Professional Documents
Culture Documents
The Role of Pulmonary Resection in Small Cell Lung Cancer
Uploaded by
Ajay TejwaniOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Role of Pulmonary Resection in Small Cell Lung Cancer
Uploaded by
Ajay TejwaniCopyright:
Available Formats
PULMONARY RESECTION IN SMALL CELL LUNG CANCER
ORIGINAL ARTICLE
The Role of Pulmonary Resection in Small Cell Lung Cancer
VIDHAN CHANDRA, MD; MARK S. ALLEN, MD; FRANCIS C. NICHOLS III, MD; CLAUDE DESCHAMPS, MD; STEPHEN D. CASSIVI, MD; AND PETER C. PAIROLERO, MD
OBJECTIVE: To analyze the outcome of surgical resection for patients with small cell lung cancer (SCLC). PATIENTS AND METHODS: We identified all patients who underwent thoracotomy for SCLC at our institution from January 1985 to July 2002. All patients were staged using the American Joint Committee on Cancer TNM system. RESULTS: The median age of the 77 patients (44 men and 33 women) was 65 years (range, 35-85 years). Operations performed included thoracotomy with biopsy of hilar mass in 10 patients, wedge excision in 30 (6 with talc pleurodesis), segmentectomy in 4, lobectomy in 28, bilobectomy in 3, and pneumonectomy in 2. Mediastinal lymphadenectomy was performed in 50 patients and lymph node sampling in 19. Postoperative therapy included chemotherapy alone in 20 patients, radiation therapy in 3, and combined chemotherapy and radiation therapy in 40. Median tumor diameter was 4 cm (range, 1.0-10.0 cm). Postsurgical tumor stage was IA in 7 patients, IB in 11, IIA in 8, IIB in 7, IIIA in 30, IIIB in 10, and IV in 4. A total of 19 patients (25%) had complications: atrial arrhythmia in 7 patients, pneumonia in 6, prolonged air leak in 3, and myocardial infarction, postoperative bleeding, and cerebrovascular accident in 1 each. Operative mortality was 3% (2/ 77). Follow-up ranged from 4 days to 170 months (median, 19 months). At last follow-up, 20 patients were alive. The estimated overall 5-year survival was 27% when excluding the 10 patients who underwent a biopsy without additional surgery. Five-year survival for stage I and II combined (n=33) was 38% compared with only 16% for stage III and IV combined (n=34) (P=.02). Overall median survival was 24 months; median survival for patients who underwent curative surgery was 25 months compared with 16 months for those who had a palliative procedure (P=.34). CONCLUSION: Pulmonary resection in patients with stage I or stage II SCLC is safe with low mortality and morbidity. Curative resection is associated with long-term survival in early stage SCLC in some patients and should be considered in selected patients.
of tumor relapse is local recurrence.1 This has led to a renewed interest in the role of surgical resection to obtain better local control. The purpose of this study was to evaluate postoperative outcome in a group of patients with SCLC who underwent surgery. PATIENTS AND METHODS All patients who underwent thoracotomy with or without pulmonary resection for SCLC at Mayo Clinic in Rochester, Minn, from January 1985 to July 2002 were retrospectively reviewed. Preoperatively, histories were taken; all patients underwent physical examination, electrocardiography, chest radiography, and computed tomography of the chest and upper abdomen; and a complete blood cell count, liver chemistries, and serum creatinine levels were obtained. Diagnosis was established by histologic examination of the resected specimen. Patients were classified using the TNM staging system according to the criteria established by the American Joint Committee for Cancer Staging and End-Results Reporting for non-SCLC.2 Operative mortality was defined as death within 30 days of operation or during the same hospitalization. The time of thoracotomy was used as the starting date. Survival for all living patients was recorded up to June 31, 2003. The length of survival was determined for all patients who died. Survival was estimated using the Kaplan-Meier method.3 The effects of potential risk factors including age, sex, symptoms, smoking more than 40-pack-years, preoperative therapy, postoperative therapy, stage, extent of surgical procedure, lymphadenectomy, tumor location, and postoperative complications on survival were evaluated using log-rank tests.4 To evaluate the joint effects of potential risk factors on survival, Cox5 proportional hazards regression was used. Stepwise variable selection was used to identify risk factors for inclusion in the model. All statistical tests were 2-sided, and the threshold of significance was 0.05. The analysis was conducted using SAS version 8.2 (SAS Institute Inc, Cary, NC). The Mayo Foundation Institutional Review Board approved this study. RESULTS The study group consisted of 77 patients (44 men and 33 women). The median age at the time of thoracotomy was
