Professional Documents
Culture Documents
Arterial Blood Gas Analysis Learning Objectives:: Introduction/ Overview
Uploaded by
janorberteOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Arterial Blood Gas Analysis Learning Objectives:: Introduction/ Overview
Uploaded by
janorberteCopyright:
Available Formats
Arterial Blood Gas Analysis Learning Objectives:
After completing this lecture, the nurses should be able to: Identify normal arterial blood gas values and interpret the meaning of abnormal values. Compare the roles of PaO2, pH, PaCO2, and Bicarbonate in maintaining acid/base balance. Interpret the oxygenation state of a patient using the reported arterial blood gas PaO2 value.
Introduction/ Overview:
Many critical illnesses can upset a patients acid-base balance, and a disturbance in acid-base equilibrium may indicate other underlying diseases or organ damage. Accurately interpreting acid-base balance requires simultaneously measurements of arterial pH and plasma electrolytes, as well as knowledge of compensatory physiologic mechanisms. ABG analysis must be done by a written physician order. Body acids are formed as end products of cellular metabolism. Under normal physiologic conditions, a person generates 50 to 100 mEq/day of acid from metabolism of carbohydrates, proteins and fats. The body loses base in the stool. Acid production must balance the neutralization or excretion. The lungs and kidneys are the main regulators of acid-base homeostasis. The lungs release CO2, an end product of carbonic acid (H2CO3). The renal tubules, with the regulation of bicarbonate (HCO3), excrete other acids produced from the metabolism of proteins, carbohydrates and fats. Acidosis is described as a physiologic condition caused by the bodys inability to buffer excess H+ ions. Alkalosis results from deficiency in H+ ion concentration.
Definition of terms:
1. ABG- arterial blood gas- analysis evaluates gas exchange in the lungs by measuring the PaO2 and the pH of an arterial blood sample. 2. Acidosis- when pH value of body fluids is below 7.35 3. Alkalosis- when pH value of body fluids above 7.45 4. pH- normal pH values body fluids between pH 7.35- 7.45 - refers to German word Poten2(power) so pH means power of Hydrogen 5. - (Arterial tension)- symbol for partial pressure of carbon dioxide in the arterial blood . 6. PaO2- (arterial O2 tension)- symbol for partial pressure of oxygen in arterial blood. 7. HCO3- Bicarbonate- main body buffer for acid-base balance. 8. SBE- (standard base excess) (deficit) - amount of strong acid or base required to titrate 1 liter of blood back to a pH of 7.4 at temperature of 37C and PCO2 of 40mmHg. 9. B.E- another measure of the metabolic (renal) component, normal range of B.E (-2 to +2). 10. Acid- compound that forms hydrogen ions 9 (proton donor).
11. Base- compound that combines with hydrogen ions in solution. The body has three compensatory mechanisms to handle changes in serum pH: Physiologic buffer, consisting of a weak acid (which can easily be broken down) and its base salt or of a weak base and its acid salt. These buffers are the bicarbonate-carbonic acid buffering system, intracellular protein buffers, and phosphate buffers in the bone. Pulmonary compensation, in which changes in ventilation work to change the partial pressure of arterial carbon dioxide and drive the pH toward the normal range. Renal compensation, which kicks in when the other mechanism have been ineffective, generally after about 6 hours of sustained acidosis or alkalosis. Metabolism- produces acidic products that lower the pH of body fluids. Example 1. Carbon dioxide- by product of metabolism - Combines with water to form carbonic acid 2. Lactic Acid- product of an aerobic metabolism; protein metabolism produces phosphoric and sulfuric acid, lipid metabolism produces fatty acids - These acidic substances must continuously be eliminated from our body to maintain pH homeostasis. - When rapid elimination of acidic products of metabolism results in alkalosis. - Failure to eliminate acidic products of metabolism results in acidosis. Major effect of acidosis- depression of central nervous system, when pH blood falls below 7.35 malfunctions the individual becomes disoriented or possibly comatose as condition worsens. Major effects of alkalosis- hyper excitability of the nervous system. Peripheral nerves are affected first resulting in spontaneous nervous stimulation of muscles. Spasms/ tetanic contractions and possibly extreme nervousness or convulsion result. Severe alkalosis can cause death as result of tetany of the respiratory muscles. Buffers- body fluids helps resist changes in pH of body fluids. The respiratory system and kidneys regulate the ph body fluids. Malfunction of either respiratory or kidneys can result to acidosis or alkalosis.
