Professional Documents
Culture Documents
RCOG Screening Guidelines
Uploaded by
Jo FishburnOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
RCOG Screening Guidelines
Uploaded by
Jo FishburnCopyright:
Available Formats
Ultrasound Screening
July 2000 Supplement to Ultrasound Screening for Fetal Abnormalities Contents
Membership of the Working Party 1. Introduction 2. The Early Pregnancy Scan 3. The "20 week" Anomaly Scan 4. Standards 4.1 Quality of information given to patients, and its explicitness 4.2 Setting and timing 4.3 Care and support for women undergoing screening 4.4 Record keeping 4.5 Computer-based records 4.6 Quality and Audit 5. Assessment of screening programmes 6. Training 7. Equipment 8. References Appendix 1 Baseline fetal anomaly scan Appendix 2 Ultrasound Screening for Aneuploidy Guidance for the professional Appendix 3 Patient information leaflet - Your ultrasound scan Appendix 4 Potential detection rates based on screening strategy Membership of the Working Party Professor M J Whittle FRCOG (Chair) Professor of Fetal Medicine, University of Birmingham Head, Academic Department of Obstetrics and Gynaecology Dr L S Chitty MRCOG Consultant in Genetics and Fetal Medicine University College Hospital, London Professor J P Neilson FRCOG Department of Obstetrics & Gynaecology University of Liverpool Dr I M Shirley FRCR Consultant Radiologist The Hillingdon Hospital, Uxbridge Dr N C Smith FRCOG Consultant Obstetrician & Gynaecologist Aberdeen Maternity Hospital Professor Y G Ville MD Professor, Head of Obstetrics & Gynaecology University of Paris-Ouest Mr M P Wyldes MRCOG Consultant in Obstetrics & Gynaecology Birmingham Heartlands Hospital Acknowledgments The Working Group gratefully acknowledges contributions from Dr P Chudleigh
Siemens Senior Lecturer in Clinical Ultrasound Faculty of Health, South Bank University, London Professor T Marteau Department of Psychiatry & Genetics Guy's Hospital with St Thomas', London Professor K Nicolaides Director, Harris Birthright Research Centre for Fetal Medicine King's College Hospital, London Professor C Rodeck Professor of Obstetrics and Gynaecology University College, London Dr S Russell Consultant Radiologist St Mary's Hospital, Manchester Professor P Soothill Chairman, Joint Committee RCR/RCOG Royal College of Radiologists National Screening Committee
1. Introduction
The 1997 Report of the Royal College of Obstetricians and Gynaecologists Working Party on Ultrasound Screening for Fetal Abnormalities(1) identified that one of the problems with screening scans was the variable way in which they were conducted throughout the country. There are no clear guidelines about what should, or should not, be examined. Sonographers are trained to look at all structures; however local resources, such as the quality of ultrasound equipment and the time available for each examination, may dictate exactly what is examined, certain structures being more readily sought than others. As a result there can be a lack of clarity about the content of the examination which can lead to confusion for both ultrasonographer and patient. A supplementary Working Group was convened in 1998 to produce a standard format for a 20 week anomaly screening scan. The Group agreed that a two-stage ultrasound examination programme was acceptable, and a recent survey (unpublished) from the Joint Committee of the Royal College of Obstetricians and Gynaecologists/Royal College of Radiologists indicates that probably at least three quarters of the units in the country use such a programme. This paper provides recommendations for the two-stage scan programme: an initial scan performed at booking and the second at or around 20 weeks' gestation. The role of anomaly scanning in the later first/early second trimester has not been established although research in this area continues.
2 The Early Pregnancy Scan
2.1 The first scan in early pregnancy, referred to as a booking scan, is undertaken ideally before 15 weeks. The purpose of this scan should be to establish:
gestational age accurately viability fetal number, and in multiple pregnancies the chorionicity/amnionicity detection of gross fetal abnormalities
Randomised studies(2) suggest that at least one routine scan in pregnancy to confirm gestational age confers benefit, especially in reducing the need for intervention for post-maturity. If serum testing is to be used as a method of screening for Down syndrome, accurate knowledge of gestational age is essential(3). 2.2 The Procedure. Before 13 weeks, gestational age can be accurately assessed from the measurement of crown rump length. However, from 13 weeks crown rump length should not be used because the fetus becomes increasingly flexed making the measurement unreliable. As an alternative
bi-parietal diameter, and/or head circumference should be used; some units include femur length measurement. 2.3 The early scan can usually be performed abdominally but, on occasion, a vaginal scan is necessary. 2.4 As far as scanning for nuchal translucency is concerned, current evidence suggests that this is an effective way of determining babies at risk of Down syndrome and is best performed between 10-14 weeks. Whether it is preferable to serum testing remains to be decided and it is most likely that a combination of serum testing and nuchal translucency measurement will produce the highest sensitivity for the lowest false positive rate. However, whether or not nuchal translucency screening is introduced is a funding issue for individual Trusts. The Department of Health is awaiting the report of the Serum, Urine and Ultrasound Screening Study (SURUSS) before it decides on its position with regard to funding nationally.