www.mayoclinicproceedings.com 619
Mayo Clin Proc. 2006;81(5):619-624
mall cell lung cancer (SCLC) is a virulent disease with a high metastatic potential. It is usually considered a systemic disease at presentation and therefore treated with chemotherapy, either alone or in combination with radiation therapy. Although the combination of chemotherapy and radiation therapy is associated with a good clinical response, long-term survival is poor. The most frequent site
From the Department of Surgery (V.C.) and Division of General Thoracic Surgery (M.S.A., F.C.N., C.D., S.D.C., P.C.P.), Mayo Clinic College of Medicine, Rochester, Minn. Dr Chandra is now with the University of Alabama, Birmingham. Presented at the American College of Chest Physicians 70th Annual International Scientific Assembly, Seattle, Wash, October 26, 2004. Individual reprints of this article are not available. Address correspondence to Mark S. Allen, MD, Department of Surgery, Mayo Clinic College of Medicine, 200 First St SW, Rochester, MN 55905 (e-mail: allen.mark@mayo.edu). 2006 Mayo Foundation for Medical Education and Research
Mayo Clin Proc.
May 2006;81(5):619-624
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
PULMONARY RESECTION IN SMALL CELL LUNG CANCER
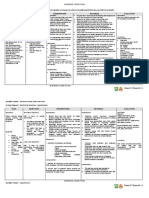
TABLE 1. Postoperative Adjuvant Therapy at Various Stages No. of patients 7 11 8 7 30 10 4 77 Stage IA IB IIA IIB IIIA IIIB IV Total Chemotherapy 3 3 2 3 5 1 3 20 Radiotherapy Chemotherapy/ radiation 2 6 5 3 19 4 1 40 No adjuvant treatment 2 2 1 1 4 4 0 14
2 1 3
65 years (range, 35-85 years). Seventy-four patients were active smokers or had a history of smoking at the time of diagnosis; the remaining 3 patients were nonsmokers. Seventy-six patients were white, and 1 was African American. At initial presentation, cough was the most common symptom; 26 patients (34%) were asymptomatic. In addition, 13 patients (17%) presented with neurological symptoms, including gait disturbances in 5, neuralgic pain in 3, paraneoplastic syndrome in 2, and visual disturbance, myasthenia, and seizure disorder in 1 each. Two patients had nonspecific symptoms, including dysphagia and chest pain. Only 5 patients had combined chemotherapy and radiation therapy before thoracotomy; 2 patients had stage IIB, and 1 each had stage IIIA, IIIB, and IV disease. All showed clinical and radiological response after neoadjuvant therapy except for the patient with stage IIIB disease, and all had evidence of residual disease in the resected specimen. Mediastinoscopy was performed in 30 patients. Surgical procedures included wedge excision in 30 patients (6 with concomitant talc pleurodesis), segmentectomy in 4, lobectomy in 28, bilobectomy in 3, pneumonectomy in 2,
100 (67) 80 60 40 20 0 0 2 4 6 8 10 12 (29) (13) (8) (8) (6) (5) (0) 14
Years from surgery
and thoracotomy with biopsy of the hilar mass in 10. Mediastinal lymphadenectomy was performed in 50 patients, mediastinal lymph node sampling was done in 19 patients, and no mediastinal lymph nodes underwent biopsy in 8 patients. Median tumor diameter was 4 cm (range, 1.0-10.0 cm). A curative resection (R0 resection) was done in 46 patients (60%). Postsurgical stage was IA in 7 patients, IB in 11, IIA in 8, IIB in 7, IIIA in 30, IIIB in 10, and IV in 4. There were 2 perioperative deaths (operative mortality, 2.6%). The cause of death was pulmonary embolism in a patient with stage IV disease and unknown in another patient with stage IV disease. Postoperative complications occurred in 19 patients (24.4%) and included atrial arrhythmias in 7, pneumonia in 6, prolonged air leak in 3, and myocardial infarction, postoperative