Professional Documents
Culture Documents
Chronic Renal Failure Chapter 261 Pp. 1653-1663
Uploaded by
Emil GulmaticoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chronic Renal Failure Chapter 261 Pp. 1653-1663
Uploaded by
Emil GulmaticoCopyright:
Available Formats
mayj & mark ______________________________________________________________________________________
CHRONIC RENAL FAILURE Chapter 261; pp. 1653-1663
Mechanisms of Chronic Renal failure
Definition: a pathophysiologic process with multiple etiologies, resulting in the inexorable attrition of nephron number and function and frequently leading to an end stage renal disease (ESRD) ESRD irreversible loss of endogenous renal function of a degree sufficient to render the patient permanently dependent upon renal replacement therapy (dialysis or transplantation) in order to avoid life threatening Uremia. Uremia reflecting a dysfunction of all organ systems as a result of untreated or under treated acute or chronic renal failure.
PATHOPHYSIOLOGY AND BIOCHEMISTRY OF UREMIA Azotemia refers to the retention of nitrogeneous waste products as renal insufficiency develops Uremia refers to the more advanced stages of progressive renal insufficiency when the complex, multiorgan system derangements become clinically manifest. = pathophysiology of uremic syndrome can be divided into 2 sets of abnormalities : 1. those consequent to the accumulation or products of protein metabolism 2. those consequent to the loss of other renal functions, such as fluid and electrolyte homeostasis and hormonal abnormalities
Pathophysiology: - involves initiating mechanisms specific to the underlying etiology as well as a asset of progressive mechanisms that are common consequence of long tem reduction of renal mass, irrespective of etiology - such reduction of renal mass causes structural and functional hypertrophy by surviving nephrons. - Definition of CRD requires that the physiologic process last more than 3 mons. Stages of CRD Stage description GFR,ml/min/1.73 m2 At increased risk 90 (with CRD risk factors) 1 kidney damage w/ 90 Normal or GFR 2 3 4 5 kidney damage with mildly/ GFR Moderately GFR 60-89 30-59
CLINICAL AND LABORATORY MANIFESTATIONS OF CRF AND UREMIA
Fluid and electrolyte, and acid-base disorders A. Sodium and water homeostasis - disruption of glomerulotubular balance and promote Na retention, or excessive Na ingestion may lead to cumulative positive Na balance and attendant ECFV expansion. - Hyponatremia is uncommon in predialysis patients. Weight gain usually associated with volume expansion may be offset in CRD by concomitant loss of lean body mass. In CRD not yet on dialysis but has clear ECFV expansion, loop diuretics coupled with restriction of salt intake remains the mainstays of therapy. Loop diuretic + metazolone inhibits Na Cl contransporter of the distal convoluted tubule, can sometimes overcome diuretic resistance. GFR < 5-10 ml/min per 1.73 m2, even in high combination diuretics are ineffective indication of dialysis
Severely GFR 15 29 Renal failure < 15 (for dialysis) - at a GFR <15ml/min per 1.73 m2, renal replacement therapy may be indicated if uremia is present. - albuminuria serves as a key adjunctive tool for monitoring nephron injury and response to therapy in many forms of CRD - persistence of >17 mg albumin per gram of creatinine in adult males and 25 mg albumin per gram creatinine for adult females usually signify CRD, irrespective of GFR. - as the decline in GFR progresses to Stage 3 and 4 (GFR < 60 ml/min per 1.73m2), clinical and lab complications of CRD becomes progressively more prominent. ETIOLOGY AND EPIDEMIOLOGY - Hypertension is a particularly common cause and consequence of CRD in elderly - Cardiovascular mortality precludes most patients with CRD from reaching ESRD
B.
