Professional Documents
Culture Documents
Drowning
Uploaded by
AidaDenisse Negrete DurazoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drowning
Uploaded by
AidaDenisse Negrete DurazoCopyright:
Available Formats
Article
respiratory
Childhood Drowning
Robyn J. Meyer, MD, MS,* Andreas A. Theodorou, MD,* Robert A. Berg, MD*
Objectives
After completing this article, readers should be able to:
Author Disclosure Drs Meyer, Theodorou, and Berg did not disclose any nancial relationships relevant to this article.
1. List preventive efforts that may decrease drowning rates in the pediatric population. 2. Name the physiologic consequences of hypoxic-ischemic injury in drowning victims. 3. Explain the importance of bystander cardiopulmonary resuscitation for pediatric drowning victims. 4. Discuss the appropriate interventions for each stage of drowning-associated cardiac arrest. 5. Specify which pediatric drowning victims may be discharged from the emergency department.
Denitions
Terminology used to describe drowning often has been confusing and inconsistent. To alleviate this confusion, an international consensus conference was convened at the 2002 World Congress on Drowning with the goal of developing uniform terminology. The recently published recommendations dene drowning as a process resulting in primary respiratory impairment from submersion/immersion in a liquid medium. (Idris et al. 2003) Accordingly, the term drowning should be used regardless of the outcome. In addition, the consensus document specically recommends that confusing and inconsistent terms, such as near-drowning, secondary drowning, passive drowning, silent drowning, wet drowning, and dry drowning be abandoned.
Epidemiology
Drowning is a major source of pediatric mortality and morbidity worldwide. Although differences in lifestyle and exposure to water may affect the circumstances under which drowning occurs in different countries, drowning consistently remains a leading cause of death throughout the world. In the United States in 1998, more than 1,500 children younger than 20 years of age died from drowning, making it the second leading cause of accidental childhood death. For children 12 to 23 months of age, drowning was the leading cause of accidental death and the second leading cause of death overall. There is less information concerning morbidity, but it is estimated that for each drowning death, there are one to four nonfatal drowning events requiring hospitalization. Such hospitalizations often result in prolonged disability requiring considerable monetary and emotional resources. Within the pediatric population, rates of drowning peak during both the toddler and adolescent years. Age also inuences the circumstances of drowning. Among younger children, drowning usually occurs within the home, often during brief lapses in adult supervision. Infants drown in bathtubs most frequently, either when they are left unattended or as the result of abusive injury. Toddlers typically drown in swimming pools. For both infants and toddlers, physical and cognitive immaturity limits their ability to rescue themselves from water. Adolescent drowning frequently occurs in natural bodies of water and is associated with risk-taking behavior and intoxication. Although most drownings occur in previously healthy children, certain pre-existing medical conditions may play a role. Children who have seizure disorders have a risk of drowning four times that of the general population. Cardiac arrhythmias have been
*The University of Arizona Steele Memorial Childrens Research Center, Tucson, Ariz. Sarver Heart Center, Tucson, Ariz. Pediatrics in Review Vol.27 No.5 May 2006 163
respiratory
childhood drowning
implicated in a small number of drowning deaths. Swimming, particularly diving in cold water, may serve as a trigger for some patients who have long QT syndrome.
Prevention
Drowning rates have been declining over the past 20 years, primarily due to improved preventive efforts. However, much remains to be accomplished, and prevention remains the key to further reductions in both mortality and morbidity. It is estimated that in spite of recent efforts, 80% of drownings remain preventable. Optimal preventive efforts vary by age group. Adult supervision of infants and young children around water is a major focus of preventive efforts, but supervision is not foolproof. A child can enter the water during a brief lapse in the supervisors attention. Adults may assume that they will hear sounds of splashing or struggling as a drowning occurs, but most childhood drownings are silent. Therefore, multiple layers of prevention, with barriers between the child and water, are recommended. Proper pool fencing that includes a self-closing, latching gate should surround the pool completely. Such fencing can reduce the incidence of drowning by 50% to 80%. Prevention for adolescents should focus on water safety education, including the dangers of intoxication while in and around the water. Although swimming lessons are presumed to improve water safety, no data demonstrate that they actually decrease the risk of drowning. Importantly, swimming skills cannot make a child drown-proof under all conditions. In addition, swimming programs are not developmentally appropriate for children younger than 4 years of age, according to the American Academy of Pediatrics.
duration of submersion, the asphyxial insult inevitably results in cardiac arrest. Lung injury in drowning patients is characterized by abnormal surfactant function and increased capillary endothelial permeability. This injury leads to increased intrapulmonary shunting, ventilation/perfusion mismatch, atelectasis, and poor lung compliance, which cause further hypoxemia and hypercarbia. When severe enough, this process may lead to acute respiratory distress syndrome (ARDS). Contrary to earlier beliefs, pulmonary injuries from fresh water and saltwater drowning typically do not differ substantially. Moreover, clinically signicant electrolyte abnormalities are relatively uncommon after either fresh water or saltwater drowning. Nevertheless, hyponatremia can occur with fresh water drownings and hypernatremia with saltwater drownings. The most devastating consequence of drowning and the most frequent cause of death is hypoxic-ischemic injury to the brain. The degree of central nervous system injury is related to the duration of untreated cardiac arrest, the effectiveness of initial cardiopulmonary resuscitation (CPR), and secondary cerebral injuries after resuscitation (eg, further hypoxic episodes, inadequate cerebral blood ow, cerebral edema, and hyperthermia).
