Professional Documents
Culture Documents
Types of CHD-Angina
Uploaded by
sunilk09Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Types of CHD-Angina
Uploaded by
sunilk09Copyright:
Available Formats
Types of CHD
CHD
Chronic Ischemic Heart Disease
Acute Coronary Syndrome
Stable
Angina
Variant
Angina
Silent
Myocardial
Ischemia
Non ST-segment
Elevation MI
(Unstable Angina)
ST-segment
Elevation MI
Angina Pectoris /
Myocardial Ischemia
Ischemia suppressed blood flow
Angina to choke
Occurs when blood supply is inadequate
to meet the hearts metabolic demands
Symptomatic paroxysmal chest pain or
pressure sensation associated with
transient ischemia
Pathophysiology
Causes: Atherosclerosis, HPN, DM, Buergers Disease,
Polycythemia Vera, Aortic regurgitation
Reduced coronary tissue perfusion
Decreased myocardial oxygenation
Anaerobic metabolism
Increased lactic acid production (lactic acidosis)
Chest pain
Types
A. Stable angina the common initial manifestation of a heart disease
Common cause: atherosclerosis (although those with advance
atherosclerosis do not develop angina)
Pain is precipitated by increased work demands of the heart (i.e..
physical exertion, exposure to cold, & emotional stress)
Pain location: precordial or substernal chest area
Pain characteristics:
- constricting, squeezing, or suffocating sensation generally
steady, increasing in intensity only at the onset & of attack
- May radiate to left shoulder, arm, jaw, or other chest areas
duration: < 15mins
- Relieved by rest (preferably sitting or standing with support)
or by use of NTG
B. Variant/Vasospastic Angina (Prinzmetal Angina)
1
st
described by Prinzmetal & Associates in 1659
Cause: spasm of coronary arteries (vasospasm) due to
coronary artery stenosis
Mechanism is uncertain (may be from hyperactive
sympathetic responses, mishandling defects of
calcium in smooth vascular muscles, reduced
prostaglandin I
2
production)
Pain Characteristics: occurs during rest or with minimal
exercise
- commonly follows a cyclic or regular pattern of
occurrence (i.e.. Same time each day usually at early
hours)
If client is for cardiac cath, Ergonovine (nonspecific
vasoconstrictor) may be administered to evoke anginal
attack & demonstrate the presence & location of
spasm
Cont
C. Nocturnal Angina - frequently occurs
nocturnally (may be associated with REM
stage of sleep)
D. Angina Decubitus paroxysmal chest pain
occurs when client sits or stands up
E. Post-infarction Angina occurs after MI
when residual ischemia may cause
episodes of angina
Cont
Dx: detailed pain history, ECG, TST, angiogram may
be used to confirm & describe type of angina
Tx: directed towards MI prevention\
- Lifestyle modification (individualized regular
exercise program, smoking cessation)
- Stress reduction
- Diet changes
- Avoidance of cold
- PTCA (percutaneous transluminal coronary
angioplasty) may be indicated if with severe
artery occlusion
Drug Therapy
Nitroglycerin (NTGs)
vasodilators:
patch (Deponit, Transderm-
NTG)
sublingual (Nitrostat)
oral (Nitroglyn)
IV (Nitro-Bid)
-adrenergic blockers:
Propanolol (Inderal)
Atenolol (Tenormin)
Metoprolol (Lopressor)
Calcium channel blockers:
Nifedipine (Calcibloc,
Adalat)
Diltiazem (Cardizem)
Lipid lowering agents
statins:
Simvastatin
Anti-coagulants:
ASA (Aspirin)
Heparin sodium
Warfarin (Coumadin)
Classification
Class I angina occurs with strenuous, rapid, or prolonged
exertion at work or recreation
Class II angina occurs on walking or going up the stairs
rapidly or after meals, walking uphill, walking more than 2
blocks on the level or going more than 1 flight of ordinary
stairs at normal pace, under emotional stress, or in cold
Class III angina occurs on walking 1-2 blocks on the level
or going 1 flight of ordinary stairs at normal pace
Class IV angina occurs even at rest
Nursing Management
Diet instructions (low salt, low fat,
low cholesterol, high fiber); avoid
animal fats
E.g.. White meat chicken w/o
skin, fish
Stop smoking & avoid alcohol
Activity restrictions are placed
within clients limitations
NTGs max of 3doses at 5-min
intervals
Stinging sensation under the
tongue for SL is normal
Advise clients to always carry 3
tablets
Store meds in cool, dry place,
air-tight amber bottles & change
stocks every 6months
Inform clients that headache,
dizziness, flushed face are
common side effects.