Potassium homeostasis - decline in GFR is not necessarily accompanied by a concomitant and proportional decline in urinary K excretion. - Hyperkalemia may be precipitated - Most commonly encountered medications that increases K are beta blockers, ACE, ARB, K sparers and NSAIDs. - Hypokalemia is uncommon, it reflects reduced dietary K intake, in association with excessive diuretic therapy or g.i losses
2. C. Metabolic acidosis - common disturbance during the advance stages of CRD - have reduced ability to produce NH3 - hyperkalemia further depresses NH4+ excretion. - Combination of hyperkalemia and hyperchloremic metabolic acidosis ( known as Type IV renal tubular acidosis, or hyporeninemic hypoaldosteronism) is most characteristically seen in patients with diabetes or in those with predominantly tubulointerstitial diseases - In advancing renal failure, o total urinary net daily acid excretion is usually limited to 30 to 40 mmol; o anion gap of ~20 mmol/L with a reciprocal fall in plasma HCO3 may develop o acidosis is mild; pH rarely < 7.35 and can usually be corrected by treating with 20 to 30 mmol of NaHCO3 or Na citrate daily. Bone disease and disorders of Ca and PO4 Metabolism The major disorders of bone disease in CRD can be classified as 1. 2. High bone turnover and high PTH levels ( including osteitis fibrosa, the hallmark lesion of secondary hyperparathyroidism) Low bone turnover with low or normal PTH levels (osteomalacia and adynamic bone disease)
Adynamic bone disease Hyperparathyroid bone lesion in CRD, esp. among DM; characterized by reduced bone volume and mineralization.
Other complications of Abnormal Ca-PO4 metabolism - Calciphylaxis abnormal Ca-PO4 product or metabolism; this represents a severe and systemic form of vascular and soft tissue ca-Po4 product deposition associated with skin and soft tissue necrosis, which can lead to extremity loss.
CARDIOVASCULAR ABNORMALITIES
leading cause of morbidity and mortality in patients with CRD at all stages emphasize prevention of cardiovascular complications aimed at alleviating the progression and complications of CRD itself
Ischemic Cardiovascular Disease Traditional/ Classic Risk Factors hypertension hypervolemia dyslipidemia sympathetic overactivity hyperhomocysteinuria CRD-Related/ Non-traditional risk factors anemia hyperphosphatemia hyperparathyroidism microinflammation state o rise in acute phase reactants such as IL-6 & CRP w/c contribute to coronary occlusive process and predictors of CV disease risk Congestive Heart Failure - abnormal cardiac function secondary to myocardial ischemic disease and/or left ventricular hypertrophy, together with salt and water retention in uremia - pulmonary congestion even in the absence of volume overload o normal or mildly elevated intracardiac and pulmonary capillary wedge pressure o radiologic: peripheral vascular congestion giving rise to butterfly wing distribution due to increased permeability of alveolar capillary membranes Hypertension and Left Ventricular Hypertrophy hypertension is the most common complication of CRD and ESRD may develop early during the course of CRD associated with adverse outcomes o more rapid loss of renal function o develop of CV disease Administration of EPO may increase BP and increase the requirement of antihypertensive drugs Absence of hypertension may o signify presence of salt wasting form of renal disease medullary cystic disease
Pathophysiology of bone disease secondary to hyperparathyroidism is related to abnormal mineral metabolism 1. 2. 3. GFR leads to iPO4 excretion and consequent PO4 retention retained PO4 has a direct stimulatory effect on PTH synthesis and on cellular mass of the parathyroid glands retained PO4 indirectly causes excessive production and secretion of PTH through lowering iCa and by suppression of calcitriol production reduced calcitriol production in CRD results both from synthesis due to reduced kidney mass and from hyperphospatemia
4.
High PTH levels stimulate osteoblasts and result in high bone turnover which leads to osteitis fibrosa cystica characterized by irregularly woven abnormal osteoid, fibrosis and cysts formation which results from decreased cortical bone and bone strength. Low-turnover disease can be classified into 2 categories: 1. Osteomalacia accumulation of mineralized bone matrix, or increased osteoid volume, which may be caused by vit. D deficiency, excess aluminum deposition, or metabolic acidosis
chronic tubulointerstitial disease papillary necrosis o ongoing antihypertensive therapy o volume depletion due to GI causes or diuretic, or reduced cardiac index volume overload is the major cause of hypertension in uremia; restore normotensive state by o appropriate salt restriction and natriuretic drugs or ultrafiltration in the dialysis setting o intravenous labetolol, fenoldopam or urapidil o Enalaprilat and other ACE inhibitors but in the face of bilateral renovascular disease, have the potential to further reduce GFR abruptly.