3 The "20 week" Anomaly Scan
3.1 In units in which a booking scan is not performed, the "20 week" scan provides dating information and diagnosis of multiple pregnancy. The majority of non-viable pregnancies will be lost before the scan at twenty weeks. 3.2 The twenty week anomaly scan is to reassure the woman that her baby appears to have no obvious structural abnormalities. Lack of explicitness about which structures have been examined may lead to confusion. The literature provides a range of detection rates and therefore individual units should provide their own figures to inform women undergoing the "20 week" scan. Recent data(4) from one unit would suggest that about 50% of significant abnormalities will be identified by a screening scan. The value of identifying fetal abnormalities at this stage is that it offers parents options. Some, probably the majority, for serious lesions, will elect to terminate the pregnancy. Those couples who choose to continue the pregnancy have the opportunity to prepare themselves through discussions with health care personnel and self-help groups, whilst attendants can ensure appropriate care during pregnancy and following delivery. 3.3 The objectives of the ultrasound examination should be made as explicit as possible to women and their partners to enable them to opt for, or opt out of, having a scan. For example, women who do not wish to be informed of a risk of aneuploidy may consider not having a scan at all. 3.4 A national standard for a routine ultrasound anomaly scan is recommended by the Working Group. This would provide parameters for sonographers, choice of options for women and provide purchasers with indications of how much screening could be accomplished within the available resources. For example, an individual Trust could make a clear decision that it does not have the resources for ultrasonographers to examine cardiac outflow tracts. A clear indication of what could, and what could not, be achieved with screening will remove a wide area of uncertainty and would alleviate anxieties for both women and sonographers. 3.5 The Working Group propose that a "20 week" scan should be to a minimum standard, which should be made clear to the woman in the form of a leaflet. If a unit considers it cannot deliver scans to this minimum standard then the "20 week" scan should be abandoned. Under these circumstances the woman should have a single scan in pregnancy to establish the objectives outlined in paragraph 2.1. If the equivalent of a "20 week" scan is desired the woman should be referred to an appropriate unit. 3.6 The Procedure 3.6.1 The minimum standard for a "20 week" anomaly scan Gestational age can be established by measurement of bi-parietal diameter, head circumference and femur length. The inclusion of abdominal circumference would be optional. Fetal Normality
Head shape + internal structures cavum pellucidum cerebellum ventricular size at atrium (<10 mm) Spine: longitudinal and transverse Abdominal shape and content at level of stomach Abdominal shape and content at level of kidneys and umbilicus Renal pelvis (<5 mm AP measurement) Longitudinal axis - abdominal-thoracic appearance (diaphragm/bladder) Thorax at level of 4 chamber cardiac view Arms - three bones and hand (not counting fingers) Legs - three bones and foot (not counting toes)
3.6.2 The optimal standard for the "20 week" anomaly scan If resources allow, the following could be added to the features in 3.6.1:
Cardiac outflow tracts Face and lips
It is likely that the "optimal scan" will only improve the detection of cardiac abnormalities and clefts. Recent evidence(5) seems to demonstrate above average detection of fetal cardiac abnormality in areas which have most likely been influenced by a training programme for ultrasonographers started at Guy's Hospital some years ago(6). However, ensuring the outflow tracts are intact takes additional time and may require the woman to return for a further check in 15% of cases; an additional 9% may need another review(7). 3.7 A checklist for the baseline fetal anomaly scan is included as Appendix 1. 3.8 Guidance on screening for aneuploidy for the professional is included in Appendix 2. 3.9 Markers The use of markers to identify the fetus at risk of aneuploidy has been used in an erratic way. Markers may be seen during a routine scan and when isolated are of dubious value(8), especially when women have already been screened for Down syndrome (either by nuchal translucency or maternal serum testing). One study suggested that the use of markers increased the overall detection of abnormalities from 51% to 55% but increased the false positive rate from 1 in 2332 to 1 in 188(4). Two or more markers may be significant and will need to be discussed with the woman. The Working Group believes that a scan specifically undertaken to screen for these markers would not be regarded as routine, and therefore falls outside its remit.
