Professional Documents
Culture Documents
Local Anesthetic
Uploaded by
Vannia Dwyputrya AdissyaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Local Anesthetic
Uploaded by
Vannia Dwyputrya AdissyaCopyright:
Available Formats
Intra-articular lidocaine for the reduction of posterior shoulder dislocation
Case Reports
Steven J. Socransky, MD; Lee V. Toner, MD Hpital Regional de Sudbury Regional Hospital, Northern Ontario Medical School of Medicine CJEM 2005;7(6):423-426
Abstract
Anterior shoulder dislocations are the most common major joint dislocation seen in emergency departments. Intra-articular lidocaine is a useful method of analgesia for facilitating the reduction of anterior shoulder dislocations. Posterior shoulder dislocations represent a small minority of shoulder dislocations. We present the case of a posterior shoulder reduction in an elderly female whose reduction was performed following the intra-articular injection of lidocaine. Intra-articular lidocaine represents a useful alternative to facilitate the reduction of shoulder dislocations, particularly in patients at higher risk for complications from sedation.
Rsum
La luxation antrieure de lpaule est le type de luxation le plus souvent rencontr au dpartement d'urgence. La lidocane intraarticulaire est une mthode analgsique efficace pour faciliter la rduction de cette luxation. La luxation postrieure reprsente un faible pourcentage des luxations de l'paule. Nous prsentons un cas de luxation postrieure de l'paule chez une patiente ge; la rduction fut effectue la suite d'une injection intra-articulaire de lidocane, une solution de rechange utile pour faciliter la rduction des luxations de l'paule, en particulier chez les patients risque plus lev de complications lies la sdation.
Introduction
Shoulder dislocations are the most common major joint dislocation seen in emergency departments (ED). 1Procedural sedation and analgesia (PSA) is commonly employed to facilitate shoulder reduction. However, there are some drawbacks to this. The use of intra-articular lidocaine (IAL) to facilitate the reduction of anterior shoulder dislocations has been described as an alternative to PSA.28 The use of IAL in posterior shoulder dislocations has not been reported in the English literature. We present a case of posterior shoulder dislocation whose reduction was facilitated by IAL.
Case report
A 77-year-old woman presented to the ED via ambulance after tripping and falling down 5 steps at home. She landed on her right elbow and then fell forward onto her right shoulder. In the ED, she complained of right shoulder, elbow and knee pain. There was no head or neck trauma or loss of consciousness. The history was not suggestive of a cardiac, neurologic or other underlying event as the precipitant for the fall. At the time of physician assessment, she had not had anything to eat or drink for over 5 hours. Past medical and surgical history included bladder surgery. Her only medication was a daily vitamin. She denied any allergies. Physical examination revealed a thin, frail, elderly woman in considerable discomfort from the right shoulder pain. Her vital signs were within normal limits. Head and neck examination revealed no signs of trauma. Respiratory, cardiac and abdominal examinations were unremarkable. Her right arm was internally rotated and adducted, with her forearm held across her anterior neck, just under her chin. Range of motion of her right shoulder was restricted. Diffuse right shoulder tenderness was centred at her proximal humerus, which appeared to be dislocated posteriorly. Neurovascular status was intact, including normal sensation over her lower deltoid. Her right knee had a contusion. Radiographs (anteriorposterior, transscapular) of her right shoulder demonstrated a posterior shoulder dislocation. Radiographs of her right knee were normal. The position of her forearm raised concern that laryngoscopy would be difficult in the event that her airway should be lost as a complication of PSA. Given the concern for a potentially difficult intubation and the patients age, IAL was used for procedural analgesia. The patient had initially received a total of 9 mg of subcutaneous morphine for pain, with only minimal effect. The patient was maintained in a semi-recumbent position. Surface landmarks were palpated, including the acromion, humeral head and the lateral sulcus formed by the absent humeral head. Using full sterile technique, a 22-gauge, 3.5-cm needle was directed into the skin
approximately 2 cm inferior and directly lateral to the acromion, and in the lateral sulcus. The needle was directed caudal toward the glenoid cavity (Fig. 1, Fig. 2). Upon aspirating serosanguinous synovial fluid, 20 mL of 1% lidocaine without epinephrine was injected into the joint over 30 seconds. Fifteen minutes after the injection, the patient noted good analgesia. Reduction was performed successfully by applying longitudinal traction and pushing the posteriorly displaced humeral head anteriorly. The patient noted only mild discomfort. There were no neurovascular complications.
