Professional Documents
Culture Documents
Canadian GMP Draft Guidelines 2007
Uploaded by
peruvdOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Canadian GMP Draft Guidelines 2007
Uploaded by
peruvdCopyright:
Available Formats
Health Products and Food Branch Inspectorate Graham Spry Building, 2nd Floor 250 Lanark Avenue Address
Locator # 2002B OTTAWA, Ontario K1A 0K9 December 8, 2006 06-125600-3
To: ALL INTERESTED PARTIES I am pleased to inform you that Health Canada has revised the guidance document entitled Good Manufacturing Practices Guidelines, which is now available for comments on Health Canadas Compliance and Enforcement website at: http://www.hc-sc.gc.ca/dhp-mps/compli-conform/index_e.html The present edition of this document has been reviewed and amended providing a clearer understanding of the application of regulatory requirements to facilitate compliance by the regulated industry and to enhance consistency in the application of the regulatory requirements. The major changes includes revisions to the following sections: Personnel (C.02.006), Raw Material Testing (C.02.009), Quality Control Department (C.02.015), Finished Product Testing (C.02.019), Samples (C.02.026), Sterile Products (C.02.029) and the Glossary of Terms. It reflects most of the recent proposed regulatory amendments, modified and/or new terminology, the incorporation of most GMP questions and answers, additional requirements such as annual product quality review, additional interpretations, and an updated table of requirements. Please note, for your convenience, the guideline features redline/strikeout in order for you to be able to view all differences from the 2002 version. The guideline is available in Portable Document Format (PDF) only. All comments must be based on the PDF format referring to the respective specific line number provided.
.../2
-2-
This document is published as a draft document for comments. Please note that every comment received within 75 days of delivery of this letter will be reviewed and considered for the final version of the document. Please submit your comments in writing by mail to the Manager, Drug GMP Inspection Unit, HPFB Inspectorate, Graham Spry Building, A.L. #2002B, 250 Lanark Avenue, Ottawa, Ontario, K1A 0K9, by fax at (613) 957-6709, or by e-mail at GMP_questions_BPF@hc-sc.gc.ca .
Original signed by Diana Dowthwaite Director General
1 2 3 4 5 6 7 8 9 10 11 12 13
Health Canada Health Products and Food Branch
OUR MANDATE:
To p romote good nutrition and informed use of drugs, food, medical devices and natural health products, and to maximize the safety and efficacy of drugs, food, natural health products, medical devices, biologics and related biotechnology products in the Canadian marketplace and health system.To take an integrated approach to managing the health-related risks and benefits of health products and food by minimizing health risk factors to Canadians while maximizing the safety provided by the regulatory system for health products and food, and prom oting conditions that enable Canadians to make healthy choices and providing information so that they can make informed decisions about their health.
14 15 16 17 18 19 20 21
Health Products and Food Branch Inspectorate GOOD MANUFACTURING PRACTICES (GMP) GUIDELINES
20022007 EDITION Version 2
GUIDE-0001
Supersedes: 2002 Edition, Version 2 Date issued: 2003-01-20 Draft for comments Date of implementation: 2003-02-01 Ce document est aussi disponible en franais.
22 23 24 25 26 27 28
Health Canada / Health Products and Food Branch Inspectorate
29
TABLE OF CONTENTS
30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68
1. INTRODUCTION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . page 4 2. PURPOSE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . page 4 3. SCOPE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . page 4 4. QUALITY MANAGEMENT . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.1 GUIDING PRINCIPLE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2 RELATIONSHIP AMONG QUALITY ELEMENTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2.1 QUALITY ASSURANCE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2.2 GOOD MANUFACTURING PRACTICES (GMP) FOR DRUGS . . . . . . . . . . . . 4.2.3 QUALITY CONTROL . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5. REGULATION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.002 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . SALE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.003 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . PREMISES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.004 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . EQUIPMENT . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.005 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . PERSONNEL . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.006 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . SANITATION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.007 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.008 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . RAW MATERIAL TESTING . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.010 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . MANUFACTURING CONTROL . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.011 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.012 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . QUALITY CONTROL DEPARTMENT . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.013 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.014 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.015 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . PACKAGING MATERIAL TESTING . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.016 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.017 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . FINISHED PRODUCT TESTING . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.018 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.019 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . RECORDS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
page 6 page 6 page 6 page 6 page 7 page 8 page 10 page 10 page 10 page 10 page 10 page 10 page 14 page 14 page 17 page 17 page 19 page 19 page 21 page 23 page 23 page 26 page 29 page 29 page 37 page 41 page 41 page 42 page 44 page 49 page 49 page 50 page 52 page 53 page 54 page 58
Page 2
Health Canada / Health Products and Food Branch Inspectorate
69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93
C.02.020 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.021 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.022 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.024 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . SAMPLES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.025 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.026 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . STABILITY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.027 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.028 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . STERILE PRODUCTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.029 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . MEDICAL GASES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C.02.030 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
page 58 page 59 page 59 page 59 page 60 page 63 page 63 page 64 page 66 page 66 page 67 page 71 page 71 page 90 page 90
APPENDIX A - INTERNATIONALLY HARMONIZED REQUIREMENTS FOR BATCH CERTIFICATION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . page 91 APPENDIX A1 CONTENT OF THE FABRICATORS/MANUFACTURERS BATCH CERTIFICATE FOR DRUG/MEDICINAL PRODUCTS EXPORTED TO COUNTRIES UNDER THE SCOPE OF A MUTUAL RECOGNITION AGREEMENT (MRA) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . page 92 APPENDIX B - ACRONYMS - GLOSSARY OF TERMS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . page 95 APPENDIX C - REFERENCES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . page 109 DRUG GMP COMMITTEE MEMBERS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . page 112 HEALTH PRODUCTS AND FOOD BRANCH INSPECTORATE - OPERATIONAL CENTRESage 114 p
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 3
Health Canada / Health Products and Food Branch Inspectorate
94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121
1. INTRODUCTION
These guidelines on Good Manufacturing Practices (GMP) refer pertain to Division 2, Part C of the Food and Drug Regulations. The guidelines apply to pharmaceutical, radiopharmaceutical, biological, and veterinary drugs and were developed by Health Canada in consultation with their stakeholders. These guidelines are designed to facilitate compliance by the regulated industry and to enhance consistency in the application of the regulatory requirements. Division 1A, Part C of the Food and Drug Regulations defines activities for which GMP compliance is to be demonstrated prior to the issuance of an a drug establishment licence. In addition to these guidelines, further guidance in specific areas is provided in the annexes Appendix C to this document or in separate documents. The content of this document should not be regarded as the only interpretation of the GMP Regulations, nor does it intend to cover every conceivable case. Alternative means of complying with these Regulations can be considered with the appropriate scientific justification. Different approaches may be called for as new technologies emerge. The guidance given in this document has been written with a view to harmonization harmonize with GMP standards from other countries and with those of the World Health Organization (WHO), the Pharmaceutical Inspection Cooperation/Scheme (PIC/S) and the International Conference on Harmonization (ICH). The present edition of thisThis document reflects takes into account the results of regulatory revisions due to the implementation of the current Mutual Recognition Agreements (MRA) Framework. The MRA establish mutual recognition of GMP compliance certification between Regulatory Authorities that are designated as equivalent. and assessment methods by regulatory authorities of countries designated as equivalent. Exemptions from requirements under C.02.012 (2) and C.02.019 (1) and (2) are provided for importers of drugs where all activities (fabrication, packaging/labelling and testing) are carried out in MRA countries. All other regulatory requirements described in the Food and Drug Regulations apply. The present edition of this document reflects recent regulatory amendments, modified and/or new terminology, the incorporation of most GMP questions and answers, additional requirements such as annual product quality review, additional interpretations, and an updated table of requirements.
122 123 124 125
2. PURPOSE
To provide interpretive guidance for Part C, Division 2, of the Food and Drug Regulations. These guidelines are designed to facilitate compliance by the regulated industry and to enhance consistency in the application of the regulatory requirements.
126 127
3. SCOPE
The guidelines apply to pharmaceutical, radiopharmaceutical, biological, and veterinary drugs and were
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002 Page 4
Health Canada / Health Products and Food Branch Inspectorate
128
developed by Health Canada in consultation with their stakeholders.
129 130 131
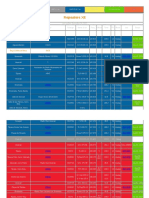
GMP Sections applying to the establishment activity GMP Regulations Applicable to Licensable Activities
Section Regulati on F P/ L I (n o nM R A) I (M RA ) D W T
132 133 134 135
1. Premises 2. Equipment 3. Personnel 4. Sanitation
C.02.00 4 C.02.00 5 C.02.00 6 C.02.00 7 C.02.00 8
U U U U U U U U U U U U U U U
U U U U U U U
U U U U
136
5. Raw Material Testing
C.02.00 9 C.02.01 0
U U U U U U U U U U U U U U U U U U U U U U U U U U U U U U U U U U
137
6. Manufacturing Control
C.02.01 1 C.02.01 2
X X X X X
138
7. Quality Control
C.02.01 3 C.02.01 4 C.02.01 5
139 140
8. Packaging Material Testing
C.02.01 6 C.02.01 7
141
9. Finished Product Testing
C.02.01 8 C.02.01 9
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 5
Health Canada / Health Products and Food Branch Inspectorate
142
10. Records
C.02.02 0 C.02.02 1 C.02.02 2 C.02.02 3 C.02.02 4
U U
U U
U U U
X X X X X X X X X
U U U U U U U U U U U U U
U U
U U U U
U U
U U U U U U
143
11. Samples
C.02.02 5 C.02.02 6
144
12. Stability
C.02.02 7 C.02.02 8
145 146 147
13. Sterile Products F =Fabricator P/L=Packager/Labeller T=Tester
C.02.02 9
U D=Distributor W=Wholesaler
I=Importer (MRA and non-MRA)
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 6
Health Canada / Health Products and Food Branch Inspectorate
148 149 150 151 152 153 154 155 156 157 158 159 160 161 162 163 164 165 166 167 168 169 170 171 172 173 174 175 176 177 178 179 180 181
4. QUALITY MANAGEMENT
4.1 GUIDING PRINCIPLE The holder of an establishment licence, or any operation to which the requirements of Division 2 Part C of the FDR are applicable, must ensure that the fabrication, packaging, labelling, distribution, testing and wholesaling of drugs comply with these requirements and of the marketing authorization, and do not place consumers at risk due to inadequate safety and quality. The attainment of this quality objective is the responsibility of senior management and requires the participation and commitment of personnel in many different departments and at all levels within the establishment and its suppliers. To achieve the objective reliably To ensure compliance, there must be a comprehensively designed and correctly implemented quality management system of quality assurance that incorporates Good Manufacturing Practices GMP and thus quality control. The system should be fully documented and its effectiveness monitored. All parts of the quality assurance management systems should be adequately resourced with qualified personnel, suitable premises, equipment, and facilities. There are additional legislative responsibilities for the holder of the establishment licence and for the person(s) authorized to market drug products. There are additional legislative responsibilities for the holder of the drug establishment licence and for the person(s) authorized to market drug products. The basic concepts of quality assurance, Good Manufacturing Pratices, and quality control, and product quality review are inter-related. They are described here in order to emphasize their relationships and their fundamental importance to the production and control of drugs. 4.2 RELATIONSHIP AMONG QUALITY ELEMENTS The basic concepts of quality assurance, Good Manufacturing Practices, and quality control are interrelated. They are described here in order to emphasize their relationships and their fundamental importance to the production and control of drugs. 4.2.1 QUALITY ASSURANCE Quality assurance is a wide-ranging concept that covers all matters that individually or collectively influence the quality of a drug. It is the total of the organized arrangements made with the objective of ensuring that drugs are of the quality required for their intended use. Quality assurance therefore incorporates Good Manufacturing Practices, along with other factors that are outside the scope of these guidelines. A system of quality assurance appropriate for the manufacture fabrication, packaging, labelling, testing, distribution, importation and wholesale of drugs should ensure that: 1. Drugs are designed and developed in a way that takes into account the GMP requirements;
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 7
Health Canada / Health Products and Food Branch Inspectorate
182 183 184 185 186 187 188 189 190 191 192 193 194 195 196 197 198 199 200 201 202 203 204 205 206 207 208 209 210 211 212 213 214
2. 3. 4.
Managerial responsibilities are clearly specified; Systems, facilities and procedures are adequate; Production and control operations are clearly specified and validated , and GMP are adopted; Arrangements are made for the supply and use of the correct raw and packaging materials; All necessary controls on intermediates, and any other in-process monitoring, and validation activities are is carried out; Outsourced activities are subject to appropriate oversight controls and meet GMP requirements; The finished product is processed, packaged/labelled, verified, and tested according to defined procedures; Fabrication, packaging/labelling, testing, distribution, importation, and wholesaling are performed in accordance with established procedures; Drugs are not sold or supplied before the quality control department has indicated certified that each batch lot has been produced and controlled in accordance with the requirements the marketing authorization and of any other regulations relevant to the production, control and release of drugs; Satisfactory arrangements exist for ensuring that the drugs are stored, distributed, and subsequently handled in such a way that quality is maintained throughout their shelf life;
5.
6.
7.
78.
89.
910.
1011. There is a procedure implemented for self-inspection and/or quality audit that regularly appraises the effectiveness and applicability of the quality assurance manamgement system; The effectiveness and applicability of the quality management system is ensured through regular self-inspection and management review; 12. An annual product quality review of all drugs should be conducted with the objective of verifying the consistency of the existing process, the appropriateness of current specifications for both raw materials and finished product to highlight any trends and to identify product and process improvements.
4.2.2 GOOD MANUFACTURING PRACTICES (GMP) FOR DRUGS Good Manufacturing Practices (GMP) are the part of quality assurance that ensures that drugs are consistently produced and controlled in such a way to meet the quality standards appropriate to their intended use, as required by the marketing authorization. GMP are concerned with both production and quality control. Their basic requirements are as
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 8
Health Canada / Health Products and Food Branch Inspectorate
215 216 217 218 219 220 221 222 223 224 225 226 227 228 229 230 231 232 233 234 235 236 237 238 239 240 241 242 243 244 245 246 247
follows: 1. Manufacturing processes are clearly defined and controlled. All critical processes are validated to ensure consistency and compliance with approved specifications. Manufacturing processes are controlled, and any changes to the process are evaluated. Changes that have an impact on the quality of the drug are validated as necessary. Critical steps of manufacturing processes and significant changes to the process are validated. All necessary key elements for GMP are provided, including the following: - qualified and trained personnel - adequate premises and space - suitable equipment and services - correct materials, containers and labels - approved procedures and instructions - suitable storage and transport 4. 5. 6. Instructions and procedures are written in clear and unambiguous language; Operators are trained to carry out and document procedures; Records are made, manually or by instruments, during manufacture that demonstrate that all the steps required by the defined procedures and instructions were in fact taken and that the quantity and quality of the drug was as expected. Deviations are investigated and documented; Records of manufacture (including) fabrication, packaging, labelling, testing, distribution, importation and wholesaling that enable the complete history of a batch lot to be traced are retained in a comprehensible and accessible form; The Control of storage, handling, and transportation distribution of the drugs minimizes any risk to their quality; A system is available for recalling any batch of drugs from sale or supply; Complaints about marketed drugs are examined, the causes of quality defects are investigated, and appropriate measures are taken with respect to the defective drugs and to prevent recurrence.
2.
3.
7.
8.
9. 10.
4.2.3 QUALITY CONTROL Quality control is the part of GMP that is concerned with sampling, specifications, testing, documentation, and release procedures. This approach Quality control ensures that materials are not released for use, and that drugs released for sale or supply, until their quality has been
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 9
Health Canada / Health Products and Food Branch Inspectorate
248 249 250 251 252 253 254 255 256 257 258 259 260 261 262 263 264 265 266 267 268 269 270 271 272 273 274 275 276 277 278 279 280 281
deemed satisfactory that the necessary and relevant tests are carried out and that raw materials, packaging materials, and products are released for use, sale or supply, only if their quality is satisfactory. Quality control is not confined to laboratory operations but must be incorporated into all activities and decisions concerning the quality of the product. The basic requirements of quality control are as follows: 1. Adequate facilities, trained personnel, and approved procedures are available for sampling, inspecting and testing of raw materials, packaging materials, intermediate bulk and finished products, and, where appropriate monitoring environmental conditions for GMP purposes; 1.1 Samples of raw materials, packaging materials, and intermediate, bulk, and finished products are taken according to procedures approved by the quality control department; Test methods are validated; Records are made that demonstrate that all the required sampling, inspecting, and testing procedures were actually carried out, and any deviations are recorded and investigated; The finished products contain active ingredients that (1) comply with the qualitative and quantitative composition requirements of the marketing authorization drug submission, (2) have the meet the purity required requirements, (3) are enclosed within their proper containers, and (4) are correctly labelled; Records are made of the results of self-inspection and management review, and to show that testing of materials, and of intermediate, bulk, and finished products is formally assessed against specifications; The procedures for product assessment release includes a review and evaluation of relevant production documentation and an assessment of deviations from specified procedures; No batch of drug is released for sale or supply prior to approval by the quality control department in accordance with the requirements of the marketing authorization; (Notice of Compliance (NOC), Drug Identification Number (DIN)); Sufficient reference samples of raw material and drugs are retained to permit future examination of the drug if necessary, and the drug is retained in its final package unless exceptionally large packages are produced.
1.2 1.3
1.4
1.54
1.65
1.76
1.87
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 10
Health Canada / Health Products and Food Branch Inspectorate
282 283 284 285 286 287 288 289 290 291 292 293 294 295 296 297 298
5. REGULATION
C.02.002 In this Division, "medical gas" means any gas or mixture of gases manufactured, sold, or represented for use as a drug; (gaz mdical) "packaging material" includes a label; (matriel d'emballage) "quality control department" means a quality control department referred to in section C.02.013; (service du contrle de la qualit) "specifications" means a detailed description of a drug, the raw material used in a drug, or the packaging material for a drug and includes: (a) a statement of all properties and qualities of the drug, raw material or packaging material that are relevant to the manufacture, packaging, and use of the drug, including the identity, potency, and purity of the drug, raw material, or packaging material, a detailed description of the methods used for testing and examining the drug, raw material, or packaging material, and a statement of tolerances for the properties and qualities of the drug, raw material, or packaging material. (spcifications)
(b)
(c)
299 300 301 302
SALE
C.02.003 No distributor referred to in paragraph C.01A.003(b) and no importer shall sell a drug unless it has been fabricated, packaged/labelled, tested, and stored in accordance with the requirements of this Division.
303 304 305 306 307 308
PREMISES
REGULATION C.02.004 The premises in which a lot or batch of a drug is fabricated, or packaged/labelled, or stored shall be designed, constructed and maintained in a manner that; (a) permits the operations therein to be performed under clean, sanitary and orderly conditions;
Page 11
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
309 310 311 312 313 314
(b) (c)
permits the effective cleaning of all surfaces therein; and prevents the contamination of the drug and the addition of extraneous material to the drug.
RATIONALE The pharmaceutical establishment should be designed and constructed in a manner such that it permits cleanliness and orderliness while preventing contamination. Regular maintenance is required to prevent deterioration of the premises. The ultimate objective of all endeavours is product quality.
315 316 317 318 319 320 321 322 323 324 325 326 327 328 329 330 331 332 333 334 335 336 337 338 339
INTERPRETATION 1. Buildings in which drugs are fabricated or packaged are located in an environment that, when considered together with measures being taken to protect the manufacturing processes, presents a minimum minimal risk of causing any contamination of materials or drugs. 2. The premises are designed, constructed, and maintained such that they prevent the entry of insects and other animals pests into the building and also prevent the migration of extraneous material from the outside into the building and from one area to another. 2.1 Doors, windows, walls, ceilings, and floors are such that no holes or cracks are evident (other than those intended by design). Doors giving direct access to the exterior from manufacturing and packaging areas are used for emergency purposes only. These doors are adequately sealed. Receiving and shipping area(s) do not allow direct access to production areas. Production areas are segregated from all non-production areas. Individual manufacturing, packaging, and testing areas are clearly defined and if necessary segregated. Areas where biological, microbiological or radioisotope testing is carried out require special design and containment considerations. Laboratory animals quarters are segregated. Engineering, boiler rooms, generators, etc. are isolated from production areas.
2.2
2.3
2.4 2.5
3. In all areas where raw materials, primary packaging materials, in-process drugs, or drugs are exposed, the following considerations apply to the extent necessary to prevent contamination. In laboratories these considerations apply only to the extent necessary to ensure the validity of test results. 3.1 Floors, walls, and ceilings permit cleaning. Brick, cement blocks, and other porous materials are sealed. Surface materials that shed particles are avoided. Floors, walls, ceilings, and other surfaces are hard, smooth and free of sharp corners where extraneous material can collect.