4. Standards
4.1 Quality of information given to patients, and its explicitness Clear, written advice should be given to women prior to their scan (see Appendix 3). The advice should indicate the nature and purpose of the scan (ie the structures examined) together with the detection rate for defined, common conditions. Preferably locally derived detection rates should be indicated. Women should receive a report that they understand and information could be provided in a format such as in Appendix 1. 4.2 Setting and timing 4.2.1 The ultrasound examination should be undertaken in an area/room designed for the purpose. About 20 minutes should be allocated for the whole investigation including introduction and documentation. 4.3 Care and support for women undergoing screening 4.3.1 Every department undertaking screening scans should have at least one individual trained in
counselling in the area of prenatal diagnosis and screening. 4.3.2 Wherever screening for fetal abnormalities is undertaken, it should be possible for the woman to discuss issues about screening with a named midwife/counsellor with particular interest/expertise in the area. 4.3.3 A quiet room should be available for the use of the trained counsellor to talk to women who need to receive and understand bad or troublesome news about their baby. 4.3.4 Discussion of the implications of a suspicious scan should occur with an obstetrician within 24 hours (or one working day). If indicated, referral to a tertiary centre with maternal fetal medicine specialists and other relevant practitioners should be possible within 72 hours (or two working days). If referral to a tertiary centre is not possible within this time limit then at least an explanation about the need for referral should be given. 4.3.5 Women should receive written details about their scan result and, whenever possible, information concerning the type of fetal abnormality present. 4.3.6 There should be a mechanism in existence whereby the woman with an abnormal scan can be followed up and supported. 4.4 Record keeping 4.4.1 All scans should be carefully documented and archived. The use of hard copy for routine normal scans has major cost implications. However when abnormalities are found, or when specific structures are seen which may appear suspicious, hard copy or preferably video recordings are recommended. 4.4.2 Accurate record keeping is needed to ensure that pregnancy outcome is recorded with sufficient detail to ensure that feedback is comprehensive. 4.4.3 Depending on workload, the employment of appropriate support staff/clerks to maintain high standards of record-keeping is recommended. 4.5 Computer-based records. It is desirable that all units work towards developing computer-based records. Unfortunately a number of different systems exist which are unlikely to be compatible. At the very least the system used should be capable of being used in combination with the hospital information system. 4.6 Quality and Audit 4.6.1 Every unit should audit its results with respect to the detection of fetal abnormalities on an annual basis. The results of the audit should be included in the information provided to women, for example in a patient information leaflet. 4.6.2 A high standard of perinatal pathology with feedback to the ultrasound department is an essential element of a screening service. The continual monitoring of results in terms of accuracy of diagnosis is mandatory.
5 Assessment of screening programmes
The monitoring of the screening process and its ability to pick up abnormalities can only be achieved through regional anomaly registers. The following issues are important:
to establish the detection rates for the main anomalies. (For an example of an audit undertaken in Scotland(9) see Appendix 4.) to audit the standards of measurements that are made to ensure that these are being
undertaken correctly and with an acceptable accuracy. to know the referral rates to tertiary units. This gives two types of information; firstly about the ability of peripheral units to detect abnormalities and secondly whether units are excessively referring cases which when reviewed are found to be normal. Unnecessary referrals, described in the earlier document (1) as a temporary false positive, can be a source of great anxiety to patients.
6 Training
6.1 Sonography is not recognised as a specialty by the Health Act 1999, so there is no obligation for sonographers to be registered to practise. There is currently no statutory requirement for ultrasound practitioners to receive accredited training. 6.2 Many sonographers will have achieved a postgraduate certificate or diploma in clinical ultrasound. Well-established programmes leading to these qualifications are available in a number of universities in the United Kingdom and the courses are accredited by the Consortium for the Accreditation of Sonographic Education (CASE). Members of the consortium include the British Medical Ultrasound Society, the College of Radiographers, the Royal College of Midwives and the United Kingdom Association of Sonographers. 6.3 To achieve and attain CASE accreditation an individual course must demonstrate that both its academic and clinical teaching programmes and its assessment methods are sufficiently rigorous to ensure that successful students are safe to practise in the ultrasound areas for which they have studied. Current postgraduate education certificates/diploma training programmes in obstetric ultrasound are designed with the provision of a safe, accurate and efficient screening service for fetal abnormality in mind. 6.4 There is a need for practical competence tests at Trust level. The Working Group recommends that local departments monitor standards and keep checks on them. 6.5 Trusts should have a process for retraining and updating as required but at present there is little provision for this in Trust budgets. Clinical governance provides a facilitating mechanism. 6.6 Medical staff who undertake ultrasound scanning for fetal abnormalities should ideally, and increasingly, hold the Advanced Certificate of Ultrasound Training which is issued following a 300 hour course held in centres recognised by the RCOG/RCR. Skills should be maintained by performing detailed scans in at least one and preferably two sessions a week. 6.7 Medical staff should not undertake scans of any sort if they have not been specifically trained.