Do not discontinue the drug.
For patches, rotate skin sites
usually on chest wall
Instruct on evaluation of
effectiveness based on pain
relief
Propanolols causes bronchospasm
& hypoglycemia, do not administer
to asthmatic & diabetic clients
Heparin monitor bleeding
tendencies (avoid punctures, use
of soft-bristled toothbrush);
monitor PTT levels; used for 2wks
max; do not massage if via SC;
have protamine sulfate available
Coumadin monitor for bleeding
& PT; always have vit K readily
available (avoid green leafy
veggies)
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Maternal PelvisDocument32 pagesMaternal Pelvissunilk09100% (1)
- Pediatric Dermatology MCQsDocument53 pagesPediatric Dermatology MCQsDr.Tawheed89% (18)
- Pulmonary Artery CatheterDocument22 pagesPulmonary Artery Cathetersunilk09100% (1)
- Community Medicine MCQsDocument355 pagesCommunity Medicine MCQsKalpu Bala100% (10)
- Case Write UpDocument15 pagesCase Write UpAmirul Hafiz100% (1)
- NCPDocument6 pagesNCPNicole Marin-ChingNo ratings yet
- Joint DislocationsDocument64 pagesJoint DislocationsSabrina Indri WardaniNo ratings yet
- Pre EclampsiaDocument39 pagesPre EclampsiaStanly Elliemo100% (1)
- Endodontic MishapsDocument34 pagesEndodontic MishapsSimpy Jindal100% (1)
- Title: Mental Health and Mental IllnessDocument14 pagesTitle: Mental Health and Mental Illnesssunilk09No ratings yet
- Identify The Bony Walls and Ligamentous Landmarks of The PelvisDocument11 pagesIdentify The Bony Walls and Ligamentous Landmarks of The Pelvissunilk09No ratings yet
- Anemia MantapDocument63 pagesAnemia MantapyasminNo ratings yet
- MeaslesDocument3 pagesMeaslessunilk09No ratings yet
- Title: Mental Health and Mental IllnessDocument14 pagesTitle: Mental Health and Mental Illnesssunilk09No ratings yet
- ScabiesDocument7 pagesScabiessunilk09No ratings yet
- Globin DisordersDocument47 pagesGlobin DisordersSutapa PawarNo ratings yet
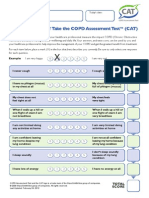
- CATest PDFDocument1 pageCATest PDFAsrie Sukawatie PutrieNo ratings yet
- Tissue Viability Training for NursesDocument3 pagesTissue Viability Training for Nursessunilk09No ratings yet
- 7284026Document8 pages7284026Mariya Mikaela Garcia SoledadNo ratings yet
- The Supplemental Oxygen Guide COPDF v1.1!6!26-15Document10 pagesThe Supplemental Oxygen Guide COPDF v1.1!6!26-15Kesava Dhika VasudevaNo ratings yet
- Contract IlityDocument9 pagesContract Ilitysunilk09No ratings yet
- Globin DisordersDocument47 pagesGlobin DisordersSutapa PawarNo ratings yet
- Home Care GuideDocument12 pagesHome Care Guidesunilk09No ratings yet
- Cloud ComputingDocument12 pagesCloud Computingsunilk09No ratings yet
- Kidney TransplantDocument1 pageKidney Transplantsunilk09No ratings yet
- Chapter 4 CPR ManualDocument4 pagesChapter 4 CPR Manualsunilk09No ratings yet
- Chapter 3 CPR ManualDocument5 pagesChapter 3 CPR Manualsunilk09No ratings yet
- Chapter 2 CPR ManualDocument6 pagesChapter 2 CPR Manualsunilk09No ratings yet
- Acute Coronary Syndrome MIDocument11 pagesAcute Coronary Syndrome MIsunilk09No ratings yet