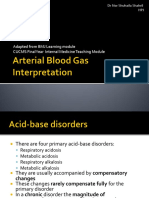
Most common acid-base derangements
1. Metabolic acidosis Increase in amount of absolute body acid either excess production of acids or excessive loss of bicarbonate, sodium and potassium. Causes include lactic acidosis, ketoacidosis, and loss of bicarbonate through severe diarrhea or bicarbonate wasting through kidneys or G.I tract. Kidneys attempts to preserved sodium by exchanging it for excreted H+ or potassium. Presence of H+ load, H+ ions move from extra cellular fluid into intracellular fluid. Potassium moves outside the cell into extracellular fluid to maintain electro neutrality. Severe acidosis, significant overall depletion of total body potassium stores can occur despite severe hyperkalemia.
2.
Treatment- Intravenous (IV) potassium given to patient with diabetic ketoacidosis, early treatment. pH is low, PaCO2 normal, HCO3 is low
Metabolic alkalosis - When HCO3 is increased, usually as result of excessive loss of metabolic acids. Causes include diuretics, secretory adenoma of colon, emesis, hyper aldosteronism, Cushing syndrome and exogenous steroids. - Some cause respond to treatment with 0.9% sodium chloride solution. Example; urine chloride concentration is less than 15mmol/L- Saline responsive. Includes G.I loss, dieresis, or renal compensation for hypercapnea. Results mineralo corticoid excess or potassium depletion. - Urine chloride concentration level above 25 mmol/L non saline responsive. - Treatment- fluid administration- foundation of treatment for saline responsive metabolic alkalosis. In case of extreme alkalosis, the patient may be given dilute hydrochloric acid. Saline-resistant alkalosis is treated by addressing the underlying etiology. - pH is high, PaCO2 normal, HCO3 is high
3. Respiratory Acidosis - Rate at which carbon dioxide is eliminated from the body fluids through the lungs falls. This increases the concentration of carbon dioxide in the body fluids. pH less than 7.35 and his PaCO2 is above 45 mmHg. - Alveolar hypoventilation is the only mechanism that causes hypercabia, PaCO2 above normal amount alveolar ventilation necessary to maintain PaCO2 varies depending upon CO2 produced. - Relationship between PaCO2 and plasma HCO3 determines arterial pH. Generally acute increases in PaCO2 are accompanied by only minimal changes in serum HCO3. However, over a period of 1 to 3 days renal conservation of HCO3 results in the increased in pH. - Chronic respiratory acidosis- occurs secondary to chronic reduction in alveolar ventilation. In chronic diseases such as chronic obstructive pulmonary disease. Acute respiratory acidosis is caused by an acute change in alveolar ventilation; respiratory depression from acute opioid ingestion is one cause. - Treatment for respiratory acidosis is largely supportive, but if opioid is ingestion is suspected, IV naloxone may be given as an antidote. - pH is low, PaCO2 high, HCO3 is normal
4. Respiratory alkalosis - Results from hyperventilation of the lungs. Increases rate at which carbon dioxide is eliminated from the body fluids and results in a decrease in the concentration of carbon dioxide in the body fluids. Occurs when PaCO2 is reduced causing an increase in pH. Common causes increase alveolar ventilation, which can happen in hyperventilation, mechanical over ventilation, hepatic disease, pregnancy, and septicemia. - Treatment- directed at discovering and correcting the underlying etiology.
Example: patient hyperventilating from anxiety have him breath into a paper bag. Mechanical ventilated patients with mechanical over ventilation reducing the minute ventilation or tidal volume will increase PaCO2 and reduce pH. Monitor closely rapid reduction of PaCO2 in a patient with chronic respiratory alkalosis may cause acute metabolic acidosis. pH is high, PaCO2 low, HCO3 is normal
Implementation Arterial 7.35- 7.36 80-100 mmHg 35-45 mmHg 22-26 mEq/L or mmol/L -2 to +2 mEq/L or mmol/L 95% - 100% Blood Gas Components pH pO2 pCO2 HCO3 Base Excess (BE) O2 Saturation Venous 7.31-7.41 35-40 mmHg 41-51 mmHg 22-26 mEq/L or mmol/L -2 to +2 mEq/L or mmol/L 68% - 77%
Steps how to determine acidosis and alkalosis
Step 1 use pH to determine acidosis or alkalosis
Acidosis
Normal or Compensated
Alkalosis
7.35 35
Tends toward alkalosis Causes high pH Neutralizes low pH
7.35-7.45 35-45
Normal or compensated
7.45 45
tends toward acidosis causes low pH neutralizes high pH
Step 2 - Use PaCO2 to determine respiratory effect
Step 3 Assume metabolic cause when respiratory is ruled out. High pH Low pH
Alkalosis High PaCO2 Metabolic Low PaCO2 Respiratory
Acidosis High PaCO2 Respiratory Low PaCO2 Metabolic
If PaCO2 is abnormal and pH is normal, it indicates compensation. pH 7.4 would be a compensated alkalosis pH < 7.4 would be a compensated acidosis.