ECG: PR interval depression and diffuse ST-segment elevation o Echocardiography: accumulation of pericardial fluid leads to cardiac tamponade TREATMENT o absolute indication for the initiation of dialysis or for the intensification of the dialysis prescription in those already in dialysis o because of the propensity of hemorrhagic pericardial fluid, heparin-free dialysis is indicated o
HEMATOLOGIC ABNORMALITIES
a normocytic normochromic anemia is attributable to CRD (stage 3 and universal in stage 4) associated with a number of physiologic abnormalities O decreased tissue O2 delivery and utilization O increased cardiac output O cardiac enlargement O ventricular hypertrophy O angina O CHF O Decreased cognition and mental acuity O Altered menstrual cycles O Impaired host defense against infections O Growth retardation (children) Primary cause of anemia is insufficient production of EPO by diseased kidneys Additional factors for anemia O Iron and Folate deficiency O Severe hyperparathyroidism O Acute and chronic inflammation O Aluminum toxicity O Shortened red cell survival O Hemiglobinopathies
TREATMENT Management of Hypertension 1. to slow the progression of CRD itself 2. prevent the extra-renal complications of hypertension such as CV disease and stroke in CRD patients with diabetes or proteinuria >1g per 24 hr, blood pressure should be further reduced to 125/75 mmHg volume control with salt restriction and diuretics is the mainstay of therapy choice of antihypertensive agents is similar to general population; cardioprotective benefit by: ACE inhibitors and ARBs hydralazine and minoxidil direct acting vasodilators reserved for those rare patients in whom refractory hypertension persists; because it may perpetuate the tendency for CARDIAC HYPERTROPHY!b
Management of Cardiovascular Disease hypertension, hyperhomocysteinuria and lipid abnormalities promote atherosclerosis but treatable complications of CRD hyperlipidemia and hypercoagulability in nephritic syndrome increase risk of occlusive vascular disease life-style changes and therapeutic measures for cardiac risk reduction vitamin therapy for hyperhomocysteinuria w/c includes folate supplementation to between 1 and 5 mg/day Hyperlipidemia if dietary measures are inadequate, the preferred lipid-lowering medications are gembrozil and HMG-CoA reductase inhibitor o Precaution: combining these two classes increases the risk of myositis and rhabdomyolysis in CRD and ESRD patients Pericarditis - Observed more often in underdialyzed patients than in predialysis CRD patients - Hallmarks of uremic pericarditis: o Pericardial pain w/ respiratory accentuation o Friction rub (multicomponent)
Treatment Factors of Anemia of CRD : O Chronic blood loss O Hemolysis O Marrow suppression by retained uremic factors O Reduced renal production of EPO Recombinant human EPO epoetin alfa Darbopoetin alfa is a hyperglycosylated analogue of recombinant human EPO that posses greater biologic activity and prolonged half-life Iron status of the patient must be assessed and adequate iron stores should be available before treatment with EPO O Because demands for Fe by erythroid marrow exceed the amount of iron that is immediately available for erythropoiesis Addition of other substrates and cofactors especially O Vitamin B12 O Folate Anemia resistant to recommended doses of EPO: O Inadequate dialysis O Uncontrolled hyperparathyroidism O Aluminum toxicity
O O
Chronic blood loss or hemolysis Associated hemoglobinopathy, malnutrition, chronic infection, multiple myeloma or other malignancy
Abnormal hemostasis Common in CRD associated with O prolongation of bleeding time , O decreased activity of platelet factor III O abnormal platelet aggregation and adhesiveness O impaired prothrombin consumption Clinical manifestations O Bleeding and bruising O Bleeding from surgical wounds O Spontaneous bleeding from GIT, pericardial sac or intracranial vault CRD patients have greater susceptibility to thromboembolic complications (especially with nephritic presentation) TREATMENT: O Abnormal bleeding and coagulopathy Desmopressin Cryoprecipitate Conj. Estrogens Blood transfusions EPO O Anticoagulant prophylaxis when indicated
