Professional Documents
Culture Documents
Head To Toe Assesment
Uploaded by
Fauzia FatharaniOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Head To Toe Assesment
Uploaded by
Fauzia FatharaniCopyright:
Available Formats
Head-to-Toe Assessment - Initial Survey: Check ABCs LOC (Awake, alert/lethargic/unresponsive) Orientation (to person, place and time)
Neuro check (PERRLA/Glasgow Coma Scale if appropriate) Skin color (pale/pink/ruddy/cyanotic/dusky) Skin temp (cool/cold/warm/hot) Skin texture (dry/diaphoretic) Skin lesions/pressure or statis ulcers/ecchymoses: color, drainage, odors, LxWxD in cm VS T (include route), P, R, BP/5th VS = PAIN S2S1, Apical-rate, Rhythm (regular/irregular/regularly irregular) Intensity (loud/distant) O2 and Pulse Ox Effort (easy/unlabored) Depth (deep/shallow/blowing)/Auscultation-ant/lat/post * Chest tubes/need for suctioning/advanced skills, i.e. tactile fremitus/diaphragmatic excursion if applicable Upper extremities if IV present note: gauge, solution, rate and infusion pump/controller. Assess IV site for: warmth, redness, edema, drainage or tenderness. Abdomen inspect (round/flat/obese/distended) * Any PEG, G-tube, NG-tube, Dobhoff tube? Auscultate (BS present x 4 quads? rhythm of BS normal/hyper/hypoactive and the intensity high/low-pitched) Palpate (soft/firm/hard/tender to light and deep palpation?) Abdomen (continued) Bowel: Last BM (size/color/consistency/odor) Postop flatus? Incontinence urinary or fecal or both? GU: Void/ Foley/ Suprapubic/Fr and balloon size, amount, color, presence of mucus/sediment, odor. Note patency and describe urine in dependent drainage bag tubing. Ostomy? (note condition of stoma and skin surrounding stoma/contents of ostomy bag-phalange or bag change/clients adaptation to ostomy) Lower extremities Homans sign (negative/positive) - with positive being a bad sign possibly indicative of DVT. Pedal pulses (Dorsalis Pedis/Posterior tibial, compare bilaterally, Grading (0 - +4)/check for edema) pitting (+1 - +4)/nonpitting? Capillary refill (brisk/sluggish-how long, >3 seconds) ROM, Gait Dressings, drains or wounds should be assessed and documented in the order they appear in the assessment i.e. RUE RLE. If a circulation check is done, place that information in the order it was assessed. Circulation Assessment, include: color/warmth/pulse/ capillary refill/movement and always compare bilaterally. Client Education: Include how client learns best, teaching done and client response.
PHYSICAL ASSESSMENT GUIDE NEUROPSYCHOLOGICAL
MENTAL STATUS: o Oriented o Person o Place o Time o Date o Alert o Dull Affect
SPEECH o Clear o Other_______________
STIMULUS RESPONSE: o Verbal o Touch o Pain
BEHAVIOR:
o Cooperative o Uncooperative o Combative o Anxious o Depressed o Restless o Unresponsive o Confused (explain)___________ o Other (explain)______________
GENERAL: o Syncope o Dizziness o Malaise o Seizures o Memory loss o Insomnia o Other______________________ COMMENTS:
HEAD/NECK:
o Symmetrical o Range of motion o Oral mucosa o Pink o Other_______________ o Moist o Dry o Teeth present condition___ o Teeth absent____________
EYES: o Drainage o Pupils o Equal o Unequal o React to light o Accommodate o Sclera o White o Jaundice o Other___________________
o Conjunctiva o Pink o Pale o Other___________________ EARS: o Drainage COMMENTS:
MUSCULOSKELETAL: o Symmetrical muscles o Full ROM o Absence of joint swelling o Full muscle strength o Steady gait o Other______________________ COMMENTS:
