Professional Documents
Culture Documents
Parkinsons Disease
Uploaded by
Pratik PatelCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Parkinsons Disease
Uploaded by
Pratik PatelCopyright:
Available Formats
ALSO KNOWN AS IDIOPATHIC PARKINSONS DISEASE The motor symptoms of Parkinson's disease result from the death of dopamine-generating
cells in the substantia nigra, a region of the midbrain; the cause of this cell death is unknown. Early in the course of the disease, the most obvious symptoms are movement-related; these include shaking, rigidity, slowness of movement and difficulty with walking and gait. Later, cognitive and behavioural problems may arise, with dementia commonly occurring in the advanced stages of the disease. Other symptoms include sensory, sleep and emotional problems. PD is more common in the elderly, with most cases occurring after the age of 50.
Parkinson's disease affects movement, producing motor symptoms . Non-motor symptoms, which include autonomic dysfunction, neuropsychiatric problems (mood, cognition, behavior or thought alterations), and sensory and sleep difficulties, are also common. Motor A man with Parkinson's disease displaying a flexed walking posture pictured in 1892. Photo appeared in Nouvelle Iconographie de la Salptrire, vol. 5. Handwriting of a person affected by PD in Lectures on the diseases of the nervous system by Charcot (1879). The original description of the text states "The strokes forming the letters are very irregular and sinuous, whilst the irregularities and sinuosities are of a very limited width. (...) the down-strokes are all, with the exception of the first letter, made with comparative firmness and are, in fact, nearly normal the finer up-strokes, on the contrary, are all tremulous in appearance
Tremor is the most apparent and well-known symptom It is
the most common; though around 30% of individuals with PD do not have tremor at disease onset, most develop it as the disease progresses] It is usually a rest tremor: maximal when the limb is at rest and disappearing with voluntary movement and sleep It affects to a greater extent the most distal part of the limb and at onset typically appears in only a single arm or leg, becoming bilateral later Frequency of PD tremor is between 4 and 6 hertz (cycles per second). A feature of tremor is pill-rolling, the tendency of the index finger of the hand to get into contact with the thumb and perform together a circular movement. The term derives from the similarity between the movement in PD patients and the earlier pharmaceutical technique of manually making pills.
(slowness of movement) is another characteristic feature of PD, and is associated with difficulties along the whole course of the movement process, from planning to initiation and finally execution of a movement. Performance of sequential and simultaneous movement is hindered .Bradykinesia is the most disabling symptom in the early stages of the disease.Initial manifestations are problems when performing daily tasks which require fine motor control such as writing, sewing or getting dressed. Clinical evaluation is based in similar tasks such as alternating movements between both hands or both feet. Bradykinesia is not equal for all movements or times. It is modified by the activity or emotional state of the subject, to the point that some patients are barely able to walk yet can still ride a bicycle. Generally patients have less difficulty when some sort of external cue is provided.
is stiffness and resistance to limb movement caused by increased muscle tone, an excessive and continuous contraction of muscles. In parkinsonism the rigidity can be uniform (lead-pipe rigidity) or ratchety (cogwheel rigidity). The combination of tremor and increased tone is considered to be at the origin of cogwheel rigidity. Rigidity may be associated with joint pain; such pain being a frequent initial manifestation of the disease. In early stages of Parkinson's disease, rigidity is often asymmetrical and it tends to affect the neck and shoulder muscles prior to the muscles of the face and extremities. With the progression of the disease, rigidity typically affects the whole body and reduces the ability to move.
Postural instability is typical in the late stages of the disease, leading to impaired balance and frequent falls, and secondarily to bone fractures. Instability is often absent in the initial stages, especially in younger people. Up to 40% of the patients may experience falls and around 10% may have falls weekly, with number of falls being related to the severity of PD. Other recognized motor signs and symptoms include gait and posture disturbances such as festination (rapid shuffling steps and aforwardflexed posture when walking), speech and swallowing disturbances including voice disorders, mask-like face expression orsmall handwriting, although the range of possible motor problems that can appear is large.
Neuropsychiatric Parkinson's disease can cause neuropsychiatric disturbances which can range from mild to severe. This includes disorders of speech, cognition, mood, behaviour, and thought. Cognitive disturbances can occur in the initial stages of the disease and sometimes prior to diagnosis, and increase in prevalence with duration of the disease.The most common cognitive deficit in affected individuals is executive dysfunction, which can include problems with planning, cognitive flexibility, abstract thinking, rule acquisition, initiating appropriate actions and inhibiting inappropriate actions, and selecting relevant sensory information. Fluctuations in attention and slowed cognitive speed are among other cognitive difficulties. Memory is affected, specifically in recalling learned information. Nevertheless, improvement appears when recall is aided by cues. Visuospatial difficulties are also part of the disease, seen for example when the individual is asked to perform tests of facial recognition and perception of the orientation of drawn lines.
