Professional Documents
Culture Documents
Dystocia
Uploaded by
Cylin DaduralOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dystocia
Uploaded by
Cylin DaduralCopyright:
Available Formats
Dystocia (Abnormal Labor)
Dr. Irma Lee
Labor
A series of processes and events that begin with the onset of uterine contractions and end with the expulsion of the products of conception (fetus and placenta). It is characterized by a progressive increase in frequency of contractions (faster) duration of contractions (longer) intensity of contractions (more painful)
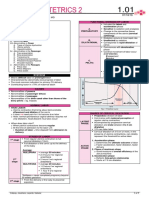
Friedmans Curve Dilatation Curve 1.Latent phase - up to 3-4 cm dilatation ( approximately 8 hours long) 2. Active phase a. Acceleration phase not always present b. Phase of Maximum Slope (PMS) - occurs at approximately 9 cm dilatation - fetus is considered fully descended as it falls one station below the ischial spines c. Deceleration - always present Fetal Descent 1. Latent phase - no fetal descent occurs - extends beyond dilatational phase of descent curve 2. Active phase - comes much later a. Acceleration b. Phase of maximum descent - occurs at around 9 cm dilatation - corresponds to the deceleration of dilatation - fetus fully descended at +1 (station at the level of ischial spines)
Criteria for the Diagnosis of Labor Documented uterine contractions (at least once in 10 minutes, or 4 in 20 minutes). Documentation can be in the form of direct observation or electronically using a cardiotocogram Documented progressive changes in cervical dilation and effacement, as observed by one observer Cervical effacement of greater then 75-80% Cervical dilatation of greater than 3 cm Factors that Affect Labor Powers - uterine contractions Passages pelvis Passenger - fetus Friedmans Curve
Functional Division of Labor Preparatory Division latent phase Dilatational Division active phase - when CERVICAL DILATATION occurs Pelvic Division concerned with descent aspect of delivery Latent Phase of Labor The point at which the mother perceives regular contractions Diagnostic Steps for the Evaluation of Latent Phase of Labor 1. Define the components of latent-phase labor a. Onset b. Interval c. End 1. Describe the antenatal history of the patient 2. Evaluate the pelvis (passage) 3. Evaluate the fetus (passenger) 4. Evaluate the contractions (powers) 5. Evaluate the labor history
WHO Partograph
Factors affecting length of Latent Phase of Labor Cervical dilatation Station of vertex Parity Maternal age Rupture of membranes during latent phase Three Parts of Active Labor A-B Acceleration: slow rate of change or transition from latent to active B-C Maximum slope of acceleration: rapid rate of change C-D Deceleration: A slowing in active phase until molding, descent, or rotation takes place and second stage begins
D
10 9 8 7 6
-5 -4 -3
B A
-2 -1 0 +1 +2 +3 +4
Partograph The active phase of labor commences at 3 cm dilatation The latent phase of labor should not be longer than 8 hours During the active phase, the rate of cervical dilatation should not be slower than 1 cm/ hour A lag time of 4 hrs between slowing of labor and need for intervention is unlikely to compromise the fetus and mother and avoids unnecessary intervention
5 4 3 2 1 0 1 2 3
10
+5
Protraction < 1 cm / hr cervical dilatation for a minimum of 4 hours
Protraction and Arrest of Cervical Dilatation
End of Active Phase
Protracted activephase dilatation
Nullipara Maximum slope of dilatation of 1.2cm/hr or less Deceleration phase duration of 3 hours or more Cessation of activephase for 2 hours or more
Multipara Maximum slope of 1.5cm/hr or less
10 9 8 7
C
End of latent phase
-5 -4 -3
B
Maximum Slope
-2 -1 0 +1 +2
Prolonged deceleration phase
Deceleration phase of 1 hr or more
6 5 4 3 2 1 0 1 2 3 4
Secondary arrest of dilatation
Latent Phase
5 6 7 8 9 10
+3 +4 +5
Pelvic Stations 3 pelvic stations -3 -2 -1 0 1 2 3 5 pelvic stations -5 -4 -3 -2 -1 0 1 2 3 4 5
PROLONGED LATENT PHASE
10 -5 -4 -3 -2 -1 0 +1 +2 +3 +4 +5 3 6 9 12 15 18 21 24 27
Pelvic Inlet
