Professional Documents
Culture Documents
Article Charge Nurse
Uploaded by
Anonymous bq4KY0mcWGOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Article Charge Nurse
Uploaded by
Anonymous bq4KY0mcWGCopyright:
Available Formats
Taking Charge: What Every Charge Nurse Needs to Know
I am just not sure that I am ready to take charge. I know I have leadership skills but I am a relatively new nurse. Am I really ready to assume all this responsibility? My nurse manager thinks I have excellent leadership potential and is encouraging me to take the plunge. But what if the staff does not respect me in the role and what if I fail? n todays turbulent health care environment, it is not unusual for nurses to feel the type of anxiety that the nurse quoted above recently conveyed to one of the authors about assuming charge nurse responsibilities. Charge nurses are expected to lead staff while managing the work systems and processes on their units to insure that the needs of patients are met. It is a skillful balancing act and not all organizations provide the type of leadership training that the charge nurse may need (Hansten, 2008; Hudson, 2008; Sherman, 2005). Yet despite the challenges, embracing the role of charge nurse can provide enormous professional satisfaction and a tremendous leadership growth experience. Important keys to success in becoming an effective charge nurse include understanding the role responsibilities and developing the skills needed to enhance communication, reduce conflict and build team synergy.
Taking Charge
Defining the role of the charge nurse is not easy in todays healthcare delivery systems due to the inconsistencies in definition and scope across facilities. The title of charge nurse has been around since the early 1980s. One definition for a charge nurse that has been given is nurses assigned to a particular unit designated by the head nurse to coordinate nursing activities on a particular shift (Connelly, Nabarrete, & Smith, 2003, p. 204). Sometimes, a title other than charge nurse may be used such as unit
Volume 2, Issue 4 July/August 2009
coordinator or shift coordinator. The role may include expanded responsibilities such as conducting performance evaluations, scheduling, payroll, and chairing committees. The charge nurse role may be formal or informal. In some facilities, the role rotates between the various senior level nurses on a shift. In other organizations, the role is more formalized as a designated support position primarily held by one individual, with a relief person on the weekends. Some charge nurses are designated to be a resource for the rest of the team but maintain responsibility for their own patient assignment. If a facility is unionized, the union contracts may prohibit the use of a formal charge nurse role. Charge nurses have accountability to the organization, staff and patients for the care that is delivered. Organizations depend on charge nurses to be the gate keepers for safe and efficient care, which meets regulatory requirements and ensures an economic return. Charge nurses conduct real time assessments of unit productivity during various points throughout the shift. They often determine how staff resources will be distributed on their shift, or the upcoming shift in response to changing institutional and patient needs. Charge nurses must also be familiar with the institutions policies and procedures in order to navigate through what is often a very complex system. Charge nurses set expectations for staff and provide support so that staff can carry out those expectations. They are expected to hold staff accountable for performance of their professional patient care duties, adherence to regulatory requirements, and documentation of this essential information. The charge nurse serves as the conduit for information provided from staff to management and from management to staff. Charge nurses assist with the orientation, training and professional development of staff. They play a key role in the competency assessment process.
6
Charge nurses are often clinical experts in their areas of assignment. Their expertise allows them to engage with the staff nurses in clinical decision making and problem solving. During their shift of responsibility, charge nurses manage people, patient flow, use of equipment, and unit communication to ensure that the patients and staff get the support that they need. In order to manage all of these responsibilities, charge nurses must be able to effectively delegate and supervise care.
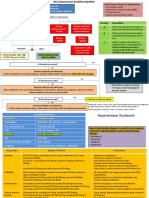
agencies also have position descriptions for each role that provide guidance for charge nurses about the expected competencies and role responsibilities of team members. Charge nurses are then ready to begin the delegation and supervision process which should include the following steps and reflective questions (NCSBN, 2005):
Step One - Assessment and Planning
Goal the Right Task, Under the Right Circumstances to the Right Person What are the needs and condition of the patient? What level of clinical decision making and assessment is needed? What is the predictability of the patients response to care? What is the potential for adverse outcomes associated with the performance of tasks and functions? What are the cognitive and technical abilities needed to perform the activity/function/task? Which team member has the scope of practice, skills, competencies and experience to perform the tasks needed? What is the context of the situation and the environment was the patient just admitted or did they have recent surgery, is it a high acuity environment such as an intensive care unit or ER? What level of interaction/communication is needed in the care of the patient and with whom?
