Professional Documents
Culture Documents
M 35, Left Upper Eyelid Nodule: Deba P Sarma, MD Omaha
Uploaded by
Deba P SarmaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
M 35, Left Upper Eyelid Nodule: Deba P Sarma, MD Omaha
Uploaded by
Deba P SarmaCopyright:
Available Formats
M 35, left upper eyelid nodule
Deba P Sarma, MD Omaha
M 35, left upper eyelid nodule
Diagnosis: Cutaneous mixed tumor Comment: Clinical: Solitary, circumscribed dermal or subcutaneous nodule. Mostly in head and neck of middle-aged man. Pathology: Epithelial cords with focal ductal lumen and cystic change within a myxoid, mesenchyma, myoepitheliod or chondroid stroma. Cytology is bland. Tumor is eccrine or apocrine in origin.
Ref: Sarma DP, Repertinger S. (2009). Cutaneous mixed tumor. The Internet J Dermatol 7(1). Indexed by Google Scholar.
Cutaneous Mixed Tumor Deba P. Sarma M.D. Department of Pathology Creighton University Medical Center Omaha Nebraska USA Susan Repertinger MD Department of Pathology Creighton University Medical Center Omaha Nebraska USA Citation: D. P. Sarma & S. Repertinger : Cutaneous Mixed Tumor . The Internet Journal of Dermatology. 2009 Volume 7 Number 1 Keywords: Mixed tumor | benign adnexal tumor | chondroid syringoma Abstract A case of cutaneous mixed tumor occurring in the cheek of a 45-year-old man is presented. Case Report An excisional biopsy of a skin papule was taken of the left cheek from a 45-year-old man. The asymptomatic lesion has been present for an unknown period of time.
Figure 1: Low power photomicrograph shows a well-circumscribed dermal nodule composed of epithelial components within a fibromyxoid stroma.
Figure 2: Higher power photomicrograph shows the epithelial component forming branching tubules, ducts and dilated cystic spaces containing eosinophilic acellular material. The stroma in between the epithelial elements is fibrotic, loose, and focally myxoid. Diagnosis: Cutaneous mixed tumor Comment Cutaneous mixed tumor is an uncommon, benign adnexal neoplasm arising from apocrine or eccrine glands of the dermis. The tumor predominantly affects middle-aged women and presents as a slowly growing, painless, firm papule or nodule, most often involving the head and neck1. Histologically, the tumor is well-circumscribed and shows a biphasic growth pattern: an epithelial component and a stromal component having myxoid, fibrous, or chondroid differentiation. The epithelial component is composed of trabeculae, tubules, or ducts. Classification into eccrine or apocrine type is based on the epithelial lining cells of the sweat duct lumina. Immunohistochemical analysis of apocrine mixed tumors shows various staining patterns similar to the those of hair follicles, sebaceous glands, and all components of apocrine glands (folliculosebaceous-apocrine unit)2. While mixed tumor of the skin is almost invariably benign, cases with cytologic atypia or malignancy are reported in the literature 3, 4. Kazakov et al. reported a series of 18 apocrine mixed tumors of the skin with architectural or cytologic atypia. The tumors ranged in size from 4 mm to 12 cm. The lesions showed good circumscription and lack of capsular breach or hypercellularity. However, some asymmetry and infiltrative and pushing borders were seen. The tumors were all excised. At a mean follow-up of 5 years, no recurrences or metastases were found. Complete excision is the treatment of choice. Tumors with infiltrative borders can recur following excision, however. Corresponding author Susan Repertinger, M.D. Department of Pathology Creighton University Medical Center Omaha Nebraska USA [srepertinger@creighton.edu]