bleeding, and cerebrovascular accident in 1 each. Adjuvant therapy included chemotherapy in 20 patients, radiation therapy in 3, and both in 40 (Table 1). Median follow-up was 19 months (range, 4 days to 170 months). At last follow-up, 20 patients were alive and 57 had died. Excluding the 10 patients who just underwent biopsy, the overall 5-year survival was 27% (Figure 1) and varied according to stage (Table 2) (Figure 2). Five-year survival for patients with stage I disease was 36%; for stage II, 40%; for stage III, 17%; and for stage IV, 0% (P=.06). Five-year survival for patients with stage I and II disease combined was 38% compared with 16% for patients with stage III and IV disease (Figure 3) (P=.02). Median survival for patients who underwent curative surgery was 25 months compared with 16 months for those who had a palliative procedure (Figure 4) (P=.34). After multivariable analysis, surgical stage (III/IV vs I/II) was the only significant predictor identified, implying that after accounting for this risk factor, no other variable contributed significantly to the survival model. DISCUSSION Small cell lung cancer accounts for 10% to 15% of all bronchogenic carcinomas in the United States. It is a dis www.mayoclinicproceedings.com
FIGURE 1. Overall survival of patients. Probability of survival (death from any cause) in 67 patients who underwent resection of small cell lung cancer. Zero time on abscissa represents date of lung resection. Patients who had surgical biopsy only are excluded. Numbers in parenthesis are the number of patients at risk. Overall median survival was 24 months.
Percentage alive
620
Mayo Clin Proc.
May 2006;81(5):619-624
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
PULMONARY RESECTION IN SMALL CELL LUNG CANCER
TABLE 2. Survival Rates at Various Stages Percentage of patients who survived No. of patients 18 15 31 3 67* Stage I II III IV All patients Median survival (mo) 29 23 22 16 24 1y 78 79 69 67 73 2y 67 40 38 50 49 3y 49 40 23 0 33 5y 36 40 17 0 27
*The 10 patients who had only a biopsy are excluded.
tinct pathological entity with the unique clinical behavior of a short doubling time and thus rapid tumor growth.6 This behavior explains the aggressive clinical nature of SCLC and its high sensitivity to cytotoxic chemotherapy.7 Usually, SCLC is considered a systemic disease at the time of diagnosis and generally carries a poor prognosis because of both its rapid growth rate and its propensity to metastasize.7,8 Two thirds of patients with seemingly localized disease (disease limited to 1 hemithorax, the mediastinum, and supraclavicular nodes, provided all disease can be included in 1 radiotherapy field) at initial diagnosis have distant occult metastasis, precluding curative radiotherapy or surgery.9 Untreated, patients with limited stage SCLC rarely survive more than 35 weeks, and when extensive disease (ie,
disease beyond the domain of limited disease)10 is present, the median survival is only 20 weeks.11 Historically, only 10% of patients with SCLC present with disease confined to the ipsilateral hemithorax without evidence of distant spread.12 Most patients who undergo surgery for SCLC represent a select subgroup with limited disease; therefore, it is not surprising that a large proportion of our patients (34%) were asymptomatic at presentation. Before 1970, patients with SCLC were treated with surgical resection, often pneumonectomy. However, the poor survival of surgically treated patients in randomized clinical trials13-16 led most clinicians to abandon surgery as the initial treatment, and chemotherapy, either alone or in combination with radiation therapy, became the standard
100 Stage I Stage II Stage III Stage IV
80
Percentage alive
60
40
20
0 0 Stage I Stage II Stage III Stage IV 18 15 31 3 2 12 5 12 1 4 6 4 3 6 4 3 1 8 4 3 1 10 3 3 12 2 3 14 0 0
Years from surgery
FIGURE 2. Survival of patients by stage. Probability of survival (death from any cause) in patients who underwent resection of small cell lung cancer. Zero time on abscissa represents date of lung resection. Patients who had surgical biopsy only are excluded. Numbers under the graph represent the number of patients at risk. Log-rank, P=.13.
Mayo Clin Proc.