Delegating and Supervising Nursing Care
Many charge nurses find it difficult to delegate tasks to other members of their health care team. When done well, delegation can be a very effective management tool. It frees professional nurses to attend to more complex client needs, develop the skills of nursing assistive personnel and promote cost containment for the organization (NCSBN, 2005). Ineffective delegation or a lack of follow-up supervision for tasks delegated can result in errors or omissions of care (Hansten, 2008). Dr. Linda Mahimeister, an attorney and nurse expert in the area of charge nurse accountability, recently noted in an interview that from a legal standpoint, charge nurses are expected to make decisions about allocating care based on staffing and patient needs. They will also be held accountable to provide surveillance and supervision of the care they delegate (Federwisch, 2008). Most states provide specific guidance about the delegation of nursing care in their professional practice acts and nursing administrative rules/regulations. The National Council of State Boards of Nursing (NCSBN, 2005) describes delegation as the transfer of authority by a qualified nurse to a competent individual for the purpose of completing selected tasks or activities. The assignment should be based on the assessment of the patients needs and the scope of practice/skills of the individual to whom care is delegated. The delegation can be to another RN, a licensed practical nurse or unlicensed assistive personnel. Follow-up guidance and supervision of care delegated is expected. In most states, activities that include the use of the nursing process or judgment/skills of the professional nurse (nursing assessment, diagnosis, plan of care, reassessment and evaluation of patient outcomes) can only be delegated to a registered nurse. Charge nurses need to become familiar with the practice acts in their own states. In addition to specific guidance about supervision and responsibilities, nurse practice acts outline the scope of practice of nursing team members. Prior to delegating care in a healthcare agency, key agency policies such as the assignment of nursing care and administration of medications should be reviewed. Healthcare
Volume 2, Issue 4 July/August 2009
Step Two Communication
Goal the Right Direction How is the task to be accomplished? When and what information is to be reported? What is the process for seeking clarification about delegated care? What are the communication expectations in emergency situations?
Step Three Supervision and Surveillance
Goal the Right Supervision What level of supervision and observation does the charge nurse need to provide? What will be the frequency of monitoring and observing care? How will the completion of care be verified and documented? How will unexpected changes in a patients condition be managed?
7
Step Four Observation and Feedback
Goal Assessment of the Effectiveness of Delegation Was the delegation successful? Is there a better way to meet the needs of the patient? Is there a need to adjust the plan of care? Were there learning moments for staff or charge nurse? Was appropriate feedback and follow-up provided by the charge nurse? Was positive feedback given when appropriate by the charge nurse? In their discussion of the qualities of an effective charge nurse, Leary and Allen (2006) have noted that there is both an art and science to delegation. The science of delegation involves understanding licensure responsibilities from a legal standpoint and the policies of agencies where nurses work. The art of delegation involves effective communication with members of the health care team.
Communicating Effectively
Charge nurses engage in both horizontal and vertical communication at the unit level. They are seen as the pivotal point person, or go to person. They must master the art of assertive and persuasive communication, as well as develop negotiation and listening skills. Conversations may be initiated by staff, patients, families, physicians, hospital leadership, or by the charge nurses themselves. Information is gathered and processed. Communication outcomes often result in changes in patient treatments plans, transfers to other levels of care, or in facilitating interdisciplinary communication with physicians or other departments. The success of the charge nurses communication efforts is often reflected in staff, patient, and physician satisfaction scores. They are frequently the first stop for any complaint. Charge nurses must also be familiar with the unique communication issues, styles, and preferences related to gender, generation, and cultural dynamics. Additionally, charge nurses must overcome the many distractions which create barriers to communication that prevent them from advocating effectively on behalf of the patients and staff. Effective communication is essential for the reduction of medical errors and promotion of safety practices. Structured techniques which permit assertive clarification of team communication and avoidance of errors can be promoted and role modeled by the charge nurse. Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) is an evidence-based communicaVolume 2, Issue 4 July/August 2009
tion model that has been developed for use in clinical practice with funding from the Agency for Healthcare Research and Quality. Tools in the model include the Two-Challenge Rule, Call-Outs, and Check-Backs (AHRQ). The Two-Challenge Rule requires the communicator to voice their concern at least twice to receive acknowledgment by the receiver. This rule may be invoked when a member of the healthcare team suggests or performs an intervention that deviates from the standard of care. The charge nurse would assertively voice their concern at least two times and if the team member who is being challenged does not acknowledge this concern, the charge nurse would then take a stronger action or utilize the hospital chain of command as needed. Call-Outs are a strategy that the charge nurse can use to inform all team members of crucial information during emergencies to assist team members in anticipating what comes next. For instance, during a stroke alert, the results of the patients NIH scale and the need to transport the patient as rapidly as possible for a CT scan may be communicated out loud to the rest of the team. Check-Backs require the sender of the communication to verify the information that is being received by the other team member, or to use closed-loop communication. For example, the charge nurse is often responsible for verifying that telephone order read backs are performed according to policy. Some communication takes place during times of escalating stress, such as in a rapid response event. Here effective and efficient communication is crucial for successful patient outcomes. Charge nurses can model and demonstrate evidenced based practice by utilizing recognized communication tools such as SBAR (SituationBackground-Assessment-Recommendation) (Institute of Healthcare Improvement). Communication handoffs that promote a shared mental model regarding the patients unique condition are essential (Haig, Sutton, & Whittington, 2006). A shared mental model is the understanding about the current patient situation that is shared among the team (AHRQ). If the team is communicating well, then responses to patient needs will be quicker and deaths due to failure to rescue will be avoided. Staff nurses must be able to trust in the charge nurses ability to assist them to respond to a sudden change in a patients condition. Skilled communication at the unit level is viewed as one measure to balance a culture of safety with the workforce challenges that exist in the current healthcare environment (Hinshaw,
8
2008). When there are communication difficulties at the unit level, it can lead to the development of conflict between one or more team members.
