Professional Documents
Culture Documents
Shock 4813
Uploaded by
docprash0 ratings0% found this document useful (0 votes)
15 views18 pagesDefinition of Shock A clinical syndrome that occurs when acute circulatory failure with inadequate or inappropriately distributed tissue perfusion results in failure to meet metabolic demands. Hypovolemic - Reduction in circulating blood volume - Hemorrhage, plasma loss (burns / ascites), or extracellular fluid loss (ketoacidosis / trauma) cardiogenic - severe heart failure (MI, acute mitral regurgitation) obstructive - circulatory obstruction (embolism
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDefinition of Shock A clinical syndrome that occurs when acute circulatory failure with inadequate or inappropriately distributed tissue perfusion results in failure to meet metabolic demands. Hypovolemic - Reduction in circulating blood volume - Hemorrhage, plasma loss (burns / ascites), or extracellular fluid loss (ketoacidosis / trauma) cardiogenic - severe heart failure (MI, acute mitral regurgitation) obstructive - circulatory obstruction (embolism
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
15 views18 pagesShock 4813
Uploaded by
docprashDefinition of Shock A clinical syndrome that occurs when acute circulatory failure with inadequate or inappropriately distributed tissue perfusion results in failure to meet metabolic demands. Hypovolemic - Reduction in circulating blood volume - Hemorrhage, plasma loss (burns / ascites), or extracellular fluid loss (ketoacidosis / trauma) cardiogenic - severe heart failure (MI, acute mitral regurgitation) obstructive - circulatory obstruction (embolism
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 18
Definition of Shock
A clinical syndrome that occurs when acute
circulatory failure with inadequate or
inappropriately distributed tissue perfusion
results in failure to meet metabolic demands
causing generalized cellular hypoxia with or
without lactic acidosis
Categories of Shock
Hypovolemic
Reduction in circulating blood volume
Hemorrhage, plasma loss (burns/ascites), or extracellular fluid loss
(ketoacidosis/trauma)
Cardiogenic
Severe heart failure (MI, acute mitral regurgitation)
Obstructive
Circulatory obstruction (embolism/tamponade)
Septic
Infection or septicemia
Vasodilation, arteriovenous shunting and capillary damage cause
hypotension and maldistribution of blood flow
Categories of Shock, cont
Anaphylactic
Due to allergen-induced vaosdilation
Bee sting, peanut allergy, food allergies
Neurogenic
Follows high spinal trauma (above T6)
Interrupts sympathetic outflow causing
vasodilation, hypothermia, and bradycardia which
can be severe if vagal (parasympathetic)
stimulation is unopposed
Clinical Features
Depend on the underlying cause of the shock
and the severity
General features
Hypotension (systolic <100)
Tachycardia (>100)
Tachypnea (>30)
Oliguria (<30 ml/hr)
Drowsiness/confusion/agitation
Clinical Features, cont
Cold, clammy shock
Hypovolemic, cardiogenic, obstructive, and late shock
Cold peripheries from skin vasoconstriction, weak pulses,
evidence of low CO (oliguria, cyanosis, confusion)
Warm, dilated shock
Early septic and anaphylactic
Warm peripheries from skin vasodilation, bounding pulses,
high CO, flushed skin
Pathophysiology
Infection, trauma, allergens, hypoxia activate
endothelial cells and white cells releasing
interleukins and tumor necrosis factor
This results in an inflammatory response and a
thrombolytic response
The coagulation cascade is started and fibrin clots
form
The capillary is now inflamed and occluded
This damages the organ the capillary is in and
reduces oxygen delivery to that organ, furthering the
damage
Investigations
Labs: routine blood tests (eg-CBC), ABGs, lactic
acid levels, cardiac enzymes, blood type/cross
match
Vital signs: temperature, RR, SaO2, UO
Hemodynamics: continuous BP, CVP, EKGmay
also need CO, SVR, PCWP, SvO2 depending on
severity
Radiology: CXR
Microbiology: blood, sputum, and urine cultures
Assessment
Clinical features, SVR, and CVP define the cause of shock
CVP
CVP is reduced
Hypovolemic or anaphylactic
CVP is high
Cardiogenic or obstructive
CVP can be low, normal, or high with septic shock
SVR
SVR is high
Cardiogenic with vasoconstriction (cold, clammy shock)