3.2
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 12
Health Canada / Health Products and Food Branch Inspectorate
340 341 342 343 344 345 346 347 348 349 350 351 352 353 354 355 356 357 358 359 360 361 362 363 364 365 366 367 368 369 370
3.3 3.4
Joints between walls, ceilings and floors are sealed. Pipes, light fittings, ventilation points and other services do not create surfaces that cannot be cleaned. Floor drains are screened and trapped. Air quality is maintained through dust control, monitoring of pressure differentials between production areas and periodic verification and replacement of air filters. The air handling system is well defined, taking into consideration airflow volume, direction, and velocity. Air handling systems are subject to periodic verification to ensure compliance with their design specifications. Records are kept. Clean areas are provided where susceptible products are fabricated and packaged.
3.5 3.6
3.7
4. Temperature and humidity are controlled, where required, in order to the extent necessary to safeguard sensitive materials (e.g. raw materials, drugs, samples, reference standards, etc.). 5. Rest, change, wash-up, and toilet facilities are well separated from production areas and are sufficiently spacious, well ventilated, and of a type that permits good sanitary practices. 6. Premises layout is designed to avoid mix-ups and generally optimize the flow of personnel and materials. 6.1 6.2 There is sufficient space for receiving and all production activities. Working spaces allow the orderly and logical placement of equipment (including parts and tools) and materials. Where physical quarantine areas are used, they are well marked, with access restricted to designated personnel. Where electronic quarantine is used, electronic access is restricted to designated personnel. A separate sampling area is provided for raw materials. If sampling is performed in the storage area, it is conducted in such a way as to prevent contamination or cross-contamination. Working areas are well lit.
6.3
6.4
6.5
7. Utilities and support systems (e.g., HVAC, dust collection, and supplies of purified water, steam, compressed air, nitrogen, etc.) for buildings in which drugs are fabricated or packaged/labelled are qualified and are subject to periodic verification. Further guidance is provided in Health Canadas document entitled Validation Guidelines for Pharmaceutical Dosage Forms (GUI-0029). 8. Outlets for liquids and gases used in the production of drugs are clearly identified as to their content. 9. Premises are maintained in a good state of repair. Repair and maintenance operations do not affect
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 13
Health Canada / Health Products and Food Branch Inspectorate
371 372 373 374 375 376 377 378 379 380 381 382 383 384 385 386 387 388 389 390 391 392 393 394 395 396 397 398 399 400 401 402 403 404 405
drug quality. 10. Where necessary, separate rooms are provided and maintained to protect analytical instruments sensitive equipment and associated control systems from vibration, electrical interference, and contact with excessive moisture or other external factors. 11. Prevention of cross-contamination during manufacturing is the responsibility of the fabricator and packager. They Fabricators and packagers must demonstrate that the premises are designed in such a manner that the risk of cross-contamination between products is minimized. 11.2 11.1 Campaign production can be accepted where, on a product by product basis, proper justification is provided, validation is conducted and rigorous validated controls and monitoring are in place and demonstrate the minimization of any risk of crosscontamination. In order to minimize the risk of a serious health hazard due to cross-contamination, additional controls, including the need for self-containment a dedicated self-contained facility should be considered must be used for each group of the following particular drugs, such as the following: -highly sensitizing drugs (e. g., penicillins) -biologicals potentially pathogenic drugs (e. g., live vaccines) -certain hormones (e. g., estrogen) -certain cytotoxic drugs -other highly active drugs 11.3 Additional controls, including segregation up to complete self-containment, should also be considered for particular drugs, such as the following: -certain hormones (e.g., estrogen) -other highly active drugs Factors to consider are the manufacturing processes, the use of closed systems, dedication of product contact equipment parts, HVAC controls, and engineering controls (such as fail-safe systems), coupled with validation and ongoing monitoring using highly sensitive analytical methods. A documented rationale should be available. 11.2 Self-contained facilities are required for certain classes of highly sensitizing drugs such as penicillins and cephalosporins. Self-contained facilities are also required for other classes of highly potent drugs such as potent steroids, cytotoxics, or potentially pathogenic drugs (e.g., live vaccines), for which validated cleaning or inactivation procedures cannot be established (e.g., the acceptable level of residue is below the limit of detection by the best available analytical methods).
11.1 11.2
11.3
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 14
Health Canada / Health Products and Food Branch Inspectorate
406 407 408 409 410 411 412 413 414
11.34 No production activities of highly toxic non-pharmaceutical materials, such as pesticides and herbicides, are conducted in premises used for the production of drugs. 11.45 Once the products are enclosed in their immediate final containers and controls are in place to eliminate risk of cross-contamination, co- mingle storage in a common warehouses is allowed. For the types of products listed in interpretations 11.2 and 11.3, external contamination with drug product residues of the final container and primary packaging does not exceed acceptable levels. Storage in common areas is allowed Oonce the products are enclosed in their immediate final containers and controls are in place to eliminate risks of cross-contamination.
415 416 417 418 419 420 421 422 423 424 425 426 427 428 429 430 431 432 433 434 435 436 437
EQUIPMENT
REGULATION C.02.005 The equipment with which a lot or batch of a drug is fabricated, packaged/labelled, or tested shall be designed, constructed, maintained, operated, and arranged in a manner that: (a) (b) (c) permits the effective cleaning of its surfaces; prevents the contamination of the drug and the addition of extraneous material to the drug; and permits it to function in accordance with its intended use.
RATIONALE The purpose of these requirements is to prevent the contamination of drugs by other drugs, by dust, and by foreign materials such as rust, lubricant and particles coming from the equipment. Contamination problems may arise from poor maintenance, the misuse of equipment, exceeding the capacity of the equipment and the use of worn-out equipment. Equipment arranged in an orderly manner permits cleaning of adjacent areas and does not interfere with other processing operations. It also minimizes the circulation of personnel and optimizes the flow of materials. The fabrication of drugs of consistent quality requires that equipment perform in accordance with its intended use. INTERPRETATION 1. The design, construction and location of equipment permit cleaning, sanitizing, and inspection of the equipment. 1.1 Equipment parts that come in contact with raw materials, in-process drugs or bulk drugs are accessible to cleaning or are removable. Tanks used in processing liquids and ointments are equipped with fittings that can be
Page 15
1.2
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
438 439 440 441 442 443 444 445 446 447 448 449 450 451 452 453 454 455 456 457 458 459 460 461 462 463 464 465 466 1.3 1.4
dismantled and cleaned. Validated Clean-In-Place (CIP) equipment can be dismantled for periodic verification. Filter assemblies are designed for easy dismantling. Equipment is located at a sufficient distance from other equipment and walls to permit cleaning of the equipment and adjacent area. The base of immovable equipment is adequately sealed along points of contact with the floor. Equipment is kept clean, dry and protected from contamination when stored.
1.5 1.6
2. Equipment does not add extraneous material to the drug. 2.1 Surfaces that come in contact with raw materials, in-process drugs or bulk drugs are smooth and are made of material that is non-toxic, corrosion resistant, non-reactive to the drug being fabricated or packaged and capable of withstanding repeated cleaning or sanitizing. The design is such that the possibility of a lubricant or other maintenance material contaminating the drug is minimized. Equipment made of material that is prone to shed particles or to harbour microorganisms does not come in contact with or contaminate raw materials, in-process drugs or bulk drugs. Chain drives and transmission gears are enclosed or properly covered. Tanks, hoppers and other similar fabricating equipment are equipped with covers.
2.2
2.3
2.4 2.5
3. Equipment is operated in a manner that prevents contamination. 3.1 Ovens, autoclaves and similar equipment contain only one raw material, in-process drug or bulk drug at a time, unless precautions are taken to prevent contamination and mix-ups. Equipment is not operated where contaminants may fall into the material. The location of equipment precludes contamination from extraneous materials. Equipment is placed in such a way to optimize The placement of equipment optimizes the flow of material and to minimizes the circulation of personnel. Equipment is located so that production operations undertaken in a common area are compatible and so that prevent cross-contamination between such operations is prevented. Fixed pipework is clearly labelled to indicate the contents and, where applicable, the direction of flow. Dedicated production equipment is provided where appropriate.
3.2
3.3
3.4
3.5
3.6
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 16
Health Canada / Health Products and Food Branch Inspectorate
467 468 469 470 471 472 473 474 475 476 477 478 479 480 481 482 483 484 485 486 487 488 489 490 491 492 493 494 495 496 497 498 499 500 501
3.7
Water purification, storage, and distribution equipment is operated in such a manner so as to that will ensure a reliable source of water of the appropriate chemical and microbial purity.
4. Equipment is maintained in a good state of repair when in use. 4.1 Where a potential for the contamination of the drug being fabricated or packaged during fabrication or packaging of a drug exists, surfaces are free from cracks, peeling paint and other defects. Gaskets are functional. The use of temporary devices such as (e.g. tape) is avoided. Equipment parts that come in contact with drugs are maintained in such a manner that drugs are fabricated or packaged within specifications. Critical Equipment used for significant processing or testing operations is maintained in accordance with a written preventative maintenance program. Maintenance records are kept.
4.2 4.3 4.4
5. Production Equipment is designed, located, and maintained to serve its intended purpose. 5.1 Scales Measuring devices and other measuring equipment are of an appropriate range, and precision and accuracy. are available for production and control operations. Such equipment is calibrated on a scheduled basis, and corresponding records are kept. Defective and unused Equipment that is unsuitable for its intended use is removed from production fabrication, packaging/labelling, and testing and quality control areas. or is at least clearly labelled as such. When removal is not feasible unsuitable equipment is clearly labelled as such. Equipment intended to be used during the critical steps of fabrication, packaging/labelling, and testing, including computerized systems, is subject to installation and operational qualification. Equipment qualification is documented. Further guidance is provided in Health Canadas document entitled Validation Guidelines for Pharmaceutical Dosage Forms (GUI0029) and PIC/S Annex 11: Computerized Systems. Automatic, mechanical, electronic, or other types of equipment including computerized systems that are used in the fabrication, packaging/labelling, and storing of a drug is routinely calibrated, inspected or checked according to a written program designed to assure proper performance. Written records of these calibration checks and inspections are maintained. Equipment used for significant processing or testing operations is calibrated, inspected or checked in accordance with a written program. Records are kept. For equipment used for significant processing or testing operations, usage logs are maintained. These logs should include identification of products, dates of operation, and equipment downtime due to malfunctions and breakdowns.downtime due to frequent or serious malfunctions or breakdowns. The information should be collected to facilitate the
Page 17
5.2
5.3
5.4
5.5
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
502 503 504 505 506 507 508 509 510 511 512 513 514 515 516 517 518 519 520 521 522 523 524 525 526 527 528 529 530 531 532 533 534
identification of negative performance trends.
PERSONNEL
REGULATION C.02.006 Every lot or batch of a drug shall be fabricated, packaged/labelled, tested, and stored under the supervision of personnel who, having regard to the duties and responsibilities involved have had such technical, academic, and other training as the Director considers satisfactory in the interests of the health of the consumer or purchaser. RATIONALE People are the most important element in any pharmaceutical operation, without the proper personnel with the right attitude and the right training, it is almost impossible to fabricate, package/label, test, or store good quality drugs. It is essential that qualified personnel be employed to supervise the fabrication of drugs. The operations involved in the fabrication of drugs are highly technical in nature and require constant vigilance, attention to details and a high degree of competence on the part of employees. Inadequate training of personnel or the absence of an appreciation of the importance of production control, often accounts for the failure of a product to meet the required standards. INTERPRETATION 1. For The individual in charge of the quality control department fabricators packagers/labellers and testers, of a fabricator, packager/labeller, tester, importer, and distributor; and the individuals individual in charge of the manufacturing department and the quality control department of a fabricator or packager/labeller; 1.1 holds a Canadian university degree or a degree recognized as equivalent by a Canadian university or Canadian accreditation body in a science related to the work being carried out; have has practical experience in their responsibility area; directly controls and personally supervises on site, each working shift during which activities under their control are being conducted for each working shift; and can may delegate their duties and responsibility (to cover all shifts) to a person in possession of a diploma, certificate or other evidence of formal qualifications awarded on completion of a course of study at a university, college or technical institute in a science related to the work being carried out combined with at least two years of relevant practical experience, while remaining accountable for those duties and responsibility.
Page 18
1.2 1.3
1.4
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
535 536 537 538 539 540 541 542 543 544 545 546 547 548 549 550 551 552 553 554 555 556 557 558 559 560 561 562 563 564
2. The individual in charge of the quality control department of a wholesaler; 2.1 2.2 is qualified by pertinent academic training and experience; and may delegate duties and responsibility to a person who meets the requirements defined under Regulation C.02.006 interpretation 2.1
3. For secondary labellers, individuals in charge of labelling operations and individuals in charge of the quality control department 3.1 3.2 are qualified by pertinent academic training and experience; and can delegate their duties and responsibilities to a person who meets the requirements defined under 3.1.
42. The Individuals individual responsible for packaging operations, including control over printed packaging materials and withdrawal of bulk drugs; 42.1 42. 2 are is qualified by training and experience; and are is directly responsible to the person in charge of the manufacturing department or a person having the same qualifications.
3. For distributors, importers, and wholesalers, individuals in charge of the quality control department; 3.1 3.2 are qualified by pertinent academic training and experience; and can delegate their duties and responsibilities to a person who meets the requirements defined under Regulation C.02.006 Interpretation 3.1.
45. An adequate number of personnel with the necessary qualifications and practical experience appropriate to their responsibilities are available on site. 45.1 The responsibilities placed on any one individual are not so extensive as to present any risk to quality. All responsible personnel have their specific duties recorded in a written description and have adequate authority to carry out their responsibilities. When key personnel are absent, qualified personnel are appointed to carry out their duties and functions.
45.2
45.3
56. All personnel are aware of the principles of GMP that affect them, and all personnel receive initial and continuing training relevant to their job responsibilities. 56.1 Training is provided by qualified personnel having regard to the function and in accordance with a written program for all personnel involved in the fabrication of a drug, including
Page 19
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
565 566 567 568 569 570 571 572 573 56.2 56.3 56.4 56.5
technical, maintenance, and cleaning personnel. The effectiveness of continuing training is periodically assessed. Training is provided prior to implementation of new or revised SOPs. Records of training are maintained. Personnel working in areas where highly active, toxic, infectious, or sensitizing materials are handled are given specific training. The performance of all personnel is periodically reviewed.
56.6
67. Consultants and contractors have the necessary qualifications, training, and experience to advise on the subjects for which they are retained.
574 575 576 577 578 579 580 581 582 583 584 585 586 587 588 589 590 591
SANITATION
REGULATION C.02.007 (1) Every person who fabricates or packages/labels a drug shall have a written sanitation program that shall be implemented under the supervision of qualified personnel. (2) The sanitation program referred to in subsection (1) shall include: (a) cleaning procedures for the premises where the drug is fabricated or packaged/labelled and for the equipment used in the fabrication or packaging/labelling of the drug; and instructions on the sanitary fabrication and packaging/labelling of drugs and the handling of materials used in the fabrication and packaging/labelling of drugs.
(b)
RATIONALE Sanitation in a pharmaceutical plant influences the quality of drug products as well as employee attitude. The quality requirement for drug products demand that such products be fabricated and packaged in areas that are free from environmental contamination and free from contamination by another drug. A written sanitation program provides some assurance that levels of cleanliness in the plant are maintained and that the provisions of Sections 8 and 11 of the Food and Drugs Act are satisfied. INTERPRETATION 1. A written sanitation program is available on the premises of every person who fabricates or
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002 Page 20
Health Canada / Health Products and Food Branch Inspectorate
592 593 594 595 596 597 598 599 600 601 602 603 604 605 606 607 608 609 610 611 612 613 614 615 616 617 618 619 620 621
packages/labels, a drug. 2. The sanitation program contains procedures that outline describe the following: 2.1 cleaning requirements applicable to all production areas of the plant with emphasis on manufacturing areas that require special attention; cleaning requirements applicable to processing equipment; cleaning intervals; products for cleaning and disinfection, along with their dilution and the equipment to be used; the responsibilities of any outside contractor; disposal procedures for waste material and debris; pest control measures; precautions required to prevent contamination of a drug when rodenticides, insecticides, and fumigation agents are used; microbial and environmental monitoring procedures with alert and action limits in areas where susceptible products are fabricated or packaged; and the personnel responsible for carrying out cleaning procedures.
2.2 2.3 2.4 2.5 2.6 2.7 2.8
2.9
2.10
3. The sanitation program is implemented and is effective in preventing unsanitary conditions. 3.1 Cleaning procedures for manufacturing equipment are validated based on the Health Canada document entitled Cleaning Validation Guidelines (GUI-0028). Residues from the cleaning process itself (e.g., detergents, solvents, etc.) are also removed from equipment; Evidence is available demonstrating that routine cleaning and storage does not allow microbial proliferation; Where necessary, sanitisers and disinfectants are filtered to remove spores (e.g. isopropyl alcohol). Analytical methods used to detect residues or contaminants are validated. Guidance on analytical method validation can be obtained from publications such as the International Conference on Harmonization (ICH) document entitled ICH Q2(R1): Validation of Analytical Procedures: Text and Methodology, or in any standard listed in Schedule B to the Food and Drugs Act. A cleaning procedure requiring complete product removal may not be necessary between batches of the same drug.
Page 21
3.2
3.3
3.4
3.5
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
622 623 624 625 626 627 628 629 630 631 632 633 634 635 636 637 638 639 640 641 642 643 644 645 646 647 648 649 650 651 652
4. Individuals who supervise the implementation of the sanitation program; 4.1 4.2 are qualified by training or experience; and are directly responsible to a person who has the qualifications described under Regulation C.02.006, interpretation 1.
5. Dusty operations are contained. The use of unit or portable dust collectors is avoided in fabrication areas especially in dispensing, unless the effectiveness of their exhaust filtration is demonstrated and the units are regularly maintained in accordance with written approved procedures. REGULATION C.02.008 (1) Every person who fabricates or packages/labels a drug shall have in writing, minimum requirements for the health and the hygienic behaviour and clothing of personnel to ensure the clean and sanitary fabrication and packaging/labelling of the drug. (2) No person shall have access to any area where a drug is exposed during its fabrication or packaging/labelling if the person (a) (b) is affected with or is a carrier of a disease in a communicable form, or has an open lesion on any exposed surface of the body
RATIONALE Employees health, behaviour, and clothing may contribute to the contamination of the product. Poor personal hygiene will nullify the best sanitation program and greatly increase the risk of product contamination. INTERPRETATION 1. Minimum health requirements are available in writing .and provide for the following: 1.1 Personnel who have access to any area where a drug is exposed during its fabrication or packaging/labelling must undergo health examinations prior to employment. Medical reexaminations, based on job requirements take place periodically. Note: A person who is a carrier of a disease in a communicable form should not have access to any area where a drug is exposed. The likelihood of disease transmission by means of a drug product would depend on the nature of the disease and the type of work the person carries out. Certain diseases could be transmitted through a drug product if proper hygiene procedures are not followed by an infected person handling the product. However, a person may also be a carrier of a communicable disease and not be aware
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002 Page 22
Health Canada / Health Products and Food Branch Inspectorate
653 654 655 656 657 658 659 660 661 662 663 664 665 666 667 668 669 670 671 672 673 674 675 676 677 678 679 680 681 682 683 684 685 686 687 1.2 1.2
of it. Therefore, in addition to strict personal hygiene procedures, systems should be in place to provide an effective barrier that would preclude contamination of the product. These procedures must be followed at all times by all personnel. Periodic eye examinations are required for personnel who conduct visual inspections. Employees are instructed to report to their supervisor any health conditions they have that could adversely affect drug products. Supervisory checks are conducted to prevent any person who has an apparent illness or open lesions that may adversely affect the quality of drugs from handling exposed raw materials, primary packaging materials, in-process drugs or finished products drugs until the condition is no longer judged to be a risk. When an employee has been absent from the workplace due to an illness that may adversely affect the quality of products, that employees health is assessed before he or she is allowed to return to the workplace. A procedure in place which describes the actions to be taken in the event that a person who has been handling exposed raw materials, primary packaging materials, in-process drugs or drugs is identified as having a communicable disease. of a positive diagnosis or a case suspected of being hazardous to consumers of the products are specified. Supervisory checks are conducted to prevent any person who has an apparent illness or open lesions that may adversely affect the quality of drugs from handling exposed raw materials, packaging materials, in-process drugs or finished products until the condition is no longer judged to be a risk.
Em ployees are instructe d to rep ort to th eir supervis or any health conditions th ey have that c ould adversely affect drug products.
1.3
1.43
1.54
1.5
1.6
1.62
Periodic eye examinations are required for personnel who conduct visual inspections.
2. The written hygiene program clearly defines clothing requirements and hygiene procedures for personnel and visitors. 2.1 Where a potential for the contamination of a raw material, in-process material or bulk drug exists, individuals wear clean clothing and protective covering. Direct skin contact is avoided between the operator's hands and raw materials, primary packaging materials, and intermediate in-process drugs or bulk drugs. Unsanitary practices such as smoking, eating, drinking, chewing, and keeping plants, food, drink, smoking material and personal medicines are not permitted in fabrication, packaging/labelling, and storage areas production areas or in any other areas where they might adversely influence affect product quality. Requirements concerning personal hygiene, with an emphasis on hand hygiene, are outlined
Page 23
2.2
2.3
2.4
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
688 689 690 691 692 693 694 695 696 2.5
and are followed by employees. Requirements concerning cosmetics and jewelry jewellery worn by employees are outlined and are observed by employees. Soiled protective garments, if reusable, are stored in separate containers until properly laundered and, if necessary, disinfected or sterilized. A formalized procedure for the washing of protective garments under the control of the company is in place. Washing garments in a domestic setting is unacceptable. Personal hygiene procedures including the use of protective clothing, apply to all persons entering production areas.
