Professional Documents
Culture Documents
SIADH (Syndrome of Inapproperiate Antidiuretic Hormone Secretion)
Uploaded by
itsmesubu100%(2)100% found this document useful (2 votes)
2K views11 pagesits my presentation hope u will like it
Original Title
SIADH ( syndrome of inapproperiate antidiuretic hormone secretion)
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentits my presentation hope u will like it
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
100%(2)100% found this document useful (2 votes)
2K views11 pagesSIADH (Syndrome of Inapproperiate Antidiuretic Hormone Secretion)
Uploaded by
itsmesubuits my presentation hope u will like it
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 11
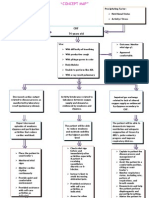
SIADH
WHAT IS ADH? AND FROM WHERE
IT IS SECRETED? AND FUNCTIONS
OF ADH.
• Anti diuretic hormone. Secreted by posterior
pituitary or neurohypophysis to the distal
convoluted tubules and collecting tubules of
the nephron.
• Functions:-function of ADH on the kidneys
is to control the amount of water reabsorbed
by kidney nephrons and causes the retention
of water, but not solute. Hence, ADH activity
effectively dilutes the blood.
hypothalamus( osmoreceptors)
posterior pituitary
ADH
aquaporins (DCT and CT)
urine out put
• ADH is secreted to prevent water loss in the kidneys.
When water is ingested, it is taken up into the
circulation and results in a dilution of the plasma.
This dilution, otherwise described as a reduction in
plasma osmolality, is detected by osmoreceptors in
the hypothalamus of the brain and these then switch
off the release of ADH.
• The decreasing concentration of ADH effectively
inhibits the aquaporins in the collecting ducts and
distal convoluted tubules in the nephrons of the
kidney. Hence, less water is reabsorbed, thereby
increasing urine output, decreasing urine osmolality,
and increasing (normalization of) blood osmolality.
WHAT IS SIADH AND ITS CAUSES
AND CLINICAL FEATURE.
• This is a syndrome characterized by
excessive release of antidiuretic hormone
(ADH or vasopressin) from the posterior
pituitary gland.
• The result is hyponatremia, and
sometimes fluid overload
Some common causes of SIADH
include:
• meningitis (treated with fluid restriction and diuretics)
• Head injury
• Subarachnoid hemorrhage
• Cancers
• Lung cancer (especially small cell lung cancer, as well
as other small-cell malignancies of other organs)
• Infections
• Brain abscess
• Drugs
• Carbamazepine
• Selective serotonin reuptake inhibitors (SSRIs, a class
of antidepressants)
• Methylenedioxymethamphetamine (MDMA)
c/f
• In general, increased ADH causes water retention
and extracellular fluid volume expansion without
edema or hypertension, owing to natriuresis
(retention of water and passing of sodium in urine).
• The water retention and sodium loss both cause
hyponatremia, which is a key feature in SIADH.
Hyponatremia and concentrated urine (UOsm >300
mOsm) are seen, as well as no signs of edema or
dehydration.
• When hyponatremia is severe (sodium <120 mOsm),
or acute in onset, symptoms of cerebral edema
become prominent (irritability, confusion, seizures,
and coma).
WHAT IS THE DIANGNOSIS AND
MANAGEMENT OF SIADH
Dx ( c/f and lab findings)
• Hyponatremia <130 mEq/L, and POsm <270 mOsm/kg.
• Other findings include-
• Urine sodium concentration >20 mEqlL (inappropriate
natriuresis)
• Maintained hypervolemia
• Suppression of renin-angiotensin system
• No equal concentration of atrial natriuretic peptide
• Low blood urea nitrogen (BUN)
• Low creatinine
• Low uric acid
• Low albumin
management
• Treating underlying causes when possible.
• Fluid restriction to 800-1,000 ml/d should
be obtained to increase serum sodium.
• Intravenous saline - For very symptomatic
patients (severe confusion, convulsions, or
coma) hypertonic saline (5%) 200-300 ml
IV in 3-4 h should be given.
• Drugs
• Demeclocycline can be used in chronic situations
when fluid restrictions are difficult to maintain;
demeclocycline is the most potent inhibitor of AVP
action.