References 1. Obaidat, N.A., K.O. Alsaad, and D. Ghazarian, Skin adnexal neoplasms--part 2: an approach to tumours of cutaneous sweat glands. J Clin Pathol, 2007. 60(2): p. 145-59. (s) 2. Yamamoto, O. and H. Yasuda, An immunohistochemical study of the apocrine type of cutaneous mixed tumors with special reference to their follicular and sebaceous differentiation. J Cutan Pathol, 1999. 26(5): p. 232-41. (s) 3. Kazakov, D.V., et al., Apocrine mixed tumors of the skin with architectural and/or cytologic atypia: a retrospective clinicopathologic study of 18 cases. Am J Surg Pathol, 2007. 31(7): p. 1094-102. (s) 4. Nather, A. and I.H. Sutherland, Malignant transformation of a benign cutaneous mixed tumour. J Hand Surg [Br], 1986. 11(1): p. 139-43. (s)
You might also like
- Medical Terminology AssignmentDocument4 pagesMedical Terminology AssignmentBeverly GraciousNo ratings yet
- (Comprehensive Gynecology and Obstetrics) Mikio Mikami - Surgery For Gynecologic Cancer-Springer Singapore (2019)Document428 pages(Comprehensive Gynecology and Obstetrics) Mikio Mikami - Surgery For Gynecologic Cancer-Springer Singapore (2019)Bakar Benk100% (2)
- Health Unit Plan Disease UnitDocument68 pagesHealth Unit Plan Disease UnitKelly0% (1)
- Emanuel Revici Part 11Document25 pagesEmanuel Revici Part 11db1970No ratings yet
- DR SARMA'S DERMPATH: Chondroma Cutis, The Internet Journal of Dermatology 2007: Volume 6 NumberDocument3 pagesDR SARMA'S DERMPATH: Chondroma Cutis, The Internet Journal of Dermatology 2007: Volume 6 NumberDeba P SarmaNo ratings yet
- M 45, Neck, Asymptomatic Dermal Nodule: Deba P Sarma, MD OmahaDocument4 pagesM 45, Neck, Asymptomatic Dermal Nodule: Deba P Sarma, MD OmahaDeba P SarmaNo ratings yet
- 49 Hemalatha EtalDocument3 pages49 Hemalatha EtaleditorijmrhsNo ratings yet
- Publications 011Document4 pagesPublications 011utamiNo ratings yet
- Solid - Cystic Hidradenoma: A Case ReportDocument5 pagesSolid - Cystic Hidradenoma: A Case ReportIOSRjournalNo ratings yet
- Malignant Myopericytoma: Report of A New Case and Review of The LiteratureDocument6 pagesMalignant Myopericytoma: Report of A New Case and Review of The LiteratureRachel AutranNo ratings yet
- Cerebellopontine Angle Epidermoid CYST: Case ReportDocument3 pagesCerebellopontine Angle Epidermoid CYST: Case ReportTamajyoti GhoshNo ratings yet
- Desdierencia Entre TFS y Glandula ParotidaDocument7 pagesDesdierencia Entre TFS y Glandula ParotidaReyes Ivan García CuevasNo ratings yet
- Rabdomyosarcoma Case ReportDocument7 pagesRabdomyosarcoma Case ReportAaslesha Jakkampudi100% (1)
- Apocrine Mixed TumorDocument5 pagesApocrine Mixed TumorFaduahSalazarNo ratings yet
- Dermatomyofibroma: A Case Report and Review of The LiteratureDocument4 pagesDermatomyofibroma: A Case Report and Review of The LiteratureDeba P SarmaNo ratings yet