2.6
2.7
697 698 699 700 701 702 703 704 705 706 707 708 709 710 711 712 713 714 715 716 717
RAW MATERIAL TESTING
REGULATION C.02.009 (1) Each lot or batch of raw material shall be tested against the specifications for the raw material prior to its use in the production of a drug. (2) No lot or batch of raw material shall be used in the fabrication production of a drug unless that lot or batch of raw material complies with the specifications for that raw material. (3) Notwithstanding subsection (1), water may, prior to the completion of its tests under that subsection, be used in the fabrication production of a drug. (4) Where any property of a raw material is subject to change on storage, no lot or batch of that raw material shall be used in the fabrication production of a drug after its storage unless the raw material is retested after an appropriate interval and complies with its specifications for that property. (5) Where the specifications referred to in subsections (1), (2) and (4) are not prescribed, they shall (a) (b) be in writing; be acceptable to the Director, who shall take into account the specifications contained in any publication mentioned in Schedule B to the Act; and be approved by the person in charge of the quality control department.
RATIONALE The testing of raw materials before their use has three objectives: to confirm the identity of the raw materials, to provide assurance that the quality of the drug in dosage form will not be altered by raw material defects, and to obtain assurance that the raw materials have the characteristics that will provide
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002 Page 24
Health Canada / Health Products and Food Branch Inspectorate
718 719 720 721 722 723 724 725 726 727 728 729 730 731 732 733 734 735 736 737 738 739 740 741 742 743 744 745 746 747 748 749 750 751 752
the desired quantity or yield in a given manufacturing process. INTERPRETATION 1. Each raw material used in the production of a drug is covered by specifications (see regulation C.02.002) that are approved and dated by the person in charge of the quality control department or by a designated alternate who meets the requirements described under Regulation C.02.006, Interpretation 1.4. 2. Specifications are of pharmacopoeial or equivalent status and are in compliance with the current marketing authorization. Where appropriate, additional properties or qualities not addressed by the pharmacopoeia (e.g., particle size, etc.) are included in the specifications. 3. Where a recognized pharmacopoeia (Schedule B of the Food and Drugs Act) contains a specification for microbial content, that requirement is included. 4. Purified water that meets any standard listed in Schedule B of the Food and Drugs Act is used in the formulation of a non-parenteral non-sterile drug product, unless otherwise required in one of these standards or as stated in the marketing authorization. 4.1 Specifications should include requirements for total microbial count, which should not exceed 100 cfu/ml. Purified water used for oral preparations should be tested for the absence of Escherichia coli and Salmonella. Purified water used for topical preparations should be tested for the absence of Staphylococcus aureus and Pseudomonas aeruginosa.
4.2
4.3
5. Test methods are validated, and the results of such validation studies are documented. Full validation is not required for methods included in any standard listed in Schedule B to the Food and Drugs Act, but the user of such a method establishes its suitability under actual conditions of use. Method transfer studies are conducted when applicable. Note: Guidance for the validation of particular types of methods can be obtained in publications such as the International Conference on Harmonization (ICH) guidelines titled document entitled ICH Q2(R1): Validation of Analytical Procedures: Text and Methodology or in any standard listed in Schedule B to the Food and Drugs Act. 6. A sample of each lot of raw material is fully tested against specifications. Sampling is conducted according to a suitable statistically valid plan. 6.1 In addition, each container of a lot of an active pharmaceutical ingredient (API) a raw material is tested for the identity of its contents using a specifically discriminating identity test. In lieu of testing each container for identity, testing a composite sample derived from sampling each container is acceptable, as long as the following conditions are met:
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002 Page 25
Health Canada / Health Products and Food Branch Inspectorate
753 754 755 756 757 758 759 760 761 762 763 764 765 766 767 768 769 770 771 772 773 774 775 776 777 778 779 780 781 782 783 784 785 786 787 788 6.3 6.2
6.1.1
the number of individual containers for each composite sample does not exceed 10; and a potency test is performed on each composite sample to establish the mass balance of the composite sample.
6.1.2
APIs originating from a dedicated facility that fabricates only one ingredient are exempted from the requirements outlined under Interpretation 6.1, provided that no re-packaging or relabelling has taken place. In lieu of testing each container for identity, testing only a proportion of the containers is acceptable where a validated procedure has been established to ensure that no single container of raw material has been incorrectly labelled. 6.2.1 Interpretation 6.2 applies to raw material coming from a single product manufacturer or plant or coming directly from a manufacturer or in the manufacturers sealed container where there is a history of reliability and regular audits of the manufacturers Quality Assurance system are conducted by or on behalf of the purchaser (drug fabricator). Interpretation 6.2 does not apply when the raw material is supplied by intermediaries such as brokers where the source of manufacture is unknown or not audited. The validation should take into account at least the following aspects; 6.2.3.1 the nature and status of the manufacturer and the supplier and their understanding of the GMP requirements of the Pharmaceutical Industry; 6.2.3.2 the Quality Assurance system of the manufacturer of the raw material; 6.2.3.3 the manufacturing conditions under which the raw material is produced and controlled; Where a batch of any raw material, after leaving the site of its fabrication is handled in any substantial way (e.g., repackaged by a third party) prior to its receipt on the premises of the person who formulates the raw material into dosage forms, each container in that batch is sampled and its contents positively identified.
6.2
6.2.2
6.2.3
7. Only raw materials that have been released by the quality control department and that are not past their established re-test date or expiry date are used in fabrication. If any API raw material is held in storage after the established re-test date, that API raw material is quarantined, evaluated, and tested prior to use. The re-test date or expiry date is based on acceptable s tability data developed under predefined storage conditions or on any other acceptable evidence. A batch of raw material can be re-tested and used immediately (i.e., within 30 days) after the re-test as long as it continues to comply with the specifications and has not exceeded its expiry date. A raw material held in storage after the established expiry date should not be used in fabrication. In
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002 Page 26
Health Canada / Health Products and Food Branch Inspectorate
789 790 791 792 793 794 795 796 797 798 799 800 801 802 803 804 805 806 807 808 809 810 811 812 813 814 815 816 817 818 819 820
exceptional circumstances, a batch of raw material can be re-tested and used immediately ( i.e., within 30 days) with suitable justification. 97.2 Any inactive raw material that is subject to chemical, microbiological, or physical changes is quarantined, evaluated and tested prior to use if the material has passed the expiration date as determined by the stability data or by any other documented evidence.
10.7.4 For most biotechnological/biological substances and certain antibiotics known to be labile, a shelf life is established rather than a re-test date. REGULATION C.02.010 (1) The testing referred to in section C.02.009 shall be performed on a sample taken (a) (b) after receipt of each lot or batch of raw material on the premises of the fabricator; or subject to subsection (2), before receipt of each lot or batch of raw material on the premises of the fabricator, if (I) the fabricator (A) has evidence satisfactory to the Director to demonstrate that raw materials sold to him by the vendor of that lot or batch of raw material are consistently manufactured in accordance with and consistently comply with the specifications for those raw materials, and undertakes periodic complete confirmatory testing with a frequency satisfactory to the Director and
(B)
(ii)
the raw material has not been transported or stored under conditions that may affect its compliance with the specifications for that raw material.
(2) After a lot or batch of raw material is received on the premises of the fabricator, the lot or batch of raw material shall be tested for identity. RATIONALE Section C.02.010 outlines options as to when the testing prescribed by Section C.02.009 is carried out. The purchase of raw materials is an important operation that requires a particular and thorough knowledge of the raw materials and their fabricator. To maintain consistency in the fabrication of drug products, raw materials should originate from reliable fabricators. INTERPRETATION 1. Testing other than identity testing:
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 27
Health Canada / Health Products and Food Branch Inspectorate
821 822 823 824 825 826 827 828 829 830 831 832 833 834 835 836 837 838 839 840 841 842 843 844 845 846 847 848 849 850 851 852 853 854 855
The testing is performed on a sample taken after receipt of the raw material on the premises of the person who formulates the raw material into dosage form, unless the vendor is certified. A raw material vendor certification program, if employed, is documented in a standard operating procedure. At a minimum, such a program includes the following: 1.1 A written contract agreement outlining the specific responsibilities of each party involved. The contract agreement specifies: 1.1.1 the content and the format of the certificate of analysis, which exhibits actual numerical results and makes reference to the raw material specifications and validated test methods used; that the raw material vendor must inform the drug fabricator of any changes in the processing or specifications of the raw material and; that the raw material vendor must inform the drug fabricator in case of any critical deviation during the manufacturing of a particular batch of a raw material.
1.1.2
1.1.3
1.2
An audit report is issued available: 1.2.1 For medicinal ingredients, the audit report is issued by a qualified regulatory authority demonstrating that the active pharmaceutical ingredient (API) fabricator vendor complies with the ICH Good Manufacturing Practice guide for API ICH document entitled ICH Q7: Good Manufacturing Practices Guide for Active Pharmaceutical Ingredients or with any standard or system of equivalent quality. This report should be less than 3 years old, but is valid for 4 years from the date of the inspection. If such an audit report is unavailable or is more than 4 years old, an on-site audit of the API fabricator vendor, against the same standard or its equivalent, by a person who meets the requirements of Interpretation 1 under Section C.02.006, is acceptable. For other raw materials, an audit report issued by a person who meets the requirements of interpretation 1 under section C.02.006 is acceptable.
1.2.2
1.3
Complete confirmatory testing is performed on the first three lots of any each raw material received from a new vendor. For APIs, a copy of the results of the impurity and residual solvent profile is also obtained. 1.3.1 Where the manufacturing process for an API has been modified, a new profile for impurity and residual solvents is obtained from the vendor.
1.4
Identification of how re-testing failures and any subsequent re-qualification of the vendor are to be addressed. The list of raw materials not subject to the reduced testing program (e.g. reprocessed lots). Complete confirmatory testing is conducted on a minimum of one lot per year of any a raw material received from each vendor, with the raw material being selected on a rotational basis.
1.5 1.6
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 28
Health Canada / Health Products and Food Branch Inspectorate
856 857 858 859 860 861 862 863 864 865 866 867 868 869 870 871 872 873 874 875 876 877 878 879 880 881 882 883 884 885 886 887 888 889 5.7. 1.7
1.6.1
In addition, where multiple raw materials are received from the same vendor, confirmatory testing is carried out for each raw material at least once every five years.
A document is issued for each vendor verifying that the vendor meets the criteria for certification. The document is approved by the quality control department and is updated at an appropriate frequency. Generally, due to the nature of its operations, a broker or wholesaler of raw materials cannot be directly certified. However, when a broker or wholesaler supplies materials received from the original vendor without changing the existing labels, packaging, certificate of analysis, and general information, then certification of the original source is still acceptable.
1.8
2. Identity testing: Specific identity testing is conducted on all lots of any raw material received on the premises of the person who formulates the raw material into dosage forms. This identity testing is performed in accordance with Regulation C.02.009, Interpretation 6. 3. Generally, due to the nature of its operations, a broker or wholesaler of raw materials cannot be directly certified. However, when the broker or wholesaler supplies materials received from the original vendor without changing the existing labels, packaging, certificate of analysis, and general information, then certification of the original source is still acceptable. 3.4. Provided that the identity test referred to in Interpretation 2 is performed, a the lot or batch of raw material selected for confirmatory testing may be used in fabrication prior to completion of all tests with the approval of the quality control department. Conditions of transportation and storage are such that they prevent alterations to the potency, purity, or physical characteristics of the raw material. In order to demonstrate that these conditions have been met, standard operating procedures and records for shipping and receiving are available and contain 45.1 45.2 the type of immediate contact and protective packaging for the raw material; the labelling requirements including storage conditions and special precautions or warnings, for the packaged raw material; the mode(s) of transportation approved for shipping the packaged raw material; a description of how the packaged raw material is sealed; the verification required to ensure that each package has not been tampered with and that there are no damaged containers; and evidence that special shipping requirements (e.g., refrigeration) have been met if required. If a delivery or shipment of raw material is made up of different batches, each batch is considered as separate for the purposes of sampling, testing, and release.
Page 29
4.5.
45.3 45.4 45.5
45.6
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
890 891 892 893 894 895 896 897 898
6.8.
If the same batch of raw material is subsequently received, this batch is also considered as separate for the purpose of sampling, testing, and release. However, full testing to specifications may not be necessary on such a batch provided that all the following conditions are met: 6.8. 1 a specifically discriminating identity test is conducted; 6.8. 2 the raw material has not been repackaged or re-labelled; 6.8. 3 the raw material is within the re-test date assigned by its vendor; and 6.8. 4 evidence is available to demonstrate that all pre-established transportation and storage conditions have been maintained.
899 900 901 902 903 904 905 906 907 908 909 910 911 912 913 914 915 916 917 918 919 920 921
MANUFACTURING CONTROL
REGULATION C.02.011 (1) Every fabricator, packager/labeller, distributor referred to in paragraph C.01A.003(b) and importer of a drug shall have written procedures, prepared by qualified personnel, in respect of the drug to ensure that the drug meets the specifications for use of that drug. (2) Every person required to have written procedures referred to in subsection (1) shall ensure that each lot or batch of the drug is fabricated, packaged/labelled and tested in compliance with those procedures. RATIONALE This Regulation requires that a number of measures be taken to maintain the integrity of a drug product from the moment the various raw materials enter the plant where the first stages of the manufacturing process start to the time the finished dosage form is released for sale and distributed. These measures seek to ensure that all manufacturing processes are clearly defined, systematically reviewed in light of experience, and shown demonstrated to be capable of consistently manufacturing pharmaceutical products of the required quality that comply with their established specifications. INTERPRETATION 1. All handling of raw materials and, products, and packaging materials such as receipt, quarantine, sampling, storage, tracking, labelling, dispensing, processing, packaging and distribution is done in accordance with pre-approved written procedures or instructions and recorded. 2. All critical production processes are validated. Detailed information is provided in various Health Canadas V validation G guidelines for pharmaceutical dosage forms.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002 Page 30
Health Canada / Health Products and Food Branch Inspectorate
922 923 924 925 926 927 928 929 930 931 932 933 934 935 936 937 938 939 940 941 942 943 944 945 946 947 948 949 950 951 952 953 954 955
3. Validation studies are conducted in accordance with predefined protocols. A written report summarizing recorded results and conclusions is prepared, evaluated, approved, and maintained. 4. Changes to production processes, systems, equipment, or materials that may affect product quality and/or process reproducibility are validated prior to implementation. 5. Any deviation from instructions or procedures is avoided. If deviations occur, qualified personnel investigate, and write a report that describes the deviation, the investigation, the rationale for disposition, and any follow-up activities required. The report is approved by the quality control department and records maintained. 6. Checks on yields and reconciliation of quantities are carried out at appropriate stages of the process to ensure that yields are within acceptable limits. 7. Deviations from the expected yield are recorded and investigated. 8. Access to production premises is restricted to designated personnel. 9. Provided that validated changeover procedures are validated and implemented, non-medicinal products drugs may be fabricated or packaged/labelled in areas or with equipment that is also used for the production of pharmaceutical products. 10. Before any processing operation is started, steps are taken and documented to ensure that the work area and equipment are clean and free from any raw materials, products, product residues, labels, or documents not required for the current operation. 10.1 Operations on different products should not be carried out simultaneously or consecutively in the same room unless there is no risk of mix-up or cross-contamination. Checks should be carried out to ensure that transfer lines and other pieces of equipment used for the transfer of products from one area to another are correctly connected. At every stage of processing, products and materials should be protected from microbial and other contamination. In-process control activities that are performed within the production areas do not pose any risk to the quality of the product. Measuring devices are regularly checked for accuracy and precision, and records of such checks are maintained. At all times during processing, all materials, bulk containers, major items of equipment and the rooms used are labelled or otherwise identified with an indication of the product or material being processed, its strength, and the batch number and, if appropriate, the stage of manufacturing. Rejected materials and products are clearly marked as such and are either stored separately in restricted areas or controlled by a system that ensures that they are either returned to their
Page 31
10.2
1011.
1112.
1213.
1314.
1415.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
956 957 958 959 960 961 962 963 964 965 966 967 968 969 970 971 972 973 974 975 976 977 978 979 980 981 982 983 984 985 986 987
vendors or, where appropriate, reprocessed or destroyed. Actions taken are recorded. 15. Equipment is located so that production operations undertaken in a common area are compatible. 16. Upon receipt, raw materials, packaging materials, in-process (intermediate) drugs, and bulk drugs, are accounted for, documented, labelled and held in quarantine until released by the quality control department. 17. Procedures are in place to ensure the identity of the contents of each container. Containers from which samples have been drawn are identified. 18. For each consignment, all containers are checked for integrity of package and seal and to verify that the information on the order, the delivery note and the vendor's labels is in agreement. 19. Damage to containers, along with any other problem that might adversely affect the quality of a material, is recorded, reported to the quality control department, and investigated. 20. Upon receipt, containers are cleaned where necessary and labelled with the prescribed data. 21. Labels for bulk drugs, in-process drugs, raw materials, and packaging materials bear the following information: 21.1 the designated name and, if applicable, the code or reference number of the material and a code reference where applicable; the specific batch number(s) given by the vendor and on receipt by the fabricator or packager/labeller; the status of the contents (e.g., in quarantine, on test, released, rejected, to be returned or recalled) appears on the label when a manual system is used; an expiry date or a date beyond which re-testing is necessary. the stage of manufacturing of in-process material, if applicable.
21.2
21.3
21.4 21.5
Note: When fully computerized storage systems are used, backup systems are available in case of system failure to satisfy the requirements of Interpretation 21. 22. Raw materials are dispensed and verified by qualified personnel, following a written procedure, to ensure that the correct materials are accurately weighed or measured into clean and properly labelled containers. Raw materials which are being staged are properly sealed and stored under conditions consistent with the accepted storage conditions for that material. MANUFACTURING MASTER FORMULA 23. Processing operations are covered by master formulae, that are prepared by, and are subject to independent checks by, persons who have the qualifications described under Regulation C.02.006 Interpretation 1, including the quality control department.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002 Page 32
Health Canada / Health Products and Food Branch Inspectorate
988 989 990 991 992 993 994 995 996 997 998 999 1000 1001 1002 1003 1004 1005 1006 1007 1008 1009 1010 1011 1012 1013 1014 1015 1016 1017 1018 1019 1020
24. Master formulae are written to provide not less than 100% of label claim. Overages may be allowed to compensate for processing losses with documented justification and approval if appropriate. In exceptional instances, overages to compensate for losses due to degradation during manufacturing or shelf-life must be scientifically justified and in accordance with the marketing authorization. Master formula also include the following: 24.1 24.2 24.3 the name of the product, with a reference code relating to its specifications; a description of the dosage form, strength of the product, and batch size; a list of all raw materials to be used, along with the amount of each, described using the designated name and a reference that is unique to that material (mention is made of any processing aids that may not be present in the final product); a statement of the expected final yield, along with the acceptable limits, and of relevant intermediate yields, where applicable; a statement and general description Identification of the principal equipment to be used, and if applicable internal codes or other identification; the procedures, or reference to the procedures, to be used for preparing the critical equipment, (e.g., cleaning (especially after a change in product), assembling, calibrating, sterilizing, etc.); detailed stepwise processing instructions (e.g., checks on materials, pretreatment, sequence for adding materials, mixing times or temperatures, etc.); the instructions for any in-process controls, along with their limits; where necessary, the requirements for storage of the products and in-process materials, including the container -closure system, the labelling and any special storage conditions, maximum validated hold time and any special precautions to be observed;
24.4
24.5
24.6
24.7
24.8 24.9
24.10 any special precautions to be observed. PACKAGING MASTER FORMULA 25. In the case of a packaged product, the master formula also includes for each product, package size and type, the following: 25.1 the package size, expressed in terms of the number, weight, or volume of the product in the final container; a complete list of all the packaging materials required for a standard batch size, including quantities, sizes and types with the code or reference number relating to the specifications for each packaging material; where appropriate, an example or reproduction of the relevant printed packaging materials and specimens, indicating where the batch number and expiry date of the product are to be
Page 33
25.2
25.3
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1021 1022 1023 1024 1025 1026 1027 1028 1029 1030 1031 1032 1033 1034 1035 1036 1037 1038 1039 1040 1041 1042 1043 1044 1045 1046 1047 1048 1049 1050 1051 25.4
positioned; special precautions to be observed, including a careful examination of the packaging area and equipment in order to ascertain the line clearance before operations begin. These verifications are recorded; a description of the packaging operations, including any significant subsidiary operations and the equipment to be used; and details of in-process controls, with instructions for sampling and acceptance limits.