Increased incidence of diverticulosis (esp. polycystic kidney disease) Increased incidence of pancreatitis Management Protein restriction is useful in diminishing nausea and vomiting late in the course of renal failure o Not implemented in protein-energy malnutrition Assessment of protein energy malnutrition should begin at Stage 3 CRD (GFR <60 mL/min per 1.73 m2)
ENDOCRINE-METABOLIC DISTURBANCES
Glucose metabolism is impaired in CRD o Slowing of the rate of blood glucose level to decline after a glucose load o Plasma levels of insulin are slightly to moderately elevated in most uremic patients (fasting and postprandial states) o Response to insulin and glucose utilization is impaired o Metformin are contraindicated when GFR diminished to 25-50% Estrogen Levels are Low, and amenorrhea and inability to carry pregnancy to term are common manifestations of uremia GFR decline to 30% = pregnancy may hasten progression of CRD Men w/ CRD (including those in chronic dialysis): o Impotence o Oligospermia o Germinal cell dysplasia o Reduced plasma testosterone
NEUROMUSCULAR ABNORMALITIES
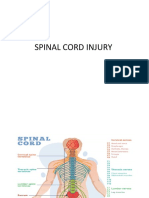
Central, peripheral and autonomic neuropathy, abnormalities in muscle composition and function Retained nitrogenous metabolites and middle molecules, PTH all contribute to the pathophysio Stage 3 CRD subtle clinical manifestations o Mild disturbances in memory, concentration and sleep disturbance Later stages (Stage 4) o Neuromuscular irritability (hiccups, cramps, fasciculations, twitching of muscles) o Asterixis, myoclonus, chorea are common in terminal uremia Peripheral neuropathy usually becomes clinically evident when the patient has been at stage 4 CRD >6months o Sensory nerves > motor nerves o LE > UE o Distal extremities > proximal restless leg syndrome ill-defined sensations of discomfort in the legs and feet requiring frequent leg movement o Dialysis is indicated o Or else, motor involvement (muscle weakness and loss of DTR)
DERMATOLOGIC ABNORMALITIES
Pallor (anemia) Ecchymoses and hematomas (defective hemostasis) Pruritus, excoriations (Calcium phosphate deposition and secondary hyperparathyroidism) Yellow discoloration (deposition of urochromes) Uremic frost (deposition of urea) Uremic pruritus remains a problem O Management: O Rule out unrelated skin disorders and control phosphate conc. Skin necrosis can occur as part of the calciphylaxis syndrome
EVALUATION AND MANAGEMENT OF PATIENTS WITH CRD
Initial Approach: History and PE Complaints referred to the kidneys themselves are often conspicuously absent in CRD Establish etiology of CRD o Hypertension o Diabetes o Systemic infectious, inflammatory or metabolic diseases o Exposure to drugs and toxins Drugs especially analgesics, NSAIDs, gold, penicillamine, antimicrobials, lithium and ACE inhibitors o Family hx of renal and urologic disease
GASTROINTESTINAL AND NUTRITIONAL ABNORMALITIES
Uremic fetor, a uriniferous odor to the breath, derives from the breakdown of urea to ammonia in saliva; associated with unpleasant metallic taste sensation Gastritis, PUD, mucosal ulcerations at any level of GIT occur in uremic patients can lead to abdominal pain, nausea, vomiting, blood loss
Uremic syndrome, ask about o Appetite o Diet o Nausea o Vomiting o Hiccupping o Shortness of breath o Edema o Weight change o Muscle cramps o Pruritus o Mental acuity o Activities of daily living Physical exam: o BP, fundoscopy, precordial exam, exam of the abdomen for bruits and palpable renal masses, exam for edema, neurologic exam for asterixis, muscle weakness, neuropathy
Demonstration of chronic metabolic bone disease w/ hyperphosphatemia, hypocalcemia, elevated PTH levels and radiologic bone disease\ Normocytic normochromic anemia Bilaterally reduced kidney size (<8.5 cm) Diagnosis of chronic hypertensive nephrosclerosis requires long history of long-standing HPN, in the absence of evidence of another renal disease. Usually proteinuria is mild to moderate (<3 g/d) and urine sediment is inactive In the absence of etiologically suggestive clinical constellation, renal biopsy may only be the recourse to establish etiology in early CRD