Most people with Parkinson's disease have idiopathic Parkinson's disease (having no specific known cause). A small proportion of cases, however, can be attributed to known genetic factors. Other factors have been associated with the risk of developing PD, but no causal relationships have been proven. PD traditionally has been considered a non-genetic disorder; however, around 15% of individuals with PD have a first-degree relative who has the disease. At least 5% of people are now known to have forms of the disease that occur because of a mutation of one of several specific genes.
Brain cell death
There is speculation of several mechanisms by which the brain cells could be lost.One mechanism consists of an abnormal accumulation of the protein alphasynuclein bound to ubiquitin in the damaged cells. This insoluble protein accumul ates inside neurones forming inclusions called Lewy bodies.According to the Braak staging, a classification of the disease based on pathological findings, Lewy bodies first appear in the olfactory bulb, medulla oblongata and pontine tegmentum,
Levodopa Levodopa has been the most widely used treatment for over 30 years.L-DOPA is converted into dopamine in the dopaminergic neurons by dopa decarboxylase. Since motor symptoms are produced by a lack of dopamine in the substantia nigra, the administration of L-DOPA temporarily diminishes the motor symptoms. Only 510% of L-DOPA crosses the bloodbrain barrier. The remainder is often metabolized to dopamine elsewhere, causing a variety of side effects including nausea, dyskinesiasand joint stiffness.] Carbidopa and benserazide are peripheral dopa decarboxylase inhibitors,which help to prevent the metabolism of L-DOPA before it reaches the dopaminergic neurons, therefore reducing side effects and increasing bioavailability. They are generally given as combination preparations with levodopa.
TREATMENT
MAO-B inhibitors
MAO-B inhibitors (selegiline and rasagiline) increase the level of dopamine in the basal ganglia by blocking its metabolism. They inhibit monoamine oxidase-B (MAO-B) which breaks down dopamine secreted by the dopaminergic neurons. The reduction in MAO-B activity results in increased L-DOPA in the striatum. Like dopamine agonists, MAO-B inhibitors used as monotherapy improve motor symptoms and delay the need for levodopa in early disease, but produce more adverse effects and are less effective than levodopa. There are few studies of their effectiveness in the advanced stage, although results suggest that they are useful to reduce fluctuations between on and off periods.An initial study indicated that selegiline in combination with levodopa increased the risk of death, but this was later disproven.[ Other drugs such as amantadine and anticholinergics may be useful as treatment of motor symptoms. However, the evidence supporting them lacks quality, so they are not first choice treatments.
Rehabilitation Further information: Rehabilitation in Parkinson's disease There is some evidence that speech or mobility problems can improve with rehabilitation, although studies are scarce and of low quality.Regular physical exercise with or without physiotherapy can be beneficial to maintain and improve mobility, flexibility, strength, gait speed, and quality of life. However, when an exercise program is performed under the supervision of a physiotherapist, there are more improvements in motor symptoms, mental and emotional functions, daily living activities, and quality of life compared to a self-supervised exercise program at home. In terms of improving flexibility and range of
Palliative care Palliative care is often required in the final stages of the disease when all other treatment strategies have become ineffective. The aim of palliative care is to maximize the quality of life for the person with the disease and those surrounding him or her. Some central issues of palliative care are: care in the community while adequate care can be given there, reducing or withdrawing drug intake to reduce drug side effects, preventing pressure ulcers by management of pressure areas of inactive patients, and facilitating end-of-lifedecisions for the patient as well as involved friends and relatives
RIGOR MORTIS
Rigor mortis (Latin: rigor "stiffness", mortis "of death") is one of the recognizable signs of death, caused by chemical changes in the muscles after death, causing the limbs of the corpse to become stiff and difficult to move or manipulate. In humans, it commences after about three to four hours, reaches maximum stiffness after 12 hours, and gradually dissipates until approximately 48 to 60 hours after death.After death, cellular respiration in organisms ceases to occur, depleting the corpse of oxygen used in the making of adenosine triphosphate (ATP).
ATPis no longer provided to operate the SERCA pumps in the membrane of the sarcoplasmic reticulum, which pump calcium ions into the terminal cisternae.[1] This causes calcium ions to diffuse from the area of higher concentration (in the terminal cisternae and extracellular fluid) to an area of lower concentration (in the sarcomere), binding with troponin and allowing for crossbridgingto occur between myosin and actin proteins. Unlike in normal muscular contraction, after death, the body is unable to complete the cycle and release the coupling between the myosin and actin, creating a state of muscular contraction until the breakdown of muscle tissue by enzymes (endogenous or bacterial) during decomposition. As part of the process of decomposition, the myosin heads are degraded by the enzymes, allowing the muscle contraction to release and the body to relax.