25.5
25.6
MANUFACTURING OPERATIONS BATCH DOCUMENT 26. Each batch processed is effectively governed by an individually numbered manufacturing order prepared by qualified personnel from the master formula by such means as to prevent errors in copying or calculation and verified by qualified personnel. 27. As it becomes available during the process, the following information is included on or with the manufacturing order manufacturing batch record: 27.1 27.2 27.3 the name of the product; the number of the batch being manufactured; dates and times of commencement and completion of significant intermediate stages, such as blending, heating, etc., and of production; the batch number and/or analytical control number, as well as the quantity of each raw material actually weighed and dispensed (for active raw material, the quantity is to be adjusted if the assay value is less than 98% calculated on as is basis and on which the master formula was based); confirmation by qualified personnel of each ingredient added to a batch; the identification of personnel performing each step of the process; and of the person who checked each of these steps; the actual results of the in-process quality checks performed at appropriate stages of the process and the identification of the person carrying them out; the actual yield of the batch at appropriate stages of processing and the actual final yields, together with explanations for any deviations from the expected yield; detailed notes on special problems with written approval for any deviation from the master formula; and
27.4
27.5 27.6
27.7
27.8
27.9
27.10 after completion, the signature of the person responsible for the processing operations.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 34
Health Canada / Health Products and Food Branch Inspectorate
1052 1053 1054 1055 1056 1057 1058 1059 1060 1061 1062 1063 1064 1065 1066 1067 1068 1069 1070 1071 1072 1073 1074 1075 1076 1077 1078 1079 1080 1081 1082 1083
28. Batches are combined only with the approval of the quality control department and according to preestablished written procedures. 28.1 The introduction of part of a previous batch, conforming to the required quality, into the next batch of the same product at a defined stage of fabrication is approved beforehand. This recovery is carried out in accordance with a validated procedure and is recorded.
PACKAGING OPERATIONS BATCH DOCUMENT 29. Packaging operations are performed according to comprehensive and detailed written operating procedures or specifications, which include the identification of equipment and packaging lines used to package the drug, the adequate separation and if necessary, the dedication of packaging lines that are packaging different drugs and disposal procedures for unused printed packaging materials. Packaging orders are individually numbered. 30. The method of preparing packaging orders is designed to avoid transcription errors. 31. Before any packaging operation begins, checks are made that the equipment and work station are clear of previous products, documents, and materials that are not required for the planned packaging operations and that equipment is clean and suitable for use. These checks are recorded. 32. All products and packaging materials to be used are checked on receipt by the packaging department for quantity, identity and conformity with the packaging instructions. 33. Precautions are taken to ensure that containers to be filled are free from contamination with extraneous material. 34. The name and batch number of the product being handled is displayed at each packaging station or line. 35. Packaging orders include the following information (recorded at the time each action is taken): 35.1 35.2 the date(s) and time(s) of the packaging operations; the name of the product, the batch number, packaging line used, and the quantity of bulk product to be packaged, as well as the batch number and the planned quantity of finished product that will be obtained, the quantity actually obtained and the reconciliation; the identification of the personnel who are supervising packaging operations and the withdrawal of bulks; the identification of the operators of the different significant steps; the checks made for identity and conformity with the packaging instructions, including the results of in-process controls; the general appearance of the packages;
35.3
35.4 35.5
35.6
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 35
Health Canada / Health Products and Food Branch Inspectorate
1084 1085 1086 1087 1088 1089 1090 1091 1092 1093 1094 1095 1096 1097 1098 1099 1100 1101 1102 1103 1104 1105 1106 1107 1108 1109 1110 1111 1112 1113 1114
35.7 35.8 35.9
whether the packages are complete; whether the correct products and packaging materials are used; whether any on-line printing is correct;
35.10 the correct functioning of line monitors; 35.11 handling precautions applied to a partly packaged product; 35.12 notes on any special problems, including details of any deviation from the packaging instructions with written approval by qualified personnel; 35.13 the quantity, lot number, and/or analytical control number of each packaging material and bulk drug issued for use; and 35.14 a reconciliation of the quantity of printed packaging material and bulk drug used, destroyed or returned to stock. 36. To prevent mix-ups, samples taken away from the packaging line are not returned. 37. Whenever possible, samples of the printed packaging materials used, including specimens bearing the batch number, expiry date, and any additional overprinting, are attached to packaging orders. 38. Filling and sealing are followed as quickly as possible by labelling. If labelling is delayed, procedures are applied to ensure that no mix-ups or mislabeling can occur. 39. Upon completion of the packaging operation, any unused batch-coded packaging materials are destroyed, and their destruction is recorded. A procedure is followed if non-coded printed materials are returned to stock. 40. Outdated or obsolete packaging materials are destroyed and their disposal is recorded. 41. Products that have been involved in non-standard occurrences during packaging are subject to inspection and investigation by qualified personnel. A detailed record is kept of this operation. 42. Any significant or unusual discrepancy observed during reconciliation of the amount of bulk product and printed packaging materials and the number of units packaged is investigated and satisfactorily accounted for before release. Validated electronic verification of all printed packaging materials on the packaging line may obviate the need for their full reconciliation. 43. Printed packaging materials are 43.1 stored in an area to which access is restricted to designated personnel who are supervised by persons who have the qualifications outlined under Regulation C.02.006 Interpretation 2 3; withdrawn against a packaging order; issued and checked by persons who have the qualifications outlined under Regulation
Page 36
43.2 43.3
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1115 1116 1117 1118 1119 1120 1121 1122 1123 1124 1125 1126 1127 1128 1129 1130 1131 1132 1133 1134 1135 1136 1137 1138 1139 1140 1141 1142 1143 1144 1145 1146 43.4
C.02.006 Interpretation 24; and identified in such a way as to be distinguishable during the packaging operations.
44. To prevent mix-ups, roll-fed labels are preferred to cut labels. Gang printing (printing more than one item of labelling on a sheet of material) is avoided. 45. Cut labels, cartons, and other loose printed materials are stored and transported in separate closed containers. 46. Special care is taken when cut labels are used, when overprinting is carried out off-line and in handpackaging operations. On line verification of all labels by automated electronic means can be helpful in preventing mix-ups. Checks are made to ensure that any electronic code readers, label counters or similar devices are operating correctly. 47. The correct performance of any printing (e.g., of code numbers or expiry dates) done separately or in the course of the packaging is checked and recorded. 48. Raw materials, packaging materials, intermediates, bulk drugs and finished products are (a) stored in locations that are separate and removed from immediate manufacturing areas, and (b) transported under conditions designated by the quality control department to preserve their quality and safety. 49. All intermediate and finished products are held in quarantine and are so identified in accordance with Interpretation 21, until released by the quality control department. 50. Every package of a drug is identified by a lot number. ANNUAL PRODUCT QUALITY REVIEW 51. Regular periodic or rolling quality reviews of all drugs, should be conducted with the objective of verifying the consistency of the existing process, the appropriateness of current specifications for both raw materials and finished product to highlight any trends and to identify product and process improvements. Such reviews should normally be conducted and documented annually, taking into account previous reviews, and should include at least: 51.1 51.2 A review of critical in-process controls and finished product testing results. A review of all batches that failed to meet established specification(s) and their investigation. A review of all significant deviations or non-conformances, their related investigations, and the effectiveness of resultant corrective and preventative actions taken. A review of all changes carried out to the processes or analytical methods. A review of the results of the continuing stability program and any adverse trends. A review of all quality-related returns, complaints and recalls and the investigations performed
Page 37
51.3
51.4 51.5 51.6
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1147 1148 1149 1150 1151 1152 1153 1154 1155 1156 1157 1158 1159 1160 1161 1162 1163 1164 1165 1166 1167 1168 1169 1170 1171 1172 1173 1174 1175 1176 1177 1178 1179 1180 51.7 51.8
at the time. A review of adequacy of any other previous product process or equipment corrective actions. The qualification status of relevant equipment and utilities (e.g. HVAC, water, compressed gases, etc.); and A review of agreements to ensure that they are up to date.
51.9
52. The fabricator and marketing authorization holder, where different, should evaluate the results of this review and an assessment should be made whether corrective and preventative action or any revalidation should be undertaken. Reasons for such corrective actions should be documented. Agreed corrective and preventative actions should be completed in a timely and effective manner. There should be procedures for the ongoing management and review of these actions and the effectiveness of these procedures verified during self- inspection. 53. Quality reviews may be grouped by product type (e.g., solid dosage forms, liquid dosage forms, sterile products, etc. where scientifically justified.) 54. Where the marketing authorization holder is not the fabricator, there should be an agreement in place between the various parties that defines their respective responsibilities in producing the quality review. The quality control department of the importer or distributor should ensure that the quality review is performed in a timely manner and is accurate. REGULATION C.02.012 (1) Every fabricator, packager/labeller or distributor referred to in section C.01A.003, importer, and wholesaler of a drug shall maintain (a) a system of control that permits complete and rapid recall of any lot or batch of the drug that is on the market; and a program of self-inspection.
(b)
(2) Every fabricator and packager/labeller and subject to subsections (3) and (4), every distributor referred to in section C.01A.003(b) and importer of a drug shall maintain a system designed to ensure that any lot or batch of the drug fabricated and packaged/labelled on premises other than their own is fabricated and packaged/labelled in accordance with the requirements of this Division. (3) The distributor referred to in paragraph C.01A.003(b) of a drug that is fabricated, packaged/labelled, and tested in Canada by a person who holds an establishment licence that authorizes those activities is not required to comply with the requirements of subsection (2) in respect of that drug. (4) If a drug is fabricated or packaged/labelled in an MRA country at a recognized building, the distributor referred to in paragraph C.01A.003(b) or importer of the drug is not required to comply with the requirements of subsection (2) in respect of that activity for that drug if
Page 38
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1181 1182 1183 1184 1185 1186 1187 1188 1189 1190 1191 1192 1193 1194 1195 1196 1197 1198 1199 1200 1201 1202 1203 1204 1205 1206 1207 1208 1209 1210 1211 1212 1213
(a) the address of the building is set out in that persons establishment licence; and (b) that person retains a copy of the batch certificate for each lot or batch of the drug received by that person. RATIONALE The purpose of a recall is to remove from the market, a drug that represents an undue health risk. Drugs that have left the premises of a fabricator, packager/labeller, distributor, wholesaler and importer can be found in a variety of locations. Depending on the severity of the health risk, it may be necessary to recall a product to one level or another. Fabricators, packagers/labellers, distributors, wholesalers, and importers are expected to be able to recall to the consumer level if necessary. Additional guidance on recalls can be found in the Heath Canadas document entitled "Product Recall Procedures". This Regulation also requires fabricators, packagers/labellers, distributors, wholesalers, and importers to maintain a program of self-inspection. The purpose of self-inspection is to evaluate the compliance with GMP in all aspects of production and quality control. The self-inspection program is designed to detect any shortcomings in the implementation of GMP and to recommend the necessary corrective actions. Drugs offered for sale in Canada, regardless of whether they are domestically produced or are imported, must meet the requirements of the GMP Part C, Division 2 of the Food and Drug Regulations. Contract production and analysis must be correctly defined, agreed on, and controlled in order to avoid misunderstandings that could result in a product, or work, or analysis of unsatisfactory quality. Normally, a contract or other written agreement exists between the parties involved, and that document clearly establishes the duties of each party. INTERPRETATION 1. A written recall system is in place to ensure compliance with Section C.01.051 of the Food and Drug Regulations and requires the following: 1.1 1.2 Health Canada is to be notified of the recall. Action that is taken to recall a product suspected or known to be in violation is prompt and in accordance with a pre-determined plan; the procedures to be followed are in writing and are known to all concerned. The person(s) responsible for initiating and co-ordinating all recall activities are identified. The recall procedure is capable of being put into operation at any time, during and outside normal working hours. The recall procedure outlines the means of notifying and implementing a recall and of deciding its extent.
1.3 1.4
1.5
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 39
Health Canada / Health Products and Food Branch Inspectorate
1214 1215 1216 1217 1218 1219 1220 1221 1222 1223 1224 1225 1226 1227 1228 1229 1230 1231 1232 1233 1234 1235 1236 1237 1238 1239 1240 1241 1242 1243 1244 1245 1246 1247 1248 1249 3.
1.6
Distribution records enable tracing of each drug product, and account is taken of any products that are in transit, any samples that have been removed by the quality control department, and any professional samples that have been distributed. Wholesalers must obtain drug products from companies that hold an establishment licence as required in Part C, Division 1A of the Food and Drug Regulations in order to facilitate a system of control that permits complete and rapid recall. A contract or written agreement clearly describes the respective responsibilities between the wholesaler and the distributor or the importer relative to the recall of a drug. Recalled products are identified and are stored separately in a secure area until their disposition is determined.
1.7
1.8
1.79
1.810 The progress and efficacy of the recall is assessed and recorded at intervals, and a final report is issued (including a final reconciliation). 1.911 All Canadian and foreign establishments involved in the fabrication, distribution, or importation of the recalled product are notified. 2. A self-inspection program appropriate to the type of operations of the company, in respect to drugs, ensures compliance with Division 2, Part C of the Food and Drug Regulations. 2.1 A comprehensive written procedure that describes the functions of the self-inspection program is available. The program of a fabricator engaged in processing a drug from raw material through to the drug in dosage form addresses itself to all aspects of the operation. For packagers/labellers, distributors, importers, and wholesalers engaged only in packaging and/or distributing drugs fabricated by another fabricator, the written program covers only those aspects of the operations over which they exercise control on their premises. The self-inspection team includes personnel who are suitably trained and qualified in GMP. Periodic self-inspections are carried out. Reports on the findings of the inspections and on corrective actions are reviewed by appropriate senior company management. Corrective actions are implemented in a timely manner.
2.2
2.3
2.4 2.5
To ensure compliance of contract fabricators and packagers/labellers contractors performing fabrication and packaging/labelling: 3.1 All arrangements for contract fabrication or packaging/labelling and testing are in accordance with the marketing authorization for the drug product concerned.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 40
Health Canada / Health Products and Food Branch Inspectorate
1250 1251 1252 1253 1254 1255 1256 1257 1258 1259 1260 1261 1262 1263 1264 1265 1266 1267 1268 1269 1270 1271 1272 1273 1274 1275 1276 1277 1278 1279 1280 1281 1282 1283
3.2
There is a written contract or other agreement covering the fabrication or packaging/labelling and/or analysis arranged among the parties involved. The contract or agreement specifies their respective responsibilities relating to the fabrication or packaging/labelling and control of the product. 3.2.1 Technical aspects of the contract or agreement are drawn up by qualified personnel suitably knowledgeable in pharmaceutical technology, analysis, and GMP. The contract or agreement permits the distributor or importer to audit the facilities of the contractor. The contract or agreement clearly describes as a minimum who is responsible for: purchasing, sampling, testing, and releasing materials undertaking production, quality, and in-process controls process validation test method validation 3.2.4 The contract-acceptor shall not subcontract any of the work entrusted to him under the contract without written authorization from the contractgiver. The contract agreement specifies the way in which the quality control department of the distributor or importer releasing the lot or batch for sale, ensures that each lot or batch has been fabricated and packaged/labelled in compliance with the requirements of the marketing authorization. The contract agreement describes the handling of raw materials, packaging materials, in-process drug, bulk drug and finished products if they are rejected.
3.2.2
3.2.3
3.2.3.1 3.2.3.2 3.2.3.3
3.2.45.
3.2.56
3.3
The contractors complaint/recall procedures specify that any records relevant to assessing the quality of a drug product in the event of complaints or a suspected defect are accessible to the distributor or importer. The fabricator, packager/labeller, distributor, or importer provides the contractor with all the information necessary to carry out the contracted operations correctly in accordance with the marketing authorization and any other legal requirements. The fabricator, packager/labeller, distributor, or importer ensures that the contractor is fully aware of any problems associated with the product, work or tests that might pose a hazard to premises, equipment, personnel, other materials or other products.
3.4
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 41
Health Canada / Health Products and Food Branch Inspectorate
1284 1285 1286 1287 1288 1289 1290 1291 1292 1293 1294
3.5
The fabricator, packager/labeller, distributor, or importer is responsible for assessing the contractors continuing competence to carry out the work or tests required in accordance with the principles of GMP described in these guidelines. 3.5.1 Distributors of drugs fabricated, packaged/labelled and tested at Canadian sites are required only to have a copy of the relevant valid Canadian establishment licence held by the Canadian fabricator or packager/labeller or tester. Importers of drugs fabricated, packaged/labelled, or tested at a foreign site must meet the requirements described in the Health Canadas policy document entitled Conditions for of Acceptance for of Foreign Inspection Reports for Listing Foreign Sites on Canadian Establishment Licences.
3.5.2
1295 1296 1297 1298 1299 1300 1301 1302 1303 1304 1305 1306 1307 1308 1309 1310 1311 1312 1313 1314 1315 1316 1317 1318 1319
QUALITY CONTROL DEPARTMENT
REGULATION C.02.013 (1) Every fabricator, packager/labeller, wholesaler, distributor referred to in paragraph C.01A.003(b), and importer, shall have on their premises in Canada a quality control department that is supervised by personnel described in section C.02.006. Except in the case of a wholesaler, the quality control department referred to in subsection (1) shall be a distinct organizational unit that functions and reports to management independently of any other functional units including the manufacturing, processing, packaging or sales unit.
(2)
RATIONALE Quality control is the part of GMP concerned with sampling, specifications, and testing and with the organization, documentation, and release procedures. This Regulation ensures that the necessary and relevant tests are actually carried out and that raw materials and packaging materials are not released for use, nor products released for sale or supply, until their quality has been judged to be satisfactory. Quality control is not confined to laboratory operations but must be incorporated into all activities and decisions concerning the quality of the product. Although manufacturing and quality control personnel share the common goal of assuring that highquality drugs are fabricated, their interests may sometimes conflict in the short run as decisions are made that will affect a company's output. For this reason, an objective and accountable quality control process can be achieved most effectively by establishing an independent quality control department. The independence of quality control from manufacturing is considered fundamental. The rationale for the requirement that the quality control department be supervised by qualified personnel is outlined under Regulation C.02.006. INTERPRETATION
Page 42
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1320 1321 1322 1323 1324 1325 1326 1327 1328 1329 1330 1331 1332 1333 1334 1335 1336 1337 1338 1339 1340 1341 1342 1343 1344 1345 1346 1347 1348 1349 1350 1351 1352
1.
A person responsible for making decisions concerning quality control requirements of the fabricator, packager/labeller, distributor, and importer, and wholesaler is on site or fully accessible to the quality control department and has adequate knowledge of on-site operations to fulfill the responsibilities of the position. The quality control department has access to adequate facilities, trained personnel, and equipment in order to fulfill its duties and responsibilities. Approved written procedures are available for sampling, inspecting, and testing raw materials, packaging materials, in-process drugs, bulk drugs, and finished products. Quality control personnel have access to production areas for sampling and investigations as appropriate.
2.
3.
4.
REGULATION C.02.014 (1) Except in the case of a wholesaler, no lot or batch of drug shall be made available for sale unless the sale of that lot or batch is approved by the person in charge of the quality control department. A drug that is returned to the fabricator, packager/labeller, wholesaler, distributor referred to in paragraph C.01A.003(b) or importer thereof shall not be made available for further sale unless the sale of that drug is approved by the person in charge of the quality control department. No lot or batch of raw material or of packaging/labelling material shall be used in the fabrication or packaging/labelling of a drug, unless that material is approved for that use by the person in charge of the quality control department. No lot or batch of a drug shall be reprocessed or reworked without the approval of the person in charge of the quality control department.
(2)
(3)
(4)
RATIONALE The responsibility for the approval of all raw materials, packaging materials and finished products is vested in the quality control department. It is very important that adequate controls be exercised by this department in order to guarantee the quality of the end product. To maintain this level of quality, it is also important to examine all returned drugs and to give special attention to reprocessed drugs. INTERPRETATION 1. All decisions made by the quality control department pursuant to Regulation C.02.014 are signed and dated by the person in charge of the quality control department or by a designated alternate meeting the requirements described under Section C.02.006. Interpretation 1.4 or Interpretation 3.1 as applicable to the activity.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 43
Health Canada / Health Products and Food Branch Inspectorate
1353 1354 1355 1356 1357 1358 1359 1360 1361 1362 1363 1364 1365 1366 1367 1368 1369 1370 1371 1372 1373 1374 1375 1376 1377 1378 1379 1380 1381 1382 1383 1384 1385 1386 1387 1388
2.
The assessment for the release of finished products embraces all relevant factors, including the production conditions, the results of in-process testing, the fabrication and packaging documentation, compliance with the finished product specifications, an examination of the finished package, and if applicable, a review of the storage and transportation conditions. 2.1 Deviations and borderline conformances are evaluated in accordance with a written procedure. The decision and rationale are documented. Where appropriate, batch deviations are subject to trend analysis. Any non-conformances, malfunctions or errors including those pertaining to premises, equipment, sanitation, and testing, and personnel, that may have an impact on the quality and safety of batches pending release or released, should be assessed and the rationale documented. The quality control department of the importer/distributor in Canada should assure compliance to the current master production documents and the marketing authorization.
2.2
2.3
3.