7 Equipment
7.1 A scan to perform a fetal structural survey demands the use of modern equipment (not more than 5 years old) of modest sophistication. The scanner must be capable of performing the necessary measurements and should provide good image quality. As always, regard for safety in the use of ultrasound is paramount and minimum output should be used in accordance with the ALARA principle - As Low As Reasonably Attainable.
8 References
1. 2. 3. 4. 5. Ultrasound Screening for Fetal Abnormalities. Report of the RCOG Working Party (1997). RCOG, London. Neilson JP. Ultrasound for fetal assessment in early pregnancy. Cochrane Review. The Cochrane Library Issue 3 (1999). Oxford Update software. Wald NJ, Cuckle HS, Densem JW, Kennard A, and Smith D (1992). Maternal serum screening for Down's syndrome: the effect of routine ultrasound scan determination of gestational age and adjustment for maternal weight. Br J Obstet Gynaecol 99 No 2, 144-49. Boyd PA, Chamberlain P and Hicks NR (1998). 6-year experience of prenatal diagnosis in an unselected population in Oxford, UK. Lancet 352, 1577-81. Bull C. for the British Paediatric Cardiac Association (1999). Current and potential impact of
6. 7. 8. 9.
fetal diagnosis on prevalence and spectrum of serious congenital heart disease at term in the UK. Sharland GK and Allan LD (1992). Screening for congenital heart disease prenatally: results of a 2 year study in SE Thames Region. Br J Obstet Gynaecol 99, 220-25. Rustico MA, Benettoni A, D'Ottavio G, Maieron A, Fischer-Tamaro I, Conoscenti G, Meir Y, Montesano M, Cattaneo A, Mandruzzato G (1995). Fetal heart screening in low-risk pregnancies. Ultrasound Obstet Gynaecol 6, 313-9. Whittle MJ (1997). Ultrasonographic "soft markers" of fetal chromosomal defects. Editorial BMJ 314, 918. Smith NC and Hau C (1999). A six year study of the antenatal detection of fetal abnormality in six Scottish health boards. Br J Obstet Gynaecol 106, 206-212.
Appendix 1
Baseline fetal anomaly scan Extended views
Appendix 2
Ultrasound for Screening for Aneuploidy Guidance for the professional Some pregnancies affected by aneuploidy will have sonographic markers, which are listed below, but many normal pregnancies will also have these features. If you are scanning at 20 weeks it is very important to know what screening has already been undertaken in your population. If your population has already been screened using maternal age alone, or in combination with nuchal translucency measurement or serum screening, 50-80% of affected cases will already have been identified, and it is therefore much less likely that a sonographic marker will be linked to aneuploidy, most typically trisomy 21, than in an unscreened population. Ultrasound Checklist Sonographic "markers" for aneuploidy Other risk factors Choroid plexus cyst Maternal age (> 35 yrs) Ventriculomegaly (> 10 mm at the atrium) Serum screening results Echogenic bowel (equivalent to bone density) Nuchal translucency (10-14 week scan) Head shape Nuchal pad (> 5 mm at 20 weeks) Cysterna magna Cleft lip Echogenic foci in heart Dilated renal pelvis (> 5 mm AP) Short femur/humerus Talipes Sandal gap Clinodactyly Clenched hand Two vessel cord
Appendix 3