9 8 7 6
Ischial Spines (engagement)
5 4 3 2
On the perineum (vertex in view w/ cxn)
1 0
Abnormalities of Descent Nullipara Protraction <1cm dilatation change/hr No change in dilatation in an hour Multipara <2cm dilatation change/hr No change in dilatation in 30 minutes
PROTRACTED ACTIVE PHASE OF DILATATION
10 9 8 7 6 5 4 3 2 +3 1 0 1 2 3 4 5 6 7 8 9 10 +4 +5 -5 -4 -3 -2 -1 0 +1 +2
Arrest
Second Stage of Labor Definitions Failed No descent is noted from the time the patient is first examined
Protraction (2nd Stage)
Nullipara: Descent <1 cm,/hr Multipara: Descent <2cm/hr
Arrest (2nd Stage)
No change after descent has begun
10
PROTRACTED DESCENT
-5 -4 -3 -2 -1 0 +1 +2 +3 +4 +5 1 2 3 4 5 6 7 8 9 10 9 8 7
Nullipara: 1 hour Multipara: 30 minutes
Labor Diagnosis Term
Prolonged latent phase
Criteria
Nulliparas >20 hours Multiparas >14 hours
5 4 3 2 1 0
Protracted active-phase dilatation
Nulliparas <1.2cm/hour Multiparas <1.5cmhour
Arrest of dilatation Protracted descent
No progress for 2 hours Nulliparas <1 cm/hour Multiparas <2cm/hour
Arrest in descent
No progress for 1 hour
PROLONGED DECELERATION PHASE
10 9 8 7 6 5 4 3 2 1 0 1 2 3 4 5 6 7 8 9 10 -5 -4 -3 -2 -1 0 +1 +2 +3 +4 +5
Fetal effects Caput succedaneum Fetal head molding
ARREST IN CERVICAL DILATATION
10 9 8 7 6 5 4 3 2 1 0 1 2 3 4 5 6 7 8 9 10
ROT ROT ROT
-5 -4 -3 -2 -1 0 +1 +2 +3 +4 +5
Shoulder Dystocia Disproportion between the fetal bisacromial diameter and the AP diameter of the pelvic inlet. Incidence: 0.2 3.0% of all vaginal deliveries Risk of Recurrence:11.9 16.7 % Risk Factors: Antepartum Fetal macrosomia increased in body size relative to head size Advanced maternal age Diabetes Mellitus Maternal Obesity Post-term pregnancy Excessive maternal weight gain Prior shoulder dystocia Platypelloid or convergent pelvis Intrapartum Prolonged second stage of labor without descent Oxytocin use Midpelvic delivery Overzealous external rotation of the fetal head by the operator Deliveries on bed Excessive fundal pressure Diabetes Mellitus 70% Increase overall risk for shoulder dystocia Author Increase in Risk Associated with Diabetic Status Rate ratio 5.2 Odds ratio 4,3; 95% CI 2.2 8.3 Relative risk <4,000g 2.6; 95% CI 1.29-5.34 Relative risk >4,000g 3.6; 95% CI 2.37-4.76 Relative risk 6.5; 95% CI 1.5-27.1
ARREST OF DESCENT
10 9 8 7 6 5 4 3 2 1 0 1 2 3 4 5 6 7 8 9 10 -5 -4 -3 -2 -1 0 +1 +2 +3 +4 +5
Acker et al 1985 Bahar 1996
Langer et al 1991
Sandmire et al 1988
Birth Weight In relation to Birth Weight and Diabetic Status Birth Weight (g) Women Without Diabetes (%) 0.1 1.1 1.1 10.0 4.1 22.6 BW > 4000 g PPV of 3.3% EFW by UTZ Sensitivity: 22-44% PPV: 30-44% Fetal Abdominal Circumference: > 35 cm (MACROSOMIA) BW > 4500 g PPV 9% Macrosomia index = chest diameter BPD = 1.4 cm (critical for vaginal delivery) Sonographic Predictors for Shoulder Dystocia Women With Diabetes (%) 0.6 3.7 4.9 23.1 20.0 50.0
<4,000
FAILURE OF DESCENT
10 9 8 7 6 5 4 3 2 1 0 1 2 3 4 5 6 7 8 9 10 -5 -4 -3 -2 -1 0 +1 +2 +3 +4 +5
4,000-4,449 > 4,500
Maternal-Fetal Effects of Dystocia Maternal effects Intrapartum infection Uterine rupture Pathologic retraction ring Fistula formation Pelvic floor injury Postpartum lower extremity nerve injuryss
Chest to head difference Shoulder to head difference Shoulder circumference Abdominal to BPD difference
1.4cm 4.8cm 40.9cm 2.6cm
CT Scan Shoulder measurement >14 cm predicts birth weight >4200 gms 100% sensitivity 87% specificity 78% PPV 100% NPV * Head to body delivery interval 24 secs. * Shoulder Dystocia >60 secs Shoulder Dystocia: Indicators Turtle sign Retraction of the fetal head against maternal perineum No spontaneous external rotation Downward traction does not deliver the anterior shoulder Multiple risk factors Sonographic features
Fractures Claviicular (10%) Humerus (5%) Prolonged head-shoulder interval (10.6 3.0 vs 4.3 0.7, P=0.03) Head-shoulder interval >7mins. 65% sensitivity 74% specificity
BRAIN INJURY Maternal Complications PPH ( Large Baby, Prolong Labor) Genital Tract Lacerations Cervical Tears, Bladder Atony, Uterine Rupture