May 2006;81(5):619-624
www.mayoclinicproceedings.com
621
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
PULMONARY RESECTION IN SMALL CELL LUNG CANCER
100
80
Stage I/II Stage III/IV
Percentage alive
60
40
20
0 0 Stage I/II Stage III/IV 33 34 2 17 12 4 10 3 6 7 1 8 7 1 10 6 12 5 14 0
Years from surgery
FIGURE 3. Survival of patients in stage I and II vs those in stage III and IV. Probability of survival (death from any cause) in patients who underwent resection of small cell lung cancer. Zero time on abscissa represents date of lung resection. Patients who had surgical biopsy only are excluded. Numbers under the graph represent the number of patients at risk. Log-rank, P=.02.
treatment.17,18 Although the initial results with combined chemotherapy and radiation therapy were encouraging,19 long-term survival is poor,20-22 with less than 15% of pa-
tients surviving more than 2 years.23 Even in patients with limited stage disease treated with chemotherapy and radiotherapy, the median survival is 15 to 20 months with 2- and
100
80
Palliative Curative
Percentage alive
60
40
20
10
12
14
Years from surgery
Curative 46 Palliative 31 22 9 10 4 6 2 6 2 6 5 0
FIGURE 4. Survival of patients who had curative surgery vs those who had noncurative procedures. Zero time on abscissa represents date of lung resection. Patients who had surgical biopsy only are included. Numbers under the graph represent the number of patients at risk. Log-rank, P=.34.
622
Mayo Clin Proc.
May 2006;81(5):619-624
www.mayoclinicproceedings.com
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
PULMONARY RESECTION IN SMALL CELL LUNG CANCER
5-year survival rates of 40% to 50% and 10% to 20%, respectively.24 The most frequent localized relapse is at the site of the tumor. Even with the addition of thoracic radiation, relapse continues to occur at the primary site in up to one third of patients.1,25,26 This suggests that if survival is to improve, more aggressive local tumor control is necessary. This has led to renewed interest in the role of surgical resection of the primary tumor and regional lymph nodes. Although our retrospective study is not randomized, our results suggest that long-term survival can be achieved with surgical resection in selected patients with SCLC. Others have found similar results.12,19,27-36 Shields et al12 reported a 5-year survival rate of 23% in patients who had curative pulmonary resection and adjuvant chemotherapy. Our own survival results at 2 and 5 years of 49% and 27%, respectively, are also similar to other series. We analyzed several clinical variables in an attempt to identify factors predicting cumulative probability of survival. The pathological TNM stage was the only factor affecting survival. Long-term survival was greatest in patients with stage I and II disease. This finding has also been reported by others.12 Although we were unable to demonstrate that pulmonary resection significantly influenced survival, as suggested by Davis et al,35 our patients survived longer when curative pulmonary resection was performed. Our inability to show a statistically significantly difference is likely because of the limited number of patients. Surgical resection alone, however, is inadequate therapy for limited SCLC. The objective of surgical resection in the treatment of these patients is to achieve better control of the primary site when combined with postoperative chemotherapy and local radiotherapy.23 Patients with stage II and stage III disease with hilar and mediastinal lymph nodes are candidates for postoperative thoracic radiotherapy. Management of SCLC should utilize principles similar to those used in the management of non-SCLC. When the diagnosis of SCLC is established preoperatively, the stage of disease should be clinically determined by obtaining the history of the patient and performing a physical examination, computed tomography, and positron emission tomography. When clinically indicated, mediastinal exploration either by mediastinoscopy or mediastinotomy should be performed before thoracotomy. If occult mediastinal lymph node metastasis is found, pulmonary resection is unlikely to benefit the patient, and combined chemotherapy and radiation therapy should be offered. Patients with advanced local disease (any T3 or N2 lesions) have an extremely poor prognosis after resection.12 In our series, only 17% patients with N2 disease survived more than 5 years. The difference in survival for patients with N2 disease
Mayo Clin Proc.