Fig. 1: Demonstration of approximate angle and location at which the needle enters the skin. The physicians left thumb is palpating the acromion process of a normal volunteer. Post-reduction radiographs confirmed reduction with no evidence of fracture. Review of the patient's follow-up hospital records revealed no post-procedural cellulitis or septic arthritis. A clinical diagnosis of possible rotator cuff tear was made during orthopedic follow-up. The patient improved with conservative management.
Discussion
Patients with shoulder dislocations commonly present to EDs. Anterior shoulder dislocations are the most common shoulder dislocation.1 Posterior shoulder dislocations represent less than 2% of shoulder dislocations.9This case represents the first report of IAL use for posterior shoulder reduction. We used a similar technique to that previously described for anterior shoulder dislocations.3 Although reduction without anesthesia is sometimes performed, PSA is often employed to facilitate reduction. Intra-articular lidocaine represents an alternative to PSA with several potential advantages. One author has even advocated that IAL be used for every shoulder reduction.10 It can be used in the non-fasting patient, the recovery time is not prolonged and it does not require additional medical personnel or resources. Several studies have compared IAL to PSA for facilitating anterior shoulder dislocation reduction. Most studies report similar success rates for anterior shoulder reductions with either IAL or PSA. 25,8 However, it should be noted that the majority of these studies used first-line reduction techniques (e.g., the Hippocratic method or external rotation methods) and PSA agents (e.g., meperidine, diazepam) not typical of current practice. Kosnik and colleagues7 reported a trend toward higher reduction success rates with sedation than IAL. This trend became significant in patients who were treated more than 5.5 hours after their dislocation occurred. Orlinsky found that pre-reduction pain relief was better with intravenous medication than with IAL, but there was no significant difference in overall pain relief after reduction. 4 There was no significant difference in pain felt to be interfering with the reduction by physicians, but there was a trend in physician perception of less muscle relaxation with IAL.4 PSA with potent opioids or anesthetic agents has the potential for serious adverse effects, such as airway compromise, hypoventilation and hypotension. Patients with significant comorbid disease, intoxicated patients, pregnant patients, multiple trauma patients and the elderly are at particularly high risk. More complications (e.g., hypotension, respiratory depression, need for reversal agent, or admission) have been reported with sedation than with IAL.2,3,5 Minor side effects such as vomiting and post-procedural lethargy are common with sedation.4 Intra-articular lidocaine can be used in patients with poor access for intravenous administration. However, sedation may offer advantages in certain patients. When used alone, IAL may not facilitate reduction in muscular patients. Sedation may be needed to provide adequate muscle relaxation.7 As well, sedation may be needed in patients who are anxious about the reduction procedure. PSA also consumes significant resources. As proposed by national guidelines, 11 a second physician, nurse or respiratory technologist is required for adequate patient monitoring during sedation. This may not be available in some EDs or at some times of the day. Prolonged and dedicated nursing care is the norm. Medications used for sedation may add significant cost compared with IAL.3,7 Emergency department throughput may be negatively impacted by more prolonged lengths of stay with PSA versus IAL.2 4,8 As well, patients need to be fasting for several hours before the sedation. 11 This can lead to a delay in definitive treatment for the
patient and result in an increased length of stay in the ED. Finally, patients at high risk for complications from PSA require reduction in the operating room with a resultant greater use of resources. Patient preference should be considered when choosing an anesthetic approach to facilitate shoulder reduction. Patient satisfaction with IAL has been good,5 although some patients with prior shoulder reductions done under sedation may prefer to receive the same treatment.7 Some patients may be fearful of sedation. Intra-articular lidocaine may provide another possible option in such cases. As well, IAL may be used as an adjunct to PSA, allowing for lower doses of sedative medications to be used. Further work needs to be done in this area.