* No clinical or theoretical data to support that elective cesarean section will prevent shoulder dystocia and avoid brachial plexus injury ACOG Guidelines Planned CS for suspected macrosomia in the general population is not reasonable Planned CS may be reasonable for diabetic pregnant women with EFW >4200 gms-4500 gms Risk factors alone or in combination lacks accuracy to predict SD Ultrasound to estimate macrosomia has limited accuracy
Cardinal Movements of Labor
Goals in Management Maximize safe delivery Shorten the time from delivery of the head to delivery of the body ACOG Proposed Management Protocol Assistance from anesthesia, pediatrics, and obstetrics Gentle attempt at traction assisted by maternal expulsive efforts Generous episiotomy Suprapubic pressure Dont apply it directly downward Apply it to an angle towards the fetal chest Lateral application from either sides of the maternal abdomen Alternating between sides (rocking pressure)
Pathophysiology Persistent Anterior-Posterior of fetal shoulders at the pelvic brim (fetal macrosomia, precipitous labor). Failure of internal rotation of the bisacromial diameter at the midpelvis. Impaction of posterior fetal shoulder on sacral promontory.
Unilateral shoulder dystocia
Bilateral shoulder dystocia
Complications Associated w/ Shoulder Dystocia Fetal complications Asphyxia Brain Damage. Perinatal Death (20-25%) Brachial plexus injury (17%) C5 - C6 Erbs Palsy C7 - C8 Klumpkes Palsy
McRoberts maneuver Benefits: The maternal sacrum is flattened in relation to the lumbar spine Cephalad rotation of the symphysis pubis leads to: Reduction in pelvic inclination from 26 to 0 Increases the size of posterior outlet May unlock the anterior shoulder Increases the intraabdominal pressure by 97% amplitude of the uterine contraction Easy, simple and effective technique Success rate = 42% If combined with episiotomy and suprapubic pressure=54.2%
Rubins maneuver (reverse of Woods) The pressure is applied to the posterior surface of the most accesible part of fetal shoulder (either the anterior or posterior shoulder) to effect shoulder abduction.
How does Mc Roberts Maneuver works Change the angle by flattening the sacrum in relation to the maternal spine and elevate SP. Enhances intrauterine pressure and amplitude of uterine contractions. Rotation of anterior shoulder Woods corkscrew maneuver Progressive rotations of shoulder girdle in a corkscrew fashion by continuous pressure on anterior surface of the posterior shoulder together with downward thrust of the left hand on the buttocks of the baby. Rotation of the posterior shoulder to anterior through 180 arch clockwise
Cephalic Replacement (ZAVANELLI MANEUVER) Return head to OA and flex and push cephalad, once replaced, hold at station 0 Give 0.25 mg terbutaline SC or general anesthesia prior to maneuver. Time of CS dictated by fetal condition
Controversial Methods Symphysiotomy Posterior arm extraction (Barum Maneuver) To do posterior arm delivery, pressure should be applied on the antecubital fossa in order to flex the fetal forearm and then pull across the chest and face until it is outside the vagina
Cleidotomy- cut clavicle, usually used on dead fetus
Clavicular fracture
Other methods: Cephalic replacement Abdominal rescue
Fundal pressure All fours (Gaskin maneuver) The patient is rolled from her existing position into her hands and knees Benefits: Downward force of gravity Favorable change in pelvic diameters
After Vaginal delivery Exploration of the uterus, vagina and cervix for lacerations Check whether the episiotomy has extended into the rectum Check for the presence of hematomas: cervix, vagina and broad ligament Explore the uterus for rupture Rate and Risk Factors for Recurrent Shoulder dystocia
Pelvic Inlet
Midpelvis Author Vaginal SD Deliveries Subsequent Recurrent SD Risk Factors Vaginal for Deliveries Recurrent SD
Fetal weight Maternal parity
AP Diameter Anatomic/True= 11 cm Obstetric (most critical)= 10 cm Diagonal= 12 cm APMP = 11.5 cm Ischial spine Sidewalls Curvature sacrum 9.5 to 11.5 cm