The quality control department ensures that raw materials and packaging materials are quarantined, sampled, tested, and released prior to their use in the fabrication or packaging/labelling of a drug. Finished products returned from the market are destroyed unless it has been ascertained that their quality is satisfactory. Returned goods may be considered for resale only after they have been assessed in accordance with a written procedure. The reason for the return, the nature of the product, the storage and transportation conditions, the products condition and history, and the time elapsed since it was originally sold are to be taken into consideration in this assessment. Records of any action taken are maintained. A written agreement should clearly described the respective responsibilities between the distributor or the importer and the wholesaler. Documentation is available to support the rationale to place returned goods into inventory for further resale. Wholesalers may require written guidance from importers/distributors to make an informed decision pertaining to the restock of the product.
4.
5.
Rejected materials and products are identified as such and quarantined. They are either returned to the vendors, reprocessed, or destroyed. Actions taken are recorded. The reworking of any lot or batch of drug is given prior approval by the quality control department. Approval of a reworked lot or batch of a drug by the quality control department is based on documented scientific data, which may include validation. The reworking of products that fail to meet their specifications is undertaken only in exceptional cases. Reworking is permitted only when the following conditions are met: 6.1 6.2 The quality of the finished product is not affected; The reworked lot meets specifications;
6.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 44
Health Canada / Health Products and Food Branch Inspectorate
1389 1390 1391 1392 1393 1394 1395 1396 1397 1398 1399 1400 1401 1402 1403 1404 1405 1406 1407 1408 1409 1410 1411 1412 1413 1414 1415 1416 1417 8. 7.
6.3
If it is done in accordance with a defined procedure approved by the quality control department; All risks have been evaluated; Complete records of the reworking are kept; A new batch number is assigned; and The reworked lot is included in the ongoing stability program.
6.4 6.5 6.6 6.7
The reprocessing of any lot or batch of drug is given prior approval by the quality control department. Approval of a reprocessed lot or batch of a drug by the quality control department is based on documented scientific data, which may include validation. The reprocessing of products that fail to meet their specifications is undertaken only in exceptional cases. Reprocessing is permitted only when the following conditions are met: 7.1 7.2 7.3 The quality of the finished product is not affected; The reprocessed lot meets specifications; The reprocessing is done in accordance with a defined procedure approved by the quality control department; All risks have been evaluated; Complete records of the reprocessing are kept; A new batch number is assigned; and Validation demonstrates that the quality of the finished product is not affected.
7.4 7.5 7.6 7.7
Recovery is not considered to be either a reprocessing or a reworking operation. Guidance regarding recovery is found under Regulation C.02.011, Interpretation 28.1. The need for additional testing of any finished product that has been reprocessed, or reworked, or into which a recovered product has been incorporated, is evaluated and acted on by the quality control department. A record is maintained.
9.
REGULATION C.02.015 (1) All fabrication, packaging/labelling, testing, storage, and transportation methods and procedures that may affect the quality of a drug shall be examined and approved by the person in charge of the quality control department before their implementation.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 45
Health Canada / Health Products and Food Branch Inspectorate
1418 1419 1420 1421 1422 1423 1424 1425 1426 1427 1428 1429 1430 1431 1432 1433 1434 1435 1436 1437 1438 1439 1440 1441 1442 1443 1444 1445 1446 1447 1448 1449 1450 1451 1452
(2)
The person in charge of the quality control department shall cause to be investigated every complaint on quality or other information respecting the quality of a drug or its deficiencies or hazards that is received and cause corrective action to be taken where if necessary. The person in charge of the quality control department shall cause all tests or examinations required pursuant to this Division to be performed by a competent laboratory.
(3)
RATIONALE Pharmaceutical processes and products must be designed and developed taking GMP requirements into account. Production procedures and other control operations are independently examined by the quality control department. Proper storage, transportation, and distribution of materials and products minimize any risk to their quality. Complaints may indicate problems related to quality. By tracing their causes, one can determine which corrective measures should be taken to prevent recurrence. Having tests carried out by a competent laboratory provides assurance that test results are genuine and accurate. Written contracts agreements for consultants and contract laboratories describe the education, training, and experience of their personnel and the type of services provided and are available for examination and inspection. Records of the activities contracted are maintained. INTERPRETATION The quality control department is responsible for the following: 1. All decisions made pursuant to Regulation C.02.015. These decisions are signed and dated by the person in charge of the quality control department or by a designated alternate who meets the requirements described under Regulation C.02.006, Interpretation 1.4 or Interpretation 3.1 as applicable to the activity. Ensuring that guidelines and procedures are in place and implemented for storage and transportation conditions, such as: temperature, humidity, lighting controls, stock rotation, sanitation, and any other precautions necessary to maintain the quality and safe distribution of the drug. Further guidance relating to storage and transportation are detailed in Health Canadas document entitled Guidelines for Temperature Control of Drug Products during Storage and Transportation (GUI-0069). Standard operating procedures and records for shipping and receiving are available and contain the following: 2.2 Conditions of transportation and storage prevent any changes to the potency, purity, and physical characteristics of the drug. a description of the shipping configuration and the type of packaging to be employed for shipping the finished product; the labelling requirements, including storage conditions and special precautions or warnings, for shipments of the finished product; mode(s) of transportation approved for shipping the finished product;
2.
2.1
2.2
2.3
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 46
Health Canada / Health Products and Food Branch Inspectorate
1453 1454 1455 1456 1457 1458 1459 1460 1461 1462 1463 1464 1465 1466 1467 1468 1469 1470 1471 1472 1473 1474 1475 1476 1477 1478 1479 1480 1481 1482 1483 1484 1485 1486 1487 1488 1489 1490 1491 3.
2.4
the verifications required to ensure that no finished product in the shipment has been tampered with and that there are no damaged containers; and evidence that shipping requirements (e.g., temperature control) have been met if required. A written agreement clearly describes the respective responsibilities between the fabricator, the packager/labeller, the distributor, the importer, the wholesaler and the transportation provider relative to the storage and transportation of the drug.
2.5 2.6
The sampling of raw materials, packaging materials, in-process drugs, bulk drugs, and finished products is carried out in accordance with detailed written procedures. Samples are representative of the batches of material from which they are taken. All complaints and other information concerning potentially defective products are reviewed according to written procedures. The complaint is recorded with all the original details and thoroughly investigated. Appropriate follow-up action is taken after investigation and evaluation of the complaint. All decisions and measures taken as a result of a complaint are recorded and referenced to the corresponding batch records. Complaint records are regularly reviewed for any indication of specific or recurring problems that require attention. The same procedures are applied to recalls. Establishing a change control system to provide the mechanisms for ongoing process optimization and for assuring a continuing state of control. All changes are properly documented, evaluated, and approved by the quality control department and are identified with the appropriate effective date. Any significant change may necessitate re-validation. The tests are performed by a laboratory that meets all relevant GMP requirements. 6.1 Laboratory facilities are designed, equipped, and maintained to conduct the required testing. 6.1.1 In the microbiology laboratory, environmental monitoring is performed periodically. Microbiological cultures and sample testing are handled in an environment that minimizes contamination. The facility used to perform the sterility testing should be such as to comply with the microbial limits of an aseptic production facility which should conform to a Grade A within a Grade B background or in an isolator of a Grade A within a Grade D background.
4.
5.
6.
6.1.2
6.2
The individual in charge of the laboratory either (a) is an experienced university graduate who holds a degree in a science related to the work being carried out and has practical experience in his or her responsibility area or (b) reports to a person who has these qualifications .02.006, Interpretation 1). Laboratory personnel are sufficient in number and are qualified to carry out the work they undertake.
6.3
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 47
Health Canada / Health Products and Food Branch Inspectorate
1492 1493 1494 1495 1496 1497 1498 1499 1500 1501 1502 1503 1504 1505 1506 1507 1508 1509 1510 1511 1512 1513 1514 1515 1516 1517 1518 1519 1520 1521 1522 1523 1524 1525 1526 1527
6.4
Laboratory control equipment and instruments are suited to the testing procedures undertaken. Equipment and records are maintained as per the interpretations under C.02.005. qualified, serviced and calibrated at suitable intervals according to an approved procedure, and records are maintained. Computerized systems are validated, and spreadsheets are qualified. Water used for microbial and analytical tests meets the requirements of the test or assay in which it is used. Sensitive apparatus are protected against conditions (e.g., humidity, temperature, vibration, etc.) that may affect their functioning. All reagents and culture media are recorded upon receipt or preparation. Reagents made up in the laboratory are prepared according to written procedures and are properly labelled. 6.7.1 Prepared media are sterilized using validated procedures and stored under controlled temperatures. All prepared media are properly Labelled with the lot numbers, expiration date and media identification. Both positive and negative controls The expiration date on media is supported by growth-promotion testing results that show the performance of the media still meets acceptance criteria up to and including the expiration date. Sterility and growth-promotion testing are applied performed to verify the suitability of culture media. The size of the inoculums used in positive controls relates to the required sensitivity. All purchased ready to use media received are accompanied by a certificate of analysis with expiry date and recommended storage conditions as well as the quality control organisms used in growth-promotion and selectivity testing of that media. Procedures are in place to ensure that media are transported under conditions that minimize the loss of moisture and control the temperature. Media are stored according to the vendors instructions. Sterility and growth-promotion testing are performed on lots received, unless the vendor is certified. Periodic confirmatory testing is performed for ready to use media received from each certified vendor. Records are maintained.
6.5 6.6
6.5
6.67
6.7.2
6.7.3
6.7.4
6.7.4.1
6.7.4.2 6.7.4.3
6.7.4.4 6.78
Reference standards are available in the form of the current reference standards listed in Schedule B to the Food and Drugs Act. When such standards have not been established or are unavailable, primary standards can be used. Secondary standards are verified against a
Page 48
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1528 1529 1530 1531 1532 1533 1534 1535 1536 1537 1538 1539 1540 1541 1542 1543 1544 1545 1546 1547 1548 1549 1550 1551 1552 1553 1554 1555 1556 1557 1558 1559 1560 1561 1562 1563 1564 6.10. 6.9
Schedule B reference standard or against the primary standard and are subject to complete confirmatory testing at predetermined intervals. All reference standards are stored and used in a manner that will not adversely affect their quality. Records relating to their testing, storage, and use are maintained. Out of Specification (OOS) test results are investigated to determine the cause of the OOS. 6.9.1 Procedures are in place to describe the steps to be taken as part of the investigation. In the case of a clearly identified laboratory or statistical error, the original results may be invalidated, and the test repeated. The original results should be retained and an explanation recorded. When there is no clearly identified laboratory or statistical error and retesting is performed, the number of retests to be performed on the original sample and/or a new sample, and the statistical treatment of the resultant data, are specified in advance in the procedure. All valid test results, both passing and suspect, should be reported and considered in batch release decisions. If the original OOS result is found to be valid, a deviation is raised against the batch and a complete investigation is conducted.
6.9.2
6.9.3
6.9.4
6.9.5
Note: Additional guidance may be obtained from published international guidelines. To ensure compliance of contractors conducting testing: 6.10.1 A Canadian external laboratory must have a relevant valid current establishment licence. A foreign testing site must be listed on the importers establishment licence, as described in Health Canadas policy document entitled Conditions of Acceptance of Foreign Inspection Reports for Listing Foreign Sites on Canadian Establishment Licences. All arrangements for external testing are in accordance with the marketing authorization for the drug product concerned, including the testing of inprocess drugs, intermediates, raw materials, packaging materials and all other necessary testing required by Part C, Division 2 of the Food and Drug Regulations. There is a written agreement covering all activities of testing between the external laboratory and the parties involved. The agreement specifies their respective responsibilities relating to all aspects of testing. Technical aspects of the agreement are drawn up by qualified personnel suitably knowledgeable in analysis and GMP.
6.10.2
6.10.3
6.10.3.1
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 49
Health Canada / Health Products and Food Branch Inspectorate
1565 1566 1567 1568 1569 1570 1571 1572 1573 1574 1575 1576 1577 1578 1579 1580 1581 1582 1583 1584 1585 1586 1587 1588 1589 1590 1591 1592 1593 1594 1595 1596
6.10.3.2
The agreement permits audit of the facilities and operations of the external laboratory. The agreement clearly describes as a minimum who is responsible for: 6.10.3.3.1 collection, transportation and storage conditions of samples before testing keeping stability samples at predetermined temperatures and humidity, if applicable testing methods to be used, limits and test method validation retention of analytical results and supporting documentation (additional guidance under interpretations of C.02.021)
6.10.3.3
6.10.3.3.2
6.10.3.3.3
6.10.3.3.4
6.10.3.4
No subcontracting of any work should occur without written authorization.
PACKAGING MATERIAL TESTING
REGULATION C.02.016 (1) Each lot or batch of packaging material shall, prior to its use in the packaging of a drug, be examined or tested against the specifications for that packaging material. No lot or batch of packaging material shall be used in the packaging of a drug unless the lot or batch of packaging material complies with the specifications for that packaging material. The specifications referred to in subsections (1) and (2) shall (a) (b) be in writing; be acceptable to the Director who shall take into account the specifications contained in any publication mentioned in Schedule B to the Act; and be approved by the person in charge of the quality control department.
(2)
(3)
RATIONALE Where a drug product is presented in an inadequate package, the entire effort put into the initial research, product development and manufacturing control is wasted. Drug quality is directly dependent on packaging quality. In many cases (e.g., metered-dose aerosols), packaging quality is critical to the overall performance and effectiveness of the drug product. Faults in the packaging and labelling of a drug
Page 50
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1597 1598 1599 1600 1601 1602 1603 1604 1605 1606 1607 1608 1609 1610 1611 1612 1613 1614 1615 1616 1617 1618 1619 1620 1621 1622 1623 1624 1625 1626 1627 1628 1629
product continue to be a major cause of drug recalls. Packaging materials are required to be tested or examined prior to their use in a packaging operation to ensure that materials of acceptable quality are used in the packaging of drugs. INTERPRETATION 1. Each packaging material used in the packaging/labelling of a drug is covered by specifications (as defined under C.02.002) that are approved and dated by the person in charge of the quality control department or by a designated alternate who meets the requirements described under Regulation C.02.006, Interpretation 1.4. The use of recycled or reprocessed primary packaging components is permitted only after a full evaluation of the risks involved, including any possible deleterious effects on product integrity. Specific provision is made for such a situation in the specifications. Where applicable, specifications are of pharmacopeial or equivalent status and are in compliance with the marketing authorization. The adequacy of test or examination methods that are not of pharmacopeial or equivalent status is established and documented. Only packaging materials released by the quality control department are used in packaging/labelling. Outdated or obsolete packaging material is adequately segregated until its disposition. The sampling plan for packaging materials should take account of at least the following: the quantity received, the level of quality required, the nature of the material (e.g., primary packaging materials and/or printed packaging materials), the production methods, and what is known of the Quality Assurance system of the packaging materials manufacturer based on audits. The number of samples taken should be determined statistically and specified in a sampling plan. 6.1 Because of the higher risk of using cut labels, these labels are inspected upon receipt for absence of foreign labels using appropriate methods. Sampling plans for bottles should also take into consideration the mold production number.
2.
3.
4.
5. 6.
6.2
7.
Sampling should take place in an appropriate environment and with adequate gowning to prevent contamination where necessary.
REGULATION C.02.017 (1) The examination or testing referred to in section C.02.016 shall be performed on a sample taken (a) after receipt of each lot or batch of packaging material on the premises of the person who packages a drug; or
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 51
Health Canada / Health Products and Food Branch Inspectorate
1630 1631 1632 1633 1634 1635 1636 1637 1638 1639 1640 1641 1642 1643 1644 1645 1646 1647 1648 1649 1650 1651 1652 1653 1654 1655 1656 1657 1658 1659 1660 1661 1662 (2)
(b)
subject to subsection (2), before receipt of each lot or batch of packaging material on the premises of the person who packages a drug, if (I) that person (A) has evidence satisfactory to the Director to demonstrate that packaging materials sold to him by the vendor of that lot or batch of packaging material are consistently manufactured in accordance with and consistently comply with the specifications for those packaging materials; and undertakes periodic complete confirmatory examination or testing with a frequency satisfactory to the Director,
(B)
(ii) the packaging material has not been transported or stored under conditions that may affect its compliance with the specifications for that packaging material. After a lot or batch of packaging material is received on the premises of the person who packages a drug, (a) (b) the lot or batch of the packaging material shall be examined or tested for identity; and the labels shall be examined or tested in order to ensure that they comply with the specifications for those labels.
RATIONALE Regulation C.02.017 outlines options as to when the testing or examination prescribed by Regulation C.02.016 is carried out. As with raw materials, the purchase of packaging materials is an important operation that involves personnel who have a particular and thorough knowledge of the packaging materials and vendor. Packaging materials originate only from vendors named in the relevant specifications. It is of benefit that all aspects of the production and control of packaging materials be discussed between the manufacturer and the vendor. Particular attention is paid to printed packaging materials; labels are examined or tested after receipt on the premises of the person who packages a drug. INTERPRETATION 1. The testing or examination of the packaging material is performed on a sample taken after their receipt on the premises of the person that packages the drug unless the vendor is certified. A packaging material vendor certification program, if employed, is documented in a standard operating procedure. The following approaches may be used for vendor certification At a minimum, such a program includes the following: 1.1 A written contract agreement outlines the specific responsibilities of each party involved. As a minimum, that contract specifies the following: The agreement specifies:
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 52
Health Canada / Health Products and Food Branch Inspectorate
1663 1664 1665 1666 1667 1668 1669 1670 1671 1672 1673 1674 1675 1676 1677 1678 1679 1680 1681 1682 1683 1684 1685 1686 1687 1688 1689 1690 1691 1692 1693 1694 1695 1696 1697 1698 1699 2. 1.2
1.1.1
all the tests to be performed by the vendor, along with the content and format of the certificate of analysis, which exhibits actual numerical results, if applicable, and makes reference to product specifications. that the vendor must inform the drug packager/labeller of any changes in the processing or specifications of the packaging material; and that the vendor must inform the drug packager/labeller of any critical deviations during the manufacturing of a particular batch of a packaging material.
1.1.2
1.1.3
In lieu of an contract agreement, an on-site audit of the vendors facilities and controls by qualified personnel is acceptable. The audit ensures that all criteria described under Interpretation 1.1 are verified. These audits are performed at an appropriate frequency, and the results are documented. The certification procedure also outlines how re-testing failures and any subsequent requalification is to be addressed. A document is issued for each vendor verifying that the certification criteria have been met. The document is approved by the quality control department and is updated at an appropriate frequency. When a certification program is implemented, complete confirmatory examination or testing of a minimum of one lot per year per vendor is required for non-printed packaging material. Generally, due to the nature of its operations, a broker or wholesaler of packaging materials cannot be directly certified. However, when evidence is available that all original labels, certificate of analysis, general information, and package supplied by the original vendor of the packaging material has not been altered in any way during the distribution sequence, certification of the original source is still acceptable. Generally, due to the nature of its operations, a broker or wholesaler of packaging materials cannot be directly certified. However, when a broker or wholesaler supplies materials received from the original vendor without changing the existing labels, packaging, certificate of analysis, and general information, then certification of the original source is still acceptable.
1.3
3.
1.4
4.
1.5
5.
1.6
62.
Provided that the material is properly identified, a the lot or batch of packaging material selected for confirmatory testing may, with the approval of the quality control department, be used in packaging prior to completion of that testing. Conditions of transportation and storage are such that they prevent alterations of the characteristics of the packaging material. In order to demonstrate that these conditions have been met, standard operating procedures and records are available and contain the following: 73.1 73.2 the type of packaging to be employed; labelling requirements;
Page 53
73.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1700 1701 1702 1703 1704 1705 1706 1707 1708 84.
73.3 73.4 73.5
mode of transportation; the type of seal used on the package; and the verification required to ensure that the package has not been tampered with and that there are no damaged containers.
Positive identification on of all packaging materials, along with examination of all labels and other printed packaging materials, is conducted following their receipt on the premises of the person who packages the drug. If a delivery or shipment of packaging material is made up of different batches, each batch is considered as separate for the purposes of sampling, testing, and release.
95.
1709 1710 1711 1712 1713 1714 1715 1716 1717 1718 1719 1720 1721 1722 1723 1724 1725 1726 1727 1728 1729 1730
FINISHED PRODUCT TESTING
REGULATION C.02.018 (1) Each lot or batch of a drug shall, prior to its availability for sale, be tested against the specifications for that drug. No lot or batch of a drug shall be available for sale unless it complies with the specifications for that drug. The specifications referred to in subsections (1) and (2) shall (a) (b) ) be in writing; be approved by the person in charge of the quality control department; and comply with the Act and these Regulations.
(2)
(3)
RATIONALE Finished product tests complement the controls employed during the manufacturing process. It is at this stage that drugs are either accepted or rejected. For these reasons, it It is the responsibility of each fabricator, packager/labeller, distributor, and importer to have use adequate specifications and test methods that will help ensure that each drug sold is safe and meets the standard under which it is represented. INTERPRETATION 1. Written specifications are approved by the person in charge of the quality control department or by a designated alternate who meets the requirements described under Regulation C.02.006 as applicable to the activity.
Page 54
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1731 1732 1733 1734 1735 1736 1737 1738 1739 1740 1741 1742 1743 1744 1745 1746 1747 1748 1749 1750 1751 1752 1753 1754 1755 1756 1757 1758 1759 1760 1761 1762 1763 1764 1765 1766 1767 35. 24.