compared to those without it was statistically significant (P=.03). Patients with stage I tumors, even when proved to be SCLC on needle biopsy, should be offered a surgical approach since many of these tumors may prove not to be SCLC, and the results of surgical resection for stage I disease are excellent.37 Although a 20% five-year survival was reported for patients with limited SCLC in a recent radiotherapy intergroup trial,38 the disease in the patients in that study was not staged using the TNM staging system. In almost all instances, the surgical pathological staging is more advanced than the preoperative clinical staging even when mediastinoscopy is used.39 For this reason, a true estimation cannot be made of the cure rate of patients with clinical stage T1 N0 or T2 N0 disease who receive combined chemotherapy and radiation as the primary treatment. As long as a complete surgical resection can be performed, surgery must be considered as the first step of the multi-modality treatment in these patients. Future trials should be encouraged to use the TNM staging system since it provides better details of the stage of the disease compared to the terms limited and extensive disease so that a more valid comparison can be made in the future.37 The timing of surgical intervention is also controversial. Whether adjuvant or neoadjuvant chemotherapy and radiotherapy are more effective is often debated. The survival rates of preoperative chemotherapy followed by surgery are inferior to those obtained by treating patients with surgery first, followed by adjuvant chemotherapy.19 The 5year survival rate for patients who underwent surgery followed by postoperative chemotherapy for pathological stage I disease was as high as 48% in a study by Shepherd et al.23 The authors concluded that surgery followed by chemotherapy was the best treatment for stage I disease. Since only 5 of our patients had preoperative therapy, we cannot make a conclusive recommendation that differs from the current literature. CONCLUSION Pulmonary resection in patients with stage I or stage II SCLC is safe with low mortality and morbidity. Curative resection is associated with long-term survival in early stage SCLC and should be considered in selected patients.
REFERENCES 1. Elliott JA, Osterlind K, Hirsch FR, Hansen HH. Metastatic patterns in small-cell lung cancer: correlation of autopsy findings with clinical parameters in 537 patients. J Clin Oncol. 1987;5:246-254. 2. American Joint Committee for Cancer Staging and End-Results Reporting. System for Staging and Lung Cancer. Chicago, Ill: American Joint Committee for Cancer Staging and End-Results Reporting; 1979. 3. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457-481. 4. Peto R, Peto J. Asymptotically efficient rank invariant procedures. J R Stat Soc [A]. 1972;135:185-206.
May 2006;81(5):619-624
www.mayoclinicproceedings.com
623
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
PULMONARY RESECTION IN SMALL CELL LUNG CANCER
5. Cox DR. Regression models and life-tables [with discussion]. J R Stat Soc [B]. 1972;34:187-220. 6. Aisner J, Whitacre M, Van Echo DA, Wiernik PH. Combination chemotherapy for small cell carcinoma of the lung: continuous versus alternating noncross-resistant combinations. Cancer Treat Rep. 1982;66:221-230. 7. Straus MJ. The growth characteristics of lung cancer and its application to treatment design. Semin Oncol. 1974;1:167-174. 8. Greco FA, Oldham RK. Current concepts in cancer: small-cell lung cancer. N Engl J Med. 1979;301:355-358. 9. Hansen HH, Dombernowsky P, Hirsch FR. Staging procedures and prognostic features in small cell anaplastic bronchogenic carcinoma. Semin Oncol. 1978;5:280-287. 10. Mountain CF. Revisions in the International System for Staging Lung Cancer. Chest. 1997;111:1710-1717. 11. Wolf J, Patno ME, Roswit B, DEsopo N. Controlled study of survival of patients with clinically inoperable lung cancer treated with radiation therapy. Am J Med. 1966;40:360-367. 12. Shields TW, Higgins GA Jr, Matthews MJ, Keehn RJ. Surgical resection in the management of small cell carcinoma of the lung. J Thorac Cardiovasc Surg. 1982;84:481-488. 13. Miller AB, Fox W, Tall R. Five-year follow-up of the Medical Research Council comparative trial of surgery and radiotherapy for the primary treatment of small-celled or oat-celled carcinoma of the bronchus. Lancet. 1969;2: 501-505. 14. Fox W, Scadding JG. Medical Research Council comparative trial of surgery and radiotherapy for primary treatment of small-celled or oat-celled carcinoma of the bronchus: ten-year follow-up. Lancet. 1973;2:63-65. 15. Takita H, Brugarolas A, Marabella P, Vincent RG. Small cell carcinoma of the lung: clinicopathological studies. J Thorac Cardiovasc Surg. 1973; 66:472-477. 16. Mountain CF. Clinical biology of small cell carcinoma: relationship to surgical therapy. Semin Oncol. 1978;5:272-279. 17. Livingston RB. Current chemotherapy of small cell lung cancer. Chest. 1986;89(4, suppl):258S-263S. 18. Morstyn G, Ihde DC, Lichter AS, et al. Small cell lung cancer 1973 1983: early progress and recent obstacles. Int J Radiat Oncol Biol Phys. 1984; 10:515-539. 19. Karrer K, Ulsperger E, ISC-Lung Cancer Study Group. Surgery for cure followed by chemotherapy in small cell carcinoma of the lung. Acta Oncol. 1995;34:899-906. 20. Chrystal K, Cheong K, Harper P. Chemotherapy of small cell lung cancer: state of the art. Curr Opin Oncol. 2004;16:136-140. 21. Sandler AB. Chemotherapy for small cell lung cancer. Semin Oncol. 2003;30:9-25. 22. Shepherd FA, Ginsberg RJ, Haddad R, et al, University of Toronto Lung Oncology Group. Importance of clinical staging in limited small-cell lung cancer: a valuable system to separate prognostic subgroups. J Clin Oncol. 1993;11:1592-1597.