Transverse Diameter Transverse Diameter of the inlet= 13cm
Pelvic Outlet
Ginsberg 39,681
602(1.5%) 66 (10.9%) 11 (16.7%)
Arch of pubis Lewis 37,465 747(2%) 101(13.5%) 17(13.8%)
Pre-pregnancy weight Weight at delivery Time of second stage of labor Fetal weight that of index pregnancy Fetal weight that of index pregnancy
Biischial/interischial= 10 cm Not prominent divergent More curved Biiscial tuberosity/intertuberous= >8 cm (mans fist) Wide (>90)
Mueller Hillis Maneuver Hands on cervix, while pushing uterine fundus down To know extent of descent Station 0: engaged Station -2: 2 cm above ischial spine Staion +2: 2cm below ischial spine Station -5: head floating above symphysis pubis Deceleration phase of 1st stage of labor Engagement: occurs later in multigravid Descent Flexion Internal rotation External rotation Note: Primigravid: usu descent first before active cxn Multigravid: cxn first before descent Asses Fetal size If mom is Diabetic or obese, a possibility of Fetal macrosomia -> risk shoulder dystocia Breech- can be delivered vaginaly
Smith
34,800
203(0.58%) 42 (20.6%) 5 (11.9%)
Conclusion No reliable and accurate predictors for SD Ultrasound for estimation of macrosomia has limited accuracy Planned CS for EFW >4200-4500 gms Early suspicion and logical sequence of maneuvers to lessen brachial plexus injury No Maneuver that is superior to release impacted shoulder Periodic review of maneuvers Summary Early recognition Initial adequate efficient treatment (mental drill) Stop the patient from pushing Stop fundal pressure Call for help Experienced OB Pediatrician Anesthesiologist Paramedics If there is nuchal cord, reduce Do the following: Anesthesia Empty the bladder Generous episiotomy Mac Roberts Suprapubic pressure Success rate 58%
Footling: Caesarian Section unless baby is small Single Double
Cervical dilatation Descent Stage 1 Stage 2 Stage 3
Primigravida 1.2 cm/hr 1 cm/hr 8 hrs 30 mins 20 mins
Multigravida 1.5 cm/hr 2 cm/hr 5 hrs 15 mins 5 mins
ADDITIONAL Notes from our Discussion 3 Factors Affecting Labor 1. Power uterine cxn for cervix to dilate 2. Passage- pelvic inlet and outlet 3. Passenger- size and presentation of fetus Blood Supply: uterine artery (uterus, Cervix) : ovarian artery: (ovary, distal FT) Diagonal Conjugate - only one measured clinically - measured from the lower border of symphysis pubis to the midpoint of the sacral promontory - if < 11.5: shortened/inadequate
Post term pregnancy (42 weeks) Induced Labor Bishops Score - Effective if > 6 Dilatation Effacement Position Consistency of uterus Gravida Augmented Labor Uterotonic Oxytocin IV (10 U in 1L NSS) 1st stage of labor: beginning dilatation-full dilatation (10cm) Latent Phase Cervix <3-4cm Uterine cxn may be present Affected by sedation (EPIDURAL) Active Phase: > 3-4cm Acceleration phase Outcome of labor Not alwas present Phase of maximum slope Rapid dilatation Efficiency of uterus
Rapid descent of fetus- 7-8 cm start descent fetal head May dilate to @ 9 cm Fetus considered descended if falls 1 cm below ischial spine (occiput anterior) Deceleration phase Fetopelvic relationship Always present (10 cm) Primi: 1 hr Multi: 30 mins Note: Prolonged latent phase Primi: > 20 hours Multi: >14 hrs Arrest for dilatation Most common No change in 2 hrs Usual cause: contracted pelvis
Hypotonic Less pressure Goes back to baseline Both are ineffective -> never lead vaginal delivery Cant dilate cervix Both can be given Oxytocin: to make cxn regular
Note:
Functional Division Preparatory: latent and acceleration phase Dilatational phase: phase of max slope Pelvic phase: deceleration phase to 1st hour after full dilatation : concern w/ descent aspect of delivery : head on perineal wall Prolonged labor: > 20 hours Irregular cxn: send Px home PROM: admit px Labor