• Conivaptan - an approved antagonist of both V1A
and V2 vasopressin receptors. Its indications are
"treatment of euvolemic hyponatremia (e.g. the
syndrome of inappropriate secretion of antidiuretic
hormone, or in the setting of hypothyroidism,
adrenal insufficiency, pulmonary disorders, etc.) in
hospitalized patients."[1]
You might also like
- Case Study RespiDocument3 pagesCase Study RespiMark Jheran AlvarezNo ratings yet
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail Abaygar100% (3)
- Hypertension Pathophysiology and Treatment PDFDocument6 pagesHypertension Pathophysiology and Treatment PDFBella TogasNo ratings yet
- Managing Electrolyte Imbalances: A Case of Self-Induced HyperkalemiaDocument3 pagesManaging Electrolyte Imbalances: A Case of Self-Induced HyperkalemiaPaul JacksonNo ratings yet
- Syndrome of Inappropriate Secretion of Anti Diuretic HormoneDocument39 pagesSyndrome of Inappropriate Secretion of Anti Diuretic Hormonefarmasi_hmNo ratings yet
- SiadhDocument10 pagesSiadhehjing75% (4)
- Acute Renal Failure Nursing Care PlanDocument15 pagesAcute Renal Failure Nursing Care PlanRanusha AnushaNo ratings yet
- Pulmonary EmbolismDocument16 pagesPulmonary EmbolismniyigokNo ratings yet
- Impaired Tissue PerfusionDocument2 pagesImpaired Tissue PerfusionLyka Mae Imbat - PacnisNo ratings yet
- Nursing Care Plan Renal FailureDocument18 pagesNursing Care Plan Renal FailureKundan KumarNo ratings yet
- Clinical Features and Diagnosis of Hemophagocytic Lymphohistiocytosis - UpToDateDocument27 pagesClinical Features and Diagnosis of Hemophagocytic Lymphohistiocytosis - UpToDateSalvatore ScutoNo ratings yet
- Pathophysiology Diagram of Congestive Heart FailureDocument3 pagesPathophysiology Diagram of Congestive Heart FailureLeng Royo BrionesNo ratings yet
- Nursing Care Plan FinalDocument16 pagesNursing Care Plan FinalErickson OcialNo ratings yet
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPRomel BaliliNo ratings yet
- NCP For CHF 3 Activity IntoleranceDocument2 pagesNCP For CHF 3 Activity IntoleranceAngelyn ArdinesNo ratings yet
- Bulacan State University: College of NursingDocument29 pagesBulacan State University: College of NursingJohn Philip M. Lacas RN100% (3)
- NCPDocument15 pagesNCPCamille PinedaNo ratings yet
- Angina Pectoris PathophysiologyDocument2 pagesAngina Pectoris PathophysiologyALIANA KIMBERLY MALQUESTONo ratings yet
- Renal Failure NCPDocument3 pagesRenal Failure NCPjsksNo ratings yet
- Actual NCPDocument3 pagesActual NCPMabz BoholNo ratings yet
- Decrease Cardiac OutputDocument6 pagesDecrease Cardiac OutputGerardeanne ReposarNo ratings yet
- Hyperosmolar Hyperglycemic State (HHS)Document21 pagesHyperosmolar Hyperglycemic State (HHS)Malueth AnguiNo ratings yet
- Impaired Tissue Perfusion Related To The Weakening / Decreased Blood Flow To The Area of Gangrene Due To Obstruction of Blood VesselsDocument3 pagesImpaired Tissue Perfusion Related To The Weakening / Decreased Blood Flow To The Area of Gangrene Due To Obstruction of Blood VesselsKat AlaNo ratings yet
- As Needed.: Environmental Stimuli 6Document4 pagesAs Needed.: Environmental Stimuli 6Nicole GumolonNo ratings yet
- Healthcare - Nursing Care Plan - Excess Fluid VolumeDocument4 pagesHealthcare - Nursing Care Plan - Excess Fluid VolumeBenjamin CañalitaNo ratings yet
- IBSDocument1 pageIBSIris MambuayNo ratings yet
- Nursing Care Plan for Functional Urinary IncontinenceDocument4 pagesNursing Care Plan for Functional Urinary IncontinenceJez RarangNo ratings yet