23. Shepherd FA, Ginsberg RJ, Feld R, Evans WK, Johansen E. Surgical treatment for limited small-cell lung cancer: the University of Toronto Lung Oncology Group experience. J Thorac Cardiovasc Surg. 1991;101:385-393. 24. Simon G, Ginsberg RJ, Ruckdeschel JC. Small-cell lung cancer. Chest Surg Clin N Am. 2001;11:165-188. 25. Perez CA, Einhorn L, Oldham RK, et al. Randomized trial of radiotherapy to the thorax in limited small-cell carcinoma of the lung treated with multiagent chemotherapy and elective brain irradiation: a preliminary report. J Clin Oncol. 1984;2:1200-1208. 26. Kies MS, Mira JG, Crowley JJ, et al. Multimodal therapy for limited small-cell lung cancer: a randomized study of induction combination chemotherapy with or without thoracic radiation in complete responders and with wide-field versus reduced-field radiation in partial responders: a Southwest Oncology Group Study. J Clin Oncol. 1987;5:592-600. 27. Higgins GA, Shields TW, Keehn RJ. The solitary pulmonary nodule: ten-year follow-up of Veterans Administration-Armed Forces Cooperative Study. Arch Surg. 1975;110:570-575. 28. Meyer JA, Comis RL, Ginsberg SJ, et al. Selective surgical resection in small cell carcinoma of the lung. J Thorac Cardiovasc Surg. 1979;77:243-284. 29. Meyer JA, Comis RL, Ginsberg SJ, et al. Phase II trial of extended indications for resection in small cell carcinoma of the lung. J Thorac Cardiovasc Surg. 1982;83:12-19. 30. Meyer JA, Comis RL, Ginsberg SJ, et al. The prospect of disease control by surgery combined with chemotherapy in stage I and stage II small cell carcinoma of the lung. Ann Thorac Surg. 1983;36:37-41. 31. Shore DF, Paneth M. Survival after resection of small cell carcinoma of the bronchus. Thorax. 1980;35:819-822. 32. Bates M, Levison V, Hurt R, Sutton M. Treatment of oat-cell carcinoma of bronchus by preoperative radiotherapy and surgery. Lancet. 1974;1:1134-1135. 33. Li W, Hammar SP, Jolly PC, Hill LD, Anderson RP. Unpredictable course of small cell undifferentiated lung carcinoma. J Thorac Cardiovasc Surg. 1981;81:34-43. 34. Shepherd FA, Ginsberg RJ, Evans WK, et al. Reduction in local recurrence and improved survival in surgically treated patients with small cell lung cancer. J Thorac Cardiovasc Surg. 1983;86:498-506. 35. Davis S, Wright PW, Schulman SF, Scholes D, Thorning D, Hammar S. Long-term survival in small-cell carcinoma of the lung: a population experience. J Clin Oncol. 1985;3:80-91. 36. Inoue M, Miyoshi S, Yasumitsu T. Surgical results for small cell lung cancer based on the new TNM staging system. Ann Thorac Surg. 2000;70: 1615-1619. 37. Ginsberg RJ. Small cell lung cancer: how should we treat it? what is it? [editorial]. Ann Thorac Surg. 2000;70:1453-1454. 38. Turrisi AT III, Kim K, Blum R, et al. Twice-daily compared with oncedaily thoracic radiotherapy in limited small-cell lung cancer treated concurrently with cisplatin and etoposide. N Engl J Med. 1999;340:265-271. 39. Holmes EC. The role of surgery in small cell carcinoma of the lung (SCLC). Lung Cancer. 1995;12(suppl 3):S17-S21.
624
Mayo Clin Proc.