Shoulder Dystocia Risk Factors Obesity DM Excessive weight gain Multiparity Postdatism Previous delivery of LGA Fetal Macrosomia (LGA: > 4500g) *External Rotation: bisacromial diameter of shoulder: parallel to AP diameter of symphysis pubis Indications Turtle sign - Cephalad retraction - Due to obstruction of shoulder because of wide bisacromial diameter/ anterior shoulder is above the sacral promontory (normally, it should go under the sacral promontory) - Should expel the baby in 60 sec If not may lead to hypoxia -> ASPHYXIA AND CEREBRAL PALSY
Frequency of cxn ( faster) Intensity of cxn (more painful) Duration of cxn (longer) Interval Peak= frequency
Cardiotopographic graph/ Labor admission test 1. Measure frequency 2. Classify if: a. Mild: indent abdominal wall b. Moderate c. Strong: skin abdominal wall cant be indented 3. Intensity (peak-baseline): Montevideo units in 10 min Should not be <180 for it to be effective Criteria for true labor 1. Uterine cxn At least 1 in 10 mins or 4 in 20 mins 2. Progressive change in cervical dilatation & effacement 3. Cervical effacement 75-80% 4. Cervical dilatation >3 cm Normal length cervix: 1 inch (2.54 cm) Fully effaced: paper thin Ripe cervix: midline in position, dilatable WHO partograph 1cm.hr dilatation 4 hours difference from alert line to action line Latent time of 4 hrs b/w slowing of labor & need for intervention is unlikely to compromise the fetus and mom ( avoids unnecessary intervention) Active phase commences at 3cm Latent phase shud not be longer than 8 hours During active phase, rate dilatation should not be slower than 1 cm/hr Uterine Cxns Hypertonic Sustaine cxn Period of relaxation very short Above the baseline Best to sedate px: to decrease anxiety 10 mg Nalbuphine HCL IV 100mg Meperidine IM
Other Complications: Brachial plexus injury Clavicular fracture Humerus fracture Increase fetal morbidity and mortality Mom Uterine rupture: prolonged labor, LGA Uterine atony: PPH : prolonged labor, LGA Birth canal injuries: especially if low forceps extraction Fistula formation: b/w 2 viscus Rectovaginal: assoc w/ operations/maneuvers in vagina Vesicovaginal Urethrovaginal Before doing procedure, empty bladder Repair: 6 weeks post delivery esp. vesicovaginal Can give antimicrobial tx Prognosis related to Fetal Macrosomia Increased perinatal loss Infants severely depressed at birth Neurological complications High infant mortality befor age 7 Note:
Contracted pelvis: absolute indication CS Elective surgery: unethical, bec of increase risk for mom & baby
Maneuvers 1. Mc Roberts Least traumatic to the mom esp if done w/ clavicular fracture CALL FOR HELP FIRST First procedure to increase outlet diameter (questionable) Flex thigh mom upto abdomen Feet on stirrups straightens the spine (lift symphysis pubis) : increase outlet diameter Rubins Push scapula baby towards chest (anterior rotation) Anterior shoulder counterclockwise Thrust on armpit -> grasp humerus -> swing it anteriorly
2.
3.
4.
5.
6. 7. 8.
9.
Woods corkscrew Push shoulder by pushing anterior surface of the posterior shoulder (posterior rotation) and dislodge posterior shoulder anteriorly clockwise direction Zavanelli Super hard Flex the shoulder Push the baby inside again ( doing internal rotation) Reposition the baby After repositioning: do CS Complication: chance to rupture Puerperal infection Gaskin Mom upside down kneeling, palms on floor twist baby towards his/her anterior surface Symphysiotomy put xylocaine, then cut symphysis pubis Duhrseen Cut the cervix to make it big Chavis Shoulder horn instrument w/ concave blade w/ long handle, is slipped b/w symphsis pubis and impacted anterior shoulder Hibbard Pressure applied at infants jaw and neck in the direction of the moms rectum, w/ strong fundal pressure applied by an assistant as the anterior shoulder is freed Complication: if fundal pressure applied at a wrong time -> fetal orthopaedic and neurologic damage
Epidural anesthesia best anesthesia in labor to alleviate pain to assist us in doing procedures for shoulder dystocia Bupivacaine
Transcribe by: Cecil Ong Notes from: Cecil Ong Lea Oiga Mae Olivares Argelyn Ong Emy Onishi
Cecil Ong Emy Onishi Mitzel Mata Fred Monteverde Regina Luz Lala Nieto Mae Olivares SEC C 2009 !