flict should be able to help team members work more effectively together to meet the needs of patients.
Building Team Synergy
Charge nurses play a crucial role in the retention and turnover of registered nurses. As team leaders, they set the tone for unit performance by creating a culture which promotes staff effectiveness and productivity, with the goal of coordinating all components of patient care. The charge nurse is at the core of everything happening on the unit. With increasing patient acuity and shortened lengths of stay, charge nurses are the essential drivers of positive patient outcomes. In environments where staff work 12hour shifts, they are often the only stable force as the other team members are fluid and always changing. Whereas the staff nurse is cued in to their individual patient assignment and isolated tasks, the charge nurse must maintain a more global systems perspective. Charge nurses anticipate the need for crisis intervention, respond to unique individual circumstances, maintain quality standards, and coordinate patient care. Charge nurses can encourage team collaboration and promote the use of interdisciplinary patient rounds. More effective teamwork and coordinated patient handoffs are critical to the promotion of a safe patient care environment (Edwards, 2008; Schmalenberg & Kramer, 2009; Shortell & Singer, 2008). The TeamSTEPPS (AHRQ) model for high functioning teams includes principles from the Crew Resource Management Model (CRM) which originated in the aviation industry (Kosnik, Brown &Maund, 2007). The CRM model is designed to promote effective team management with a goal of addressing errors in dynamic environments that could be caused by ineffective communication in interdependent processes. The charge nurse role is uniquely positioned to guide the team in the use of these strategies. In healthcare, the entire team is responsible for the patient. Charge nurses are at the front lines of patient care, and remain accessible to the staff while facilitating and overseeing the multitude of human interactions which take place in a typical patient care day. As a result, they can provide strong team leadership. This is essential to inspire a clear, shared vision, and to build the necessary trust and confidence necessary to optimize patient and productivity outcomes. Team members who clearly understand their roles and responsibilities can then be proactive, rather than reactive. Effective charge nurses actually create the climate that allows teamwork to happen. The TeamSTEPPS model emphasizes that the charge nurse, as the team leader, must remain both situationally aware and cognizant of the current conditions which may
9
Managing Conflict
Casey Stengel, the beloved manager of many major league baseball teams, once noted that Finding good players is easy. Getting them to play as a team is another story (Stengel). The same could be said of teams in healthcare settings. Communication breakdowns and conflict are inevitable on teams. The results of recent research indicate that few members of healthcare teams are comfortable having the type of crucial conversations that teams need to have when there is conflict or poor performance (Vital Signs, 2005). Guiding team members past their day to day problems, conflicts and communication issues to work together as a team can be challenging for charge nurses. If conflict is managed effectively, it can be viewed as an opportunity for team growth. The necessity of effectively managing team conflict should be framed in terms of a patient safety issue. Root cause analysis studies done by the Joint Commission on Accreditation of Healthcare Organizations since 1995 indicate that a breakdown in communication among caregivers is the top contributor to sentinel events (JCAHO, 2008). Conflict between team members usually evolves from differences in experiences, attitudes, behaviors, and work values. Left unresolved, conflict can cause a loss of productive work time, medical errors, decreased patient satisfaction, and staff turnover (Manion, 2005). Open discussion with staff about differences in attitudes and values is an important first step. Staff may not be willing to consider other viewpoints as legitimate unless they are required to participate in conflict resolution. The following steps in the conflict resolution process can be used to help staff discuss and mediate conflict that involves differences (Moss, 2005): 1. Agree to ground rules for discussion that are acceptable to all parties. 