Step 4 Use HCO3 to verify metabolic effect Normal HCO3 is 22-26
Please note:
Remember, the first three steps apply to the majority of cases, but do not take into account: the possibility of complete compensation, but those cases are usually less serious, and Instances of combined respiratory and metabolic imbalance, but those cases are pretty rare. . Combined disturbance means HCO3 alters the pH in the same direction as the PaCO2 . High PaCO2 and low HCO3 (acidosis) . Low HCO3 and high HCO3 (alkalosis)
Patient and Family Education
1. Explain the purpose and tell the watcher/ mother that the arterial blood gas analysis requires blood sample. 2. Explain who will perform the arterial puncture, when it will occur, and where the puncture will be: radial, brachial or femoral artery.
You might also like
- Arterial Blood Gas Analysis - making it easyFrom EverandArterial Blood Gas Analysis - making it easyRating: 4.5 out of 5 stars4.5/5 (4)
- Sample Questions For HAAD Prometric and DHA For Nurses PDFDocument23 pagesSample Questions For HAAD Prometric and DHA For Nurses PDFAasmeetaa Thapa100% (2)
- Acid Base Balancing ActDocument6 pagesAcid Base Balancing ActjohnkuysNo ratings yet
- Acid Base Balance and ImbalanceDocument72 pagesAcid Base Balance and ImbalanceAnusha Verghese100% (2)
- Acid Base Balance: Carol Johns, MSN, RNDocument36 pagesAcid Base Balance: Carol Johns, MSN, RNkatrinasdNo ratings yet
- Understanding Acid-Base BalanceDocument3 pagesUnderstanding Acid-Base Balanceabxaz100% (1)
- Kertas Litmus Merupakan Alat Untuk Mengukur Bahan Yang Mempunyai Asid Atau Alkaline.Document56 pagesKertas Litmus Merupakan Alat Untuk Mengukur Bahan Yang Mempunyai Asid Atau Alkaline.Rizal FarieNo ratings yet
- Clinical BiochemistryDocument11 pagesClinical BiochemistryKrushna SaiNo ratings yet
- BG For NeonatesDocument18 pagesBG For NeonatesNick AlfaroNo ratings yet
- ABG MMHG InterpretationDocument92 pagesABG MMHG InterpretationManmeet SNo ratings yet
- Arterial Blood GasDocument55 pagesArterial Blood GasLal NandaniNo ratings yet
- Acid BaseDocument6 pagesAcid BaseCarol Solanyi Gacha QuinteroNo ratings yet
- Acid-Base Balance and Anion GapDocument37 pagesAcid-Base Balance and Anion GapMsa AhhfaaNo ratings yet
- Understanding Acid Base Balance.3Document3 pagesUnderstanding Acid Base Balance.3YuniParaditaDjunaidi100% (1)
- Acid Base DisordersDocument51 pagesAcid Base Disordersmmkavitha98No ratings yet
- Audio 2021 03 29 12 31 31Document41 pagesAudio 2021 03 29 12 31 31wafaa moNo ratings yet
- Acid - Base Imbalance and Its Impact On ElectrolytesDocument40 pagesAcid - Base Imbalance and Its Impact On ElectrolytesahmadNo ratings yet
- Acid-Base Homeostasis: Dr. Abeer KhurshidDocument42 pagesAcid-Base Homeostasis: Dr. Abeer Khurshidسلة فواكة100% (2)
- How To Interpret Arterial Blood Gas ResultsDocument9 pagesHow To Interpret Arterial Blood Gas ResultsteleasadgramNo ratings yet
- AbgDocument7 pagesAbgChin ChanNo ratings yet
- Acid Base BalanceDocument43 pagesAcid Base Balanceanju KvNo ratings yet
- Acid Base BalanceDocument20 pagesAcid Base BalanceAyat AdilNo ratings yet
- ABG AnalysisDocument57 pagesABG AnalysisHardik RathodNo ratings yet
- Arterial Blood Gas AnalysisDocument6 pagesArterial Blood Gas AnalysisMaribee Tagayun EspirituNo ratings yet
- Acid Base Disorders DR Kwaifa - PPTX 1Document99 pagesAcid Base Disorders DR Kwaifa - PPTX 1DICKSONNo ratings yet
- Week 4 Buffers, Carbohydrates Metabolic PathwaysDocument16 pagesWeek 4 Buffers, Carbohydrates Metabolic PathwaysangeliaNo ratings yet