You might also like
- RISE REVIEW - Female Reproductive SystemDocument9 pagesRISE REVIEW - Female Reproductive SystemGerben Villanueva100% (1)
- Abnormal Labor and Dystocia Causes, Evaluation and ManagementDocument63 pagesAbnormal Labor and Dystocia Causes, Evaluation and ManagementJoan LuisNo ratings yet
- OB 1.01 DystociaDocument9 pagesOB 1.01 DystociaRaquel Reyes100% (1)
- POGS PB Dystocia Sept 2022Document6 pagesPOGS PB Dystocia Sept 2022John Piox Badiang100% (1)
- psc006 PDFDocument2 pagespsc006 PDFPHitphitt Jeleck SangaattNo ratings yet
- Name: Year & Course: Test Type Timing Process ResultsDocument3 pagesName: Year & Course: Test Type Timing Process ResultsAllyah Anthonette Ferwelo100% (1)
- Normal Conduct of LaborDocument62 pagesNormal Conduct of LaborFaye Cabotaje LinganNo ratings yet
- OB - CPG HTN in Pregnancy BEADocument138 pagesOB - CPG HTN in Pregnancy BEAEllieAdlerNo ratings yet
- Fetal MonitoringDocument6 pagesFetal MonitoringRraouzmaaliNo ratings yet
- gtg60 Cervicalcerclage PDFDocument21 pagesgtg60 Cervicalcerclage PDFLijoeliyas100% (1)
- OB 1.01 DystociaDocument7 pagesOB 1.01 DystociaDan Paolo Diña SolayaoNo ratings yet
- Global Strategy For Asthma Management and Prevention: OR DistributeDocument211 pagesGlobal Strategy For Asthma Management and Prevention: OR DistributeHenny Rahmawati100% (1)
- Post Partum Haem.Document90 pagesPost Partum Haem.rachael annorNo ratings yet
- Forceps Delivery For Gravidocardiac PatientsDocument80 pagesForceps Delivery For Gravidocardiac PatientsTots A. Macahilo-LayawonNo ratings yet
- Philippine CPG-2013-uti in Adults-Part1 PDFDocument82 pagesPhilippine CPG-2013-uti in Adults-Part1 PDFVirginia AbalosNo ratings yet
- 002 Intrapartum Fetal Heart Rate Monitoring 3a - ACOG Bulletin 106 PDFDocument11 pages002 Intrapartum Fetal Heart Rate Monitoring 3a - ACOG Bulletin 106 PDFale_fearNo ratings yet
- Management of CA Vulva 2Document33 pagesManagement of CA Vulva 2api-3705046No ratings yet
- CPG Uterine InversionDocument3 pagesCPG Uterine InversionRahmayanti YuliaNo ratings yet
- Benign and Malignant Ovarian Tumors: Case 1Document14 pagesBenign and Malignant Ovarian Tumors: Case 1Charrie RagadiNo ratings yet
- Breech - Management Of: 1. PurposeDocument15 pagesBreech - Management Of: 1. PurposeMuathNo ratings yet
- Obstetrics - Operative Vaginal DeliveryDocument5 pagesObstetrics - Operative Vaginal DeliveryJonathanNo ratings yet
- CC C C: June 8, 2011 By: Santos, Edilberto DBDocument63 pagesCC C C: June 8, 2011 By: Santos, Edilberto DBHakugeiNo ratings yet
- Planes and Diameters of The PelvisDocument32 pagesPlanes and Diameters of The PelvisRumelle ReyesNo ratings yet
- OSCE Revision OBG DocumentDocument60 pagesOSCE Revision OBG DocumentshreyaNo ratings yet
- Operative Vaginal DeliveryDocument6 pagesOperative Vaginal DeliveryCT Johara MusorNo ratings yet
- ACOG Management of Stillbirth PDFDocument14 pagesACOG Management of Stillbirth PDFLêMinhĐứcNo ratings yet
- Cholestatic Disease in PregnancyDocument25 pagesCholestatic Disease in Pregnancyarifbotwin100% (1)
- Abnormal Labor Guide: Dystocia, Causes, and ManagementDocument20 pagesAbnormal Labor Guide: Dystocia, Causes, and ManagementAiszel Angeli Pepito LigoNo ratings yet
- Hypertension in PregnancyDocument34 pagesHypertension in PregnancyMusekhirNo ratings yet
- Operative Vaginal Delivery PDFDocument56 pagesOperative Vaginal Delivery PDFFarehan Md IsaNo ratings yet