RESPIRATORY: Rate_______________ o Effort o Norma; o Shallow o Hyperpnea
o Wheezing o Dyspnea o Apneic periods o Orthopnea o Labored o Painful o Other______________ o Rhythm o Regular o Irregular o Sounds o Equal o Clear o Other COMMENTS:
CARDIOVASCULAR: o Apical pulse o Regular o Irregular o Rate______________
o Jugular Neck Distention o Pain
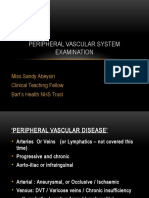
PERIPHERAL VASCULAR: o Pulses RT LT o Carotid_____________ o Radial______________ o Brachial____________ o Femoral____________ o Popliteal____________ o Posterior tibial_______ o Dorsalis pedis________ o Rhythm o Regular o Irregular o Homans o Pain o Blood pressure o Right arm o Left arm COMMENTS:
GASTROINTESTINAL: o Abdomen o Soft o Distended o Painful o Rigid o Other_________________ o Bowel sounds o URQ o LLQ o LLQ o RLQ o Intake/Appetite o Percentage____________ o Dysphagia o Trouble chewing o Nausea o Vomiting o Weight loss o Weight gain
o Other_________________
Food Intolerances:
BOWEL HABITS: o Frequency____________________ o Diarrhea o Constipation o Date last BM__________________ o Aids for elimination____________ o Color o Black o Bloody o Other________________ COMMENTS:
RENAL/UROLOGICAL: o Urine flow o No problems o Urgency o Incontinent
o Burning o Hesitancy o Dysuria o Hematuria o Frequency o Other_________________ o Appearance/color_______________ COMMENTS:
INTEGUMENTARY: o Coloring o Skin o Pink o Cyanotic o Jaundice o Other_________________ o Texture/Turgor o Dry o Moist o Inelastic o Other_________________
o Nail beds o Pink o Pale o Cyanotic o Capillary blanching__sec o Edema o Absent o Pedal o Sacral COMMENTS
You might also like
- PT Seated, Facing Examiner Doctor-Pt Interactions: Response To Light (CN II, III) & Visual Fields (CN II)Document2 pagesPT Seated, Facing Examiner Doctor-Pt Interactions: Response To Light (CN II, III) & Visual Fields (CN II)Anonymous fj68MsNo ratings yet
- Head To Toe AssessmentDocument3 pagesHead To Toe Assessmentsandaman2225No ratings yet
- PVD Case ProformaDocument2 pagesPVD Case ProformaRiyaSinghNo ratings yet
- Physical ExaminationDocument5 pagesPhysical ExaminationAmniAzmi100% (1)
- 1st Assessment 2nd Assessment: VitalsDocument1 page1st Assessment 2nd Assessment: Vitalsiluvmy3galsnjeffNo ratings yet
- Focused AssessmentDocument5 pagesFocused AssessmentPiyali SahaNo ratings yet
- System Exams - Promotion Exam MusculoskeletalDocument4 pagesSystem Exams - Promotion Exam Musculoskeletalespo176No ratings yet
- OSCE SURGERY ايناس صالحDocument9 pagesOSCE SURGERY ايناس صالحmahmoud alhelal100% (1)
- Physical Exam-1 2022 RevampDocument6 pagesPhysical Exam-1 2022 RevampAnanya ANo ratings yet
- Physical Assessment FormatDocument24 pagesPhysical Assessment FormatSruthi Krishna100% (1)
- Comfort/sleep Well?: (Or Observe/stimulate)Document4 pagesComfort/sleep Well?: (Or Observe/stimulate)kayewhite02No ratings yet
- Peripheral Arterial Disease ExaminationDocument3 pagesPeripheral Arterial Disease Examinationjackfruit5887No ratings yet
- AssessmentDocument1 pageAssessmentpradeepeee08kingNo ratings yet
- Physical Assessment Head To ToeDocument4 pagesPhysical Assessment Head To ToeFely Theresa Lanes Loreno95% (43)
- Comfort/sleep Well? Prior To Eating/feeding)Document3 pagesComfort/sleep Well? Prior To Eating/feeding)John MelanconPhotographyNo ratings yet
- Examination of Varicose VeinDocument4 pagesExamination of Varicose VeinManas RanjanNo ratings yet
- Assessment SheetDocument1 pageAssessment SheetnkuligowskiNo ratings yet