Clinical Diagnosis and Management
The critical moment in the care of the severely affected drowning victim generally occurs before he or she comes to the attention of medical professionals. The most important determinants of neurologically normal survival are prompt rescue from the water and immediate institution of effective basic life support. Because time is the crucial element, bystander rescue and resuscitation are the most important interventions. Delays in rescue and resuscitation often are lethal. Sadly, although early effective CPR is key to survival, only about 30% of pediatric cardiac arrest victims, including drowning victims, receive bystander CPR.
Pathogenesis
The physiologic consequences of drowning are due primarily to hypoxic-ischemic and reperfusion injuries. The devastating long-term neurologic consequences of drowning occur almost exclusively among patients who have drowning-associated asphyxial cardiac arrests. Patients who do not experience cardiac arrest rarely have signicant sequelae. Drowning-associated asphyxia is caused by laryngospasm, apnea, or pulmonary aspiration of water. Furthermore, when the victim loses consciousness, he or she may vomit and aspirate swallowed water. The resultant hypoxia, hypercarbia, and acidosis can decrease myocardial contractility, elevate pulmonary artery and systemic vascular resistance, and produce cardiac arrhythmias (bradycardia, asystole, ventricular brillation). With sufcient
164 Pediatrics in Review Vol.27 No.5 May 2006
Resuscitation
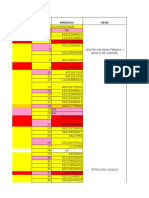
It is increasingly clear that there are four stages of cardiac arrest: prearrest, the no-ow stage of untreated arrest, the low-ow stage of CPR, and postresuscitation (Table). Interventions prearrest include drowning prevention efforts and rescue interventions (removal from the water and rescue breathing). Prompt institution of bystander CPR can shorten the untreated arrest stage, and provision of effective CPR can improve the outcome during the low-ow CPR stage. Finally, anticipating and minimizing secondary injuries are important issues postresuscitation.
respiratory
childhood drowning
stroke volume. During CPR, the primary determinant of stroke volume is the force of chest compressions; the only determinant of heart Stage Intervention rate is the rate of compressions. Prearrest Prevention Chest compressions should be pro Adequate supervision vided by pressing the lower half of Pool fencing the sternum to a relative depth of Water safety education one third to one half of the No-Flow Rapid rescue anterior-posterior diameter of the Prompt bystander cardiopulmonary resuscitation (CPR) Low-Flow (CPR) Effective CPR chest at a rate of approximately 100 Push Hard compressions/min. Properly per Push Fast formed CPR can achieve cardiac Minimize Interruptions outputs of approximately 10% to CPR training 15% of normal, which can be sufPostresuscitation Advanced Life Support Specialized pediatric facilities and personnel cient for successful resuscitation. Continuous cardiorespiratory monitoring During every interruption in chest Meticulous supportive care compressions, cardiac output ceases, Consideration of therapeutic hypothermia and there is no blood ow to the heart or brain. Therefore, the mantra for adequate cardiac output durThe hypoxia and ischemia that occur during drowning CPR is: PUSH HARD, PUSH FAST, and minimize ing can result in severe myocardial dysfunction, manifestinterruptions. ing clinically as shock. If rescue efforts are not provided, Although the electrocardiography (ECG) tracing of the hypoxic-ischemic shock soon is followed by complete most pulseless drowning victims shows either bradycarcardiac arrest. With either severe hypoxic-ischemic shock dia or asystole, ventricular brillation is not uncommon. or cardiac arrest, the victim may be clinically unresponBecause denitive treatment of ventricular brillation sive, exhibit apnea, and have no pulse. Prompt CPR with requires debrillation, early ECG assessment is indicated. mouth-to-mouth rescue breathing and effective chest The child should be transported to a facility where compressions can be lifesaving. advanced life support can be provided. Pediatric emerAt the earlier phase of hypoxic-ischemic shock, either gency care clinicians should be prepared for the immedirescue breathing alone or chest compressions alone can ate critical care needs of drowning victims. For many be lifesaving (although the combination is superior). practitioners outside of a hospital and in many emerAccordingly, some bystander resuscitation is better than gency departments, care of a pediatric drowning victim is no bystander resuscitation. After full cardiac arrest, the an unusual occurrence. Preparation for relatively rare combination of chest compressions plus rescue breathing occurrences is difcult. The availability of clinicians who generally is needed for successful resuscitation. The Heimhave appropriate pediatric equipment, as well as pediatric lich maneuver or other attempts to clear the airway of emergency experience and expertise, increases the likeliwater not only are ineffective, but frequently are detrimenhood of successful resuscitation. tal by inducing emesis and aspiration of gastric contents. Comprehensive evaluation and treatment should beAfter opening the airway with the head tilt-chin lift gin immediately upon arrival at the hospital. In addition maneuver, two mouth-to-mouth rescue breaths should to rapid cardiopulmonary assessment focusing on evibe provided. Single rescuers should provide two rescue dence of shock, the drowning victim should be evaluated breaths before each cycle of 30 chest compressions. New for hypothermia and associated trauma as well as for signs information from animal models suggests that rescue of neurologic and pulmonary injury. Drowning events breathing at an excessive rate can impede venous return encompass a wide range of severity. The patient may have during CPR and possibly worsen outcome. Consequently, had a brief immersion with no clinical sequela or a rescue breathing at rates much higher than 20 breaths/min prolonged episode resulting in full cardiopulmonary argenerally should be avoided. rest and all the associated complications. The goal of chest compressions is to maximize cardiac In nearly all instances, CPR should be continued until output. Cardiac output is the product of heart rate and spontaneous circulation has returned or until resuscitaTable.