- Epidemiological Trends in Malignant Lacrimal Gland TumorsDocument5 pagesEpidemiological Trends in Malignant Lacrimal Gland TumorsRochnald PigaiNo ratings yet
- Benign Extrapleural Solitary Fibrous Tumorofthe Headand NeckDocument7 pagesBenign Extrapleural Solitary Fibrous Tumorofthe Headand NeckCara Danielle PabellanoNo ratings yet
- Articulo de Serie de CasoDocument8 pagesArticulo de Serie de CasoJairo Lino BNo ratings yet
- (12204749 - Romanian Journal of Internal Medicine) Multiple Histological Subtypes of Dermatofibrosarcoma Protuberans Occurring in The Same TumorDocument10 pages(12204749 - Romanian Journal of Internal Medicine) Multiple Histological Subtypes of Dermatofibrosarcoma Protuberans Occurring in The Same TumordrelvNo ratings yet
- Small Round Cells of Head and NeckDocument10 pagesSmall Round Cells of Head and NeckBlazxy EyreNo ratings yet
- Posterior Auricular Mass: Interesting Case SeriesDocument5 pagesPosterior Auricular Mass: Interesting Case SeriesMaria EsterNo ratings yet
- Pilo Matri Coma PosterDocument1 pagePilo Matri Coma Posterkjv5gxdw4fNo ratings yet
- E - Uniform Round Tumour Cells With Small Nucleus and Clear Vacuolated CytoplasmDocument16 pagesE - Uniform Round Tumour Cells With Small Nucleus and Clear Vacuolated CytoplasmAien LeeNo ratings yet
- UC Davis: Dermatology Online JournalDocument4 pagesUC Davis: Dermatology Online Journalma hNo ratings yet
- MTT LabialDocument3 pagesMTT LabialRobertoNo ratings yet
- Adenomyoepithelioma of The Breast: A Brief Diagnostic ReviewDocument5 pagesAdenomyoepithelioma of The Breast: A Brief Diagnostic ReviewSFCHIKINo ratings yet
- Desmoplastic MelanomaDocument3 pagesDesmoplastic MelanomamakhanmdNo ratings yet
- Syringoma 3Document2 pagesSyringoma 3Anita PermatasariNo ratings yet
- Pediatric Desmoid Fibromatosis of TheDocument4 pagesPediatric Desmoid Fibromatosis of ThevatankhahpooyaNo ratings yet
- Pleomorphic Sarcoma in Paratesticular Region: Case Report Open AccessDocument5 pagesPleomorphic Sarcoma in Paratesticular Region: Case Report Open AccessNurulDiniaPutriNo ratings yet
- 1 Ijdrdjun20191Document4 pages1 Ijdrdjun20191TJPRC PublicationsNo ratings yet
- ENGLISH REFARAT 3.2 - Sem 5 - Septina - Malignant Tumours With Follicular DifferentiationDocument28 pagesENGLISH REFARAT 3.2 - Sem 5 - Septina - Malignant Tumours With Follicular DifferentiationAffan Akbar TalamiNo ratings yet
- Keywords: Pilomatrixoma, Skin Nodule, Fine Needle Aspiration CytologyDocument4 pagesKeywords: Pilomatrixoma, Skin Nodule, Fine Needle Aspiration CytologyachmadaNo ratings yet
- Basal Cell AdenomawDocument3 pagesBasal Cell AdenomawDrRobin SabharwalNo ratings yet
- Ameloblastoma: Notorious Tumor of The Jaw - Report of A CaseDocument3 pagesAmeloblastoma: Notorious Tumor of The Jaw - Report of A CaseUwie MoumootNo ratings yet
- Dermatology Research and Therapy: Nodular Hidradenoma: A Forgotten Tumor of The ScalpDocument3 pagesDermatology Research and Therapy: Nodular Hidradenoma: A Forgotten Tumor of The ScalpannibaNo ratings yet
- Ijohns 2015083115062935 PDFDocument6 pagesIjohns 2015083115062935 PDFradifNo ratings yet
- Chondrosarcoma of Breast - A Case ReportDocument2 pagesChondrosarcoma of Breast - A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- RPB14150079015Document5 pagesRPB14150079015Ijupbs IjupbsNo ratings yet