- ResucNeonatBasica OMSDocument65 pagesResucNeonatBasica OMSAsPonceMichNo ratings yet
- Operative ObstetricsDocument4 pagesOperative Obstetricssarguss14100% (3)
- Abruptio Placentae: Insert or Drag & Drop Your PhotoDocument42 pagesAbruptio Placentae: Insert or Drag & Drop Your PhotoClareen JuanicoNo ratings yet
- Miscarriage Early Pregnancy LossDocument10 pagesMiscarriage Early Pregnancy LossiwennieNo ratings yet
- Preterm Prelabour Rupture of MembranesDocument12 pagesPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanNo ratings yet
- Hypertension in Pregnancy: N.L. Meyer, M.DDocument52 pagesHypertension in Pregnancy: N.L. Meyer, M.DnushadNo ratings yet
- Benign Disease of The UterusDocument27 pagesBenign Disease of The UterusnyangaraNo ratings yet
- (OBS) 3.08b Sexually Transmitted Diseases in Pregnancy - Bongala (Nov 30)Document18 pages(OBS) 3.08b Sexually Transmitted Diseases in Pregnancy - Bongala (Nov 30)Gerben VillanuevaNo ratings yet
- Antepartum HaemorrhageDocument7 pagesAntepartum HaemorrhageYerra SukumalaNo ratings yet
- 1 GYNE 3 - History, PE, Prevention Interaction of Disease and PhysiologyDocument6 pages1 GYNE 3 - History, PE, Prevention Interaction of Disease and PhysiologyIrene FranzNo ratings yet
- Molar PregnancyDocument14 pagesMolar Pregnancyfardeal_mckk100% (1)
- History and Pe ObgynDocument4 pagesHistory and Pe ObgynCara Marrero IguidNo ratings yet
- Hypertension in PregnancyDocument20 pagesHypertension in PregnancyFAMED RESIDENTS CESMED100% (1)
- Prenatal Care 2Document3 pagesPrenatal Care 2Joan Rose Rendon-HungNo ratings yet
- Obstetric Summm 1Document46 pagesObstetric Summm 1ملك عيسىNo ratings yet
- Induction of Labour Techniq SADocument18 pagesInduction of Labour Techniq SAPujanaWiaktaNo ratings yet
- Ob SGDDocument88 pagesOb SGDFerdinand Luis SuarezNo ratings yet
- Pelvic Inflammatory DiseaseDocument6 pagesPelvic Inflammatory DiseaseJoel Tito100% (1)
- OB Evals 1Document28 pagesOB Evals 1Zelle Pamplona RamosNo ratings yet
- Clinical Packet OBDocument7 pagesClinical Packet OBLiza Jean BakerNo ratings yet
- StratOG Vaginal BreechDocument17 pagesStratOG Vaginal BreechNalin AbeysingheNo ratings yet
- University of Gondar College of Medicine and Health ScienceDocument100 pagesUniversity of Gondar College of Medicine and Health ScienceCHALIE MEQUNo ratings yet
- OB TriageDocument11 pagesOB TriageRuchi Jhoom PatelNo ratings yet
- Gynecological History Taking and ExaminationDocument17 pagesGynecological History Taking and Examinationnmsiswaridewi100% (1)
- 2023 OB/GYN Coding Manual: Components of Correct CodingFrom Everand2023 OB/GYN Coding Manual: Components of Correct CodingNo ratings yet
- Handbook of Current and Novel Protocols for the Treatment of InfertilityFrom EverandHandbook of Current and Novel Protocols for the Treatment of InfertilityMichael H. DahanNo ratings yet
- PROLOG: Obstetrics, Ninth Edition (Assessment & Critique)From EverandPROLOG: Obstetrics, Ninth Edition (Assessment & Critique)No ratings yet
- Dewhurst's Textbook of Obstetrics & GynaecologyFrom EverandDewhurst's Textbook of Obstetrics & GynaecologyChristoph LeesRating: 2 out of 5 stars2/5 (1)
- Abortion and Sterilization: Medical and Social AspectsFrom EverandAbortion and Sterilization: Medical and Social AspectsJane E. HodgsonNo ratings yet
- Role of Dietary Fibers and Nutraceuticals in Preventing DiseasesFrom EverandRole of Dietary Fibers and Nutraceuticals in Preventing DiseasesRating: 5 out of 5 stars5/5 (1)