Laboratory Investigations Immunologic tests for SLE and vasculitis Serum and urinary protein electrophoresis (>40 y/o w/ unexplained CRD and anemia) = to rule out paraproteinemia Plasma creatinine and estimation of GFR, urea and electrolytes (including bicarbonate, calcium, phosphate and ALP) Urinalysis (when indicated, 24-h urine collection for protein excretion) BROAD CAST = reflects chronic tubulointerstitial scarring and tubular atrophy with widened tubule diameter Imaging studies Renal ultrasound verify the presence of two symmetric kidneys, estimate of kidney size, rule out renal masses and obstructive uropathy O Normal kidney size suggests acute rather than chronic, EXCEPT:
Polycystic kidney disease Amyloidosis Diabetes HIV-assoc. renal disease
Treatment It is of benefit to follow and plot the rate of decline in GFR in all patients Any acceleration in the rate of decline should prompt for search for superimposed acute processes that may lead to an acute and reversible decline in GFR in patients with CRD o Superimposed volume depletion o Accelerated and uncontrolled HPN o UTI o Superimposed obstructive uropathy o Nephrotoxic effects of medications (NSAID) o Radiocontrast agents o Reactivation or flare of original disease process Slowing progression of CRD Protein Restriction o Ameliorating the complications of uremia o Slow the rate of nephron injury (protein mediated hyperfiltration in progressive nephron injury) o Optimizes nutritional status and avoid malnutrition (0.6 g protein/kg per day) Composition of dietary protein be higher in energy supply sufficient to mitigate catabolic state Reducing Intraglomerular Hypertension and Proteinuria o Antihypertensive therapy aims to slow the progression of nephron injury, by ameliorating intragglomerular hypertension and hypertrophy o Target for pharma therapy is highly dependent on the level of proteinuria Elevated BP increases the proteinuria due to the transmission to the glomeruli of the elevated systemic pressure o Treatment guideline establishing 125/75 mmHg as the target blood pressure valie in proteinuric CRD patients o ACE inhibitors and ARB are now clearly established as effective, antiproteinuric agents The slowing in the progression of renal failure by these drugs is strongly related to their proteinuria-lowering effect Contraindications: o Intractable cough o Anaphylaxis o Hyperkalemia not controlled by dietary restriction Calcium channel blockers o 2nd line therapeutic approach if ACEI and ARB are contraindicated
Voiding cystourethrography O Rule out reflux O May be indicated in patients with hx of enuresis or family hx of reflux O Avoid exposure to IV radiocontrast dye = nephrotoxic!
Renal Biopsy Patients with near normal kidney size in whom clear cut diagnosis can not be made by les invasive means and when a possibility of reversible disease process remains tanable Contraindications: O Bilateral small kidneys O Polycystic kidney disease O Uncontrolled HPN O UTI or perinephric infection O Bleeding diathesis O Respiratory distress O Morbid obesity
ESTABLISHING THE DIAGNOSIS AND ETIOLOGY OF CRD
Urinary sediment that is inactive and reveals proteinuria and broad casts
o o
Diltiazem and verapamil More effective in preventing or ameliorating progressive renal injury than some other classes
Slowing Diabetic Renal Disease Diabetic nephropathy is now the leading cause of CRD eventuating in ESRD Prognosis of diabetic patients on chronic renal replacement therapy is POOR Glucose Control o Reduces the risk of kidney disease in patients with type I diabetes as well as type II o Achieve plasma values: 90-130 mg/dL preprandial glucose 110-150 mg/dL average bedtime glucose <7% - HbA1C o GFR reduction = mandates dose adjustment of many antihypertensive agents Discontinuation of metformin when plasma creatinine >1.5mg/dL Control of Blood Pressure and Proteinuria o Hypertension or abnormal circadian BP profile is found in 80% of type 2 diabetes; plus the presence of albuminuria = powerful predictors of CV and renal events o Microalbuminuria testing is recommended to all diabetic patients at least annually , and to follow therapeutic interventions