2. Allow each person to tell their story from their perspective. 3. Highlight an overall goal that all team members value example providing the best care possible to our patients 4. Develop interventions collaboratively and agree to disagree on points of contention. 5. Keep the lines of communication open and respect differences in attitudes, values and behaviors. The charge nurses overall goal in the mediation of conVolume 2, Issue 4 July/August 2009
be impacting the work of the team (AHRQ). Briefings are encouraged at the beginning of the shift to plan for patient care, huddles can occur on an as needed basis to problem solve, and timely conflict resolution is recommended. Team members can then assist each other with tasks and provide effective feedback. The charge nurse can then lead debriefings in order to provide crucial feedback after intense patient events, or at the end of the shift. This process promotes performance improvement and encourages all members of the team to learn and grow. Staff members need to feel valued and essential to unit function. Many times nurses go without needed breaks. If nurses are not supported in caring for self, this leads to low staff morale. The charge nurses can assist with seeing that these breaks are taken and heavy workloads are redistributed. An additional stressor is when staff nurses precept orientees or novice nurses. When making assignments, the orientation for new staff must be adjusted for and supported. Although this type of knowledge may not have been formally discussed in their education or training, charge nurses must ensure that the orientation period is adjusted to meet the unique needs of each individual nurse. Leadership attributes of charge nurses should include motivating and inspiring collaboration among team members. Every effort must be made to ensure that adequate resources of staff, supplies, information, and feedback are present. Charge nurses also model promoting the mission and vision of the organization for the team members. Effective leadership by charge nurses at the unit level can then create working conditions which empower the nurses and foster their commitment to the organization (Spence Laschinger, Finegan, & Wilk, 2009).
Summary
Charge nurses play a key role in providing leadership at the point of care on their units. Developing the skills to effectively supervise and delegate, communicate, resolve conflict and build strong team synergy are important success factors. The charge nurse role can be compared to air traffic controllers in the aviation industry. On todays busy and often chaotic patient care units, patients, staff and interdisciplinary team members rely heavily on charge nurses for their guidance and direction. Rising to meet this leadership challenge can provide enormous professional satisfaction and a tremendous leadership growth experience.
References
Agency for Healthcare Research and Quality. (b). TeamSTEPPS. Retrieved July 1, 2009 from http://teamstepss.ahrq.gov Connelly, L.M., Nabarrete, S.R., & Smith, K.K. (2003). A charge
Volume 2, Issue 4 July/August 2009