- Addison'sDocument4 pagesAddison'sKoRnflakesNo ratings yet
- HypokalemiaDocument3 pagesHypokalemiaSergeiNo ratings yet
- NCP CKDDocument3 pagesNCP CKDRiel TumandaNo ratings yet
- Aminogen Drug StudyDocument2 pagesAminogen Drug Studymilesmin100% (1)
- Week 10 Drug Card - Hydrochlorothiazide (HCTZ)Document2 pagesWeek 10 Drug Card - Hydrochlorothiazide (HCTZ)RCurry09No ratings yet
- Myocardial Infarction (Diseases For Oral Revalida)Document12 pagesMyocardial Infarction (Diseases For Oral Revalida)Suzette PipoNo ratings yet
- Case Study - ESRD (DS, NCP)Document8 pagesCase Study - ESRD (DS, NCP)Zhy CaluzaNo ratings yet
- Intracranial HemorrhageDocument41 pagesIntracranial Hemorrhagedoctormussieaberra100% (1)
- Drug StudyDocument7 pagesDrug StudyMelody Forca FranciscoNo ratings yet
- NCP PainDocument2 pagesNCP PainApril_Ivy_Raga_3835No ratings yet
- COLCHICINE pptx1800128929Document15 pagesCOLCHICINE pptx1800128929April Mergelle LapuzNo ratings yet
- Case StudyDocument34 pagesCase StudyBSNNursing101No ratings yet
- What Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistDocument12 pagesWhat Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistLidiaAMonroyRNo ratings yet
- Parenteral Fluid Therapy: Types of Intravenous SolutionDocument18 pagesParenteral Fluid Therapy: Types of Intravenous SolutionKathleen Joy Costales Magtanong100% (1)
- 6 Nursing Care Plan 1Document2 pages6 Nursing Care Plan 1Denise Louise PoNo ratings yet
- Managing Fall Risk in an 84-Year-Old Asian MaleDocument4 pagesManaging Fall Risk in an 84-Year-Old Asian Malesavvy_as_98-1No ratings yet
- Nursing Care Plan: Cues Nursing Diagnosis Goals Adnd Desired Outcome Nursing Intervention Implementation EvaluationDocument5 pagesNursing Care Plan: Cues Nursing Diagnosis Goals Adnd Desired Outcome Nursing Intervention Implementation EvaluationNur SanaaniNo ratings yet
- Novilyn C. Pataray BSN - Ii Hemophilia: St. Paul College of Ilocos SurDocument1 pageNovilyn C. Pataray BSN - Ii Hemophilia: St. Paul College of Ilocos SurCharina AubreyNo ratings yet
- DM & DI ExamsDocument11 pagesDM & DI ExamsTomzki CornelioNo ratings yet
- NCP BMDocument1 pageNCP BMSourabh MehraNo ratings yet
- Co DiovanDocument2 pagesCo DiovanianecunarNo ratings yet
- Impaired kidney function nursing careDocument21 pagesImpaired kidney function nursing careKate ManalastasNo ratings yet
- Impaired Gas ExchangeDocument1 pageImpaired Gas Exchangeruggero07No ratings yet
- NCP Self CaRE DeficitDocument1 pageNCP Self CaRE Deficitnicole pageNo ratings yet
- Pathophysiology of Portal HYPERTENSION PDFDocument11 pagesPathophysiology of Portal HYPERTENSION PDFCamilo VidalNo ratings yet
- Managing Fever in a Child with PoliomyelitisDocument4 pagesManaging Fever in a Child with PoliomyelitisMonica RamboyongNo ratings yet
- NCP FVDDocument1 pageNCP FVDsisjing88510No ratings yet
- SiadhDocument16 pagesSiadhGokul Rajan100% (1)
- HypopituitarismDocument2 pagesHypopituitarismAnne de VeraNo ratings yet
- Soapie Charting: Date/ Time/ ShiftDocument2 pagesSoapie Charting: Date/ Time/ Shiftspain michaelisNo ratings yet
- Ineffective Tissue Perfusion PDFDocument4 pagesIneffective Tissue Perfusion PDFgcodouganNo ratings yet
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezNo ratings yet
- Neuroimaging and DNA Profiling New AvenuesDocument52 pagesNeuroimaging and DNA Profiling New AvenuesDr-Ajay TripathiNo ratings yet