Conclusion
Intra-articular lidocaine represents a useful alternative to facilitate the reduction of anterior shoulder dislocations. Advantages over PSA include fewer serious systemic adverse events, less use of resources and improved ED throughput. Our case demonstrates that IAL may also be useful for posterior shoulder dislocations. Further study of IAL for posterior shoulder dislocations is required.
References
1. McNamara R. Management of common dislocations. In: Roberts JR, Hedges JR, editors. Clinical procedures in emergency medicine, 3rd ed. Philadelphia: WB Saunders; 1998. p. 818-52. 2. Suder PA, Mikkelsen JB, Houggard K, Jensen PE. Reduction of traumatic secondary shoulder dislocations with lidocaine. Arch Orthop Trauma Surg 1995;114:233-6. 3. Matthews DE, Roberts T. Intraarticular lidocaine versus intravenous analgesic for reduction of acute anterior shoulder dislocations. Am J Sports Med 1995;23:54-8. 4. Orlinsky M, Shon S, Chiang C, Chan L, Carter P. Comparative study of intra-articular lidocaine and intravenous meperidine/diazepam for shoulder dislocations. J Emerg Med 2002;22:241-5. 5. Lippitt SB, Kennedy JP, Thompson TR. Intraarticular lidocaine versus intravenous analgesia in the reduction of dislocated shoulders. Orthop Trans 1991;15:804. 6. Gleeson AP, Graham CA, Jones I, Beggs I, Nutton RW. Comparison of intra-articular lignocaine and a suprascapular nerve block for acute anterior shoulder dislocation. Injury 1997;28:141-2. 7. Kosnik J, Shamsa F, Raphael E, Huang R, Malachias Z, Georgiadis GM. Anesthetic methods for reduction of acute shoulder dislocations: a prospective randomized study comparing intraarticular lidocaine with intravenous analgesia and sedation. Am J Emerg Med 1999;17:566-70. 8. Miller SL, Cleeman E, Auerbach J, Flatow EL. Comparison of intra-articular lidocaine and intravenous sedation for reduction of shoulder dislocations: a randomized, prospective study. J Bone Joint Surg 2002;84-A(12):2135-9. 9. Cicak N. Posterior dislocation of the shoulder. J Bone Joint Surg Br 2004;86:324-32. 10. Sineff SS, Reichman EF. Shoulder joint dislocation reduction. In: Reichman EF, Simon RR, editors. Emergency medicine pProcedures. 1st ed. McGraw-Hill, 2004. p. 593-613. 11. Innes G, Murphy M, Nijssen-Jordan C, Ducharme J, Drummond A. Procedural sedation and analgesia in the emergency department. J Emerg Med 1999;17:145-56. Acknowledgement: This article has been peer reviewed. Correspondence to:
Dr. Steve Socransky, Emergency Department, Hpital regional de Sudbury Retional Hospital, 700 Paris St., Sudbury ON P3E 3B5 Submitted: July 18, 2005; revisions received: Sept. 10, 2005; accepted Sept. 29, 2005
http://www.cjem-online.ca/v7/n6/p423
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Final Booklist For First Year - 2019Document1 pageFinal Booklist For First Year - 2019RPh FarhatainNo ratings yet
- DDD Rawat Inap ExcelDocument10 pagesDDD Rawat Inap ExcelJakobus Benny SalimNo ratings yet
- SOP 12: Validation of Bioanalytical Methods: Background and ObjectivesDocument4 pagesSOP 12: Validation of Bioanalytical Methods: Background and ObjectivesMaheshNo ratings yet
- Chapter 1. Medication Management Services: Key ConceptsDocument418 pagesChapter 1. Medication Management Services: Key ConceptsJulaiha Qosim100% (4)