- 1868-Article Text-6804-1-10-20180620Document3 pages1868-Article Text-6804-1-10-20180620Wina ViqaNo ratings yet
- Oligodendroglioma in The Cervical Spinal Cord of A Dog: T. M, A. M - L, M. H - T, W. BDocument3 pagesOligodendroglioma in The Cervical Spinal Cord of A Dog: T. M, A. M - L, M. H - T, W. BSamir BazanNo ratings yet
- Plastic Surgery & Advanced Scalp Tumors: Epidemiological Profile and Surgical Management About 65 CasesDocument7 pagesPlastic Surgery & Advanced Scalp Tumors: Epidemiological Profile and Surgical Management About 65 CasesIJAR JOURNALNo ratings yet
- Additional Article Information: Keywords: Adenoid Cystic Carcinoma, Cribriform Pattern, Parotid GlandDocument7 pagesAdditional Article Information: Keywords: Adenoid Cystic Carcinoma, Cribriform Pattern, Parotid GlandRizal TabootiNo ratings yet
- Laryngeal Plasmacytoma in Kahlers Disease: A Case ReportDocument6 pagesLaryngeal Plasmacytoma in Kahlers Disease: A Case ReportIJAR JOURNALNo ratings yet
- Adenoid Cystic Carcinoma of Hard Palate: A Case ReportDocument5 pagesAdenoid Cystic Carcinoma of Hard Palate: A Case ReportHemant GuptaNo ratings yet
- Case Report Reference Article (Published)Document3 pagesCase Report Reference Article (Published)manojananthappanNo ratings yet
- Metaplastic Carcinoma Breast: A Case SeriesDocument4 pagesMetaplastic Carcinoma Breast: A Case SeriesIJAR JOURNALNo ratings yet
- Adult LymphangiomaDocument3 pagesAdult LymphangiomaRini RahmawulandariNo ratings yet
- A Rare Case of Zosteriform Cutaneous Metastasesfrom Squamous Cell Carcinoma of Hard PalateDocument4 pagesA Rare Case of Zosteriform Cutaneous Metastasesfrom Squamous Cell Carcinoma of Hard PalateShiva PNo ratings yet
- 45syam EtalDocument3 pages45syam EtaleditorijmrhsNo ratings yet
- Article - Cytological Features of The Warthin-Like Variant of Salivary Mucoepidermoid CarcinomaDocument5 pagesArticle - Cytological Features of The Warthin-Like Variant of Salivary Mucoepidermoid CarcinomaCandeNo ratings yet
- Hasil Penelitian KSSDocument3 pagesHasil Penelitian KSSMarlboro LightsNo ratings yet
- Abstract: Kimura Disease Is A Rare Form of Chronic Inflammatory Disorder InvolvingDocument4 pagesAbstract: Kimura Disease Is A Rare Form of Chronic Inflammatory Disorder InvolvingpriyokNo ratings yet
- CH15 Patho D&R AgamDocument11 pagesCH15 Patho D&R AgamBio CheNo ratings yet
- 8veda EtalDocument7 pages8veda EtaleditorijmrhsNo ratings yet
- Case Report Epithelial-Myoepithelial Carcinoma of The Breast With Rhabdoid FeaturesDocument4 pagesCase Report Epithelial-Myoepithelial Carcinoma of The Breast With Rhabdoid FeaturesGabriela Izabela BaltatescuNo ratings yet
- Melanome Acral: Du Diagnostic Au TraitementDocument8 pagesMelanome Acral: Du Diagnostic Au TraitementIJAR JOURNALNo ratings yet
- A Case Report of Eruptive Syringoma: Clinical, Dermoscopic and Histological FeaturesDocument5 pagesA Case Report of Eruptive Syringoma: Clinical, Dermoscopic and Histological FeaturesIJAR JOURNALNo ratings yet
- ContentsDocument3 pagesContentsNaim CalilNo ratings yet
- 18 Extra-GuptaNDocument3 pages18 Extra-GuptaNGalih rarang gatiNo ratings yet