- Nursing Care Plan PrenatalDocument5 pagesNursing Care Plan PrenatalKim Galamgam100% (2)
- Evaluation of The Patient With Vertigo - UpToDate PDFDocument29 pagesEvaluation of The Patient With Vertigo - UpToDate PDFDanna GarcíaNo ratings yet
- HIV and PregnancyDocument2 pagesHIV and PregnancyMagdalena Dwiyani HutajuluNo ratings yet
- Postpartum Complications: Donald G. Camatura, RNDocument96 pagesPostpartum Complications: Donald G. Camatura, RNDonald Garcesa Camatura100% (4)
- QA03005 Critical Testand Critical Result ReportingDocument7 pagesQA03005 Critical Testand Critical Result Reportingdebbie o. azcunaNo ratings yet
- 8 Emergency Formative Clinical Evaluation ChecklistDocument1 page8 Emergency Formative Clinical Evaluation Checklistمهند الرحيليNo ratings yet
- Instrument ProcessingDocument47 pagesInstrument ProcessingMarwa Temirek100% (1)
- IV Induction Agents: Propofol, Ketamine, Etomidate, ThiopentoneDocument2 pagesIV Induction Agents: Propofol, Ketamine, Etomidate, ThiopentoneNdalilashiwa Penehafo Ndakondja-VictorNo ratings yet
- Neuro-Associative Conditioning: Programing Your Trading Mind'Document21 pagesNeuro-Associative Conditioning: Programing Your Trading Mind'ediNo ratings yet
- 2014 AHA/ACC Guidelines for Managing NSTE-ACSDocument46 pages2014 AHA/ACC Guidelines for Managing NSTE-ACSEmmieNo ratings yet
- Effects of Maitland Mobilization and Mul PDFDocument6 pagesEffects of Maitland Mobilization and Mul PDFKuroha Hagane KunNo ratings yet
- Exodus SMLXL Rem KoolhaasDocument11 pagesExodus SMLXL Rem Koolhaasjako60No ratings yet
- Cholera El TorDocument16 pagesCholera El Torisabelleilagan0% (1)
- Megan Talbott ResumeDocument3 pagesMegan Talbott Resumeapi-291314145No ratings yet
- 4 INT Hana Adiva Praditri 22295 BloodFilmtoDiagnoseMalariaDocument6 pages4 INT Hana Adiva Praditri 22295 BloodFilmtoDiagnoseMalariaHana AdivaNo ratings yet
- Literature Review For Specimen Labeling and Blood BankDocument3 pagesLiterature Review For Specimen Labeling and Blood Bankapi-236445988No ratings yet
- Safe SuctioningDocument31 pagesSafe SuctioningKatrina Ponce100% (2)
- Adult Grip Strength Norms For The Baseline Digital DynamometerDocument25 pagesAdult Grip Strength Norms For The Baseline Digital DynamometerOmar Escalante DíazNo ratings yet
- Change Your Breakfast Change Your Life PDFDocument189 pagesChange Your Breakfast Change Your Life PDFDrUmeshSharmaNo ratings yet
- Pharmacology Test 3 Drug ListDocument32 pagesPharmacology Test 3 Drug ListSHRIKANTNo ratings yet
- AFI + Trombocytopenia, Dyspepsia SyndromeDocument20 pagesAFI + Trombocytopenia, Dyspepsia SyndromeMuhammad Bilal SaifulhaqNo ratings yet
- NeocortexDocument1 pageNeocortexZeromalisNilNo ratings yet
- Acquired Brain en Una Tienda de LibrosDocument428 pagesAcquired Brain en Una Tienda de Libroslig100% (1)
- Chronic Suppurative Otitis MediaDocument4 pagesChronic Suppurative Otitis MediarchristoverNo ratings yet
- Trypanosomiasis & LeishmaniasisDocument50 pagesTrypanosomiasis & LeishmaniasisMardoni Efrijon75% (4)
- ICU Liberation PosterDocument1 pageICU Liberation PosterhelenaNo ratings yet
- Theraband Clinical Reference GuideDocument48 pagesTheraband Clinical Reference GuideSan DyNo ratings yet
- Parotid Tumors and Other Salivary Gland TumorsDocument41 pagesParotid Tumors and Other Salivary Gland Tumorsdrhiwaomer100% (9)
- Aiswarya Krishna: Professional SummaryDocument4 pagesAiswarya Krishna: Professional SummaryRejoy RadhakrishnanNo ratings yet