1.11.
The written specifications contain a description of the drug in dosage form. This description includes all properties and qualities, including physical characteristics, identity, purity, and potency. The S specifications also include tolerances and a description describe of all tests used to measure compliance with the established tolerances, determine those properties and qualities, in sufficient detail to permit performance by qualified personnel. When a unique identifier is used for identity testing, it is described in the specifications. These specifications are approved by the person in charge of the quality control department or by a designated alternate who meets the requirements described under Regulation C.02.006, Interpretation 1.4 or Interpretation 3.1 as applicable to the activity. Specifications are equal to or exceed a recognized standard as listed in Schedule B to the Food and Drugs Act and are in compliance with the marketing authorization. Specifications are in compliance with the marketing authorization. When a monograph exists in a pharmacopoeia listed in Schedule B to the Food and Drug Act, specifications meet the monograph. Where a recognized pharmacopoeia (Schedule B to the Food and Drugs Act) contains a specification for microbial content, that requirement is included.
1.22.
1.33.
Test methods are validated, and the results of such validation studies are documented. Method transfer studies are conducted when applicable. Note: Guidance for the validation of particular types of methods can be obtained in publications such as the ICH guidelines document entitled ICH Q2(R1): Validation of Analytical procedures: Text and Methodology or any standard listed in Schedule B to the Food and Drugs Act. All tests are performed according to the approved specifications. These tests may be carried out by the distributor or by their contracted testing laboratory when a written contract agreement specifically excludes the fabricator from this obligation. Any lot or batch of a drug that does not comply with specifications is quarantined pending final disposition and is not made available for sale.
4.
REGULATION C.02.019 (1) Subject to subsections (3) and (4), in the case of a packager/labeller, distributor referred to in paragraph C.01A.003(b) or importer, the testing referred to in section C.02.018 shall be performed on a sample taken (a) after receipt of each lot or batch of the drug on the premises in Canada of the packager/labeller, distributor referred to in paragraph C.01A.003(b) or importer of the drug; or subject to subsection (2), before receipt of each lot or batch of the drug on the premises described in paragraph (a), if;
Page 55
(b)
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1768 1769 1770 1771 1772 1773 1774 1775 1776 1777 1778 1779 1780 1781 1782 1783 1784 1785 1786 1787 1788 1789 1790 1791 1792 1793 1794 1795 1796 1797 1798 1799 1800 1801 (2)
(I) the packager/labeller, distributor referred to in paragraph C.01A.003(b) or importer (A) has evidence satisfactory to the Director to demonstrate that drugs sold to him by the vendor of that lot or batch of the drug are consistently manufactured in accordance with and consistently comply with the specifications for those drugs; and undertakes periodic complete confirmatory testing with a frequency satisfactory to the Director; and
(B)
(ii) the drug has not been transported or stored under conditions that may affect its compliance with the specifications for that drug. Where the packager/labeller, distributor referred to in paragraph C.01A.003(b) or importer of a drug receives a lot or batch of a drug on the premises in Canada, and the useful life of the drug is more than 30 days, the lot or batch of the drug shall be tested for identity, and the packager/labeller shall confirm the identity after the lot or batch is packaged/labelled. The distributor referred to in paragraph C.01A.003(b) of a drug that is fabricated, packaged/labelled and tested in Canada by a person who holds an establishment licence that authorizes those activities is not required to comply with the requirements of subsections (1) and (2) in respect of that drug. If a drug is fabricated, packaged/labelled and tested in an MRA country at a recognized building, the distributor referred to in paragraph C.01A.003(b) or importer of that drug is not required to comply with the requirements of subsections (1) and (2) in respect of that drug if (a) the address of the building is set out in that persons establishment licence; and (b) that person retains a copy of the batch certificate for each lot or batch of the drug received by that person. RATIONALE C.02.019 outlines conditions and exemptions as to when finished product testing is to be performed. Paragraph C.02.019(1) (b) outlines requirements that are to be met if the finished product testing is done before receipt on the premises of the packager/labeller, distributor, or importer of the drug. Paragraphs C.02.019(3) and C.02.019(4) outline exemptions to this requirement finished product testing. INTERPRETATION 1. Identity is confirmed by the packager/labeller after the lot or batch is packaged.
(3)
(4)
TRANSPORTATION AND STORAGE Discuss move of this section to C.02.015. The intent of C.02.019 is to require testing on the premise in Canada if not shipped or stored properly prior to receipt. C.02.015 may be a better fit to describe requirements for procedures relating to storage and transportation.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 56
Health Canada / Health Products and Food Branch Inspectorate
1802 1803 1804 1805 1806 1807 1808 1809 1810 1811 1812 1813 1814 1815 1816 1817 1818 1819 1820 1821 1822 1823 1824 1825 1826 1827 1828 1829 1830 1831 1832 1833 1834 1835 1836 1837
2.
Conditions of transportation and storage prevent any changes to the potency, purity, and physical characteristics of the drug. Further guidance relating to storage and transportation are detailed in the guide Guidelines for Temperature Control of Drug Products during Storage and Transportation (GUIDE-0069). Standard operating procedures and records for shipping and receiving are available and contain the following: 2.1 a description of the shipping configuration and the type of protective packaging to be employed for shipping the finished product; the labelling requirements, including storage conditions and special precautions or warnings, for shipments of the finished product; mode(s) of transportation approved for shipping the finished product; a description of how shipments of the finished product are to be sealed; the verifications required to ensure that no finished product in the shipment has been tampered with and that there are no damaged containers; and evidence that shipping requirements (e.g., temperature control) have been met if required.
2.2
2.3 2.4 2.5
2.6
SITES HOLDING A CANADIAN ESTABLISHMENT LICENCE 32. To demonstrate compliance with finished product specifications, distributors of drugs fabricated, packaged/labelled and tested at Canadian sites are required only to have a copy of the authentic certificate of analysis from the licensed Canadian fabricator. This certificate shows actual numerical results and refers to the product specifications and validated test methods used. Retesting, including identity testing, is not required.
RECOGNIZED BUILDINGS BY A REGULATORY AUTHORITY IN A MRA COUNTRY 43. To demonstrate compliance with finished product specifications, importers of drugs fabricated, packaged/labelled, and tested at recognized buildings authorized by a Regulatory Authority as listed by virtue of Regulation C.01A.019 and identified on their establishment licence are required only to have a fabricators batch certificate from the foreign fabricator in the format agreed on by the MRA partners for each lot or batch of the drug received. Re-testing, including identity testing, is not required when the drug is fabricated, packaged/labelled, and tested in an MRA country.
SITES IN NON-MRA COUNTRIES 54. For testing other than identity testing, the following conditions are to be met if the packager/labeller or importer chooses to rely on the test results provided by a fabricator an establishment located in a non-MRA country: 54.1 Evidence of ongoing GMP compliance is provided according to a system described in the interpretation of Regulation C.02.012 as demonstrated by listing on the packager/labellers or importers establishment licence. Five consecutive lots from the establishment located in a non-MRA country are tested and found to comply with the specifications.
Page 57
4.2
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1838 1839 1840 1841 1842 1843 1844 1845 1846 1847 1848 1849 1850 1851 1852 1853 1854 1855 1856 1857 1858 1859 1860 1861 1862 1863 1864 1865 1866 1867 1868 1869 1870 1871 1872 1873 1874 76. 65.
5.24.3 Each lot is accompanied by an authentic certificate of analysis or by a copy thereof (an electronic copy with an electronic signature is acceptable). The certificate of analysis exhibits actual numerical results and makes reference to the product specifications and validated test methods used. 5.2.1 4.3.1 For terminally sterilized products, documented evidence is available from the fabricator to demonstrate that each sterilizer load was individually tested. 5.2.24.3.2 For aseptically filled products, evidence demonstrates that samples tested for sterility included the first container filled, the last container filled, and those filled after any significant interruption of work. 5.34.4 Evidence is available to demonstrate that each lot or batch received has been transported and stored in a manner that maintains the quality of the drug. Further requirements are described in interpretation 2 of section C.02.015. 5.44.5 Periodic complete confirmatory testing is performed on every fifth lot received or two lots a year, whichever is greater. on at least one lot per year per dosage form per fabricator. For each dosage form, products are selected on a rotational basis. Re-testing by the original laboratory is acceptable; however, it is recommended that re-testing be performed by an alternate laboratory. No confirmatory testing for sterility, pyrogen (endotoxin), bacterial endotoxin, particulate matter, or general safety is required. 54.6 Provided that a specific identity test is performed, a lot or batch of the finished product selected for periodic confirmatory testing may, with the approval of the quality control department, be released for sale prior to completion of all tests.
Should any failure to conform to finished product testing requirements be identified, an investigation of the extent of the non-compliance is to be conducted. This investigation may lead to reassessment and re-testing of all dosage forms from the fabricator. This procedure may include: 65.1 65.2 re-evaluation of GMP compliance; and additional complete confirmatory testing, based on the risk associated with the noncompliance.
Positive identification of each lot or batch in a shipment of a drug is carried out on a sample taken after receipt on the premises of the packager/labeller or the importer. This identity testing requirement applies to lots received from any non-MRA site. Laboratory chemical/biological testing is required unless the dosage form has unique physical characteristics. Acceptable identity testing methods include the following: 76.1 76.2 76.3 chemical testing; biological testing; and physical verification in cases where the product has unique identifiers.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 58
Health Canada / Health Products and Food Branch Inspectorate
1875 1876 1877 1878 1879 1880 1881 1882 1883 1884 1885 1886 1887 1888 1889 1890 1891 1892 1893 1894 1895 1896 1897 1898 1899 1900 1901 1902 1903 1904 1905
76.3.1
The unique identifier principle must be applied before the final chemical or biological identity testing is performed by the fabricator. Where only a portion of a lot is packaged/labelled for Canada, the identity testing must be performed after the unique identifier is applied on the Canadian labelled product. For each product and each strength, uniqueness must be confirmed in writing by the fabricator to the importer at least once a year, as well as whenever a change occurs. When no such confirmation can be obtained, chemical or biological identity testing will be required from the importer. The unique identifier must be confirmed on the certificate of analysis for each lot received from the fabricator. Label review or examination of the shape and size of the container is not generally considered adequate identity testing. The following unique identifiers are considered acceptable: Tablets and capsules that are engraved, embossed, or printed with a unique logo; Permanent identification on the drugs closure system that indicates the name and strength of the contents. This marking must be applied as part of a continuous filling process and only where the closure cannot be removed without being destroyed. Colour closure systems as part of a continuous filling process when the fabricator uses a uniquely coloured cap or closure for only one product and strength; A coloured vial, sometimes used for light-sensitive drugs, if it is unique to one product, strength, and fabricator; A dedicated facility fabricating only one product; Labelling, where preprinted containers are issued to the filling line and where the lot number either is pre-printed or is printed or crimped onto the package in a continuous process; and Group 2 products subject to Health Canadas lot release program.
76.3.2
76.3.3
Note:
7.46.3.4 76.3.4.1
76.3.4.2
76.3.4.3
76.3.4.4
76.3.4.5 76.3.4.6
76.3.4.7
1906 1907
RECORDS
REGULATION
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 59
Health Canada / Health Products and Food Branch Inspectorate
1908 1909 1910 1911 1912 1913 1914 1915 1916 1917 1918 1919 1920 1921 1922 1923 1924 1925 1926 1927 1928 1929 1930 1931 1932 1933 1934 1935 1936 1937
C.02.020 (1) Every fabricator, packager/labeller, distributor referred to in paragraph C.01A.003(b) and importer shall maintain on their premises in Canada for each drug sold (a) (b) master production documents for the drug; evidence that each lot or batch of the drug has been fabricated, packaged/labelled, tested and stored in accordance with the procedures described in the master production documents; evidence that the conditions under which the drug was fabricated, packaged/labelled, tested and stored are in compliance with the requirements of this Division; evidence establishing the period of time during which the drug in the container in which it is sold will meet the specifications for that drug; and adequate evidence of the testing referred to in section C.02.018.
(d)
(e) (2)
Every distributor referred to in paragraph C.01A.003(b) and importer shall make available on request the results of testing performed on raw materials and packaging/labelling materials for each lot or batch of a drug sold. Every fabricator shall maintain on his premises (a) (b) the written specifications for the raw material; and adequate evidence of the raw materials testing referred to in section C.02.009.
(3)
(4)
Every person who packages a drug shall maintain on his premises (a) (b) the written specifications for the packaging materials; and adequate evidence of the packaging material examination or testing referred to in section C.02.016.
(5)
Every fabricator shall maintain on their premises in Canada: (a) detailed plans and specifications of each building in Canada at which they fabricate, package/label or test; and a description of the design and construction of those buildings.
(b) (6)
Every fabricator, packager/labeller and tester shall maintain on their premises in Canada details of the personnel employed to supervise the fabrication, packaging/labelling and testing, including each person's title, responsibilities, qualifications, experience and training.
C.02.021
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 60
Health Canada / Health Products and Food Branch Inspectorate
1938 1939 1940 1941 1942 1943 1944 1945 1946 1947 1948 1949 1950 1951 1952 1953 1954 1955 1956 1957 1958 1959 1960 1961 1962 1963 1964 1965 1966 1967 1968 1969 1970 1971 1972
(1)
Subject to subsection (2), all records and evidence on the fabrication, packaging/labelling, testing and storage of a drug that are required to be maintained under this Division shall be retained for a period of at least one year after the expiration date on the label of the drug, unless otherwise specified in the person's establishment licence. All records and evidence on the testing of raw materials and packaging/labelling materials that are required to be maintained under this Division shall be retained for a period of at least five years after the materials were last used in the fabrication or packaging/labelling of a drug unless otherwise specified in the person's establishment licence.
(2)
C.02.022 Every distributor referred to in section C.01A.003, wholesaler and importer of a drug shall retain records of the sale of each lot or batch of the drug, which enable them to recall the lot or batch from the market for a period of at least one year after the expiration date of the lot or batch unless otherwise specified in their establishment licence. C.02.023 (1)On receipt of a complaint or other information respecting the quality of a drug or its deficiencies or hazards, every fabricator, packager/labeller, wholesaler, distributor referred to in paragraph C.01A.003(b), and importer of the drug, as the case may be, shall make a record of the complaint or other information and of its investigation and retain the records for a period of at least one year after the expiration date of the lot or batch of the drug, unless otherwise specified in their establishment licence their establishment licence specifies otherwise. (2) On receipt of any information respecting the quality or hazards of a drug, every distributor referred to in paragraph C.01A.003(b), and importer of the drug shall make a record of the information and retain it for a period of at least one year after the expiration date of the lot or batch of the drug unless otherwise specified in their establishment licence.
C.02.024 (1) Every fabricator, packager/labeller, distributor referred to in section C.01A.003 importer and wholesaler shall (a) maintain records of the results of the self-inspection program required by section C.02.012 and of any action taken in connection with that program; and retain those records for a period of at least three years.
(b) (2)
Every person who fabricates or packages/labels a drug shall (a) maintain records on the operation of the sanitation program required to be implemented under section C.02.007, and retain those records for a period of at least three years.
(b)
RATIONALE
Page 61
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
1973 1974 1975 1976 1977 1978 1979 1980 1981 1982 1983 1984 1985 1986 1987 1988 1989 1990 1991 1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010
Good documentation is an essential part of the quality assurance system and should therefore be related to all aspects of GMP. Its aims are to define the specifications for all materials and methods of fabrication, packaging/labelling, and control; to ensure that the quality control department has all the information necessary to decide whether or not to release a batch of a drug for sale; and to provide an audit trail that will permit investigation of the history of any batch that is suspected to be defective. Evidence that drugs have been fabricated and packaged/labelled under prescribed conditions can be maintained only after developing adequate record systems. The information and evidence should provide assurance that imported drugs are fabricated and packaged/labelled in a like manner to those produced in Canada. INTERPRETATION For all sections of Good Manufacturing Practices guidelines, standard operating procedures (SOPs) are retained for reference and inspection. These SOPs are regularly reviewed and kept up to date by qualified personnel. The reasons for any revisions are documented. A system is in place to ensure that only current SOPs are in use. Records of SOPs for all computer and automated systems are retained where appropriate. All relevant GMP documents (such as associated records of actions taken or conclusions reached) and SOPs are approved, signed, and dated by the quality control department. Documents are not altered without the approval of the quality control department. Any alteration made to a document is signed and dated; the alteration permits the reading of the original information. Where appropriate, the reason for the change is recorded. Records may be maintained in electronic format provided that backup copies are also maintained. Electronic data must be readily retrievable in a printed format. During the retention period, such records must be secured and accessible within 48 hours to the fabricator, packager/labeller, distributor, or importer. An electronic signature is an acceptable alternative to a handwritten signature. When used, such a system must be evaluated and tested for security, validity, and reliability, and records of those evaluations and tests must be maintained. The validation of electronic signature identification systems is documented. Any documentation requested for evaluation by Health Canada is provided in one of the official languages. 1. The following documents are maintained by the fabricator, packager/labeller, distributor referred to in paragraph C.01A.003(b) and importer of a drug: 1.1 Master production documents as defined in the Glossary of Terms. 1.1.1 When the fabricator is located in Canada, specific parts of a master production document considered to be a trade secret or confidential may be held by the fabricator rather than the distributor. When the fabricator is located outside Canada, specific parts of a master production document considered to be a trade secret or confidential may be held on behalf of the distributor or importer by an independent party in Canada. In either case, the distributor or
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 62
Health Canada / Health Products and Food Branch Inspectorate
2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021 2022 2023 2024 2025 2026 2027 2028 2029 2030 2031 2032 2033 2034 2035 2036 2037 2038 2039 2040 2041 2042 2043 2044 2045 2046 2047 2048 2049 2050 1.3 1.2 1.1.2
importer must ensure that Health Canada has access to the data in a timely manner. Regardless of whether the fabricator is Canadian or foreign, the master production documents retained by the distributor or importer describes in general terms whatever information has been deleted as a trade secret or confidential.
Evidence that each lot or batch of the drug has been fabricated, packaged/labelled, tested and stored in accordance with the procedures described in the master production documents. 1.2.1 This evidence includes manufacturing orders, packaging orders, and test results for raw materials, packaging materials, and drugs in dosage form. However, when the drug is fabricated or packaged outside the premises of the distributor or importer, test results for raw materials and packaging materials need only be made available on request in a timely manner. A certificate of manufacture is considered an acceptable alternative to complete batch documentation, provided that complete documentation is made available on request in a timely manner. Where an importer of drugs from non-MRA countries employs a system involving a certificate of manufacture, complete batch documentation is obtained at least once per year per drug. A certificate of manufacture alone cannot be employed where reworking has taken place. Should there be changes to the production documents, the complete documentation is provided to the importer or distributor, and any changes that have been made are indicated.
1.2.2
1.2.3.
1.2.4.
Evidence that the conditions under which the drug was fabricated, packaged/labelled, tested, and stored are in compliance with the requirements of this Part C, Division 2 of the Food and Drug Regulations. 1.3.1 This evidence includes records generated under subsection C.02.012(2) and evidence of validation. For additional guidance, refer to the Health Canadas document entitled Validation Documentation Requirements and Responsibilities for Drug Fabricators, Packagers/Labellers, Testers, Distributors and Importers (GUI-0042). Records include the name, address, and qualifications/experience of any consultant employed for GMP purposes, along with the services that each consultant provides. Records of consultants activities (contracts) are maintained. Records are maintained detailing the qualifications/experience of any consultant employed for GMP purposes, along with the services that each consultant provides.
Page 63
1.3.2
1.3.2
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
2051 2052 2053 2054 2055 2056 2057 2058 2059 2060 2061 2062 2063 2064 2065 2066 2067 2068 2069 2070 2071 2072 2073 2074 2075 2076 2077 2078 2079 2080 2081 2082 4. 3. 2.
1.4
Evidence establishing the period of time during which the drug in the container in which it is sold will meet the specifications for that drug. 1.4.1 The documentation to be maintained includes the written stability program, the data generated in accordance with that program, and the conclusions leading to the establishment of the period of time during which each drug in the package in which it is sold complies with the specifications for that drug. Also included are data generated as part of the continuing stability program.
1.5
For each lot of drug in dosage form, there is adequate evidence of compliance with finished product specifications.
The following documents are maintained by the fabricator, packager/labeller, distributor, wholesaler, and importer of a drug as they relate to all operations in Canada: 2.1 Distribution records of all sales of drugs, including those of professional samples. 2.1.1 Records of all sales are retained or are kept readily accessible in a manner that will permit a complete and rapid recall of any lot or batch of a drug. This requirement need not necessarily involve tracking by lot number. Records to indicate that all customers who have received a recalled drug have been notified.
2.1.2
2.2
Records of the results of the self-inspection program, evaluation, and conclusions, and corrective measures implemented.
The following documents are maintained by every fabricator, packager/labeller, wholesaler, distributor, and importer of a drug: 3.1 Records of complaints or other information received relating to quality, deficiencies or hazards of a drug and of subsequent investigations of complaints, including corrective actions taken. Records concerning information received respecting the quality or hazards of a drug.