May 2006;81(5):619-624
www.mayoclinicproceedings.com
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Acute Kidney Injury W/ Hyperkalemia NCPDocument5 pagesAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNo ratings yet
- Sanctification of The Heart 4th Edition by DR Michelle StrydomDocument771 pagesSanctification of The Heart 4th Edition by DR Michelle StrydomDios Estrella67% (3)
- Litrature & Case StudyDocument74 pagesLitrature & Case Studynaol buloNo ratings yet
- Typhoid Fever NCPDocument46 pagesTyphoid Fever NCPLyra Lustre RN67% (3)
- Definition:: Between 16Document3 pagesDefinition:: Between 16NIDA MUSTAFANo ratings yet
- Acute Respiratory Distress Syndrome Nursing Management and Interventions - NurseslabsDocument2 pagesAcute Respiratory Distress Syndrome Nursing Management and Interventions - NurseslabsSachin SinghNo ratings yet
- Aula 1Document14 pagesAula 1Brigida Cirqueira GuimaraesNo ratings yet
- Autism and Dietary Therapy: Case Report and Review of The LiteratureDocument6 pagesAutism and Dietary Therapy: Case Report and Review of The LiteratureAntiopi PanteliNo ratings yet
- IV To PO Poster VersionDocument1 pageIV To PO Poster VersionJohn Benedict Sta AnaNo ratings yet
- Assessment and Management of Patients With Hearing and Balance DisordersDocument9 pagesAssessment and Management of Patients With Hearing and Balance Disordersxhemhae100% (1)
- Prescriptions On Asthma & APDDocument9 pagesPrescriptions On Asthma & APDeesha shahNo ratings yet
- Chapter 22: The Thyroid Gland: by Marissa Grotzke, Dev AbrahamDocument21 pagesChapter 22: The Thyroid Gland: by Marissa Grotzke, Dev AbrahamJanielle FajardoNo ratings yet
- Health Check Template FormDocument2 pagesHealth Check Template Form백만호No ratings yet
- Health and IllnessDocument2 pagesHealth and IllnessLize Decotelli HubnerNo ratings yet
- List of Empanelled Hospitals in CGHS NagpurDocument58 pagesList of Empanelled Hospitals in CGHS NagpurRajatNo ratings yet
- Infectiile Grave Extensive Ale Partilor MoiDocument49 pagesInfectiile Grave Extensive Ale Partilor MoiLoredana BoghezNo ratings yet
- ACTIVIDAD INGLES Reading ComprehensionDocument3 pagesACTIVIDAD INGLES Reading Comprehensionyulis mesaNo ratings yet
- English Nursing: Have You Gave A Chamber Pot To Mrs. Johnson?Document2 pagesEnglish Nursing: Have You Gave A Chamber Pot To Mrs. Johnson?Faris Albert WenasNo ratings yet
- Resume - Viroja Sweta For PortfolioDocument1 pageResume - Viroja Sweta For Portfolioapi-608195339No ratings yet
- Electrocardiography Wave Analysis: Using MATLABDocument19 pagesElectrocardiography Wave Analysis: Using MATLABSMNo ratings yet
- Morpho - Pathology Final Summary: Chapter 1: Cellular Reactions To AggressionDocument21 pagesMorpho - Pathology Final Summary: Chapter 1: Cellular Reactions To Aggressiondjxela89No ratings yet
- Centenarian Gut Microbiota Effects On Bile AcidDocument32 pagesCentenarian Gut Microbiota Effects On Bile Acidjl18904lamNo ratings yet
- Prolonged LaborDocument13 pagesProlonged Laborsujinaranamagar18No ratings yet
- Assignment 1 Cs 0902Document4 pagesAssignment 1 Cs 0902prince12No ratings yet
- Jomi 7657Document27 pagesJomi 7657casto.carpetasmiaNo ratings yet
- Introducing The Epidermis.: ReallyDocument47 pagesIntroducing The Epidermis.: ReallyNaila JinNo ratings yet
- OSCE Chart Cough (KK)Document4 pagesOSCE Chart Cough (KK)api-26938624No ratings yet
- Fetal risks of macrosomia in diabetic pregnanciesDocument27 pagesFetal risks of macrosomia in diabetic pregnanciesIful SaifullahNo ratings yet
- 020 - Metabolism of Proteins 3Document12 pages020 - Metabolism of Proteins 3Sargonan RaviNo ratings yet
- Case Report模板Document18 pagesCase Report模板ChenNo ratings yet