Pediatrics in Review Vol.27 No.5 May 2006 165
Interventions for Drowning-associated Cardiac Arrest
respiratory
childhood drowning
tion is demonstrated to be futile. Although aggressive resuscitation may result in neurologically devastated survivors, no predictive factors can determine early in resuscitation who will or will not do well. All factors used to predict dismal outcomes are imperfect; some children have had unexpected full recoveries despite predictors of certain death or devastation. Good outcomes have been reported after submersion for more than 1 hour, when body temperatures were 56.7F (13.7C), or when the pH was 6.29. Due to this uncertainty, it generally is recommended that all drowning victims receive aggressive care for the rst 24 hours until the prognosis can be better determined.
Shock
Following initial resuscitation, patients often remain in shock, as evidenced by inadequate tissue perfusion. Clinical signs of shock include tachycardia, altered level of consciousness, poor peripheral pulses and perfusion, oliguria, and acidosis. Even when the child is normotensive, he or she may be in a state of compensated shock. Hypotension is the fundamental indicator of uncompensated shock. Following a drowning episode, shock commonly results from postresuscitation myocardial dysfunction, with poor cardiac output due to acidosis and hypoxemia. Fluid shifts with resultant intravascular hypovolemia also may contribute to cardiac instability. Appropriate management requires careful, continuous hemodynamic monitoring. Inotropic support and uid resuscitation typically are needed to treat postdrowning shock.
severe hypothermia ( 82F [28C]). Rewarming should be considered for moderate hypothermia (82 to 90F [28 to 32C]) for children who have cardiovascular instability or shock-related coagulopathy. There are three types of rewarming. Passive warming, whereby the patient is kept warm and protected from wind and cold, can be initiated at the scene but is inadequate in the face of signicant hypothermia. Active external warming such as by warmed air or heat packs may cause surface vasodilatation, leading to cardiovascular instability. The gold standard for warming patients who have cardiac arrest or ongoing cardiovascular instability is active internal warming, most commonly with cardiopulmonary bypass or extracorporeal life support. Arteriovenous circulation and body cavity lavage (peritoneal, bladder, pleural, gastric) are other methods of active internal warming that have been described in case reports as being effective. Whether therapeutic hypothermia or rewarming is the treatment of choice, hyperthermia should be avoided and treated aggressively.
Trauma
Drowning may occur during traumatic events such as diving, boating, or motor vehicle accidents that result in submersion. In these scenarios, other traumatic injuries must be considered and full trauma evaluation performed. Computed tomography (CT) scans may be useful to diagnose occult cervical spine, intracranial, or intra-abdominal injury. Except in these settings, cervical spine injury in a drowning victim is uncommon. A recent study demonstrated that cervical spine injuries during drowning only occurred when the history or physical examination ndings evidenced high-impact trauma.
Hypothermia
Dramatic recoveries following icy water drownings are well documented, but hypothermia after drowning in non-icy water is strongly associated with prolonged submersion and a consequent poor prognosis. Decisions regarding treatment of drowning-related hypothermia must take into account several factors. Maintenance of mild hypothermia may be indicated in some cases. Exciting evidence suggests that induced mild hypothermia after resuscitation can improve outcome for adults after cardiac arrest with ventricular brillation. In addition, there are numerous remarkable case reports of children who had excellent outcomes after prolonged submersion in ice water. Although more investigation is needed, maintenance of hypothermia (90 to 93F [32 to 34C]) for 12 to 24 hours is a reasonable therapeutic option for children who remain comatose but who are cardiovascularly stable following return of spontaneous circulation. Rewarming should be provided to children who have
166 Pediatrics in Review Vol.27 No.5 May 2006
Hypoxia-Ischemia
The brain is the organ most susceptible to hypoxicischemic injury. Unfortunately, the initial neurologic examination on presentation often is of limited use in predicting outcome. Although children who have normal initial examination ndings continue to have normal ndings, children who present comatose or severely impaired require serial examinations over the following 24 hours to clarify the prognosis. Those who survive and have a good outcome generally demonstrate spontaneous, purposeful movement and normal brainstem function in the rst 24 hours. Measures specically directed to limiting neurologic injury in the postresuscitation phase have not yet demonstrated benets for drowning victims. Immediate resuscitation and therapeutic hypothermia are the only measures shown to reduce brain damage in the setting of
respiratory
childhood drowning
hypoxic-ischemic injury. There is no proof of benet from pharmacologic therapies, intracranial pressure monitoring, or treatments to reduce intracranial pressure. Optimal supportive care, with attention to adequate oxygen delivery and prompt treatment of seizures, is important to avoid secondary hypoxic-ischemic damage. Hypoglycemia can have detrimental neurologic effects and should be avoided (and treated promptly when it does occur). Hyperglycemia also is associated with worse neurologic outcomes, but it is not clear whether treatment of hyperglycemia improves neurologic outcomes.