3.2
The following documents are maintained by the fabricator: 4.1 4.2 4.3 4.4 4.5 the written specifications for the raw materials; the results of the raw material testing; the sources of the raw materials supplied; records on the operation of the sanitation program required by Regulation C.02.007; and detailed plans and specifications of each building where fabrication occurs, including a description of the design and construction.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 64
Health Canada / Health Products and Food Branch Inspectorate
2083 2084 2085 2086 2087 2088 2089 2090 2091 2092 2093 2094 2095 2096 2097
5.
The following documents are maintained by the person who packages or labels a drug: 5.1 5.2 5.3 5.4 the written specifications for the packaging materials; the results of the packaging material examinations or testing; the sources of the packaging materials supplied; and records on the operation of the sanitation program required by Regulation C.02.007.
6.
Every fabricator, packager/labeller, and tester maintains 6.1 Details of the personnel employed to supervise the fabrication, packaging/labelling, and testing, including organization charts; each persons title, job description, responsibilities, qualifications, experience, and training; and the name(s) of each persons designated alternate(s).
7.
Records required under Regulations C.02.021(1), C.02.022, and C.02.023 are retained for a period of at least one year past the expiration date of the drug to which the records apply. 7.1 For medical gases, which do not require an expiration date, records required under Regulations C.02.021(1), C.02.022, and C.02.023 are retained for a period of at least five years from the date of fabrication of the drug.
2098 2099 2100 2101 2102 2103 2104 2105 2106 2107 2108 2109 2110 2111 2112
SAMPLES
REGULATION C.02.025 (1) Every distributor referred to in paragraph C.01A.003(b) and importer of a drug shall retain in Canada a sample of each lot or batch of the packaged/labelled drug for a period of at least one year after the expiration date on the label of the drug unless otherwise specified in the distributor's or importer's establishment licence. The fabricator shall retain a sample of each lot or batch of raw materials used in the fabrication of a drug for a period of at least two years after the materials were last used in the fabrication of the drug unless otherwise specified in the fabricator's establishment licence the fabricators establishment licence specifies otherwise.
(2)
C.02.026 The samples referred to in section C.02.025 shall be in an amount that is sufficient to determine whether the drug or raw material complies with the specifications for that drug or raw material. RATIONALE
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 65
Health Canada / Health Products and Food Branch Inspectorate
2113 2114 2115 2116 2117 2118 2119 2120 2121 2122 2123 2124 2125 2126 2127 2128 2129 2130 2131 2132 2133 2134 2135 2136 2137 2138 2139 2140 2141 2142 2143 2144 2145 2146
These requirements help ensure that responsible officials at fabricating, distributing, or importing establishments the establishment and at Health Canada have ready access to those samples that are essential for re-examination should a product quality concern arise. INTERPRETATION 1. A sample of each lot or batch of a packaged drug finished product is retained in Canada by the distributor referred to in paragraph C.01A.003(b) or and by the importer of the drug. 1.1 The sample is retained in its trade package, or in a container of the same material and construction, or in a container that is equivalent with respect to stability. In the case of large containers of finished products, a smaller representative sample may be substituted. retained, as supported by stability data. This allowance does not apply to sterile products hermetically sealed containers. The sample is stored under the conditions indicated on the label. Retention samples are maintained in accordance with a written procedure.
1.2 1.3 2.
A sample of each lot or batch of a raw material (including both active and inactive ingredients), is retained by the fabricator of the drug. 2.1 The sample is stored in the same packaging system in which the raw material is stored or in one that is equivalent to or more protective than the vendors marketed packaging system of the raw material. The sample is stored under the conditions indicated in the specifications. recommended by the vendor. Retention samples are maintained in accordance with a written procedure.
2.2
2.3 3.
In determining the size of sample to be maintained, it is to be kept in mind that Health Canada needs at least enough of the material to carry out tests to determine whether the drug or the raw material complies with its specifications. The fabricator, distributor, or importer may also wish to test the material in the event of a complaint; the sample should therefore be at least double the amount needed to complete all required tests. This requirement is not considered to be applicable to the number of units normally required for sterility and pyrogen (endotoxin) testing, or to water, solvents, and medical gases. Health Canada will consider alternate sample retention procedures for distributors and importers as referred to in sub-section C.02.025(1) if a product specific request is submitted as outlined in AnnexAppendix B to these guidelines. This product specific request canshould be submitted annually with an establishment licence application, amendment, or notification, or renewal. The establishment licence for the distributor or the importer may be modified with respect to sample retention of specific products where
4.
5.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 66
Health Canada / Health Products and Food Branch Inspectorate
2147 2148 2149 2150 2151 2152 2153 2154 2155 2156 2157 2158 2159 2160 2161 2162 2163 2164 2165 2166 2167 2168 2169 2170 2171 2172 2173 2174 2175 2176 2177 2178 2179 2180 2181 2182
the fabricator of the product has committed to retaining the sample using the same container-closure system as the one made a commitment to retain the sample in equivalent packaging to that used for the drug marketed in Canada; or the information supplied by the applicant supports a shorter retention period than that required under Regulation C.02.025. The application demonstrates that the product meets one or more of the following criteria: 5.1.1. Testing of the drug requires specialized product-specific methodology that is not available in Canada The drug is subject to Health Canadas lot release program. There is a limited volume of the drug sold in Canada due to the indications for use (e.g, orphan-like drugs) There is a limited quantity of the drug available to the Canadian market (e.g., small portions of many batches) Individual samples of the drug are very expensive. The number of samples to be retained (e.g., high volume) is not an acceptable factor. Perishable drugs that have expiration dates based solely on the shelf life of the food ingredients, not on the stability of the active drug ingredient (e.g., juices with added calcium or vitamins). Radiopharmaceuticals. The following non-prescription drugs (see Category IV product monographs): Acne therapies (topical) Anticaries products containing fluoride Antidandruff products Antiperspirants Antiseptic skin cleansers Athletes foot treatments Medicated skin-care products Sunburn protectants Hard-surface disinfectants
5.1
5.1.2. 5.1.3.
5.1.4.
5.1.5.
5.1.6.
5.1.7. 5.1.8. 5.1.9 5.2.
An alternate sample retention site request or notification provides the following: 5.2.1. evidence that sufficient numbers of samples of lots sold in Canada will be maintained to allow access to those samples by all pertinent regulatory authorities, including Health Canada; and a commitment to provided provide samples within 48 hours of receiving a request from Health Canada.
Page 67
5.2.2.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
2183 2184
5.3.
Should circumstances change regarding any of the above criteria, the applicant must inform Health Canada so that the alternate means may be reassessed..
2185 2186 2187 2188 2189 2190 2191 2192 2193 2194 2195 2196 2197 2198 2199 2200 2201 2202 2203 2204 2205 2206 2207 2208 2209 2210 2211 2212 2213 2214 2215 2216 2217
STABILITY
REGULATION C.02.027 Every distributor referred to in paragraph C.01A.003(b) and importer shall establish the period of time during which each drug in the package in which it is sold will comply with the specifications. RATIONALE The purpose of the written stability program is to ascertain the normal shelf life of the products that is to determine how long the products can be expected to remain within specifications under recommended storage conditions. The requirements for the formal stability studies (primary and commitment batches) are outlined in the various Health Canada, and ICH Guidelines, and Veterinary International Conference on Harmonisation (VICH) Guidelines. Each packaged dosage form must be covered by a sufficient amount of data to support its asserted shelf life in its trade package. INTERPRETATION 1. The stability of the drug is determined prior to marketing and prior to adoption of significant changes in formulation, fabrication procedures, or packaging materials that may affect the shelf life of the drug. This determination is made in accordance with ICH guidelines, which include conditions for storage of stability samples. 1.1 Accelerated stability data are considered to be preliminary information only. The accelerated data are supported by long term testing. When the assignment shelf-life is assigned of the expiry date is based on accelerated data and extrapolated the long-term testing data, it should be verified by additional long term stability data as these data become available. Stability studies are carried out on the drug in each package type in which it is to be sold in Canada. For new chemical entities, at least three primary lots batches of each strength are sampled for the development of shelf life data, unless such data are submitted as a part of the application for marketing approval. For existing chemical entities (e.g., generic drugs), two lots of each strength are sampled. The principle of bracketing and matrixing designs may be applied if justified. For imported products, stability data studies originating from foreign fabricators sites are acceptable provided that the data meet the requirements of the various Health Canada and ICH guidelines regarding stability and that the site can demonstrate GMP compliance. The data provide evidence that the drug product is not affected by transportation.
Page 68
1.2
1.3
1.4
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
2218 2219 2220 2221 2222 2223 2224 2225 2226 2227 2228 2229 2230 2231 2232 2233 2234 2235 2236 2237 2238 2239 2240 2241 2242 2243 2244 2245 2246 2247 2248 2249 2250 2251 2252 2253 2254
1.5 1.6
The shelf life is established from based on the date of fabrication. Stability data are available for drugs that are to be reconstituted or further diluted before and after constitution, reconstitution or dilution, if applicable. Analytical test procedures used in stability evaluation are validated in accordance with the ICH guidelines document entitled ICH Q2(R1): Validation of Analytical Procedures: Text and Methodology. Assays are to be stability-indicating, (i.e.,e.g. sufficiently specific to detect and quantify breakdown degradation products and to distinguish between degraded and non-degraded materials). Limits for individual unidentified specified, individual identified unspecified, and total degradation products are included.
1.7
REGULATION C.02.028 Every distributor referred to in paragraph C.01A.003(b) and importer shall monitor, by means of a continuing program, the stability of the drug in the package in which it is sold. RATIONALE The purpose of the written continuing stability program is to monitor the validity of the product shelf life of the product on an on-going basis. It also serves to determine how long the product can be expected to remain within specifications under recommended storage conditions. Each packaged dosage form must be covered by a sufficient amount of data to support its labelled expiry date in its trade package. Any significant change that may have an impact on the quality of the product should be assessed and may require further stability studies. INTERPRETATION 1. A continuing stability program is implemented to ensure compliance with the approved shelf life specifications. A protocol is available and is implemented for each drug marketed in Canada. A summary of all the data generated, including the evaluation and the conclusions of the study, is prepared. This program includes but is not limited to the following parameters: - number of batch(es) per strength, packaging, and batch sizes, - relevant physical, chemical, microbiological or biological test methods, - tests and acceptance criteria, - container closure system(s), - testing frequency, - storage conditions (and tolerances) of samples, and - other applicable parameters specific to the drug. 1.1 A minimum of one batch of every strength of the drug is enrolled into the continuing stability program each year. The principle of bracketing and matrixing designs may be applied if justified in accordance with ICH guideline Q1A(R).Any differences in the protocol for the continuing stability program and the protocol for the formal stability studies are scientifically justified.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 69
Health Canada / Health Products and Food Branch Inspectorate
2255 2256 2257 2258 2259 2260 2261 2262 2263 2264 2265 2266 2267 2268 2269 2270 2271 2272 2273 2274 2275 2276 2277 2278 2279 2280 2281 2282 2283 2284 2285 2286 2287 2288 2289 2290 2291 2292 2.
1.2
Any differences in the protocol for the continuing stability program and the protocol for the formal stability studies are scientifically justified. A minimum of one batch of every strength of the drug is enrolled into the continuing stability program each year the drug is produced. The principle of bracketing and matrixing designs may be applied if justified in accordance with the ICH document entitled ICH Q1A): Stability Testing of New Drug Substances and Products. Worst case situations should be addressed by the continuing stability program (e.g., inclusion of reworked or reprocessed lots). Any significant change confirmed out of specification result, or significant negative trend that may have an impact on the quality of the product should be assessed and may require further stability studies. For imported products, stability data studies originating from foreign fabricators sites are acceptable, provided that the data meet the requirements of the various Health Canada and ICH guidelines regarding stability and that the site can demonstrate GMP compliance. The data provide evidence that the drug product is not affected by transportation. It is the importers responsibility to obtain and maintain up to date records associated with the ongoing stability program.
1.3
1.4
1.35
Minor changes (e.g., addition, deletion, or substitution of a fragrance, flavour, or colour) to the formulations of certain designated non-prescription drugs may be acceptable without new stability data, provided that the following conditions are met: 2.1 Ongoing stability studies are conducted on the revised formulation to demonstrate that the proposed change does not affect the quality of the drug product. A continuing stability program of stability is conducted concurrently with the marketing of the modified product throughout the shelf life of the product. Minor changes are acceptable for the following non-prescription products (see Category IV product monographs): Acne therapies (topical) Anti-caries products containing fluoride Antidandruff products Antiperspirants Antiseptic skin cleansers Athletes foot treatments Medicated skin-care products Secondary sunburn protectants (e.g., lipstick with SPF)
2.2
2.3
Note: The chart shown on the next page is a guide for selecting parameters to be studied in the stability program. Each product must be examined separately. a) The inclusion of a sterility test in the stability study of a sterile drug may not be necessary if the container closure system has been proven to be hermetic.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 70
Health Canada / Health Products and Food Branch Inspectorate
2293 2294 2295
b)
In addition to preservative content testing, a single regular production batch of the drug is to be tested for antimicrobial preservative effectiveness at the end of the proposed shelf life.
2296 2297
Note: For further information on the requirements of the formal stability studies, see references listed in Annex C of these guidelines.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 71
Health Canada / Health Products and Food Branch Inspectorate
2298 2299
TAB LE TS CAPSU LES L IQ U I DS AND GELS
STABILITY (Ch art to b e us ed a s a gu ide on ly) OINTM ENTS AND CREA MS Assay all active ingredients as w ell as other "elemen ts" outlined below Plus: preserv atives, antioxi dants, and Plus: preserva tives, antiox id ants, and bac terio stats if effective ness not checked under Pu rity section Plus: com ple te testing data on reconst ituted fo rm s Plus: pres erva tiv es, antioxidant s, and bacteriostat s if effectivene ss not checked under Pu rity section Qu antit y delivere d per spray for metered dose product s P O WD ERS INJECTA BLES SUPPOSI TORIES AERO SO LS
2300 2301
POTEN CY
bacteri ostats if effec tiv eness not checke d under Pu rity section
2302 2303 2304 2305
Physica l Charact eristics
Containers: (1) Appearance of inner walls and cap interiors colour (2) Integrity of seals (3) Appearance and adhesion of label
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 72
Health Canada / Health Products and Food Branch Inspectorate
dissolut ion disinteg ration -odour hardnes s -color appeara nce dissolut ion disinteg ration con ditio n of sh ells -color appeara nce -odour visco sit y specifi c gravity -pH -clarity of solutio n prec ipit ation of ingredi ents -nonhom og ene ity of suspen sions hom og ene ity (gels) -odour -texture -pH hom oge neity prec ipit ation of ingre die nts -odour texture -clarity of solutio n hom og ene ity - pH (after reconst itution) pa rtic le size -flow charact eristics (inhalat ion powder s) -clarity -partic ulate matter -pH prec ipitatio n of ingre dien ts -optical rotation -m ultiple dos e vials: product integr ity after initial use -melting point homogen eity -net weight delivery weight delivery pressur e -pH delivery effec tiv eness (e.g. spray pattern and droplet size) num ber of doses or spra ys per packag e Containers: (1) M igration of drug into plastic (2) M igration of plasticisers into drug (3) Corrosion moistur e content moistur e content sterility for ophthal mics -sterility for ophthal mics pa rtic ula te matter for ophthal mics moistur e content -sterility
2306 2307
PU RIT Y
particul ate matter for ophthal mics
Microbial Test De grad ation p rodu cts
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 73
Health Canada / Health Products and Food Branch Inspectorate
2308 2309 2310 2311 2312 2313 2314 2315 2316 2317 2318 2319 2320 2321 2322 2323 2324 2325 2326 2327 2328 2329 2330 2331 2332 2333 2334 2335 2336 2337 2338 2339 2340
STERILE PRODUCTS
REGULATION C.02.029 In addition to the other requirements of this Division, a drug that is intended to be sterile shall be fabricated and packaged/labelled (a) (b) ) in separate and enclosed areas; under the supervision of personnel trained in microbiology; and by a method scientifically proven to ensure sterility.
RATIONALE Sterile drugs are susceptible to particulate, pyrogenic and microbiological contamination. Due to the health hazard associated with the use of contaminated sterile products, special precautions are required in the production of these products. The skill, training, and competency of all personnel involved are critical. Quality assurance is important and the production must follow carefully established and validated methods of preparation and sterilization. INTERPRETATION GENERAL 1. Separate packaging and labelling operations of hermetically sealed containers are not subject to Regulation C.02.029 but are covered under Regulation C.02.011. When designing procedures for achieving sterility, a number of factors must be considered, particularly airborne microorganisms, particulate matter, the size of the opening of the container, the length of time contents are exposed, and assurance that all the material is exposed to the sterilization condition or process. All aqueous-based sterile products are must be subjected to terminal steam sterilization, with the following exceptions: 3.1 Instances where terminal steam sterilization is not practicable (e.g., where the sterilization process would cause product or packaging degradation). The rational for the departure from the standard Such instances are is fully evaluated and documented. Aseptic processes that exclude human intervention (e.g., robotics, form-fill-seal, and barrier systems) may be employed in lieu of terminal sterilization, provided that the data developed demonstrate equivalent an acceptable level of sterility assurance. Any such methods introduced are fully validated, taking into account all critical factors of the technology used as well as the routine monitoring to be carried out.
2.
3.
3.2
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 74
Health Canada / Health Products and Food Branch Inspectorate
2341 2342 2343 2344 2345 2346 2347 2348 2349 2350 2351 2352 2353 2354 2355 2356 2357 2358 2359 2360 2361 2362 2363 2364 2365 2366 2367 2368 2369 2370 2371 2372 2373 2374 2375
4.
Environmental g Grade requirements and monitoring: Drugs subject to terminal sterilization: 4.1 Formulation takes place in an environmental where a minimum of Grade C conditions is maintained, provided that the formulated bulk is immediately subjected to its subsequent processing step, (e.g., filtration, sterilization), in order to minimize bio-burden and particulates. Formulation may take place in a Grade D environment if additional measures (e.g., the use of closed systems of manufacture) are taken to minimize contamination. Parenterals are filled in an aseptic area with at least a Grade B environment or in a Grade A zone with at least a Grade C background, before terminal sterilization. 4.3.1 Parenterals that are to be terminally sterilized may be filled in a Grade C area if the process or product does not pose a high-risk of microbial contamination. Examples of high-risk situations include slow filling operations, the use of wide-necked containers, or the exposure of filled containers to the environment for more than a few seconds before sealing.
4.2
4.3
4.4
Non-parenterals may be filled in a Grade C environment before terminal sterilization.
Drugs not subject to terminal sterilization: 4.5 Parenterals sterilized by filtration, are formulated in an environment where a minimum of a Grade C conditions is maintained. Non-parenteral products may be formulated in a Grade D environment if additional measures are taken to minimize contamination, such as the use of closed systems. Sterile filtration requires a minimum filter rating of 0.22 m. The integrity of the filter is verified before and after use by an appropriate method such as a bubble point, diffusion or pressure hold tests. Filling operations are performed under local Grade A conditions within a Grade B background environment. However a lower-grade background environment may be acceptable if specialized automated or barrier techniques are employed and if those techniques are validated to demonstrate that their use has no negative impact on the quality of the drug.
4.6
4.7
4.8
Drugs not subject to filtration or terminal sterilization: 4.9 Sterile products subject to neither filtration nor terminal sterilization, are produced from sterile raw materials and packaging components in an aseptic area under local Grade A conditions with a Grade B background. Additional information pertaining to blow-fill-seal and isolator technology is provided in interpretations 82 and 82 under the Sterile Products section.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 75
Health Canada / Health Products and Food Branch Inspectorate
2376 2377 2378 2379 2380 2381 2382 2383 2384 2385 2386 2387 2388 2389 2390 2391 2392 2393 2394 2395 2396 2397 2398 2399 2400
5.
The air standards described in the following tables are to be achieved throughout the area when it is occupied and in operation. In the operational condition for Grade A zone, the air standards apply in the zone immediately surrounding the drug whenever it is exposed, and with at least a Grade B background. It may not always be possible to demonstrate conformity with air standards for non-viable particulates at the point of fill when filling is in progress, owing to the generation of particles or droplets by the product itself. 5.1 The at rest state is the condition where the installation is complete, including fabrication equipment installed and present in an operational condition but not in use and with operating personnel absent. The in operation state should not commence until all the predefined criteria have been met with the equipment and personnel in place.
6.
The classification of aseptic and clean areas is based on environmental results obtained using acceptable standardized air sampling methods. Such methods take into account the volume and number of samples taken at each location and the total number of sampling locations. The number of sampling locations is based on room volume and on the nature of the operations being undertaken. Sampling methods used during the operational state do not interfere with zone protection. Radiation sterilization is used mainly for heat-sensitive materials. Since drugs and packaging materials are radiation-sensitive, this method is permissible only when, prior to use, evidence has confirmed the absence of any damaging effects on the material. Ethylene Oxide sterilization is used only when other methods are not practicable. Evidence must be available to show the absence of any damaging effect on the drug when this method is used. The conditions and time allowed for degassing the drug are such that residual gas and reaction products are reduced to clearly defined acceptable limits. Ultraviolet irradiation is not an acceptable method of sterilization.