- Quick Guide To ProscriptDocument20 pagesQuick Guide To ProscriptAmit Raj100% (2)
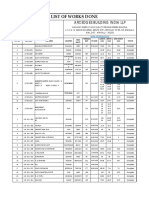
- List of Works Done 27042020 PDFDocument3 pagesList of Works Done 27042020 PDFZankar R ParikhNo ratings yet
- Effectiveness of Otc Drug Advertising and Its Impact On Consumer BehaviorDocument9 pagesEffectiveness of Otc Drug Advertising and Its Impact On Consumer BehaviorUdevir Singh100% (1)
- Finals 109 6Document202 pagesFinals 109 6JHOANA MARIE LOONo ratings yet
- 1026 FullDocument5 pages1026 FullMuhammad Yufimar Rizza FadilahNo ratings yet
- Essensial DrugDocument363 pagesEssensial Drugwilliam28asshole100% (1)
- Medikolegal Pengobatan Untuk Diri Sendiri (Swamedikasi) Sebagai Upaya Menyembuhkan PenyakitDocument8 pagesMedikolegal Pengobatan Untuk Diri Sendiri (Swamedikasi) Sebagai Upaya Menyembuhkan PenyakitMiftahul JannahNo ratings yet
- Pharmicalogical Info On GingerDocument261 pagesPharmicalogical Info On GingerAngelNo ratings yet
- Dissolution: in The Pharmaceutical IndustryDocument4 pagesDissolution: in The Pharmaceutical IndustryAhmed EdamNo ratings yet
- Bus 101Document2 pagesBus 101Showrov RahmanNo ratings yet
- Date Sheet For The Doctor of Pharmacy PharmD Annual Examination 2023 t8008Document2 pagesDate Sheet For The Doctor of Pharmacy PharmD Annual Examination 2023 t8008Haniya RajpootNo ratings yet
- S.N o Name of Drug Recommended Paediatrics Dose Strength 1.: CPM - 2 mg/5mlDocument3 pagesS.N o Name of Drug Recommended Paediatrics Dose Strength 1.: CPM - 2 mg/5mlmrs raamNo ratings yet
- SymptomAssessmentRevised Sept09Document2 pagesSymptomAssessmentRevised Sept09Nicole Lopez DaquiadoNo ratings yet
- Dossier 1325Document166 pagesDossier 1325Daniel PorumbNo ratings yet
- Daman Taxpayers With UTGST - 2594Document70 pagesDaman Taxpayers With UTGST - 2594archana.rout0919No ratings yet
- PHD211 - Ointment 2019Document147 pagesPHD211 - Ointment 2019honeylemon.co100% (2)
- Hypertonic Saline (3% and 5% Sodium Chloride Injection) Drug Information - Description, User Reviews, Drug Side Effects, Interactions - Prescribing Information at RxListDocument2 pagesHypertonic Saline (3% and 5% Sodium Chloride Injection) Drug Information - Description, User Reviews, Drug Side Effects, Interactions - Prescribing Information at RxListMuhammad AsadNo ratings yet
- Confuseddrugnames 201902Document11 pagesConfuseddrugnames 201902Detya PertiwiNo ratings yet
- CETIRIZINEDocument2 pagesCETIRIZINEAngelica Cassandra Villena100% (10)
- Post Marketing SurveillanceDocument19 pagesPost Marketing SurveillanceAnoopInderNo ratings yet
- Overall Strategy For Treatment of Critical Limb IschemiaDocument83 pagesOverall Strategy For Treatment of Critical Limb IschemiaamurachNo ratings yet
- Pharmacology For NursesDocument2 pagesPharmacology For Nursesjoy abuanNo ratings yet
- Ranbaxy Laboratories LTD.: Accounting For Managers ProjectDocument7 pagesRanbaxy Laboratories LTD.: Accounting For Managers ProjectAnmol SinghviNo ratings yet
- Sy0089 PDFDocument44 pagesSy0089 PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Compilation of Community Procedures in Inspections and Exchange of InformationDocument6 pagesCompilation of Community Procedures in Inspections and Exchange of InformationDaoNo ratings yet
- ONE Compartment Open ModelDocument29 pagesONE Compartment Open ModelNOORUDDINNo ratings yet