Pulmonary Involvement
Mechanical ventilation should be directed toward providing normocarbia and adequate oxygenation to injured tissues. Hypercarbia that can increase cerebral blood ow and severe hypocarbia that can result in cerebral ischemia can be deleterious in the postdrowning setting. It is important to provide adequate support while also avoiding either atelectasis or overdistention. Management of mechanical ventilation may be particularly complex in the initial hours after drowning when dynamic changes in lung compliance, airway resistance, and cardiovascular status are common. In this setting, innovative modes of ventilation, including pressure-limited ventilation, airway pressure release ventilation, and high-frequency oscillation, may be benecial. Chest radiography may be useful to detect pulmonary involvement, although when abnormalities are seen, they often are nonspecic. Pneumonia should be considered in the presence of inltrates or consolidation on chest radiography accompanied by leukocytosis, fever, and purulent secretions. Prophylactic antibiotics generally are not indicated. However, for the patient who develops signs of pneumonia, a bacterial cause should be aggressively sought and treated. It is noteworthy that Aeromonas can cause a severe pneumonia that develops rapidly after drowning. In the face of clinical pneumonia without culture-proven etiology, antibiotic coverage should be directed toward the nosocomial ora that are prevalent in the institution. ARDS may occur due to the alveolar-capillary insult imposed by drowning-related lung injury. In addition to drowning, ARDS can result from any process that directly or indirectly injures the lung, including pneumonia, aspiration, lung contusion, smoke inhalation, blood product transfusion, and sepsis. A delay of hours to days between the initial injury and the development of ARDS in other settings is typical, but evidence of ARDS usually occurs more promptly in the setting of drowning-related lung injury.
The diagnostic triad of ARDS is noncardiogenic pulmonary edema, impaired oxygenation, and bilateral pulmonary inltrates. Clinical manifestations include tachypnea, decreased lung compliance, and worsening hypoxemia leading to respiratory muscle fatigue. The natural history of ARDS consists of three stages. The initial exudative stage characterized by rapid development of respiratory failure can progress to an inammatory stage characterized by brosing alveolitis and surfactant deciency. In the setting of drowning-related acute lung injury, surfactant washout or destruction of surfactant during the drowning event may result in surfactant deciency earlier in the process. The nal stage of ARDS is resolution; many patients recover normal lung function, although residual brosis may be present in others. Corticosteroids are not indicated acutely for drowning-induced lung disease, but high-dose intravenous glucocorticoids can be benecial for ARDS that is not resolving. Mortality rates in ARDS patients are high, but the immediate cause of death typically is sepsis or multiple organ system failure rather than respiratory failure.
Other Organ Involvement
Renal and hepatic damage and dysfunction also may occur with drowning. The clinical appearance of these injuries often is delayed 24 to 72 hours after the initial hypoxic-ischemic insult. Hepatic injury typically is revealed by elevated transaminase concentrations and, if severe, may include impaired liver function with an elevated bilirubin value, decreased albumin concentration, and prolonged clotting times. The renal injury may manifest as acute tubular necrosis with elevated creatinine and oliguria or anuria. Attention to a multitude of details involving diverse organ systems is essential to prevent complications in the severely injured drowning victim. When possible, affected children generally should receive their care in a pediatric intensive care unit. In addition, the long-term outcome of the neurologically impaired drowning victim may be improved with a comprehensive rehabilitation program. Clearly, not all children who suffer a drowning episode require resuscitation or intensive care unit care, and routine admission is not necessary. A large number of children may be asymptomatic or only mildly symptomatic after being retrieved from the water. Children who require no resuscitation and have Glasgow Coma Scale scores greater than 13 on arrival at the emergency department may be candidates for discharge to home after full evaluation and a period of observation. If oxygen saturation and the physical examination ndings remain normal by 6 to 8 hours, these children can be discharged
Pediatrics in Review Vol.27 No.5 May 2006 167
respiratory
childhood drowning
with close follow-up. Late electrolyte changes or neurologic decompensation rarely are seen in these children. Some otherwise normal children may require admission for safety concerns related to the drowning incident. The use of chest radiography is debated. Because a chest radiograph is not a reliable predictor of the clinical course, it is not essential in asymptomatic children. Some sources advocate normal chest radiographic ndings as a requirement for discharge from the emergency department; others believe that abnormalities on chest radiography should not be used as the sole indicator for hospitalization.