Microalbuminuria precedes the decline of GFR in diabetic patients and heralds renal and CV complications
o o
Antihypertensive agents = reduce albuminuria and diminishes the risk of albuminuria ACE inhibitors and ARBs have renoprotective properties to diabetic patients
Evidence of protein malnutrition Fluid and electrolyte abnormalities that are refractory to conservative measures Hx of hiccupping, intractable pruritus, morning nausea and vomiting, muscle twitching and cramps, presence of asterixis on PE It is ill-advised to assign a certain usual level of BUN, serum creatinine, or GFR to the need to dialysis because of interinvidual variability Patient Education and Adjustment o Prepare them with an intensive educational program explaining the likelihood and timing of initiation of renal replacement therapy and various forms of therapy available o Exploration of social service support resources o Only kidney transplantation offers the potential for nearly complete rehabilitation o Kidney transplantation follows a prior period of dialysis treatment: With dialysis first, at least for some period of time, to allow for the possible return to renal function before consideration of transplantation o For patients approaching ESRD in whom a reversible component has been excluded, and who have a good antigenic match with a willing donor, consideration should be given to preemptive or primary transplantation w/o intervening dialysis
Managing other complications of chronic renal failure Impending Uremic Symptomatology o Anorexia, nausea, vomiting, asterixis, lassitude and other CNS manifestations = temporarily relieved by protein restriction Medication Dose Adjustment o >70% excretion is nonrenal = no need for dosage adjustment o Entirely avoided Meperidine Metformin Other oral hypoglycemics with renal elimination o Reduction in dosage: Allopurinol Many antibiotics Several antihypertensives\ Antiarrythmics o Drugs that are nephrotoxic: NSAIDs Aggravate tendency to Na retention, HPN, HyperK, HypoNa, and further reduce GFR Preparation for Renal Replacement Therapy o NOT be indicated if the patient is asymptomatic o If w/ symptoms, start sufficiently early to prevent serious complications of uremic state o INDICATIONS for initiation of renal replacement therapy: Pericarditis Progressive neuropathy attributable to uremia Encephalopathy Muscle irritability Anorexia and nausea not ameliorated by protein restriction
You might also like
- Renal Failur E: Mamta Kumari Asst - Prof. Igims-ConDocument51 pagesRenal Failur E: Mamta Kumari Asst - Prof. Igims-ConMamta KumariNo ratings yet
- Disseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandDisseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Renal FailureDocument41 pagesRenal Failure12046No ratings yet
- Diabetic Ketoacidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandDiabetic Ketoacidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Chronic Renal FailureDocument13 pagesChronic Renal FailureAnusha VergheseNo ratings yet
- Chronic Renal FailureDocument14 pagesChronic Renal FailureyazzzNo ratings yet
- Myocardial InfarctionDocument23 pagesMyocardial InfarctionAnelle Umali50% (2)
- Congestive Heart FailureDocument14 pagesCongestive Heart FailureBella Trix PagdangananNo ratings yet
- Chronic Renal FailureDocument46 pagesChronic Renal Failurestepharry08100% (1)
- Deficiency Iron AnemiaDocument9 pagesDeficiency Iron AnemiaNadia Puspita DewiNo ratings yet
- Chronic Renal FailureDocument28 pagesChronic Renal FailuremarshmalouNo ratings yet
- Acute Renal FailureDocument34 pagesAcute Renal Failureaibaloca67% (9)
- 19 Cardiac DisordersDocument51 pages19 Cardiac DisordersChessie Garcia100% (1)
- Spinal Cord InjuryDocument33 pagesSpinal Cord InjuryNi Made Dwiki Andriyani100% (2)
