposable container holding the contaminated
films to the darkroom.
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Clinico-Pathological Conference: Presented by The Department of Internal MedicineDocument3 pagesClinico-Pathological Conference: Presented by The Department of Internal MedicineCloudy ClaudNo ratings yet
- Physical Education Essential Learning Out Comes and Learning TargetsDocument8 pagesPhysical Education Essential Learning Out Comes and Learning TargetsJessa May RapadasNo ratings yet
- Module 7. Presented - The Phil Health Program On Degenerative Diseases 93Document105 pagesModule 7. Presented - The Phil Health Program On Degenerative Diseases 93Roma ClaireNo ratings yet
- Zotc 116 Exer 3Document2 pagesZotc 116 Exer 3Leighna Ricci CruzNo ratings yet
- Docet CPD Resources - Competencies and Cet PointsDocument1 pageDocet CPD Resources - Competencies and Cet PointsWEDHNo ratings yet
- BA 89402175 001100 Innopack EN 00 PDFDocument293 pagesBA 89402175 001100 Innopack EN 00 PDFBruno GiffoniNo ratings yet
- Deborah Falla The Role of Motor Learning and Neuroplasticity in Designing RehabilitationDocument5 pagesDeborah Falla The Role of Motor Learning and Neuroplasticity in Designing RehabilitationDago Angel Prieto PalavecinoNo ratings yet
- Reflection PaperDocument7 pagesReflection Paperapi-623973327No ratings yet
- Ccws Candida Cell Wall Suppressor Treatment Protocol A5 4ppDocument4 pagesCcws Candida Cell Wall Suppressor Treatment Protocol A5 4ppcandida cell wall suppressor ccwsNo ratings yet
- Disaster Readiness Risk Reduction: Quarter 2-Module 13: DRR-related Laws and PoliciesDocument16 pagesDisaster Readiness Risk Reduction: Quarter 2-Module 13: DRR-related Laws and PoliciesUel Cabz LaquihonNo ratings yet
- How To Sleep BetterDocument9 pagesHow To Sleep BetterMariaNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaameliaaarrNo ratings yet
- Steps To Reduce Drug Abuse 1800 11 0031 National Toll Free Drug de Addiction Helpline NumberDocument4 pagesSteps To Reduce Drug Abuse 1800 11 0031 National Toll Free Drug de Addiction Helpline NumberimranNo ratings yet
- SOP-016-Testing of LPG ResidueDocument9 pagesSOP-016-Testing of LPG ResidueAmnaKamranNo ratings yet
- Colgate Marketing ReportDocument16 pagesColgate Marketing ReportRaja GuruNo ratings yet
- Budget Equity ToolDocument22 pagesBudget Equity ToolEd PraetorianNo ratings yet
- Enucleation Surgery-Orbital Implants and Surgical Techniques - 1Document3 pagesEnucleation Surgery-Orbital Implants and Surgical Techniques - 1Satria Adi MarhendraNo ratings yet
- Climbing Training Log - TemplateDocument19 pagesClimbing Training Log - TemplateKam Iqar ZeNo ratings yet
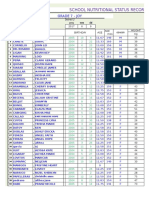
- School Nutritional Status Record: Grade 7 - JoyDocument4 pagesSchool Nutritional Status Record: Grade 7 - JoySidNo ratings yet
- DLL - Mapeh 6 - Q4 - W6Document4 pagesDLL - Mapeh 6 - Q4 - W6Bernard Martin100% (1)
- Matter For PGDIPC Course PromotionDocument1 pageMatter For PGDIPC Course PromotionAnkur VasudevaNo ratings yet
- Stages of LaborDocument3 pagesStages of Laborkatzuhmee leeNo ratings yet
- What Is ISO 22000 S. 2005?: An OverviewDocument23 pagesWhat Is ISO 22000 S. 2005?: An OverviewMario Norman B. CelerianNo ratings yet
- Stacey Waters CVDocument5 pagesStacey Waters CVapi-479651018No ratings yet
- Diet's CardDocument8 pagesDiet's CardJORGE ATRIANONo ratings yet
- Fluid Overload and Kidney Injury Score As A PredicDocument7 pagesFluid Overload and Kidney Injury Score As A Predicmira srikandiNo ratings yet
- Jonathan Glover-Alien LandscapesDocument448 pagesJonathan Glover-Alien LandscapesIrina Soare100% (1)
- Ayurveda y Psicoterapia PDFDocument6 pagesAyurveda y Psicoterapia PDFsastalNo ratings yet
- Psychiatric Disability AssessmentDocument19 pagesPsychiatric Disability AssessmentDivya ThomasNo ratings yet
- RLE Module 3F Course Module and Procedure Guide 2Document7 pagesRLE Module 3F Course Module and Procedure Guide 2KaiNo ratings yet