- Acid - Base Basics: Dr. Fawzeya Aboul Fetouh Prof of Anesthesia Cairo UnversityDocument54 pagesAcid - Base Basics: Dr. Fawzeya Aboul Fetouh Prof of Anesthesia Cairo UnversityPaolo Uccello100% (1)
- Acid-Base Balance Kampang: Abdul Salam M. Sofro Faculty of Medicine YARSI UniversityDocument78 pagesAcid-Base Balance Kampang: Abdul Salam M. Sofro Faculty of Medicine YARSI UniversityAndy SelvianNo ratings yet
- Electrolytes Used in Acid-Base TheraphyDocument30 pagesElectrolytes Used in Acid-Base TheraphySuresh ThanneruNo ratings yet
- Arterial Blood GasDocument55 pagesArterial Blood GasRathis Dasan100% (1)
- Acid Base TutorialDocument74 pagesAcid Base TutorialuedmarineNo ratings yet
- AbgDocument52 pagesAbgm07wwpNo ratings yet
- Arterial Blood Gases Easyas: InterpretingDocument5 pagesArterial Blood Gases Easyas: Interpretingoccam1132No ratings yet
- ABG (Arterial Blood Gas Analysis)Document30 pagesABG (Arterial Blood Gas Analysis)kalyan kumarNo ratings yet
- Understanding Acid Base Balance.3Document3 pagesUnderstanding Acid Base Balance.3Hazel Vivian Soliz AlconzNo ratings yet
- Assignment: Submitted by Ali Ahmed Roll No #12164Document12 pagesAssignment: Submitted by Ali Ahmed Roll No #12164Zafar Iqbal ManjNo ratings yet
- Jill Getchell, BS, CCP, LCP, LPNDocument115 pagesJill Getchell, BS, CCP, LCP, LPNapi-301270014No ratings yet
- Acid - Base BalanceDocument41 pagesAcid - Base BalanceEgun Nuel DNo ratings yet
- Acid Base Fall 2008Document34 pagesAcid Base Fall 2008anon-252165No ratings yet
- Abg PPT NewDocument69 pagesAbg PPT NewMalaka Atapattu100% (2)
- Acid Base BalanceDocument59 pagesAcid Base BalanceFratila IuliaNo ratings yet
- Indication For Arterial Blood Gas AnalysisDocument10 pagesIndication For Arterial Blood Gas AnalysisRohini RaiNo ratings yet
- Lecture 2 - Fluid & Electrolyre Balance 2021Document28 pagesLecture 2 - Fluid & Electrolyre Balance 2021عمار عاشورNo ratings yet
- Acid-Base Balance: Acidosis & AlkalosisDocument30 pagesAcid-Base Balance: Acidosis & AlkalosisrathanNo ratings yet
- Acid-Base BalanceDocument7 pagesAcid-Base BalanceMichelle Mae JulianaNo ratings yet
- Alkalosis 2Document15 pagesAlkalosis 2g8pn6pt8nhNo ratings yet
- Acid Base Self Study With Practice QuestionsDocument13 pagesAcid Base Self Study With Practice QuestionsfriendofnurseNo ratings yet
- Lect 04Document4 pagesLect 04الحاج كاملNo ratings yet
- NCM 3114 Acid Base Imbalance-2Document13 pagesNCM 3114 Acid Base Imbalance-2Fayeh Harah PadrillanNo ratings yet
- Basics of Acid-Base Balance: When It Comes To Acids and Bases, The Difference Between Life and Death IsDocument5 pagesBasics of Acid-Base Balance: When It Comes To Acids and Bases, The Difference Between Life and Death IsAyaz Ahmed BrohiNo ratings yet
- Arterial Blood Gas (ABG) Interpretation For Medical Students, OSCEs and MRCP - Oxford Medical EducatDocument8 pagesArterial Blood Gas (ABG) Interpretation For Medical Students, OSCEs and MRCP - Oxford Medical EducatmuhammadridhwanNo ratings yet
- Abg Analysis - 2014Document28 pagesAbg Analysis - 2014Dylan ThomasNo ratings yet
- Blood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIDocument39 pagesBlood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSISalsabila RahmaNo ratings yet
- Echilibrul Acido-Bazic: Respiratory If The Change Is Primarily Due To A Change in PcoDocument3 pagesEchilibrul Acido-Bazic: Respiratory If The Change Is Primarily Due To A Change in PcoIoana CNo ratings yet