- Current Controversies in The Management of Malignant Parotid TumorsDocument8 pagesCurrent Controversies in The Management of Malignant Parotid TumorsDirga Rasyidin LNo ratings yet
- Low Grade Endometrial Stromal Sarcoma: A Case ReportDocument3 pagesLow Grade Endometrial Stromal Sarcoma: A Case ReportNazia BhatNo ratings yet
- 03.04 - Intraventricular TumoursDocument185 pages03.04 - Intraventricular TumoursBivolaru AlinNo ratings yet
- Basal Cell Carcinoma: Advances in Treatment and ResearchFrom EverandBasal Cell Carcinoma: Advances in Treatment and ResearchMichael R. MigdenNo ratings yet
- Accessory TragusDocument3 pagesAccessory TragusDeba P SarmaNo ratings yet
- Acantholytic Dermatosis With DyskeratosisDocument11 pagesAcantholytic Dermatosis With DyskeratosisDeba P SarmaNo ratings yet
- Pilar Cyst With CrystalsDocument2 pagesPilar Cyst With CrystalsDeba P SarmaNo ratings yet
- Acantholytic Solar Keratosis, M 67, Forehead PDFDocument6 pagesAcantholytic Solar Keratosis, M 67, Forehead PDFDeba P SarmaNo ratings yet
- Acantholytic Bullous DiseaseDocument4 pagesAcantholytic Bullous DiseaseDeba P SarmaNo ratings yet
- Acantholytic Actinic KeratosisDocument4 pagesAcantholytic Actinic KeratosisDeba P SarmaNo ratings yet
- Acantholytic Bullous Disease (Darier's Disease, Keratosis Follicularis)Document3 pagesAcantholytic Bullous Disease (Darier's Disease, Keratosis Follicularis)Deba P SarmaNo ratings yet
- Xanthogranuloma PPT DSDocument9 pagesXanthogranuloma PPT DSDeba P SarmaNo ratings yet
- Acantholytic Acanthoma. M 60, ScrotumDocument8 pagesAcantholytic Acanthoma. M 60, ScrotumDeba P SarmaNo ratings yet
- Results of Search in Google Scholar On 'Deba P Sarma'Document28 pagesResults of Search in Google Scholar On 'Deba P Sarma'Deba P SarmaNo ratings yet
- Balanitis Circumscripta Plasmacellularis (Zoon's Balanitis, Plasma Cell Balanitis)Document6 pagesBalanitis Circumscripta Plasmacellularis (Zoon's Balanitis, Plasma Cell Balanitis)Deba P SarmaNo ratings yet
- Xanthomatous Synovial Cyst (Xanthomatous Ganglion Cyst), M 74, Left PalmDocument7 pagesXanthomatous Synovial Cyst (Xanthomatous Ganglion Cyst), M 74, Left PalmDeba P SarmaNo ratings yet
- Xanthogranuloma, M 30, Right ElbowDocument4 pagesXanthogranuloma, M 30, Right ElbowDeba P SarmaNo ratings yet
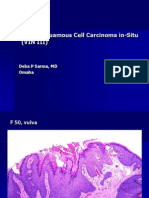
- Vulvar Squamous Cell Carcinoma In-Situ (VIN III), F 50, VulvaDocument6 pagesVulvar Squamous Cell Carcinoma In-Situ (VIN III), F 50, VulvaDeba P SarmaNo ratings yet
- Verrucous Epidermal Nevus. F 43, ScalpDocument4 pagesVerrucous Epidermal Nevus. F 43, ScalpDeba P SarmaNo ratings yet
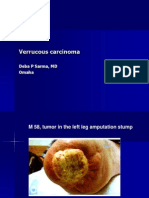
- Verrucous Carcinoma., M 58, Left Leg Amputation StumpDocument7 pagesVerrucous Carcinoma., M 58, Left Leg Amputation StumpDeba P SarmaNo ratings yet
- Verrucous Carcinoma of The Foot, M 63, Left FootDocument8 pagesVerrucous Carcinoma of The Foot, M 63, Left FootDeba P Sarma100% (1)
- Verruca Vulgaris., M 22.,PPTDocument2 pagesVerruca Vulgaris., M 22.,PPTDeba P SarmaNo ratings yet
- Jurnal Autoimun PDFDocument7 pagesJurnal Autoimun PDFRara Anglis AninditaNo ratings yet
- Agenda - Biblioteka de Biomarkeri - FINALDocument1 pageAgenda - Biblioteka de Biomarkeri - FINALOlteanu Gheorghe-EmilianNo ratings yet