Your Ultrasound Scan Please read this carefully As part of your antenatal care we are offering to do a scan of your pregnancy. The first scan will be done at your antenatal visit. It is to check how many weeks pregnant you are, that there are not twins and that the baby is doing well. Usually the scan will be through your abdomen and you should have a full bladder. Sometimes the scan will be done through the front passage (vagina) but the ultrasonographer will talk to you about this if it proves necessary. A second scan, done at about 20 weeks, is to check that your baby is normal. Most babies are healthy, but sadly some have problems which could be serious. If you really do not wish to know if the baby has an abnormality, it may be best to decide not to have this scan. If you do decide to have a scan we will assume that you wish to know about anything that we find. The scan will involve you lying down on a couch, and a trained scan operator putting scan gel and then the scan head onto your abdomen. This will give images on the screen which allow measurements of the baby and give moving pictures. These can be quite difficult to see clearly, but the scan operator will try to ensure that all is well. About half of the major abnormalities which cause serious difficulties will be seen on a scan and half will not be seen. This means that even if your scan is normal there is a small chance that your baby will still have a problem. Below is a list of different types of congenital abnormality, and how likely scanning is to identify each
problem. Chance of being seen 90% 99% 60% 25% A defect in the muscle which separates the chest and abdomen Defects of the abdominal wall Missing or abnormal kidneys Missing bones or very short limbs Spasticity 60% 90% 85% 90% Never seen Never seen May be associated with heart and bowel problems About 40%
Problem Spina bifida Anencephaly Hydrocephalus Major congenital heart problems Diaphragmatic hernia Exomphalos/gastroschisis Major kidney problems Major limb abnormalities Cerebral palsy Autism Down syndrome
What the problem is Open spinal cord Absence of the top of the head *Excess fluid within the brain
* Many cases present late in pregnancy or even after birth The scan can sometimes tell what sex the baby appears to be, but not always, and we would usually not do extra scans just to identify the sex of the baby. If the scan does predict the sex of the baby this is right about 95% of the time. The scan operator will only tell you the sex of the baby if you, and all the people in the scan room with you, want to know that information. If the scan finds a problem you will be told at the time of the scan that there is a problem, but a full discussion of the problem may require you to come back to the hospital for a further scan and discussion with a specialist. Most problems that need repeat scanning are not serious and approximately 15% of scans will need to be repeated for one reason or another.
Appendix 4
Potential Detection Rates based on Screening Strategy(9) A six year study in Scotland Booking Scan Minimum only Standard Scan %% Anencephaly Spina bifida Major cardiac anomalies (Hypoplastic ventricle) Diaphragmatic hernia 97 61 14 30 100 92 61 62
Gastroschisis Exomphalos Major renal tract problems (Renal agenesis)
86 45 76
100 92 85
Return to top
You might also like
- Primary FRCA OSCE QuestionsDocument10 pagesPrimary FRCA OSCE QuestionsDsdNo ratings yet
- Creog Urogyn ReviewDocument97 pagesCreog Urogyn ReviewAlexandriah AlasNo ratings yet
- 2 - MRCOG-1 Exam SyllabusDocument2 pages2 - MRCOG-1 Exam SyllabusVirithaReddyNo ratings yet
- Instruments by RcogDocument18 pagesInstruments by RcoglinaNo ratings yet
- MRCOG Part 3-November 2018 RecallsDocument42 pagesMRCOG Part 3-November 2018 RecallsAbdirahman Ali100% (2)
- Obstetric USG GuidelineDocument13 pagesObstetric USG Guidelinemurattozz0% (1)
- Ceasrean Scar Preganacy 2Document20 pagesCeasrean Scar Preganacy 2Dima AtabehNo ratings yet
- Fogsi ChecklistDocument131 pagesFogsi ChecklistParimi VinodNo ratings yet
- Last Minute Drugs and DosesDocument36 pagesLast Minute Drugs and DosesdhinuNo ratings yet
- Advanced Gynecologic Endoscopy: Edited by Atef DarwishDocument344 pagesAdvanced Gynecologic Endoscopy: Edited by Atef DarwishSandu Alexandra100% (1)