- Peripheral Vascular AssessmentDocument11 pagesPeripheral Vascular AssessmentPaul P. YambotNo ratings yet
- AbdomenDocument7 pagesAbdomenAbhishek DussaNo ratings yet
- Physical Exam SheetDocument6 pagesPhysical Exam SheetDidi SaputraNo ratings yet
- Peripheral Vascular Exam OSCE GuidesDocument5 pagesPeripheral Vascular Exam OSCE GuidesYusnida RahmawatiNo ratings yet
- Post Op CareDocument1 pagePost Op CareAishwarya SivakumarNo ratings yet
- Head To Toe Assessment GuideDocument3 pagesHead To Toe Assessment GuideUmer Masood0% (1)
- Rs ExaminationDocument7 pagesRs ExaminationMiracle MathangiNo ratings yet
- Physical Assessment Learning Guide Med SurgDocument4 pagesPhysical Assessment Learning Guide Med SurgTremain LinsonNo ratings yet
- Examination of Hip JointDocument8 pagesExamination of Hip JointRebecca WongNo ratings yet
- UntitledDocument5 pagesUntitledPinimNo ratings yet
- GridDocument4 pagesGridCarmen MartinezNo ratings yet
- Hip Joint AssessmentDocument8 pagesHip Joint AssessmentmaitriNo ratings yet
- Cardiovascular Examination: Preparation of The PatientDocument4 pagesCardiovascular Examination: Preparation of The PatientLolla SinwarNo ratings yet
- Physical ExaminationDocument10 pagesPhysical ExaminationChristine NaNo ratings yet
- Peripheral Vascular ExaminationDocument27 pagesPeripheral Vascular ExaminationnurminsyahNo ratings yet
- Assessin Thorax and LungsDocument62 pagesAssessin Thorax and LungssrslytrdNo ratings yet
- GridDocument2 pagesGridJohn MelanconPhotography100% (1)
- NUR 317L Head-to-Toe Assessment 8 NUR 317L Head-to-Toe Assessment 8Document4 pagesNUR 317L Head-to-Toe Assessment 8 NUR 317L Head-to-Toe Assessment 8Mary LowryNo ratings yet
- Clinical Examinations Crib Sheet v7Document36 pagesClinical Examinations Crib Sheet v7aparish10100% (1)
- CVS Examination ProformaDocument4 pagesCVS Examination ProformaAnantha KrishnanNo ratings yet
- Head To ToeDocument4 pagesHead To Toenazbeen.ahmadiNo ratings yet
- CSI Physical ExamDocument3 pagesCSI Physical ExamSympaschoNo ratings yet
- Clinical Assessment DatasheetDocument2 pagesClinical Assessment DatasheetBeth Crosson-DendlerNo ratings yet
- Head To Toe AssessmentDocument7 pagesHead To Toe AssessmentShine TorricerNo ratings yet
- Comfort/sleep Well? Prior To Eating/feeding)Document3 pagesComfort/sleep Well? Prior To Eating/feeding)kayewhite02No ratings yet
- Comfort/sleep Well?: (Or Observe/stimulate)Document4 pagesComfort/sleep Well?: (Or Observe/stimulate)kayewhite02No ratings yet
- The Complete Physical Assessment GuideDocument10 pagesThe Complete Physical Assessment GuideHappy CherryNo ratings yet
- Normal PE Sample Write-UpDocument5 pagesNormal PE Sample Write-UpMikie BausinNo ratings yet
- Head To Toe AssessmentDocument2 pagesHead To Toe AssessmentBen0% (1)
- Postop Checklist-1Document1 pagePostop Checklist-1Jona josfin JecinthNo ratings yet
- Cheat SheetDocument1 pageCheat SheetGarry LeeNo ratings yet
- VSS - BP, HR, Temp, RR, Sp02. Methods of AssessmentDocument1 pageVSS - BP, HR, Temp, RR, Sp02. Methods of AssessmentGarry LeeNo ratings yet
- AbdomenDocument7 pagesAbdomenMiracle MathangiNo ratings yet
- Diabetic FootDocument2 pagesDiabetic FootShatha AlgahtaniNo ratings yet
- Rs Case SheetDocument8 pagesRs Case SheetBhanu PrakashNo ratings yet
- GIT NotesDocument6 pagesGIT Notesco230156No ratings yet
- Clinical History Taking Format in Medicine - Physical, Systemic ExaminationDocument3 pagesClinical History Taking Format in Medicine - Physical, Systemic ExaminationNishad PatelNo ratings yet