nurse workshop based on research. Journal for Nurses in Staff Development, 19(4), p. 203-208. Edwards, C. (2008). Using interdisciplinary shared governance and patient rounds to increase patient safety. MEDSURG Nursing, 17(4), 255-257. Federwisch, A. (June 12th, 2008). Whos in charge? Retrieved July 6th, 2009 from http://news.nurse.com/apps/pbcs.dll/article?AID=2008106160049 Haig, K. M., Sutton, S., & Whittington, J. (2006). National patient safety goals. SBAR: A shared mental model for improving communication between clinicians. Joint Commission Journal on Quality and Patient Safety, 32(3), 167-175. Hansten, R.I. (2008). Why nurses still must learn to delegate. Nurse Leader, 6(5), 19-25. Hinshaw, A.D. (2008). Navigating the perfect storm: Balancing a culture of safety with workforce challenges. Nursing Research, 57(1S), S4-10. Hudson, T. (2008). Delegation: Building a foundation for our future nurse leaders. MEDSURG Nursing, 17(6), 396-399, 412. Institute for Healthcare Improvement. SBAR technique for communication: A situational briefing model. Retrieved July 1, 2009 from http://www.ihi.org/IHI/Topics/PatientSafety/ SafetyGeneral/Tools/SBARTechniqueforCommunicationASituatio nalBriefingModel.htm Joint Commission on Accreditation of Health Care Organizations (JCAHO). Root causes of sentinel events. Retrieved June 18th, 2009 from http://www.jointcommission.org/SentinelEvents/ Statistics/ Leary, C. & Allen, S.J. (2006). Navigating the path of leadership: 12 qualities of an effective charge nurse. Nurse Leader, 4(6), 22-23. Manion, J. (2005). Create a positive health care environment. Chicago: Health Forum Inc. Moss, M.T. (2005). The emotionally intelligent nursing leader. San Francisco: Josey-Bass. National Council State Boards of Nursing (NCSBN, 2005). Working with others: Delegation and other health care interfaces. Retrieved June 10th from https://www.ncsbn.org/ 1625.htm Schmalenberg, C. & Kramer, M. (2009). Nurse-physician relationships in hospitals: 20 000 nurses tell their story. Critical Care Nurse, 29(1), 74-83. Sherman, R.O. (2005). Dont forget our charge nurses. Nursing Economics, (3), 125-130, 143. Shortell, S.M. & Singer, S.J. (2008). Improving patient safety by taking systems seriously. JAMA, 299(4), 445447. Spence, Laschinger, H.K., Finegan, J., & Wild, P. (2009). Context matters: The impact of unit leadership and empowerment on nurses organizational commitment. JONA, 39(5), 228-235. Stengel, C. Brainy quotes. Retrieved June 15th, 2009 from http://www.brainyquote.com/quotes/quotes/c/caseysteng38482 2.html Vital SmartsTM (2005). Silence Kills: The Seven Crucial Conversations for Healthcare. Retrieved July 1, 2009 from http://www.silencekills.com/Download.aspx
10
You might also like
- The Secret Language of AttractionDocument278 pagesThe Secret Language of Attractionsandrojairdhonre89% (93)
- Week 2 Case StudyDocument8 pagesWeek 2 Case StudyMelissa Cerny100% (3)
- Charge Nurse WorksheetDocument1 pageCharge Nurse WorksheetFitz JaminitNo ratings yet
- Download 12,000 Shed PlansDocument27 pagesDownload 12,000 Shed PlansRadu_IS100% (2)
- Utilizing Bedside Shift Report To Improve The Effectiveness of Shift HandoffDocument6 pagesUtilizing Bedside Shift Report To Improve The Effectiveness of Shift HandoffselviNo ratings yet
- Difficult IV Access C PGDocument42 pagesDifficult IV Access C PGFitrii WulanDari FitriNo ratings yet
- List of PEGA Interview Questions and AnswersDocument33 pagesList of PEGA Interview Questions and Answersknagender100% (1)
- Charge Nurse GuidelinesDocument97 pagesCharge Nurse GuidelinesLeofe Corregidor100% (1)
- Acute Critical Care Nursing HandoutDocument17 pagesAcute Critical Care Nursing HandoutJulie May100% (6)
- 17 Tips To Improve Your Nursing DocumentationDocument26 pages17 Tips To Improve Your Nursing DocumentationAgustin Lutfiana100% (1)
- Arterial Lines Mark Hammerschmidt, RN FromDocument9 pagesArterial Lines Mark Hammerschmidt, RN FromMark Hammerschmidt100% (3)
- 1990-Fleming Suturing Method and PainDocument7 pages1990-Fleming Suturing Method and PainAnonymous bq4KY0mcWG0% (1)
- Anatomy 090819Document30 pagesAnatomy 090819Vaishnavi GourabathiniNo ratings yet
- The Role of The Registered Nurse As Charge NurseDocument6 pagesThe Role of The Registered Nurse As Charge NurseJaic Ealston D. TampusNo ratings yet
- Nursing's Leading Edges: Advancing the Profession through Specialization, Credentialing, and CertificationFrom EverandNursing's Leading Edges: Advancing the Profession through Specialization, Credentialing, and CertificationNo ratings yet