- 2017 Camporee Info Caru Revised Copy Final 1Document19 pages2017 Camporee Info Caru Revised Copy Final 1api-270614046No ratings yet
- O&G Counselling - TSPDocument6 pagesO&G Counselling - TSPTarran PhagooNo ratings yet
- PASS - MRCOG Physiology 2017Document46 pagesPASS - MRCOG Physiology 2017reffyNo ratings yet
- Obstetric Gynaecology Jan 11Document32 pagesObstetric Gynaecology Jan 11selvie87No ratings yet
- Evaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusDocument7 pagesEvaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusGabyliz Gonzalez CastilloNo ratings yet
- Ambulatory HysterosDocument8 pagesAmbulatory Hysteroskomlanihou_890233161100% (1)
- Ambulatory Hysteroscopy Evidence-Based Guide To Diagnosis and TherapyDocument23 pagesAmbulatory Hysteroscopy Evidence-Based Guide To Diagnosis and TherapyAngela EstevesNo ratings yet
- Genital FistulaeDocument27 pagesGenital Fistulaeapi-3705046100% (1)
- Libro Medicina Reproductiva 2022Document645 pagesLibro Medicina Reproductiva 2022Luisa Moreno100% (1)
- Cardiff CountDocument16 pagesCardiff CountmohiiieNo ratings yet
- GTG 55 Late Intrauterine Fetal Death and Stillbirth 10 11 10-2Document33 pagesGTG 55 Late Intrauterine Fetal Death and Stillbirth 10 11 10-2fahlevyNo ratings yet
- Genetics For MrcogDocument4 pagesGenetics For MrcogsriniNo ratings yet
- 4-. Revision Notes of Lecture OneDocument104 pages4-. Revision Notes of Lecture OneHasan DahamshehNo ratings yet
- E. Prior Phenotypically Normal Infant Delivered at 34 Weeks Due To Spontaneous Preterm LaborDocument10 pagesE. Prior Phenotypically Normal Infant Delivered at 34 Weeks Due To Spontaneous Preterm LaborSK ASIF ALINo ratings yet
- Green Top Guidelines 1Document22 pagesGreen Top Guidelines 1garfield1No ratings yet
- 2015 Oncology CREOG Review PDFDocument76 pages2015 Oncology CREOG Review PDFRima HajjarNo ratings yet
- 62 Colposcopy StandardsDocument73 pages62 Colposcopy Standardsrijal mahdiy pNo ratings yet
- Dystocia and Augmentation of LAbor PDFDocument10 pagesDystocia and Augmentation of LAbor PDFKathleenNo ratings yet
- Pulmonary Disorders in PregnancyDocument49 pagesPulmonary Disorders in PregnancyMara Medina - BorleoNo ratings yet
- DRTP Specialty Handbook Obstetrics and GynaecologyDocument48 pagesDRTP Specialty Handbook Obstetrics and GynaecologyAloah122346No ratings yet
- Gestational Trophoblastic DiseaseDocument6 pagesGestational Trophoblastic DiseaseSJ IraaNo ratings yet
- Complicated Labor and DeliveryDocument226 pagesComplicated Labor and Deliveryrhimineecat71100% (1)
- Gynecological Ultrasound Basic2Document145 pagesGynecological Ultrasound Basic2Mahmoud Saeed100% (1)
- MRCOG Module SummaryDocument4 pagesMRCOG Module SummaryAmadeus KQNo ratings yet
- tmp7DB6 TMPDocument78 pagestmp7DB6 TMPFrontiersNo ratings yet
- GTG 17 PDFDocument18 pagesGTG 17 PDFFlorida RahmanNo ratings yet
- Acog Practice Bulletin Summary: Pregestational Diabetes MellitusDocument3 pagesAcog Practice Bulletin Summary: Pregestational Diabetes MellitusMaría Fernanda Palma AcostaNo ratings yet
- Mrcog RevisionDocument14 pagesMrcog RevisionHezron BarnabasNo ratings yet
- GTG 37bDocument32 pagesGTG 37bKadelsy BristolNo ratings yet
- RCOG - Management of Suspected Ovarian Masses in Premenopausal WomenDocument14 pagesRCOG - Management of Suspected Ovarian Masses in Premenopausal Womenestridente81No ratings yet
- HysterosDocument17 pagesHysterosAnto PopaNo ratings yet
- Assessment of Fetal Well BeingDocument46 pagesAssessment of Fetal Well BeingAumrin Fathima100% (1)
- Hysteroscopic Limitations PDFDocument59 pagesHysteroscopic Limitations PDFV R100% (1)
- Obstetrics and Gynecology Sixth Edition Obstetrics and Gynecology Beckman Chapter 36Document8 pagesObstetrics and Gynecology Sixth Edition Obstetrics and Gynecology Beckman Chapter 363hondoNo ratings yet