Prognosis
The search for predictive factors in drowning victims to guide the aggressiveness of resuscitation has been difcult. The outcome of drowning is closely related to the duration of submersion. When submersion extends beyond 25 minutes, prospects for functional recovery generally have been dismal. However, there are case reports of children surviving neurologically intact after prolonged drowning, particularly in icy water. These case reports tend to indicate the need for aggressive intervention. In addition, accurate determinations of submersion times usually are not available. Aggressive resuscitation provides the best chance for good survival, but also may lead to increased numbers of neurologically devastated survivors. Several investigators have sought early indicators of poor outcome, including coma, xed and dilated pupils, low Glasgow Coma Scale score, and scoring systems based on initial presentation. However, no one factor or combination of factors has consistently predicted ultimate outcomes. Unfortunately, studies have been relatively few, and those that have been published included small numbers of surviving patients. These issues deserve further investigation. For patients who survive initial resuscitation, the ability to predict their outcome improves over time. In one important study, all survivors who eventually had favorable neurologic outcomes showed spontaneous, purposeful movement within 24 hours of admission. These patients recovered normal neurologic status or had minor decits such as seizures, motor decits, or learning disabilities amenable to rehabilitation. However, the extent of subtle neuropsychological sequelae in patients who have mild hypoxic-ischemic injuries has not been well studied. Neurologic outcome in patients who remained without purposeful movement at 24 hours after admission for a drowning incident was dismal. These children exhibited severe neurologic decits, including spasticity, persistent vegetative states, or lack of self-help
168 Pediatrics in Review Vol.27 No.5 May 2006
skills. Serial neurologic examinations may be the most useful source of information to predict the outcome of drowning injury. Although the brain is the organ affected most by drowning, chronic pulmonary morbidity also may occur. Children may develop new-onset reactive airway disease. Severe chronic lung disease is a rare sequela of childhood drowning. The outcomes of pediatric drowning-associated cardiac arrests tend to be considerably better than those from other out-of-hospital pediatric cardiac arrests. For example, in King County, Washington, the survival rate in the pediatric population following prehospital cardiac arrest was 32% for drowning victims compared with 7% for all other causes of cardiac arrest.
Conclusion
Drowning is a leading cause of pediatric morbidity and mortality throughout the world. Poor outcomes are due largely to drowning-associated cardiac arrest with resultant neurologic injury. The most important intervention to improve outcome from drowning is prevention. Preventive efforts should focus on adequate supervision, pool fencing legislation, and water safety education. Once drowning has occurred, rapid water rescue and provision of effective bystander CPR are critical to limit the duration of hypoxic-ischemic injury. To that end, pediatricians should support the promotion and teaching of CPR. In the postresuscitation stage, continuous cardiorespiratory monitoring and supportive care are the mainstays of care. Further research is needed to identify ways to improve educational interventions regarding water safety, to encourage bystander CPR, and to improve postresuscitation care for critically ill children.
Suggested Reading
Dowd MD, Keenan HT, Bratton SL. Epidemiology and prevention of childhood injuries. Crit Care Med. 2002;30(suppl):S385S392 Ibsen LM, Koch T. Submersion and asphyxial injury. Crit Care Med. 2002;30(suppl):S402S408 Idris AH, Berg RA, Bierens J, et al. Recommended guidelines for uniform reporting of data from drowning: the Utstein style. Resuscitation. 2003;59:4557 Orlowski JP, Szpilman D. Drowning: rescue, resuscitation, and reanimation. Pediatr Clin North Am. 2001;48:627 646 Pepe PE, Wiggington JG, Mann DM, et al. Prospective, decadelong, population-based study of pediatric drowning-related incidents. Acad Emerg Med. 2002;9:516 517 Quan L, Wentz K, Gore EJ, Copass MK. Outcome and predictors of outcome in pediatric submersion victims receiving prehospital care in King County, Washington. Pediatrics. 1989;83: 10351040
respiratory
childhood drowning
PIR Quiz
Quiz also available online at www.pedsinreview.org. 1. You are invited to speak to a group of high school seniors regarding safety and prevention of childhood accidents. Of the following, the best means of preventing drowning in a home swimming pool is by: A. B. C. D. E. Barring children who cannot swim from the pool area. Drown-proong toddlers by having them take swimming lessons. Emphasizing that children never be left unattended near a body of water. Installing a fence that has a self-closing, latching gate surrounding the entire pool area. Installing an alarm system that detects water movement in the pool when it is unattended.
2. You are lecturing at a local community adult education class about drowning accidents. Of the following, the best immediate action to be taken by a bystander when a toddler is rescued from a swimming pool and is found to be limp and unconscious with infrequent, gasping respiration is to: A. B. C. D. E. Call the local emergency telephone number for further management. Immobilize the cervical spine by holding the neck in a neutral position. Initiate mouth-to-mouth breathing with chest compressions. Keep the child prone and administer four back blows. Perform the Heimlich maneuver to expel aspirated water.
3. A 2-year-old boy is brought to the emergency department after a drowning accident in a home swimming pool. The submersion time is estimated to be 2 minutes. He was resuscitated at the pool side by his neighbor and subsequently by the emergency medical technicians during transport to the hospital. On arrival at the hospital, he is receiving manual ventilation through the endotracheal tube. His heart rate is 120 beats/min, blood pressure is 100/60 mm Hg, and rectal temperature 95F (35C). Arterial blood gases are: pH, 7.08; PaCO2, 42 torr; and PaO2, 122 torr. He is comatose, does not respond to verbal stimulation, and exhibits nonpurposeful exion withdrawal to pain. His pupils are equal and reactive. Neurologic examination 12 hours after the accident shows spontaneous eye opening and purposeful response to verbal and tactile stimulation. Of the following, the best prognostic indicator of his future neurologic outcome is: A. B. C. D. E. Immediate CPR at the pool side and during transport. Normal oxygenation, ventilation, and acid/base status in the emergency department. Normally reactive pupils in the emergency department. Purposeful response at 12 hours. Young age.