- The Nurse Manager Accelerator Transition from Bedside Nursing to Nurse Manager in 6 stepsFrom EverandThe Nurse Manager Accelerator Transition from Bedside Nursing to Nurse Manager in 6 stepsNo ratings yet
- Advanced Practice Nursing Leadership: A Global PerspectiveFrom EverandAdvanced Practice Nursing Leadership: A Global PerspectiveNo ratings yet
- Charge Nurse, Reading, Kardex, AnecdotalDocument10 pagesCharge Nurse, Reading, Kardex, AnecdotalAubrey Unique EvangelistaNo ratings yet
- Charge Nurses: How To Be A Great Leader - The Nurse Leader Handbook by Quint Studer Lesson 1 - What Is A Leader?Document21 pagesCharge Nurses: How To Be A Great Leader - The Nurse Leader Handbook by Quint Studer Lesson 1 - What Is A Leader?eman mamdohNo ratings yet
- Critical Care Note PDFDocument10 pagesCritical Care Note PDFlml100% (1)
- Improving Nursing Handoff Process in The Cardiovascular IntensiveDocument77 pagesImproving Nursing Handoff Process in The Cardiovascular IntensiveBheru LalNo ratings yet
- Proper Nursing Documentation WillDocument4 pagesProper Nursing Documentation Willbel_dawn019No ratings yet
- VUMC Preceptor Guide for New GraduatesDocument14 pagesVUMC Preceptor Guide for New GraduatesScheila Mai100% (1)
- Central Venous Catheter Care and ManagementDocument2 pagesCentral Venous Catheter Care and ManagementMissy Wyckoff HartNo ratings yet
- Critical Care Nursing Manuall IDocument90 pagesCritical Care Nursing Manuall ILesley Gonzalez75% (4)
- 50 IV Therapy Tips and TricksDocument10 pages50 IV Therapy Tips and TricksAmar Freebiker Abaza0% (1)
- Improving Bedside Shift-To-shift Nursing Report ProcessDocument34 pagesImproving Bedside Shift-To-shift Nursing Report ProcessJaypee Fabros Edra100% (2)
- Icu NotesDocument47 pagesIcu NotesChryst Louise SaavedraNo ratings yet
- 128 Professional StandardsDocument40 pages128 Professional StandardsPaul BensonNo ratings yet
- A Nurse’s Medicine Basket: Tools for Compassionate Self-CareFrom EverandA Nurse’s Medicine Basket: Tools for Compassionate Self-CareNo ratings yet
- Nurse's Role as Part of an Interprofessional Healthcare TeamDocument11 pagesNurse's Role as Part of an Interprofessional Healthcare TeamOmi EdNo ratings yet
- Ec&fac&pla&sur 6Document448 pagesEc&fac&pla&sur 6Raihan IsvandiarNo ratings yet
- Nurse Student Exercise BookDocument16 pagesNurse Student Exercise BookA GNo ratings yet
- A Guide for the Nurse Entrepreneur: Make a DifferenceFrom EverandA Guide for the Nurse Entrepreneur: Make a DifferenceNo ratings yet
- Advanced Practice Resources Guideline 9.5.13Document23 pagesAdvanced Practice Resources Guideline 9.5.13nunungNo ratings yet
- Career Development For Nurse Managers.9Document5 pagesCareer Development For Nurse Managers.9Pkrs Rsud Provinsi Ntb50% (2)
- Professional Development PowerpointDocument12 pagesProfessional Development Powerpointapi-400385739No ratings yet
- Nursing Bullets Fundamentals ReviewDocument65 pagesNursing Bullets Fundamentals Reviewjoan olanteNo ratings yet
- Patient Education: You Can Do It!: A Practical Guide to Teaching and Motivating PatientsFrom EverandPatient Education: You Can Do It!: A Practical Guide to Teaching and Motivating PatientsNo ratings yet
- Managing Change Towards Bedside Shift ReportDocument12 pagesManaging Change Towards Bedside Shift Reportapi-438607141No ratings yet
- CNL Final Exam Study GuideDocument15 pagesCNL Final Exam Study GuideGelsey Gelsinator JianNo ratings yet
- Critical Care Nursing EssentialsDocument42 pagesCritical Care Nursing Essentialsikram ullah khanNo ratings yet
- Mastering ICU Nursing: A Quick Reference Guide, Interview Q&A, and TerminologyFrom EverandMastering ICU Nursing: A Quick Reference Guide, Interview Q&A, and TerminologyNo ratings yet
- Nurse Commitment: How to Retain Professional Staff Nurses in a Multigenerational WorkplaceFrom EverandNurse Commitment: How to Retain Professional Staff Nurses in a Multigenerational WorkplaceNo ratings yet
- Standards For Wound Prevention and Management 2016Document66 pagesStandards For Wound Prevention and Management 2016sidney drecotteNo ratings yet