- The Patient With Altered ConsciousnessDocument59 pagesThe Patient With Altered Consciousnesssunilk09No ratings yet
- HealthcareDocument38 pagesHealthcaresunilk09No ratings yet
- DVT ProphylaxisDocument11 pagesDVT Prophylaxissunilk09No ratings yet
- Case Study OnDocument1 pageCase Study Onsunilk09No ratings yet
- Notes AlocDocument9 pagesNotes Alocsunilk09No ratings yet
- GroupDocument3 pagesGroupsunilk09No ratings yet
- AtherosclerosisDocument4 pagesAtherosclerosissunilk09No ratings yet
- Mapping Bedah Saraf ICUDocument1 pageMapping Bedah Saraf ICUDessy FarwasNo ratings yet
- Pengenalan DiabetesDocument57 pagesPengenalan DiabetesAsma MandaNo ratings yet
- NCP LymphomaDocument3 pagesNCP LymphomaJohn Emmanuel Tatad TudNo ratings yet
- Hesi MHDocument3 pagesHesi MHangeladbranchNo ratings yet
- Dialog Dental PatientDocument2 pagesDialog Dental PatientLiza ChumikaNo ratings yet
- Anal Sphincter Muscles Strengthening Exercises - Jun20Document2 pagesAnal Sphincter Muscles Strengthening Exercises - Jun20Naved ShaikhNo ratings yet
- Health Teaching PlanDocument3 pagesHealth Teaching PlanSonia MambaNo ratings yet
- Myofascial Trigger Points - Pathophysiology and Evidence-Informed Diagnosis and Management (Contemporary Issues in Physical Therapy and Rehabilitation Medicine) (PDFDrive)Document306 pagesMyofascial Trigger Points - Pathophysiology and Evidence-Informed Diagnosis and Management (Contemporary Issues in Physical Therapy and Rehabilitation Medicine) (PDFDrive)Christine DiVirgilioNo ratings yet
- Bhoomi PatelDocument9 pagesBhoomi PatelPooja PanchalNo ratings yet
- Shibashi BenefitsDocument2 pagesShibashi BenefitschandramouuliNo ratings yet
- Coagulation Problems PPTDocument69 pagesCoagulation Problems PPTBao NguyenNo ratings yet
- Brain InfectionsDocument18 pagesBrain InfectionsSarah Naura IrbahNo ratings yet
- CD 34845Document2 pagesCD 34845ReaMetrix100% (2)
- ملخص د. سامر رستم - الجهاز التنفسي - تشريح مرضي خاصDocument3 pagesملخص د. سامر رستم - الجهاز التنفسي - تشريح مرضي خاصd-khaldounNo ratings yet
- Adams-Stokes 1º Sintoma Febre ReumáticaDocument5 pagesAdams-Stokes 1º Sintoma Febre Reumáticacarvalho.tr4270No ratings yet
- Original ArticleDocument8 pagesOriginal ArticleAshlea HunterNo ratings yet
- PhenomenalDocument10 pagesPhenomenalPeter Ngicur CarthemiNo ratings yet
- International Journal of Nursing StudiesDocument10 pagesInternational Journal of Nursing StudiesMuhammad Muslih, S.Kep., NS.No ratings yet
- Obesity Disease: Polikandrioti Maria, Stefanou EvageliaDocument7 pagesObesity Disease: Polikandrioti Maria, Stefanou Evageliaali amineNo ratings yet
- Chapter 3Document28 pagesChapter 3naveen chitiralaNo ratings yet
- Vulstan James Shedura-Curriculum Vitae (CV)Document14 pagesVulstan James Shedura-Curriculum Vitae (CV)Vulstan James SheduraNo ratings yet
- Delatorrecanales 2019Document11 pagesDelatorrecanales 2019ELIAS DAVID NOBMAN ALVARADONo ratings yet
- What Is The Most Important Component of Blood Pressure: Systolic, Diastolic or Pulse Pressure?Document5 pagesWhat Is The Most Important Component of Blood Pressure: Systolic, Diastolic or Pulse Pressure?Susan SuárezNo ratings yet