4. A 6-year-old girl is admitted to the intensive care unit after being rescued from a drowning accident in a lake. During the rst hour of admission, she receives 60 mL/kg of 0.9% saline for poor perfusion and hypotension. She responds to verbal communication. Over the next 8 hours, she develops a progressive increase in alveolar arterial oxygen gradient. Her arterial PO2 is 88 torr while breathing 60% oxygen on mechanical ventilation. Chest radiography shows marked worsening of lung inltrates bilaterally. Her rectal temperature is 100.0F (37.8C). Her central venous pressure is 5 mm Hg. Of the following, the most likely underlying mechanism for her deteriorating respiratory status is: A. B. C. D. E. Fluid overload. Increased pulmonary capillary permeability. Left ventricular failure. Progressive viral pneumonitis. Secondary bacterial infection.
Pediatrics in Review Vol.27 No.5 May 2006 169
You might also like
- Essay On Drowning CasesDocument2 pagesEssay On Drowning CasesReyansh AyaanshNo ratings yet
- Solving the Stray Dogs ProblemDocument3 pagesSolving the Stray Dogs ProblemMicaela Andrea CieloNo ratings yet
- Drowning: David Slocum MD Albany Medical CenterDocument39 pagesDrowning: David Slocum MD Albany Medical CenterPawan SujaneNo ratings yet
- Near DrowningDocument53 pagesNear DrowningDr. Anish GolchhaNo ratings yet
- Multiple Physical Injuries Secondary To Vehicular AccidentDocument31 pagesMultiple Physical Injuries Secondary To Vehicular AccidentJane Arian BerzabalNo ratings yet
- Case Study PNEUMONIADocument40 pagesCase Study PNEUMONIAHomework PingNo ratings yet
- Management of Acute Gastroenteritis in ChildrenDocument14 pagesManagement of Acute Gastroenteritis in ChildrenYayaNo ratings yet
- Pulmonary Contusion - WikipediaDocument15 pagesPulmonary Contusion - WikipediaRony OktarizalNo ratings yet
- SaraDocument1 pageSaraapi-649513506100% (1)
- Pathophysiology of Shock Sepsis and Organ Failure PDFDocument1,179 pagesPathophysiology of Shock Sepsis and Organ Failure PDFNotInterested100% (1)
- Legal Aspects of Nursing - An Important Necessity for NursesDocument4 pagesLegal Aspects of Nursing - An Important Necessity for Nursesgladz25No ratings yet
- EpiglDocument2 pagesEpiglfifiNo ratings yet
- Oral CareDocument3 pagesOral CareLucy CenizaNo ratings yet
- Increase Vaccination Rates Using PICO FrameworkDocument1 pageIncrease Vaccination Rates Using PICO FrameworkArga ScorpianusNo ratings yet
- Malnutrition in Stroke PatientDocument8 pagesMalnutrition in Stroke PatientFetria MelaniNo ratings yet
- A Correlational Study On The Relationship Between Research Anxiety and Self-Efficacy For Ethics Review Committee - FinalDocument42 pagesA Correlational Study On The Relationship Between Research Anxiety and Self-Efficacy For Ethics Review Committee - FinalClarissa Victoria Lumain100% (1)
- COPD Case Study: 52-Year-Old Woman with Recurring BronchitisDocument4 pagesCOPD Case Study: 52-Year-Old Woman with Recurring BronchitisMary Mae Bercacio BuellaNo ratings yet
- Suctioning The Nasopharygeal and Oropharyngeal AirwaysDocument8 pagesSuctioning The Nasopharygeal and Oropharyngeal AirwaysChamelli RobinNo ratings yet
- 151nursingdocumentation PDFDocument24 pages151nursingdocumentation PDFpademenNo ratings yet
- Health History and Interview GuidelinesDocument2 pagesHealth History and Interview GuidelinesGeraldine GonzalesNo ratings yet
- Newest Research Paper The Challenges of Student Nurses in Their Clinical Skills Development Using Digital Technology. UwuDocument50 pagesNewest Research Paper The Challenges of Student Nurses in Their Clinical Skills Development Using Digital Technology. UwuMaryan SubaldoNo ratings yet
- Chapter 007Document34 pagesChapter 007calfornianursingacadNo ratings yet
- Pain AssessmentDocument15 pagesPain AssessmentAvash ZhaNo ratings yet
- BFCDocument8 pagesBFCIrene GunongNo ratings yet
- Nurse's Safety Attitudes As Perceived by Geriatric Patients in Homecare InstitutionsDocument16 pagesNurse's Safety Attitudes As Perceived by Geriatric Patients in Homecare InstitutionsGlobal Research and Development ServicesNo ratings yet
- Nasal PolypsDocument4 pagesNasal PolypsGaby Fitria BahriNo ratings yet