- New Grad Nurse Career Success Resource PacketDocument18 pagesNew Grad Nurse Career Success Resource Packetapi-290351537100% (1)
- Nursing AssessmentDocument28 pagesNursing AssessmentKierstine Joy YamatNo ratings yet
- Critical Care Nursing ClinicsDocument133 pagesCritical Care Nursing ClinicsJune DumdumayaNo ratings yet
- Welcome TO Intensive Care UnitDocument42 pagesWelcome TO Intensive Care UnitKharene Lirazan100% (1)
- Clinical Nursing Journal CapstoneDocument7 pagesClinical Nursing Journal Capstoneapi-455776552No ratings yet
- Perianesthesia Nursing Standards of Practice Jennifer J SmithDocument11 pagesPerianesthesia Nursing Standards of Practice Jennifer J Smithapi-239605726No ratings yet
- Wound - Wound CareDocument189 pagesWound - Wound CareMoenaIsmailNo ratings yet
- ICU Basic Critical Care For NursesDocument8 pagesICU Basic Critical Care For Nursesarv rskoNo ratings yet
- Heart Nursing: Learn, Grow & Succeed in the First Year of PracticeFrom EverandHeart Nursing: Learn, Grow & Succeed in the First Year of PracticeRating: 4 out of 5 stars4/5 (1)
- ACAQ Crit Care Nursing CurriculumDocument91 pagesACAQ Crit Care Nursing CurriculumAnne Julia Agustin100% (1)
- Nur 862 Clinical Competencies PortfolioDocument11 pagesNur 862 Clinical Competencies Portfolioapi-457407182No ratings yet
- WHNP CoalitionDocument1 pageWHNP CoalitionAnonymous bq4KY0mcWGNo ratings yet
- Wellness Nutritionforwomenslides PDFDocument16 pagesWellness Nutritionforwomenslides PDFAnonymous bq4KY0mcWGNo ratings yet
- Wet Mount Proficiency Test 2007A CritiqueDocument6 pagesWet Mount Proficiency Test 2007A CritiqueAnonymous bq4KY0mcWGNo ratings yet
- Wet Mount Proficiency 2008A Critique2Document4 pagesWet Mount Proficiency 2008A Critique2Anonymous bq4KY0mcWGNo ratings yet
- Wellness Nutritionforwomenslides PDFDocument16 pagesWellness Nutritionforwomenslides PDFAnonymous bq4KY0mcWGNo ratings yet
- Kennedy-Model of Exemplary Midwifery PracticeDocument16 pagesKennedy-Model of Exemplary Midwifery PracticeAnonymous bq4KY0mcWGNo ratings yet
- Suture Types PDFDocument2 pagesSuture Types PDFAnonymous bq4KY0mcWGNo ratings yet
- WHNP Research PrioritiesDocument18 pagesWHNP Research PrioritiesAnonymous bq4KY0mcWGNo ratings yet
- Erwin-Demystifying The Nurse-Midwifery MGMT Process 1987Document7 pagesErwin-Demystifying The Nurse-Midwifery MGMT Process 1987Anonymous bq4KY0mcWGNo ratings yet
- Beebe - Expectations, Perceptions, and Management of Labor in Nulliparas Prior To HospitalizationDocument7 pagesBeebe - Expectations, Perceptions, and Management of Labor in Nulliparas Prior To HospitalizationAnonymous bq4KY0mcWGNo ratings yet
- A Healthy Menopause: Diet, Nutrition and Lifestyle GuidanceDocument8 pagesA Healthy Menopause: Diet, Nutrition and Lifestyle GuidanceAnonymous bq4KY0mcWGNo ratings yet
- Greulich - The Latent Phase of Labor-Diagnosis and ManagementDocument9 pagesGreulich - The Latent Phase of Labor-Diagnosis and ManagementAnonymous bq4KY0mcWGNo ratings yet
- King & Pinger, Pearls of Midwifery PDFDocument14 pagesKing & Pinger, Pearls of Midwifery PDFAnonymous bq4KY0mcWGNo ratings yet
- LOC Certificate For 'Assessing COPD in Primary Care - 0.5 Credit PDFDocument1 pageLOC Certificate For 'Assessing COPD in Primary Care - 0.5 Credit PDFAnonymous bq4KY0mcWGNo ratings yet
- Shingles - Patient Information PDFDocument4 pagesShingles - Patient Information PDFAnonymous bq4KY0mcWGNo ratings yet
- Fetal DevelopmentDocument4 pagesFetal DevelopmentAnonymous bq4KY0mcWGNo ratings yet
- Shingles - Patient Information PDFDocument4 pagesShingles - Patient Information PDFAnonymous bq4KY0mcWGNo ratings yet
- Statin Drug Interaction Pocket GuideDocument6 pagesStatin Drug Interaction Pocket GuideAnonymous bq4KY0mcWGNo ratings yet
- Clinical Pearls and Memory Aids for PediatriciansDocument26 pagesClinical Pearls and Memory Aids for PediatriciansAnonymous bq4KY0mcWGNo ratings yet
- Special Report: Vitamins and MineralsDocument8 pagesSpecial Report: Vitamins and MineralsAnonymous bq4KY0mcWGNo ratings yet
- A Healthy Menopause: Diet, Nutrition and Lifestyle GuidanceDocument8 pagesA Healthy Menopause: Diet, Nutrition and Lifestyle GuidanceAnonymous bq4KY0mcWGNo ratings yet