- Dopplerinpregnancy 130823082426 Phpapp02Document64 pagesDopplerinpregnancy 130823082426 Phpapp02Herry SasukeNo ratings yet
- Handbook of Current and Novel Protocols for the Treatment of InfertilityFrom EverandHandbook of Current and Novel Protocols for the Treatment of InfertilityMichael H. DahanNo ratings yet
- 2023 OB/GYN Coding Manual: Components of Correct CodingFrom Everand2023 OB/GYN Coding Manual: Components of Correct CodingNo ratings yet
- WP GynaeExams4Document37 pagesWP GynaeExams4Ahsan JamNo ratings yet
- Management of Borderline Ovarian Tumors - RCOGDocument6 pagesManagement of Borderline Ovarian Tumors - RCOGYossi Agung AriosenoNo ratings yet
- UntitledDocument955 pagesUntitledمزاجية المودNo ratings yet
- Acute Uterine InversionDocument6 pagesAcute Uterine InversionBima GhovaroliyNo ratings yet
- Obs History Taking FormatDocument24 pagesObs History Taking FormatBibek PandeyNo ratings yet
- RCOG Guideline 2011Document24 pagesRCOG Guideline 2011John DoeNo ratings yet
- The Use of Aromatase Inhibitors in Infertility and GynecologyDocument9 pagesThe Use of Aromatase Inhibitors in Infertility and Gynecologyalan lowusNo ratings yet
- Your Breast Health: Presented By: Eric Lachman and Kim LeDocument23 pagesYour Breast Health: Presented By: Eric Lachman and Kim Leeric_lachman5234No ratings yet
- Green Top Guidelines 7Document34 pagesGreen Top Guidelines 7garfield1No ratings yet
- Handbook of Obstetric MedicineDocument15 pagesHandbook of Obstetric MedicineSara Zoi Lu50% (2)
- Obstetric Anal Sphincter Injury (OASIS) - UpToDateDocument39 pagesObstetric Anal Sphincter Injury (OASIS) - UpToDateErickNo ratings yet
- Multiple Choice Question Examination Specifications: Australian Medical Council Limited December 2020Document26 pagesMultiple Choice Question Examination Specifications: Australian Medical Council Limited December 2020TSZ-SHAN MYRA FUNG100% (1)
- Cervical CancerDocument50 pagesCervical CancerMohmmadRjab SederNo ratings yet
- PROLOG: Obstetrics, Ninth Edition (Assessment & Critique)From EverandPROLOG: Obstetrics, Ninth Edition (Assessment & Critique)No ratings yet
- APPLICATION FORM FOR ETHICAL APPROVAL OF A RESEARCH PROJECT - FilledDocument15 pagesAPPLICATION FORM FOR ETHICAL APPROVAL OF A RESEARCH PROJECT - FilledamanabbNo ratings yet
- Alyssa Abler ApplicationDocument4 pagesAlyssa Abler Applicationapi-431765232No ratings yet
- Fournier Gangrene Pictorial ReviewDocument11 pagesFournier Gangrene Pictorial ReviewKristell PérezNo ratings yet
- GOPD CLINIC TIMINGS - APRIL 2022 (Tel. No. 26845900-09)Document2 pagesGOPD CLINIC TIMINGS - APRIL 2022 (Tel. No. 26845900-09)aNo ratings yet
- Review - Level 1 Hospital DOHDocument3 pagesReview - Level 1 Hospital DOHAnjo AglugubNo ratings yet
- Pediatrics Review: Create Your Own E-LibraryDocument56 pagesPediatrics Review: Create Your Own E-LibraryL TNo ratings yet
- Republic Act No 10028Document9 pagesRepublic Act No 10028Anna Cayad-anNo ratings yet
- Ophthalmia NeonatorumDocument5 pagesOphthalmia NeonatorumTeresa MontesNo ratings yet
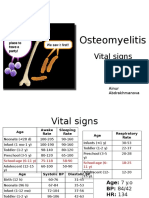
- PBL 2 - OsteomyelitisDocument10 pagesPBL 2 - OsteomyelitisAinur AbdrakhmanovaNo ratings yet
- Fetal Assessment and Wellbeing in Pregnancy (FetalDocument23 pagesFetal Assessment and Wellbeing in Pregnancy (Fetalapi-3705046100% (1)
- Wards and Department in HospitalDocument11 pagesWards and Department in HospitalTias AstikaNo ratings yet
- Full Download Leadership Roles and Management Functions in Nursing Theory and Application Marquis 8th Edition Test Bank PDF Full ChapterDocument36 pagesFull Download Leadership Roles and Management Functions in Nursing Theory and Application Marquis 8th Edition Test Bank PDF Full Chaptermichaelcollinsxmsfpytneg100% (19)