- Case Analysis On Geriatrics FinalDocument30 pagesCase Analysis On Geriatrics Final3D - AURELIO, Lyca Mae M.No ratings yet
- 8 Steps Stroke Care Chain SurvivalDocument3 pages8 Steps Stroke Care Chain Survivalmuhammad fahrizaNo ratings yet
- Nurse's Role in Multidisciplinary Stroke CareDocument12 pagesNurse's Role in Multidisciplinary Stroke CareLauren GatesNo ratings yet
- Stroke GuidelinesDocument60 pagesStroke GuidelinesMuhammad Agus NashirNo ratings yet
- Acute Poisoning in Adults: Dr. S.P. Hewawasam MBBS, MDDocument76 pagesAcute Poisoning in Adults: Dr. S.P. Hewawasam MBBS, MDSamapriya Pasan Hewawasam100% (1)
- CPR Checklist PDFDocument2 pagesCPR Checklist PDFSakura SaitoNo ratings yet
- Wound CareDocument4 pagesWound CareChrisTine M. MoralesNo ratings yet
- Chronic Osteomyelitis: Dr. F. Abdul Khader Professor & HOD Department of Orthopaedics SSSMC & RiDocument31 pagesChronic Osteomyelitis: Dr. F. Abdul Khader Professor & HOD Department of Orthopaedics SSSMC & RiDr. F. Abdul KhaderNo ratings yet
- Postoperative PhaseDocument8 pagesPostoperative PhasereymarhayNo ratings yet
- 2020 CPG For Sepsis in Adults Full ManuscriptDocument162 pages2020 CPG For Sepsis in Adults Full ManuscriptWila GatchalianNo ratings yet
- Acute Respiratory Distress SyndromeDocument16 pagesAcute Respiratory Distress SyndromePawan BatthNo ratings yet
- Chapter 1-3Document27 pagesChapter 1-3JellyAnnGomezNo ratings yet
- Diagnosis and Management of Dehydration in ChildrenDocument5 pagesDiagnosis and Management of Dehydration in ChildrenCitlalli MorenoNo ratings yet
- Corona Virus InfographicDocument1 pageCorona Virus Infographicapi-510312435No ratings yet
- HemodialysisDocument11 pagesHemodialysisjuan_sioNo ratings yet
- SeizuresDocument2 pagesSeizureskaythe08No ratings yet
- Learning Module in NCM 114Document28 pagesLearning Module in NCM 114JIMENEZ, TRISHA MARIE D.No ratings yet
- Nephritis Case StudyDocument20 pagesNephritis Case StudyJosh AquinoNo ratings yet
- Nursing Physical AssessmentDocument5 pagesNursing Physical AssessmentApril Louise PaluganNo ratings yet
- Applying a Tourniquet for Bleeding EmergenciesDocument3 pagesApplying a Tourniquet for Bleeding EmergenciesTom-tom LunaNo ratings yet
- DrowningDocument7 pagesDrowningmedhatsabriNo ratings yet
- Assignment 2 EvidenceDocument18 pagesAssignment 2 EvidenceDhiren RabadiaNo ratings yet
- Midterms - Geria LecDocument5 pagesMidterms - Geria LecGiel Margareth LindoNo ratings yet
- Bachelor of Science in Nursing: Intensive Nursing Practicum: Rle LCP Module Rle LCP Unit WeekDocument8 pagesBachelor of Science in Nursing: Intensive Nursing Practicum: Rle LCP Module Rle LCP Unit WeekMichelle Gliselle Guinto MallareNo ratings yet
- Nursing Care Plan: Priority #1 Decreased Cardiac OutputDocument2 pagesNursing Care Plan: Priority #1 Decreased Cardiac Output1S - LASTIMOSA ATHENA IRISH D.No ratings yet
- EpistaxisDocument9 pagesEpistaxisapi-285171922No ratings yet
- HSNS264 A1 COPDDocument2 pagesHSNS264 A1 COPDKC Nilam100% (1)
- Geriatric Assessment FormDocument3 pagesGeriatric Assessment FormEsmeralda Barnaha100% (1)
- Research - Group4 - BSN3 1 1 1Document119 pagesResearch - Group4 - BSN3 1 1 1ruth samuel0% (1)
- Case Study Near DrowningDocument6 pagesCase Study Near DrowningNashwa Fathira0% (1)
- Coughs and Colds Nurse Management of Upper Respiratory Tract InfectionDocument3 pagesCoughs and Colds Nurse Management of Upper Respiratory Tract InfectionMichael Anthony ErmitaNo ratings yet
- Pediatric Community Acquired Pneumonia - Moderate Risk: University of The Cordilleras College of NursingDocument22 pagesPediatric Community Acquired Pneumonia - Moderate Risk: University of The Cordilleras College of NursingJemimah AdaclogNo ratings yet
- Drowning: David Szpilman, James P. Orlowski, and Joost BierensDocument8 pagesDrowning: David Szpilman, James P. Orlowski, and Joost BierensIhsan M NauvalNo ratings yet
- Management For The Drowning PatientDocument27 pagesManagement For The Drowning PatientDanieli Bello Chimer da SilvaNo ratings yet
- 0102 LayDocument1 page0102 LayAidaDenisse Negrete DurazoNo ratings yet
- 0101 Lay YoumanDocument1 page0101 Lay YoumanAidaDenisse Negrete DurazoNo ratings yet
- Motor Exam GuideDocument16 pagesMotor Exam GuideNohemí Gómez ANo ratings yet