- Health Maintenance PostmenopauseDocument9 pagesHealth Maintenance PostmenopauseAnonymous bq4KY0mcWGNo ratings yet
- Critical Drug InteractionsDocument5 pagesCritical Drug InteractionsAnonymous bq4KY0mcWGNo ratings yet
- Lisinopri - CHF Dose Conversion For ARBsDocument1 pageLisinopri - CHF Dose Conversion For ARBsAnonymous bq4KY0mcWGNo ratings yet
- JNC 8 Guideline Algorithm for Treating HypertensionDocument2 pagesJNC 8 Guideline Algorithm for Treating HypertensionTaradifaNurInsi0% (1)
- 2017 JNC 8 Lipid and HTN GuidelinesDocument28 pages2017 JNC 8 Lipid and HTN GuidelinesAnonymous bq4KY0mcWGNo ratings yet
- 1APHA2012HVNAslide2012 10 23handoutDocument34 pages1APHA2012HVNAslide2012 10 23handoutAnonymous bq4KY0mcWGNo ratings yet
- Group B Strep and Pregnancy: Frequently Asked Questions FAQ105 PregnancyDocument3 pagesGroup B Strep and Pregnancy: Frequently Asked Questions FAQ105 PregnancyAnonymous bq4KY0mcWGNo ratings yet
- HP1Document5 pagesHP1Qusay AliraqiNo ratings yet
- The Daily Tar Heel For September 18, 2012Document8 pagesThe Daily Tar Heel For September 18, 2012The Daily Tar HeelNo ratings yet
- Remembrance 23 Names PDFDocument1 pageRemembrance 23 Names PDFJennifer ThuncherNo ratings yet
- Unitisation of Legal Methodsalsdkgh GHNJFKL A SDFG LKJH Asdfgf Lkjhasdfg LKKJ Asdfg LKJH A Slkjfs Aaaaaaaaaaaaslkdfj Asldkjf SLDKFJDocument3 pagesUnitisation of Legal Methodsalsdkgh GHNJFKL A SDFG LKJH Asdfgf Lkjhasdfg LKKJ Asdfg LKJH A Slkjfs Aaaaaaaaaaaaslkdfj Asldkjf SLDKFJKailashnath Reddy AjjuguttuNo ratings yet
- 7 Tools for Continuous ImprovementDocument202 pages7 Tools for Continuous Improvementvivekanand bhartiNo ratings yet
- IntuitionDocument10 pagesIntuitionmailsonNo ratings yet
- Italian Painters 02 MoreDocument450 pagesItalian Painters 02 Moregkavvadias2010No ratings yet
- Potato Peroxidase LabDocument2 pagesPotato Peroxidase LabKarla GutierrezNo ratings yet
- OM - Rieter - UNIMix A76Document321 pagesOM - Rieter - UNIMix A76Phineas FerbNo ratings yet
- Intraoperative Nursing Care GuideDocument12 pagesIntraoperative Nursing Care GuideDarlyn AmplayoNo ratings yet
- OTGNNDocument13 pagesOTGNNAnh Vuong TuanNo ratings yet
- L P 10Document13 pagesL P 10Bình Minh HoàngNo ratings yet
- Sample of Accident Notification & Investigation ProcedureDocument2 pagesSample of Accident Notification & Investigation Procedurerajendhar100% (1)
- ANAPHYDocument23 pagesANAPHYYu, Denise Kyla BernadetteNo ratings yet
- Joel Werner ResumeDocument2 pagesJoel Werner Resumeapi-546810653No ratings yet
- Practical Finite Element Simulations With SOLIDWORKS 2022Document465 pagesPractical Finite Element Simulations With SOLIDWORKS 2022knbgamageNo ratings yet
- Statement Bank MBBDocument11 pagesStatement Bank MBBminyak bidara01No ratings yet
- Focus Group Discussion PDFDocument40 pagesFocus Group Discussion PDFroven desu100% (1)
- Horizontal Vertical MarketDocument4 pagesHorizontal Vertical MarketVikasNo ratings yet
- Lazo v. Judge TiongDocument9 pagesLazo v. Judge TiongKing BadongNo ratings yet
- Trishasti Shalaka Purusa Caritra 4 PDFDocument448 pagesTrishasti Shalaka Purusa Caritra 4 PDFPratik ChhedaNo ratings yet
- Tutorial Backpropagation Neural NetworkDocument10 pagesTutorial Backpropagation Neural NetworkHeru PraNo ratings yet
- PS Neo HSK2LCD ICON LED RF Keypad v1 0 Installation Guide R001 en FR Es PoDocument40 pagesPS Neo HSK2LCD ICON LED RF Keypad v1 0 Installation Guide R001 en FR Es Po7seguridadNo ratings yet
- A. Hardened Concrete (Non-Destructive Tests) : The SAC Programme Is Managed by Enterprise SingaporeDocument2 pagesA. Hardened Concrete (Non-Destructive Tests) : The SAC Programme Is Managed by Enterprise Singaporeng chee yongNo ratings yet
- Cat TSDDocument55 pagesCat TSDvarsha sharmaNo ratings yet
- EMarketer Time Spent With Media SnapshotDocument13 pagesEMarketer Time Spent With Media SnapshotWei ShingNo ratings yet
- Strategy 13 Presentation - Social Emotional LearningDocument29 pagesStrategy 13 Presentation - Social Emotional Learningapi-588940234No ratings yet