SVR is low
Septic with vasodilation (warm, dilated shock)
Assessment, cont
Hypovolemic Shock
Low CVP/PCWP + low CO + high SVR
Cardiogenic Shock
High CVP/PCWP + low CO + high SVR
Septic Shock
Low CVP/PCWP + high CO + low SVR
Complications
Circulatory failure with tissue hypoxia leads
to multi-organ failure including ARDS, SIRS,
acute renal failure, GI ulceration
Eventually refractory shock with irreversible
tissue damage occurs leading to death
Multi-organ Failure
Brain: coma, intracerebral bleed
Lungs: ARDS
Heart: MI
Liver: failure
Kidneys: failure
GI: mucosal damage
Blood vessels: DIC, hemorrhagic purpura, bleeding
at injection and line insertion sites
Skin/extremities: ischemia, gangrene
Management
Mortality increases if shock lasts more than
an hour (the golden hour)
Try to correct the underlying cause of the
shock, reverse the tissue oxygen debt, and
prevent organ damage
Management, cont
Identify and treat the cause of the shock
Correct hypoxemia
Use supplemental oxygen
Intubate and ventilate (obtunded patients have a
high risk of aspiration)
Ventilatory support reduces the WOB, improves
cardiac function, and increases tissue oxygen
delivery
Management, cont
Resuscitation
Fluid resuscitation
Hypovolemia with low CVP/PCWP requires fluid
replacement
Cardiogenic shock with high CVP/PCWP needs fluid
restriction
At the onset of septic shock, fluid replacment is essential
but later fluid restriction may be needed to avoid
pulmonary edema
Management, cont
Inotropic support
Indicated when hypotension (MAP <60) or tissue
hypoxemia persist despite adequate fluid replacement or
when fluid is contraindicated
Type of inotrope depends on the cause of the shock
With warm shock, the CO is high but vasodilation may
cause hypotension, inadequate tissue perfusion, and organ
hypoxianorepinephrine increases SVR restoring the BP
and tissue perfusion
With cold shock, the CO is low due to poor myocardial
contractility and SVR is high from sympathetic
vasoconstrictiondobutamine increases contractility and
reduces SVR
Management, cont
Correct acidosis
Remove circulatory obstructions
Thrombolysis for pulmonary emboli (TPA,
Streptokinase)
Drainage of cardiac tamponade/pneumothorax
Correction of DIC to prevent microcirculatory
obstruction
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Inflammation GrayscaleDocument132 pagesInflammation GrayscaledocprashNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- USMLE Step 1 Board Exam High Yield Anatomy For MedicineDocument7 pagesUSMLE Step 1 Board Exam High Yield Anatomy For Medicinesirp328100% (2)
- USMLE World NotesDocument50 pagesUSMLE World NotesScott Buchowski50% (4)
- Integumentary Diseases and PathologyDocument16 pagesIntegumentary Diseases and PathologydocprashNo ratings yet
- Hallmark Findings: Medical PG Entrance Made Easy©Document6 pagesHallmark Findings: Medical PG Entrance Made Easy©docprashNo ratings yet
- Fmge Important TopicsDocument33 pagesFmge Important Topicsdocprash100% (1)
- Thrombo EmbolismDocument45 pagesThrombo EmbolismdocprashNo ratings yet
- Laboratory 1221572191937440 9Document144 pagesLaboratory 1221572191937440 9docprashNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Basics 110329114833 Phpapp02Document383 pagesBasics 110329114833 Phpapp02docprashNo ratings yet
- The Bourne Identity (DVDrip) (Dual Audio) (Eng-Hindi)Document4 pagesThe Bourne Identity (DVDrip) (Dual Audio) (Eng-Hindi)docprashNo ratings yet
- USMLE Step 1 Board Exam High Yield Anatomy For MedicineDocument7 pagesUSMLE Step 1 Board Exam High Yield Anatomy For Medicinesirp328100% (2)
- Hallmark Findings: Medical PG Entrance Made Easy©Document6 pagesHallmark Findings: Medical PG Entrance Made Easy©docprashNo ratings yet
- Environmental, Congenital, and Iatrogenic Syndrome GuideDocument4 pagesEnvironmental, Congenital, and Iatrogenic Syndrome GuideFranspolNo ratings yet
- Path SecretDocument6 pagesPath SecretdocprashNo ratings yet
- Table of Genetic DisordersDocument14 pagesTable of Genetic DisordersdocprashNo ratings yet
- Mnemonics in Emergency MedDocument9 pagesMnemonics in Emergency MeddocprashNo ratings yet
- Some Key Points PathologyDocument4 pagesSome Key Points PathologydocprashNo ratings yet
- Most Common CausesDocument8 pagesMost Common CausesdocprashNo ratings yet