- Cholesterol Up DateDocument10 pagesCholesterol Up DateAidaDenisse Negrete DurazoNo ratings yet
- Review On Smart Sanitizing Robot With Medicine Transport System For Covid-19Document6 pagesReview On Smart Sanitizing Robot With Medicine Transport System For Covid-19IJRASETPublicationsNo ratings yet
- CV Widasari Sri Gitarja 2016 Update-2Document3 pagesCV Widasari Sri Gitarja 2016 Update-2Radya GinandaNo ratings yet
- Module 1-Week 1-4 - Diet and HealthDocument31 pagesModule 1-Week 1-4 - Diet and HealthAsteria RafalloNo ratings yet
- Invent A RioDocument56 pagesInvent A RioJhoel Eusebio Parraga IsidroNo ratings yet
- EPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREDocument6 pagesEPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREArjun CVNo ratings yet
- The - Erlangen - Test - of - Activities - of - Daily - Living - in ADocument3 pagesThe - Erlangen - Test - of - Activities - of - Daily - Living - in Akwstas79No ratings yet
- Reminder Dengan Short Message Service (SMS) Untuk Meningkatkan KepatuhanDocument10 pagesReminder Dengan Short Message Service (SMS) Untuk Meningkatkan KepatuhanTaniaNo ratings yet
- Update On Prenatal Diagnosis and Fetal Surgery ForDocument15 pagesUpdate On Prenatal Diagnosis and Fetal Surgery ForJULIETH ANDREA RUIZ PRIETONo ratings yet
- 3 Most Common Biochemical ImbalancesDocument4 pages3 Most Common Biochemical Imbalancescarlos100% (1)
- Unit 2Document2 pagesUnit 2asolaNo ratings yet
- Adolescent Health and Youth ProgramDocument77 pagesAdolescent Health and Youth ProgramRijane Tabonoc OmlangNo ratings yet
- Helicopter interventions for polytraumatized patients in North-East RomaniaDocument2 pagesHelicopter interventions for polytraumatized patients in North-East RomaniaN.DanielaNo ratings yet
- Why Bladder Training Prior To Foley Catheter Removal Is Not BestDocument10 pagesWhy Bladder Training Prior To Foley Catheter Removal Is Not BestManoj KumarNo ratings yet
- Study On Empowering Youth and Adults To Overcome Mental Health Hardships Using A Web ApplicationDocument6 pagesStudy On Empowering Youth and Adults To Overcome Mental Health Hardships Using A Web ApplicationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Pulsed Dye Laser Therapy For Cutaneous Vascular LesionsDocument3 pagesPulsed Dye Laser Therapy For Cutaneous Vascular LesionsOogway MasterNo ratings yet
- EBPM Dalam Audit Operasional BPJS KesehatanDocument8 pagesEBPM Dalam Audit Operasional BPJS KesehatanluciaNo ratings yet
- Epidemiology & Health Information: NU1103 Tara Brookes @tarapb8Document40 pagesEpidemiology & Health Information: NU1103 Tara Brookes @tarapb8smartisaacNo ratings yet
- Nursing Concept Map TemplateDocument4 pagesNursing Concept Map TemplateAris Kendell BungabongNo ratings yet
- Edition: You Are Logged-InDocument142 pagesEdition: You Are Logged-InJoenabie Andoy Encanto0% (1)
- (L-7) - Human Health and Disease - Dec 6, 2019Document68 pages(L-7) - Human Health and Disease - Dec 6, 2019Omar GillNo ratings yet
- What Is Autism?: Characteristics of Children With AutismDocument7 pagesWhat Is Autism?: Characteristics of Children With AutismAnandNarayananNo ratings yet
- Hypertension Related To Faulty Eating Habits As Evidence My Blood Pressure of 13080.Document2 pagesHypertension Related To Faulty Eating Habits As Evidence My Blood Pressure of 13080.Senyorita KHayeNo ratings yet
- Adverse Effect of Malnutrition On EnvironmentDocument18 pagesAdverse Effect of Malnutrition On Environmentankit palNo ratings yet
- Administration of Medication in SchoolsDocument8 pagesAdministration of Medication in SchoolsDavid KefferNo ratings yet
- Healthcare Stats - Assignment #2Document6 pagesHealthcare Stats - Assignment #2erickgregs0% (1)
- Ca BookDocument80 pagesCa BookSteivy Umaming TiwakenNo ratings yet
- Helping Babies Breathe™ 06.27.2014Document18 pagesHelping Babies Breathe™ 06.27.2014Emily EresumaNo ratings yet
- MUHAMMAD NAJEEB KALLIDUKKIL LECTURER CVDocument4 pagesMUHAMMAD NAJEEB KALLIDUKKIL LECTURER CVnajeeb500No ratings yet
- Nciph ERIC16Document4 pagesNciph ERIC16AMELIA CAROLINA HERRERA BRICEÑONo ratings yet
- IM HandbookaDocument378 pagesIM HandbookakkNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)