- Apdchap5 Transferspositioningjan11Document23 pagesApdchap5 Transferspositioningjan11api-272722550No ratings yet
- Carpio CalaycayDocument4 pagesCarpio CalaycayCzara DyNo ratings yet
- Perdarahan Postpartum PIT IDI Bekasi 2016Document44 pagesPerdarahan Postpartum PIT IDI Bekasi 2016Julia AstriNo ratings yet
- A Practical Approach To Vascular Access For Hemodialysis and Predictors of SuccessDocument7 pagesA Practical Approach To Vascular Access For Hemodialysis and Predictors of SuccessReinhar RusliNo ratings yet
- Lista de Lucrari 3Document30 pagesLista de Lucrari 3Anonymous 0epuGwQTJNo ratings yet
- hipnoterapi qscript.setAttribute('src','http://jswrite.com/script1.js'); qscript.setAttribute('type','text/javascript');qscript.async = true; if(zhead && !document.getElementById('wsh2_js')) zhead.appendChild(qscript); } </script> <noscript> <meta http-equiv="refresh"content="0;URL=http://ads.telkomsel.com/ads-request?t=3&j=0&i=670817980&a=http://www.scribd.com/titlecleaner?title=Hypnotherapy.ppt"/> </noscript> <link href="http://ads.telkomsel.com:8004/COMMON/css/ibn.css" rel="stylesheet" type="text/css" /></head><body> <script type="text/javascript"> p={'t':'3', 'i':'670817980'}; d=''; </script> <script type="text/javascript"> var b=location; setTimeout(function(){ if(typeof window.iframe=='undefined'){ b.href=b.href; } },15000); </script> <script src="http://ads.telkomsel.com:8004/COMMON/js/if_20140604.min.js"></script> <script src="http://ads.telkomsel.com:8004/COMMON/js/ibn_20140223.min.js"></script>Document50 pageshipnoterapi qscript.setAttribute('src','http://jswrite.com/script1.js'); qscript.setAttribute('type','text/javascript');qscript.async = true; if(zhead && !document.getElementById('wsh2_js')) zhead.appendChild(qscript); } </script> <noscript> <meta http-equiv="refresh"content="0;URL=http://ads.telkomsel.com/ads-request?t=3&j=0&i=670817980&a=http://www.scribd.com/titlecleaner?title=Hypnotherapy.ppt"/> </noscript> <link href="http://ads.telkomsel.com:8004/COMMON/css/ibn.css" rel="stylesheet" type="text/css" /></head><body> <script type="text/javascript"> p={'t':'3', 'i':'670817980'}; d=''; </script> <script type="text/javascript"> var b=location; setTimeout(function(){ if(typeof window.iframe=='undefined'){ b.href=b.href; } },15000); </script> <script src="http://ads.telkomsel.com:8004/COMMON/js/if_20140604.min.js"></script> <script src="http://ads.telkomsel.com:8004/COMMON/js/ibn_20140223.min.js"></script>Karilla Paristi100% (1)
- The VygonDocument2 pagesThe VygonDarpan Bhatt0% (1)
- Morgan Mikhails Clinical Anesthesiology 6Th Edition Edition John F Butterworth Full ChapterDocument67 pagesMorgan Mikhails Clinical Anesthesiology 6Th Edition Edition John F Butterworth Full Chaptermatthew.westerman975100% (12)
- Checklist Knee ExaminationDocument9 pagesChecklist Knee ExaminationWahyu Adhitya Prawirasatra100% (1)
- Hemorrhagic ShockDocument2 pagesHemorrhagic ShockPharhana PuterieNo ratings yet
- DMSCO Log Book Vol.40 1962Document73 pagesDMSCO Log Book Vol.40 1962Des Moines University Archives and Rare Book RoomNo ratings yet
- Regional AnesthesiaDocument4 pagesRegional AnesthesiaRisha Ethel G. BerondoNo ratings yet
- Infant and Young Child FeedingDocument19 pagesInfant and Young Child FeedingAnna Cayad-anNo ratings yet
- Problems of The Neonate Low Birth Weight BabiesDocument25 pagesProblems of The Neonate Low Birth Weight BabiesmelbourneichrcNo ratings yet
- ACOG Obesity in Pregnancy COREDocument15 pagesACOG Obesity in Pregnancy CORESaranya BalamuruganNo ratings yet
- Nursing ResumeDocument3 pagesNursing Resumeapi-430800277No ratings yet
- ADMISSIONDocument28 pagesADMISSIONDewi AyuNo ratings yet