- Peripheral Arterial DisordersDocument98 pagesPeripheral Arterial Disorderspheonixmtbt100% (1)
- MF3 - Ischemic Heart DiseaseDocument28 pagesMF3 - Ischemic Heart DiseaseAnnbe BarteNo ratings yet
- MICU Case Study PresentationDocument55 pagesMICU Case Study Presentationjmarc_21100% (4)
- Heart Muscle Shortness of Breath Tired Swelling of The Legs Heart Failure Irregular Heart Beat Fainting Sudden Cardiac DeathDocument6 pagesHeart Muscle Shortness of Breath Tired Swelling of The Legs Heart Failure Irregular Heart Beat Fainting Sudden Cardiac DeathSachin DwivediNo ratings yet
- Glasgow Coma Scale: - Eye-Opening - Motor - Verbal ResponsesDocument13 pagesGlasgow Coma Scale: - Eye-Opening - Motor - Verbal ResponsesSofianNo ratings yet
- What Is HyperglycemiaDocument7 pagesWhat Is HyperglycemiaFelisa Lacsamana GregorioNo ratings yet
- What Is Hypertensive NephropathyDocument11 pagesWhat Is Hypertensive NephropathyIvy Pamanian DeldaNo ratings yet
- Heart Failure With Preserved Ejection FractionDocument19 pagesHeart Failure With Preserved Ejection Fractioncosmin balanNo ratings yet
- Case Study: Congestive Heart FailureDocument7 pagesCase Study: Congestive Heart FailureXI-E / 21 / MARY TRIANANo ratings yet
- Acute Renal Failure Powerpoint PresentationDocument18 pagesAcute Renal Failure Powerpoint PresentationSteven Paul DaclesNo ratings yet
- CardiomyopathyDocument2 pagesCardiomyopathyBianca SarmientoNo ratings yet
- HemophiliaDocument20 pagesHemophiliaNavirohit GillNo ratings yet
- HypertensionDocument8 pagesHypertensiongilma100% (3)
- SCI (Spinal Cord Injury)Document51 pagesSCI (Spinal Cord Injury)Awal AlfitriNo ratings yet
- Liver CirrhosisDocument2 pagesLiver CirrhosisAzette Agpi100% (3)
- Spinal Cord InjuryDocument47 pagesSpinal Cord InjuryShitaljit IromNo ratings yet
- Myocardial InfarctionDocument18 pagesMyocardial InfarctionYanna Habib-MangotaraNo ratings yet
- Transposition of The Great ArteriesDocument17 pagesTransposition of The Great ArteriesGaram Esther GohNo ratings yet
- Case Study Congestive Heart Failure Patho)Document8 pagesCase Study Congestive Heart Failure Patho)Mj Silva100% (3)
- Syndrome of Inapropriate Antidiuretic Hormone (SIADH)Document15 pagesSyndrome of Inapropriate Antidiuretic Hormone (SIADH)Asrul Rahim100% (1)
- Stroke and Cerebrovascular DiseaseDocument14 pagesStroke and Cerebrovascular DiseaseMarwan M.No ratings yet
- Cardiogenic ShockDocument20 pagesCardiogenic Shockanimesh pandaNo ratings yet
- AsthmaDocument39 pagesAsthmamits98No ratings yet
- Cardiomyopathy: By: P.Dhilip KumarDocument29 pagesCardiomyopathy: By: P.Dhilip Kumarpreet kaur100% (1)
- Gastro Intestinal Bleeding DR - muayAD ABASSDocument59 pagesGastro Intestinal Bleeding DR - muayAD ABASSMAFADHELNo ratings yet
- Hypertrophic CardiomyopathyDocument57 pagesHypertrophic CardiomyopathycynNo ratings yet
- Diabetic Ketoacidosis: Presented by The Students From Roll Numbers 31 - 40Document20 pagesDiabetic Ketoacidosis: Presented by The Students From Roll Numbers 31 - 40HUSSAIN NAZEESHANo ratings yet
- Cardiogenic ShockDocument21 pagesCardiogenic ShockIslamOteshNo ratings yet
- Brief Description: Pleural EffusionDocument3 pagesBrief Description: Pleural EffusionJessica CatacutanNo ratings yet
- 1st, 2nd, 3rd Degree AV BLockDocument8 pages1st, 2nd, 3rd Degree AV BLockladydreamer_92No ratings yet
- Atrial FibrillationDocument24 pagesAtrial FibrillationFani Butt50% (2)
- Myocardial Infarction With ST Segment ElevationDocument27 pagesMyocardial Infarction With ST Segment ElevationRika Yulizah GobelNo ratings yet
- Cardiogenic Shock PDFDocument14 pagesCardiogenic Shock PDFAdreiTheTripleANo ratings yet
- CardiomyopathyDocument17 pagesCardiomyopathysarguss1450% (2)
- Hypovolemic Shock: Dr. Sherwin BuluranDocument8 pagesHypovolemic Shock: Dr. Sherwin BuluranChristian UretaNo ratings yet
- Hemorrhagic Cerebro Vascular DiseaseDocument37 pagesHemorrhagic Cerebro Vascular Diseasejbvaldez100% (1)
- PottsDocument17 pagesPottsdadahjNo ratings yet
- Tricuspid Stenosis (TS)Document8 pagesTricuspid Stenosis (TS)rameshbmcNo ratings yet
- Congestive Heart Failure ReportDocument6 pagesCongestive Heart Failure ReportSunshine_Bacla_4275100% (1)