- Combating Lifestyle Diseases in Kerala With Ayurvedic RegimenDocument6 pagesCombating Lifestyle Diseases in Kerala With Ayurvedic RegimenarcherselevatorsNo ratings yet
- Cap. 1 PDFDocument44 pagesCap. 1 PDFOscarNo ratings yet
- Tumori Fibrohistiocitare IntermediareDocument39 pagesTumori Fibrohistiocitare IntermediareOana BarbuNo ratings yet
- Survivor Stories: Living With, Through & Beyond CancerDocument24 pagesSurvivor Stories: Living With, Through & Beyond CancerTedEscobedoNo ratings yet
- USPSTF Screening Recommendations (Across The Ages)Document8 pagesUSPSTF Screening Recommendations (Across The Ages)Jessica MooreNo ratings yet
- Cell Division - Mitosis and The Cell CycleDocument43 pagesCell Division - Mitosis and The Cell CycleJomar CarabotNo ratings yet
- Cordyceps Militaris CapsuleDocument32 pagesCordyceps Militaris CapsuleDeborah o100% (1)
- Nejmoa1113162 AppendixDocument35 pagesNejmoa1113162 AppendixayuannisahusnaNo ratings yet
- Chapter 5 - Autosuggestion - Think and Grow Rich - The 21st-Century Edition (Workbook)Document33 pagesChapter 5 - Autosuggestion - Think and Grow Rich - The 21st-Century Edition (Workbook)Naveed AhmedNo ratings yet
- Kep KritisDocument193 pagesKep Kritisari cahyaNo ratings yet
- Optic Nerve Tumours: Presenter-Dr Adheela Abdulla Moderator - DR Shikha BassiDocument54 pagesOptic Nerve Tumours: Presenter-Dr Adheela Abdulla Moderator - DR Shikha BassiMohammed Jazeel 2549No ratings yet
- Pharmaceutical Probability of SuccessDocument42 pagesPharmaceutical Probability of SuccesskennyNo ratings yet
- Elective Clinical Target Volumes For Conformal Therapy in Anorectal Cancer - An Radiation Therapy Oncology Group Consensus Panel Contouring AtlasDocument7 pagesElective Clinical Target Volumes For Conformal Therapy in Anorectal Cancer - An Radiation Therapy Oncology Group Consensus Panel Contouring AtlasAnonymous 8KN8IR1GTWNo ratings yet
- Nutrition Assessment 1Document22 pagesNutrition Assessment 1KHALEEL SALEHNo ratings yet
- 10 1 Paraneoplastic SyndromesDocument31 pages10 1 Paraneoplastic SyndromesTeky WidyariniNo ratings yet
- Care of Clients With Problems in Cellular Aberrations Key TermsDocument2 pagesCare of Clients With Problems in Cellular Aberrations Key Termsjoyrena ochondraNo ratings yet
- Basic Oncology RadiationDocument30 pagesBasic Oncology Radiationnugra raturandangNo ratings yet
- 28 11 2019 8th Aitong Medical Camp ReportDocument26 pages28 11 2019 8th Aitong Medical Camp ReportStacy NeetNo ratings yet
- Top 10 Healthiest FruitDocument15 pagesTop 10 Healthiest FruitFauzia IkaNo ratings yet
- Cancer - 2011 - Hajdu - A Note From History Landmarks in History of Cancer Part 2Document10 pagesCancer - 2011 - Hajdu - A Note From History Landmarks in History of Cancer Part 2Pilar AufrastoNo ratings yet
- CPH LEC (05-05) - Unit 4Document4 pagesCPH LEC (05-05) - Unit 4Ruthenie RedobleNo ratings yet
- HPV QUANT-21 - Form A6 - Specification of ProductDocument4 pagesHPV QUANT-21 - Form A6 - Specification of ProductLAB PCRNo ratings yet
- Pyrexia of Unknown OriginDocument81 pagesPyrexia of Unknown OriginJithin Bhagavati Kalam100% (1)
- End of Term 3 Musomhs Cat MCQ July 2020-1Document16 pagesEnd of Term 3 Musomhs Cat MCQ July 2020-1MustafaNo ratings yet