- Table of Genetic DisordersDocument3 pagesTable of Genetic DisordersdocprashNo ratings yet
- DocDocument30 pagesDocdocprashNo ratings yet
- Fmge 2012Document2 pagesFmge 2012docprashNo ratings yet
- Msuacidbaseimbalancemedicine 120707105320 Phpapp02Document55 pagesMsuacidbaseimbalancemedicine 120707105320 Phpapp02docprashNo ratings yet
- Fmge 2012Document1 pageFmge 2012docprashNo ratings yet
- USMLE World NotesDocument11 pagesUSMLE World NotesdocprashNo ratings yet
- Path SecretDocument6 pagesPath SecretdocprashNo ratings yet
- PathologyDocument2 pagesPathologydocprashNo ratings yet
- Usmle Step 1 NotesDocument5 pagesUsmle Step 1 NotesdocprashNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- HANDOUTS Brain SurgeryDocument3 pagesHANDOUTS Brain SurgerynieltresNo ratings yet
- Butamirate CitrateDocument2 pagesButamirate CitratenisircNo ratings yet
- PE1 ReviewerDocument4 pagesPE1 ReviewerZoe BeatrizNo ratings yet
- Acute Myeloid LeukemiaDocument1 pageAcute Myeloid LeukemiaAlleah Salbo KepusNo ratings yet
- Head Injury and concussion-ENDocument5 pagesHead Injury and concussion-ENJasly SafeerNo ratings yet
- Graduate SOAP NOTE TEMPLATEDocument7 pagesGraduate SOAP NOTE TEMPLATEMiley MunozNo ratings yet
- Protect Yourself From Needlestick InjuriesDocument2 pagesProtect Yourself From Needlestick InjuriesBidang Mutu & Akreditasi RS Hermina BogorNo ratings yet
- About This Leaflet: FibroadenomaDocument2 pagesAbout This Leaflet: FibroadenomaEnvhy WinaNo ratings yet
- Guideline Karsinoma HepatoselulerDocument11 pagesGuideline Karsinoma HepatoselulerMohammad Ihsan RifasantoNo ratings yet
- Grave's Ophthalmopathy: Susy Fatmariyanti Delfitri Lutfi, Hendrian D. SoebagjoDocument12 pagesGrave's Ophthalmopathy: Susy Fatmariyanti Delfitri Lutfi, Hendrian D. SoebagjoriskhapangestikaNo ratings yet
- Obg MCQSDocument11 pagesObg MCQSShriyansh ChaharNo ratings yet
- Endometriosis & Adenomyosis Dr. Selly Septina, SpogDocument25 pagesEndometriosis & Adenomyosis Dr. Selly Septina, SpogRezkiRamadhanNo ratings yet
- CHN Rle Midterm Exam ReviewerDocument3 pagesCHN Rle Midterm Exam Reviewercassy SadieNo ratings yet
- Vocal Cord ParalysisDocument74 pagesVocal Cord ParalysisWaqas KhanNo ratings yet
- Pediatric TB Diagnosis UpdatesDocument39 pagesPediatric TB Diagnosis UpdatesSiddhartha NandiNo ratings yet
- HAAD Exam For Nurses Questions 2018Document46 pagesHAAD Exam For Nurses Questions 2018Asif Newaz100% (6)
- Adult Vancomycin Dosing Guidelines DefinitionsDocument2 pagesAdult Vancomycin Dosing Guidelines DefinitionsPhạm DuyênNo ratings yet
- MECONIUM Aspiration SyndromeDocument37 pagesMECONIUM Aspiration SyndromekamalaNo ratings yet
- Med SurgDocument23 pagesMed SurgReymart AcalaNo ratings yet
- Causes, Symptoms and Treatment of Left Ventricular Hypertrophy (LVHDocument5 pagesCauses, Symptoms and Treatment of Left Ventricular Hypertrophy (LVHJàson Vòrhees100% (1)
- No Evidence For Contraindications To The Use of Propofol in Adults Allergic To Egg, Soy or Peanut 2016Document6 pagesNo Evidence For Contraindications To The Use of Propofol in Adults Allergic To Egg, Soy or Peanut 2016Jhon RodriguezNo ratings yet
- Low-Level AutoimmunityDocument13 pagesLow-Level AutoimmunityBeeBee SethNo ratings yet
- Breast - Calcifications Differential Diagnosis: Anatomy Diagnostic ApproachDocument22 pagesBreast - Calcifications Differential Diagnosis: Anatomy Diagnostic ApproachDokdem AjaNo ratings yet
- ModuleIV RespiratoryEmergencies CHF COPD AsthmaDocument96 pagesModuleIV RespiratoryEmergencies CHF COPD AsthmaSaiKiranNo ratings yet
- Triads in Surgery ListDocument2 pagesTriads in Surgery ListTalha AnwarNo ratings yet
- Dr. Satyam Rajvanshi Dr. Ram Manohar Lohia Hospital, New DelhiDocument124 pagesDr. Satyam Rajvanshi Dr. Ram Manohar Lohia Hospital, New DelhiazizhaNo ratings yet
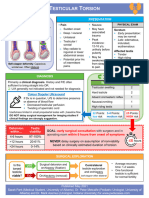
- Testicular Torsion, Peds Cases NotesDocument1 pageTesticular Torsion, Peds Cases NotesdzalhcNo ratings yet
- Horner Syndrome: DescriptionDocument3 pagesHorner Syndrome: DescriptionMeike WinataNo ratings yet
- LoperamideDocument1 pageLoperamidekimglaidyl bontuyanNo ratings yet
- Understanding Thrombophilia Risk FactorsDocument9 pagesUnderstanding Thrombophilia Risk FactorsSeraj Abed ElmoatiNo ratings yet