- Congestive Heart FailureDocument6 pagesCongestive Heart Failureseigelystic100% (1)
- ENCEPHALOPATHYDocument5 pagesENCEPHALOPATHYSepta RinaldyNo ratings yet
- HepatitisDocument8 pagesHepatitisudaybujjiNo ratings yet
- Chronic Kidney DiseaseDocument30 pagesChronic Kidney DiseaseLALITH SAI KNo ratings yet
- Chronic Kidney DiseaseDocument17 pagesChronic Kidney Diseaseniken_rizkiNo ratings yet
- Chronic Kidney Disease. GolwallaDocument8 pagesChronic Kidney Disease. GolwallaAbdul QuyyumNo ratings yet
- Drug De-Addiction Programme (DDAP) Ministry of Health and Family Welfare (MOH&FW), Government of IndiaDocument19 pagesDrug De-Addiction Programme (DDAP) Ministry of Health and Family Welfare (MOH&FW), Government of IndiaHari BabooNo ratings yet
- Articol Metode de ExtractieDocument22 pagesArticol Metode de ExtractieDiana JugănaruNo ratings yet
- MastitisDocument27 pagesMastitisLaprida RecoletaNo ratings yet
- ENLS V4.0 ME Manuscript FINALDocument17 pagesENLS V4.0 ME Manuscript FINALkoko komarudinNo ratings yet
- Rishikesh Seminar Content - SSSOHADocument13 pagesRishikesh Seminar Content - SSSOHARabindra DhitalNo ratings yet
- RO-INMED 2016 ProgramDocument18 pagesRO-INMED 2016 Programmamulasioan9675No ratings yet
- Russian FastingDocument41 pagesRussian FastingTanks A Lot100% (1)
- JIAP July 2011 - Guided Tissue Regeneration - A Decision-Making ModelDocument8 pagesJIAP July 2011 - Guided Tissue Regeneration - A Decision-Making ModelLouis HutahaeanNo ratings yet
- ASD Interventions Theories, Age Range and SettingsDocument4 pagesASD Interventions Theories, Age Range and SettingstracycwNo ratings yet
- Case Studies On DisordersDocument5 pagesCase Studies On DisordersAshwin Hemant LawanghareNo ratings yet
- Status AsthmaticusDocument5 pagesStatus AsthmaticusHimmzNo ratings yet
- HIV Policy MemoDocument3 pagesHIV Policy MemoZhihong XuNo ratings yet
- End of Life Dissertation TopicsDocument8 pagesEnd of Life Dissertation TopicsIWillPayYouToWriteMyPaperCanada100% (1)
- NeutrophilDocument61 pagesNeutrophilJenivic Empig PuedanNo ratings yet
- ArenavirusDocument29 pagesArenavirusRamirez GiovarNo ratings yet
- AppendectomyDocument6 pagesAppendectomyapi-3797941100% (10)
- Glucose-Loesung 5 08-07 03Document2 pagesGlucose-Loesung 5 08-07 03Andreea CaticiNo ratings yet
- Milieu TherapyDocument2 pagesMilieu Therapysivagiri.pNo ratings yet
- Hyperthermia in Cancer Treatment: Cabuy E. Reliable Cancer Therapies. Energy-Based Therapies. 2011 1 (2) :1-48Document48 pagesHyperthermia in Cancer Treatment: Cabuy E. Reliable Cancer Therapies. Energy-Based Therapies. 2011 1 (2) :1-48Eliza LlenzaNo ratings yet
- Adverse Drug Reactions in A ComplementaryDocument8 pagesAdverse Drug Reactions in A Complementaryrr48843No ratings yet
- Carmin WentworthDocument4 pagesCarmin Wentworthapi-356549360No ratings yet
- Infection Control in NurseryDocument6 pagesInfection Control in NurserysobinjohnpklNo ratings yet
- Prasentation Evenlyn Water Management in Germany and Waste Water TreatmentDocument20 pagesPrasentation Evenlyn Water Management in Germany and Waste Water Treatmentashutosh paridaNo ratings yet
- Giraud2013 Obesity and MigraineDocument6 pagesGiraud2013 Obesity and MigraineEcaterina PozdircăNo ratings yet
- Design Manual - Municipal Wastewater DisinfectionDocument264 pagesDesign Manual - Municipal Wastewater DisinfectionPillaca Ugarte Ulises RansesNo ratings yet
- Presentasi Pit Perbani 2000Document16 pagesPresentasi Pit Perbani 2000Meta ParamitaNo ratings yet
- Tugas Mandiri Bahasa Inggris Keperawatan Pertemuan Ke 3 Case 1Document4 pagesTugas Mandiri Bahasa Inggris Keperawatan Pertemuan Ke 3 Case 1IqbaaleNo ratings yet
- IN25 Sensory Overload Induction - PHPDocument3 pagesIN25 Sensory Overload Induction - PHPlucianmateoNo ratings yet
- Oral Preparations: Erdosteine ZertinDocument4 pagesOral Preparations: Erdosteine ZertinmagreaNo ratings yet
- Interferon AlphaDocument22 pagesInterferon AlphaFedri BaysarNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (27)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)