- Arterial Blood Gas Analysis: BY-Shivam Sachan (JR Ii) Moderator - Dr. R.K YADAV (M.D)Document52 pagesArterial Blood Gas Analysis: BY-Shivam Sachan (JR Ii) Moderator - Dr. R.K YADAV (M.D)imranqazi11No ratings yet
- Ivma Ce Acid BaseDocument11 pagesIvma Ce Acid BaseGhozy IANo ratings yet
- Acid-Base BalanceDocument6 pagesAcid-Base BalanceStanley OdiraNo ratings yet
- Blood Gas AnalysisDocument39 pagesBlood Gas Analysisjtalan9No ratings yet
- The Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentDocument36 pagesThe Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentCamelia A. ParuschiNo ratings yet
- Metabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMetabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Ophthalmology - Diseases of The EyelidsDocument9 pagesOphthalmology - Diseases of The EyelidsjbtcmdtjjvNo ratings yet
- Topnotch Pathology Supplemental PICTURES Powerpoint Based On Handouts September 2019Document53 pagesTopnotch Pathology Supplemental PICTURES Powerpoint Based On Handouts September 2019croixNo ratings yet
- Paragraph DevelopmentDocument7 pagesParagraph DevelopmentJacqueline Gregorio RamosNo ratings yet
- Obat Yang Melebarkan PupilDocument4 pagesObat Yang Melebarkan PupilElyza AimanNo ratings yet
- Rutgers Public Health Course BrochureDocument2 pagesRutgers Public Health Course BrochureRutgersCPENo ratings yet
- Goddess Isis - 7D InitiationDocument6 pagesGoddess Isis - 7D InitiationEmeraldRayNo ratings yet
- Hiatal HerniaDocument6 pagesHiatal HerniaMaria Donabella OngueNo ratings yet
- Environmental Mercury and Its Toxic Effects: ReviewDocument10 pagesEnvironmental Mercury and Its Toxic Effects: ReviewZusely Garcia SanchezNo ratings yet
- Cholecystitis COURSE in The WARDDocument7 pagesCholecystitis COURSE in The WARDJisel-Apple BulanNo ratings yet
- A Vegan PowerDocument3 pagesA Vegan PowerashankarNo ratings yet
- ChleraDocument26 pagesChleraadelekeyusufNo ratings yet
- Effects of Junk Food and Beverages On AdDocument7 pagesEffects of Junk Food and Beverages On AdAnonymous OP6R1ZSNo ratings yet
- Using Paida Lajin For Urgent SymptomsDocument5 pagesUsing Paida Lajin For Urgent SymptomsSam100% (1)
- Labs and NCP #2Document3 pagesLabs and NCP #2Yen Valien CugayNo ratings yet
- Keshe - Nano and Gans Health Apps 3of4 29ppDocument29 pagesKeshe - Nano and Gans Health Apps 3of4 29ppExopolitika MagyarországNo ratings yet
- Raynaud's DiseaseDocument8 pagesRaynaud's DiseaseDana del PilarNo ratings yet
- Streptococcus Suis Meningitis, Hawaii: Berculosis May Vary in Host Range, andDocument3 pagesStreptococcus Suis Meningitis, Hawaii: Berculosis May Vary in Host Range, andIkhwanul KhairiaNo ratings yet
- Formula Tepung Okkara Dan Tepung Beras Hitam PDFDocument7 pagesFormula Tepung Okkara Dan Tepung Beras Hitam PDFSistha oklepeNo ratings yet
- PneumoniaDocument102 pagesPneumoniaJay Kumar100% (1)
- ISBDFinal Book 2012 BDocument53 pagesISBDFinal Book 2012 BvadamadaNo ratings yet
- Palliative CareDocument35 pagesPalliative CareChucky Vergara75% (4)
- Kelompok 2 H2S 97-2003 PPT ToksikDocument38 pagesKelompok 2 H2S 97-2003 PPT ToksikHerfando Maulana AlhafizhNo ratings yet
- Case Study Rle - Pedia Charity WardDocument40 pagesCase Study Rle - Pedia Charity WardKrizelle MesinaNo ratings yet
- Buildings and Structures: Padua EsteDocument2 pagesBuildings and Structures: Padua EsteKevin LavinaNo ratings yet
- Speech DelayDocument16 pagesSpeech Delayian ismail100% (1)
- 0-0013 PDFDocument24 pages0-0013 PDFisabellaprie3No ratings yet
- C1 Ob-Gyn-2020Document33 pagesC1 Ob-Gyn-2020yabsera mulatuNo ratings yet