Physical changes At the time of death, a condition called "primary flaccidity" occurs. Following this, the muscles stiffen in rigor mortis. All muscles in the body are affected. Starting between two and six hours following death, rigor mortis begins with the eyelids, neck, and jaw. The sequence may be due to different lactic acid levels among different muscles, which is directly related to the difference in glycogen levels and different types of muscle fibers. Rigor mortis then spreads to the other muscles within the next four to six hours, including the internal organs. The onset of rigor mortis is affected by the individual's age, sex, physical condition, and muscular build. Rigor mortis may not be perceivable in many infant and child corpses due to their smaller muscle mass.[5]
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Food and Nutrients in Disease Management - DepressionDocument21 pagesFood and Nutrients in Disease Management - DepressionJJJPARKERNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Neurobiological Basis of HypersexualityDocument21 pagesNeurobiological Basis of HypersexualityUgur BuyuktezgelNo ratings yet
- AMISULPRIDEDocument26 pagesAMISULPRIDERajmohan VNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Science of Swearing - A Look Into The Human MIND and Other Less Socially Acceptable Four-Letter Words - Harvard Science ReviewDocument9 pagesThe Science of Swearing - A Look Into The Human MIND and Other Less Socially Acceptable Four-Letter Words - Harvard Science ReviewShaimaa Suleiman100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Homoeopathic Treatment of Parkinson DieseDocument23 pagesHomoeopathic Treatment of Parkinson DieseNidhi SrivastavaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- C11 SchizophreniaDocument22 pagesC11 SchizophreniaMaJoy OrdoñezNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Dopamine PrecursorDocument5 pagesDopamine Precursormarie gold sorilaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- (Norton Professional Book) Erickson, Carlton K - The Science of Addiction - From Neurobiology To Treatment-W. W. Norton Company (2018 - 2007)Document381 pages(Norton Professional Book) Erickson, Carlton K - The Science of Addiction - From Neurobiology To Treatment-W. W. Norton Company (2018 - 2007)Muhammed Huzeyfe GültekinNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Sem14-Egyptians-Browncitos Team-IacsDocument10 pagesSem14-Egyptians-Browncitos Team-IacsSILVIA ROSARIO CHALCO MENDOZANo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Nursing Care For Persons With Drug AddictionDocument25 pagesNursing Care For Persons With Drug AddictionMalik MashooqNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Dopamine Detox and Its Role in Positive Mental Health-Reaserch PaperDocument4 pagesDopamine Detox and Its Role in Positive Mental Health-Reaserch PaperNihla RahmanNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Chapter 7: The Biologic Foundations of Psychiatric NursingDocument3 pagesChapter 7: The Biologic Foundations of Psychiatric NursingKINDATNo ratings yet
- Psychopharmacology HandoutsDocument13 pagesPsychopharmacology HandoutsAyuy Welliss MedusaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
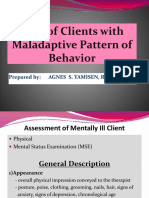
- Care of Clients With Maladaptive Pattern of Behavior NCM 105 LectureDocument70 pagesCare of Clients With Maladaptive Pattern of Behavior NCM 105 LectureMay June100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Amphetamine DebateDocument263 pagesThe Amphetamine DebateAndrew Kamen100% (2)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Anti Obesity Studies - Gamma OryzanolDocument1 pageAnti Obesity Studies - Gamma OryzanolRAJESH ANNAMALAI ALNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Nicotinic Receptors and ParkinsonDocument1 pageNicotinic Receptors and ParkinsonAnubhav NagalNo ratings yet
- Teal Swan's FrequenciesDocument11 pagesTeal Swan's FrequencieslaniNo ratings yet
- Brigitte King - InformativeDocument2 pagesBrigitte King - Informativeapi-262025468No ratings yet
- Materi 11 Efek Narkoba Pemaparan BNNDocument33 pagesMateri 11 Efek Narkoba Pemaparan BNNdummy002No ratings yet
- Summary Mental HealthDocument2 pagesSummary Mental HealthFebriansyah AslamNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- English For Academic and Professional Purposes: Quarter 2 - Module 8Document35 pagesEnglish For Academic and Professional Purposes: Quarter 2 - Module 8Unick Soriano NastorNo ratings yet
- Louis Harris - Problems of Drug Dependence 1991Document721 pagesLouis Harris - Problems of Drug Dependence 1991SmokeysamNo ratings yet
- Schizophrenia NCMH Case StudyDocument41 pagesSchizophrenia NCMH Case StudyJohn Crisostomo89% (36)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- All-Natural 5-Meo-Dmt Sigma Receptor 1 Agonist and Its Therapeutic Impact in Mental and Neurodegenerative Diseases Through Mitochondrial ActivationDocument22 pagesAll-Natural 5-Meo-Dmt Sigma Receptor 1 Agonist and Its Therapeutic Impact in Mental and Neurodegenerative Diseases Through Mitochondrial ActivationLex UNo ratings yet
- Psychology and Abnormality Notes - CIE Psychology A-LevelDocument17 pagesPsychology and Abnormality Notes - CIE Psychology A-LevelRajasekar Krishnasamy100% (1)
- Biological Approach Booklet 2021Document41 pagesBiological Approach Booklet 2021Abigail HARTNo ratings yet
- An Approach To Drug Induced Delirium in The Elderly BMJDocument7 pagesAn Approach To Drug Induced Delirium in The Elderly BMJLeonela Ramirez Almanza y Lina Maria Ossa HerreraNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- 2014 Parkinsons Report4Document12 pages2014 Parkinsons Report4ALLIA LOPEZNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)