- Antenatal Care SheetDocument11 pagesAntenatal Care SheetRaveena100% (1)
- IGCSE Science WorksheetsDocument103 pagesIGCSE Science WorksheetsYoshua Yanottama89% (9)
- CH 2 - Maternal AnatomyDocument8 pagesCH 2 - Maternal AnatomyRandom CommenterNo ratings yet
- Human Reproduction - II Puc - Regular NotesDocument23 pagesHuman Reproduction - II Puc - Regular NotesVasudevNo ratings yet
- Anatomy and Physiology of Female Reproductive SystemDocument42 pagesAnatomy and Physiology of Female Reproductive SystemLiangkiuwiliuNo ratings yet
- Maternal Child Nursing ModuleDocument7 pagesMaternal Child Nursing ModuleWizzardNo ratings yet
- Transverse and Unstable LieDocument31 pagesTransverse and Unstable LieRose Ann GonzalesNo ratings yet
- Hypermobile Ehlers Danlos Syndrome Is A Determinant of FetalDocument8 pagesHypermobile Ehlers Danlos Syndrome Is A Determinant of FetaljoanaclemNo ratings yet
- MCN FINALS MergedDocument193 pagesMCN FINALS MergedNeru RoriNo ratings yet
- Care of Mother, Childbirth & Labor ProcessesDocument13 pagesCare of Mother, Childbirth & Labor ProcessesBardiaga JmayNo ratings yet
- OSCE Gynae-OSCE-MMSSDocument24 pagesOSCE Gynae-OSCE-MMSSMohammad Saifullah100% (1)
- Science 10 Module 2 Version 3 1Document17 pagesScience 10 Module 2 Version 3 1Skyler MontalvoNo ratings yet
- University of Shendi Faculty of Medicine and Surgery OSCE GuideDocument35 pagesUniversity of Shendi Faculty of Medicine and Surgery OSCE GuideYassin Jamal67% (3)
- Agesta Sacred Codes ListDocument22 pagesAgesta Sacred Codes Listmimigogo92% (12)
- Physiology of Cesarean DeliveryDocument4 pagesPhysiology of Cesarean DeliveryDante SalesNo ratings yet
- Uterine Inversion Case AnalysisDocument3 pagesUterine Inversion Case AnalysisDivina Gracia Vibal CieloNo ratings yet
- 208-230 CH08 Lowdermilk - QXDDocument23 pages208-230 CH08 Lowdermilk - QXDSyarifah Ro'fahNo ratings yet
- Romania Fact SheetDocument2 pagesRomania Fact SheetEmeseDengNo ratings yet
- Lecture Learning Objectives for BIO 210 SystemsDocument14 pagesLecture Learning Objectives for BIO 210 SystemsAmber DavisNo ratings yet
- Bulacan Medical Center Post-Operative Obstetric Ward Ectopic Pregnancy Case StudyDocument36 pagesBulacan Medical Center Post-Operative Obstetric Ward Ectopic Pregnancy Case StudyJohn Robert PescadorNo ratings yet
- Final MCNDocument3 pagesFinal MCNKyla R. PinedaNo ratings yet
- Spaying Your DogDocument10 pagesSpaying Your Dogjmw5250No ratings yet
- Human Reproduction: Points To RememberDocument9 pagesHuman Reproduction: Points To RememberPREM277272No ratings yet
- LACERATION - Large Laceration Can Be VAGINAL Laceration - Easier To Locate andDocument2 pagesLACERATION - Large Laceration Can Be VAGINAL Laceration - Easier To Locate andرجمه ديوانNo ratings yet
- Fundamental Nursing LabDocument15 pagesFundamental Nursing LabDev0% (1)
- Vacuum Extraction Is An Artificial LaborDocument6 pagesVacuum Extraction Is An Artificial LaborYuriko_L7No ratings yet
- Nursing Care Plan Placenta PreviaDocument2 pagesNursing Care Plan Placenta PreviaApril Ann HortilanoNo ratings yet
- Incomplete AbortionDocument2 pagesIncomplete AbortionKEn PilapilNo ratings yet
- High Risk Pregnancy 1Document205 pagesHigh Risk Pregnancy 1Vanessa Angel Bugarin100% (3)
- 5.case Presentation On Puerperial SepsisDocument38 pages5.case Presentation On Puerperial SepsisAngela Jolhnem Langhu91% (23)