7.
8.
9.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 76
Health Canada / Health Products and Food Branch Inspectorate
2401 2402
BASIC ENVIRONMENTAL STANDARDS FOR THE MANUFACTURE OF STERILE PRODUCTS
The airborne particulate classification is given in the following table:
at rest (5) in operation
2403
Grade 0.5 m
Maximum permitted number of particles / m 3 equal to or above (3) 5 m 1 (6) 1 (6) 2,000 20,000 0.5 m 3,500 350,000 3,500,000 not defined (4) 5 m 1 (6) 2,000 20,000 not defined (4)
2404 2405 2406 2407 2408 2409 2410 2411 2412 2413 2414 2415 2416 2417 2418 2419 2420 2421 2422 2423 2424 Notes:
1.
A (1) B (2) C (2) D (2)
3,500 3,500 350,000 3,500,000
Unidirectional (laminar) airflow systems provide a homogeneous air speed of 0.45 m/s meters/ second +/- 20% (guidance value) at the working position in open clean room applications. Precise air speeds will depend on the type of equipment. The maintenance of laminarity should be demonstrated and validated. A uni-directional air flow and lower velocities may be used in closed isolators and glove boxes. In order to attain air Grades B, C, and D, the number of air changes will be related to the size of the area and to the equipment and personnel present in the area. Low values for contaminants are reliable only when a large number of air samples are taken. Adequate data is available to generate confidence that the required conditions are met throughout the duration of the operations. The requirement and limits for this area will depend on the nature of the operations carried out. The particulate conditions given in the at rest column are to be achieved after a short clean-up period (15 to 20 minutes) after the operation has been completed. in an unmanned state after completion of operations. It is expected to get these areas completely free from particles sized equal or greater than 5 :m. As it is impossible to demonstrate absence of particles with any statistical significance the limits are set to 1 particle / m3. During the qualification of classified rooms it should be shown that the areas could be maintained within the defined limits. Recommended limits for microbial contamination (a) (e) GRADE air sample cfu/m3 settle plates (diameter 90mm), cfu/4 hours (b) <1 5 50 100 contact plates (diameter 55 mm), cfu/plate ( c) <1 5 25 50 glove print (5 fingers) cfu/glove (d) <1 5 -
2.
3.
4. 5.
6.
2425 2426 2427 2428 2429
Notes:
A B C D
<1 10 100 200
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 77
Health Canada / Health Products and Food Branch Inspectorate
2430 2431 2432 2433 2434 2435 2436 2437 2438 2439 2440 2441 2442 2443 2444 2445 2446 2447 2448 2449 2450 2451 2452 2453 2454 2455 2456 2457 2458 2459 2460 2461 2462
(a)
These are average values; however, averaging of results can mask unacceptable localized conditions, therefore individual excursions should be treated with caution. For a Grade A area, no individual result should exceed 3 cfu without investigation given that the samples from Grade A critical area environments should normally yield no microbial contaminants. Individual settle plates may be exposed for less than 4 hours. The surface sampled with a contact plate is subject to appropriate cleaning immediately after use. Monitoring is conducted after critical operations are complete. All indicated sampling methods are required unless alternative methods demonstrate equivalency.
(b) ( c) (d) (e)
PREMISES 10. To the extent possible, premises are designed to avoid the unnecessary entry of supervisory or control personnel. Grade B areas are designed so that all critical operations can be observed from outside. To prevent the shedding or accumulation of dust and other particulate matter, ceilings, floors, and walls in aseptic areas, and floors and walls in clean areas, have smooth impervious surfaces that permit the repeated application of cleaning and disinfecting agents. To reduce the accumulation of dust and to facilitate cleaning, projecting ledges or shelves and electrical and mechanical equipment are kept to a minimum. Covings are required where walls meet floors or ceilings. Walls, floors, and ceilings form an effective seal around any traversing pipe or duct. False ceilings are sealed to prevent contamination from the space above them. Uncleanable devices, such as certain sliding-door rails, are avoided. Where required, sinks and drains are designed, located, and maintained so as to minimize risks of microbial contamination. Sinks and drains are excluded from areas where aseptic operations are carried out. Hand-washing facilities are provided only in changing rooms. Changing rooms are designed as airlocks and are used to separate the different stages of changing, thus minimizing microbial and particulate contamination of protective clothing. They are effectively flushed with filtered air. In the final stage, they are, at rest, the same grade as the area into which they lead. Access to the clean and aseptic areas is provided only through air-locks. Doors to airlocks are arranged so that, either by design or by procedure, only one side or door may be opened at one time (except for emergencies).
2.11
3.12
4.13 5.14 6.15
7.16 8.17
9.18
10.19 The air for clean and aseptic areas is supplied through filters of suitable efficiency. Laminar unidirectional air flow systems are of appropriate design.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 78
Health Canada / Health Products and Food Branch Inspectorate
2463 2464 2465 2466 2467 2468 2469 2470 2471 2472 2473 2474 2475 2476 2477 2478 2479 2480 2481 2482 2483 2484 2485 2486 2487 2488 2489 2490 2491 2492 2493 2494 2495 2496 2497 2498 2499 2500 2501 2502
11.20 The filtered air supply for clean and aseptic areas is designed to provide a fabrication environment that meets the required grade classifications. Under all operational conditions, a positive pressure of filtered airflow is maintained in relation to surrounding areas of a lower grade. Particular attention is paid to protecting the zone of greatest risk critical areas, that is, the immediate environment to in which the sterilized drug product, containers, and closures and the treated components are exposed. 20.1 The air system should be provided with appropriate terminal filters such as HEPA for Grades A, B and C. An intact HEPA filter should be capable of retaining at least 99.97% of particulates greater than 0.3 m in diameter. In Grade A areas the air velocity should be sufficient to protect exposed product, product contact components and product contact surfaces from environmental contamination, by sweeping particles away from the filling/ closing area and maintain a unidirectional airflow during operations. Air velocity measurements should be taken at locations where meaningful and reproducible results can be obtained. Such locations should normally be not more than 1 foot away from the work site, within the air flow. The particle counting probe should be placed in the orientation demonstrated to obtain a meaningful sample. Regular particulate monitoring should be performed during each production shift. In critical areas HEPA filters should be leak tested at least twice a year. The purpose of performing regularly scheduled leak tests is to detect leaks from the filter media, filter frame or seal. The aerosol selected for HEPA leak testing should not support microbial growth and should be composed of a sufficient number of particles at approximately 0.3 m. HEPA filtered air should be supplied in critical areas at a velocity sufficient to sweep particles away from the filling/ closing area and maintaining a unidirectional airflow. In situ air pattern analysis should be conducted at the critical area to demonstrate unidirectional air flow, sweeping action over and away from the product, and the absence of turbulence or eddy currents. For aseptically filled products, the transportation and loading of partially sealed containers, such as between filling and lyophilization, should be under Grade A conditions.
20.2
20.3
20.4
20.5
12.21 Warning systems alert personnel when air pressure or airflow falls below established limits. Pressure differentials between areas are monitored and recorded where such differences are of importance. 21.1 Pressure differentials between 10 and 15 Pa (0.10 cm and 0.15 cm or 0.04" and 0.06" of water) are considered effective between zones of different environmental classifications. Pressure differentials between aseptic areas and adjacent areas should be monitored continuously and documented. All alarms should be documented and deviations from established limits should be investigated. When doors are open, outward air flow should be sufficient to minimize ingress of contamination. It is critical that the time the door can remain ajar be strictly controlled.
21.2
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 79
Health Canada / Health Products and Food Branch Inspectorate
2503 2504 2505 2506 2507 2508 2509 2510 2511 2512 2513 2514 2515 2516 2517 2518 2519 2520 2521 2522 2523 2524 2525 2526 2527 2528 2529 2530 2531 2532 2533 2534 2535 2536 2537
13.22 Airflow patterns do not present a contamination risk. For example, care is taken to ensure that airflows do not distribute particles from a particle-generating person, operation, or machine to a zone of higher product risk. 14.23 All work with microorganisms and other infectious agents known to require special precautions in manipulation is safely segregated. EQUIPMENT 1.24 Equipment is designed in such a way as to facilitate cleaning, disinfection, or sterilization. Electronic accessories and those parts of large equipment that are not readily amenable to such treatment are appropriately and adequately sealed or effectively isolated. To the extent possible, equipment fittings and services are designed and installed so that operations, maintenance, and repairs can take place outside clean or aseptic areas. When equipment maintenance is carried out within clean or aseptic areas during operations, clean sterilized instruments and tools are used. If the required standards of cleanliness and/or asepsis are not maintained during the maintenance work, the area is cleaned and disinfected before processing recommences. All equipment, including sterilizers, air-filtration systems, and water-treatment systems, are subject to planned maintenance, validation, and monitoring. Following maintenance/validation, the approval for use of the equipment is documented. For aseptically filled products, conveyor belts do not pass through a partition from a Grade A or grade B area to an area of lower cleanliness unless the belts are continuously sterilized (e.g., they pass through a sterilizing tunnel). Vent filters used on equipment directly involved in aseptic filling such as receiving tanks, transfer lines, and surge vessels should be integrity tested upon installation where practical or prior to installation and after batch completion. Vent filters used on stationary equipment such as WFI storage tanks and sterilizers, and membrane filters used to filter compressed gases, should be integrity tested prior to installation and periodically thereafter. Integrity test failures should be investigated. Filters should be replaced according to written criteria at appropriate, predefined intervals, and documented. All critical surfaces that come in direct contact with sterile materials should be sterile.
2.25
3.26
4.27
5.28
29.
30.
31.
32.
WATER TREATMENT SYSTEMS 1.33 Water treatment facilities are designed, constructed, and maintained so as to ensure the reliable production of water of an appropriate quality. They are not operated beyond their designed capacity. Water is produced, stored, and distributed in a manner that minimizes microbial growth and prevents other types of contamination.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 80
Health Canada / Health Products and Food Branch Inspectorate
2538 2539 2540 2541 2542 2543 2544 2545 2546 2547 2548 2549 2550 2551 2552 2553 2554 2555 2556 2557 2558 2559 2560 2561 2562 2563 2564 2565 2566 2567 2568 2569 2570
2.34
The quality of the raw feed water is established by specification and is periodically monitored for compliance. The sampling plan takes seasonal variations into account. Records are maintained. Purified water is used as feed water for Water for Injection (WFI) systems and for clean steam generators. WFI is produced either by distillation or by reverse osmosis. WFI is used in the formulation of parenteral, irrigation, and intra-ocular products. Purified water may be used in the formulation of ophthalmic products. WFI should be used in the direct cooling (or heating) of filled drug product containers (e.g. for the cool down cycle of sterilization loads). Purified Water may be used as cooling water provided that it consistently meets the microbiological and endotoxin levels as established for WFI. Purified water and WFI systems are validated that is, the ability of the systems and its procedures to maintain the appropriate level of chemical and microbial control, taking seasonal variations into account, is demonstrated and documented. Alert and action levels should be established for bacterial endotoxins and microbial load. These limits should meet any standard listed under Schedule B to the Food and Drugs Act. WFI storage tanks are equipped with hydrophobic bacterial-retentive vent filters. Sanitization or regeneration of water systems is carried out according to a predetermined schedule and also whenever established microbial counts are exceeded within any of the system's components. Consideration is given to controlling biofilm formation. The WFI system is maintained at an elevated temperature and kept in continuous movement. Water velocity through pipes is sufficient to prevent microbial attachment.
3.35
4.36
37.
538.
639.
740. 841.
942.
1043. Piping is sloped to provide for complete drainage of the system. The system is free of dead legs. 1144. All metal surfaces in contact with WFI should be, as a minimum, 316 stainless steel, and should be passivated upon or prior to installation and after changes. 1245. While in use during processing, WFI is sampled daily from at least two points of use on a rotating basis so as to cover all outlets. 1346. Revalidation of water systems is required if any of the following situations arise: 1346.1 Unscheduled or extensive maintenance is performed on the system. 1346.2 New or revised sections or components are added to or removed from the system. 1346.3 The system exhibits an out-of-control trend in either chemical or microbiological parameters. 1447. The extent of the re-validation work necessary is determined jointly by the personnel from the quality control, engineering, production, and any other appropriate departments. A pre-approved protocol is signed and dated by the parties involved.
Page 81
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
2571 2572
Note: Refer to Interpretations 11 and 12 under Manufacturing Control 75 and 76 in the Sterile Products section for further requirements regarding water to be used in fabrication.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 82
Health Canada / Health Products and Food Branch Inspectorate
2573 2574 2575 2576 2577 2578 2579 2580 2581 2582 2583 2584 2585 2586 2587 2588 2589 2590 2591 2592 2593 2594 2595 2596 2597 2598 2599 2600 2601 2602 2603 2604 2605 2606 2607 2608 2609 2610
PERSONNEL 1.48 In addition to the requirements outlined under Regulation C.02.006, the personnel responsible for the fabrication and testing of sterile products have had training in microbiology. High standards of personal hygiene and cleanliness are maintained. Personnel involved in the fabrication of sterile preparations are instructed to report any condition that may cause the shedding of abnormal numbers or types of contaminants. Periodic health checks for such conditions are conducted, and appropriate action (e.g., deciding whether to allow an individual to be involved in a particular operation) is taken by designated qualified personnel when necessary. All personnel (including those whose duties involve cleaning and maintenance) employed in such areas receive regular training in disciplines relevant to the correct fabrication of sterile products, including reference to hygiene and to the basic elements of microbiology. When outside personnel who have not received such training (e.g., building or maintenance contractors) need to be brought in, particular care is taken with regard to their supervision. Personnel who have been engaged in the processing of animal-tissue materials or of cultures of microorganisms other than those used in the current fabrication process do not enter areas where sterile products are fabricated unless rigorous and clearly defined decontamination procedures have been followed. Only the minimum number of personnel required are present in areas where sterile products are fabricated; this is particularly important during aseptic processes. Inspections and controls are conducted from outside such areas to the extent that such an approach is possible. Outdoor clothing is not brought into these areas. Personnel entering the changing rooms are already clad in standard protective garments designed for factory facilities. Changing and washing follow written procedures. The clothing worn by personnel and its quality are adapted to the particular process and workplace, and the clothing is worn in such a way as to protect the product from contamination. Clothing is appropriate to the air environmental grade of the area where the personnel will be working. Written gowning procedures must be established for each environmental grade. Personnel must be trained according to these procedures prior to entry. Such training must be documented. Descriptions of the clothing required for each grade are given below. For Grade A and B areas: Headgear totally encloses the persons hair, as well as any beard or mustache, the headgear is tucked into the neck of the suit; a face mask is worn to prevent the shedding of droplets; sterilized non-powdered rubber or plastic gloves and sterilized or disinfected footwear are worn; trouserbottoms are tucked inside the footwear and garment sleeves are tucked into the gloves. The protective clothing sheds virtually no fibres or particulate matter and retains particles shed by the body.
2.49
3.50
4.51
5.52
6.53
7.54
8.55
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 83
Health Canada / Health Products and Food Branch Inspectorate
2611 2612 2613 2614 2615 2616 2617 2618 2619 2620 2621 2622 2623 2624 2625 2626 2627 2628 2629 2630 2631 2632 2633 2634 2635 2636 2637 2638 2639 2640 2641 2642 2643 2644 2645 2646 9.56
For Grade C areas: The persons hair, as well as any beard or mustache, is covered. A one- or two-piece trouser suit, gathered at the wrists and with a high neck, and appropriate shoes or overshoes are worn. The protective clothing sheds virtually no fibres or particulate matter. For Grade D areas: The persons hair, as well as any beard or mustache, is covered. Protective clothing and appropriate shoes or overshoes are worn. For every worker in an aseptic Grade B area, clean sterilized protective garments are provided at each re-entry and or at least once a day if monitoring results justify it. Gloves are regularly disinfected during operations. Masks and gloves are changed prior to every new working session.
10.57 Clothing used in clean and aseptic areas is laundered or cleaned in such a way that it does not gather additional particulate contaminants that can later be shed. Separate laundry facilities for such clothing are desirable. If fibres are damaged by inappropriate cleaning or sterilization, there may be an increased risk of shedding particles. Washing and sterilization operations follow standard operating procedures. Repair of clothing is carried out using appropriate materials (e.g., non-shedding thread). 58. Behavioural techniques aimed at maintaining sterility should be employed by personnel working in aseptic areas. These include: 58.1 58.2 58.3 moving slowly and deliberately keeping the entire body out of the path of unidirectional airflow approaching any manipulation in a manner that does not compromise sterility of the product maintaining proper gown control
58.4
SANITATION 1.59 Walls, floors, ceilings, and equipment in clean areas are cleaned and, when required, disinfected in accordance with a written procedure. This procedure differentiates between procedures that are followed daily and those that are undertaken whenever fabrication of a different drug is about to begin. Walls, floors, ceilings, and equipment in aseptic areas are cleaned and, when required disinfected in accordance with a written procedure. This procedure differentiates between the cleaning and disinfection procedures that are followed daily and those that are undertaken whenever fabrication of a different drug is about to begin. Where disinfectants are used, it is recommended that more than one type be employed. Disinfectants and cleaning agents to be used in aseptic processing areas should be sterile. 61.1 A disinfectant program should also include a sporicidal agent since many common disinfectants are ineffective against spores.
Page 84
2.60
3. 61.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
2647 2648 2649 2650 2651 2652 2653 2654 2655 2656 2657 2658 2659 2660 2661
4.62
Disinfectants and detergents cleaning agents are monitored for microbial contamination and are sterile when used in Grade A or grade B areas. Dilutions are kept in previously cleaned and sterilized containers and are not stored for long periods unless sterilized. Partly emptied containers are not topped up. Fumigation of clean and aseptic areas may be useful for reducing microbiological contamination in inaccessible places. During operations, clean and aseptic areas, are monitored at planned intervals for particulate and microbial counts of air and surfaces. Where aseptic operations are performed, monitoring is conducted frequently to ensure that environmental specifications are met. The results of such monitoring are considered when batches are assessed for approval. Additional monitoring is desirable even when no production operations are taking place (e.g., after validation of systems, cleaning, and fumigation). The cleaning procedures are validated, and the disinfection procedures are monitored. 64.1 The suitability, efficacy and limitations of disinfecting agents and procedures should be assessed including their ability to adequately remove potential contaminants from surfaces.
5.63
6.
764.
2662 2663 2664 2665 2666 2667 2668 2669 2670 2671 2672 2673 2674 2675 2676 2677 2678 2679 2680 2681 2682
MANUFACTURING CONTROL 1.65 2.66 During all processing stages, precautions are taken to minimize contamination. Preparations containing live microorganisms are neither made nor transferred into containers in areas used for the processing of other pharmaceutical products. Preparations containing only dead organisms or bacterial extracts may be dispensed into containers, in the same premises as other sterile pharmaceutical products, provided that validated inactivation procedures and validated cleaning procedures are followed. Activities in these areas are kept to a minimum, especially when aseptic operations are performed. The movement of personnel is controlled and methodical in order to avoid excessive shedding of particles and organisms. The ambient temperature and humidity are controlled and monitored to ensure the comfort of personnel. Prior to sterilization, possibilities for microbiological contamination of raw materials and packaging materials are kept to a minimum. Specifications include requirements for microbiological quality when monitoring has indicated the need for such requirements. Articles are sterilized and passed into the aseptic areas by the use of doubled-ended sterilizers equipped with interlocking doors or by another validated method. Written standards are available specifying the air quality, including microbiological and particulate viable and non viable matter counts, to be maintained in clean and aseptic areas. Microbiological and particulate Viable and non viable counts are taken at least once a day per shift in aseptic areas, while aseptic filling and aseptic fabrication operations are carried out, and at appropriate intervals in areas where other fabrication takes place.
3.67
4.68
5.69
6.70
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 85
Health Canada / Health Products and Food Branch Inspectorate
2683 2684 2685 2686 2687 2688 2689 2690 2691 2692 2693 2694 2695 2696 2697 2698 2699 2700 2701 2702 2703 2704 2705 2706 2707 2708 2709 2710 2711 2712 2713 2714 2715 2716 2717 2718 2719 2720 7.71
70.1
Air monitoring of critical areas, Grade A environments should normally yield no microbiological contaminants. Contamination in a critical area should be investigated and corrective actions implemented. In Grade A and B areas regular monitoring for particulates and viables should be performed during each operating shift. In Grade C areas monitoring for particulates and viables should be performed at least twice per week. The total sample volume should not be less than 1 cubic meter per sample. Monitoring frequency is justified based on the criticality of the operations, and historical data for the specified area. Personnel working in aseptic processing areas should be microbiologically monitored once per shift. Typical monitoring sites should include operators gloves and one gown site. Manual aseptic production processes require more aggressive personnel monitoring than automated aseptic production processes.
70.2
70.3
The presence of containers and materials liable to generate fibres is minimized in clean and aseptic areas. Following cleaning and sterilization, components, bulk-product containers, and equipment are handled in such a way that they are not re-contaminated. The stage of processing of components, bulk-product containers, and equipment is properly identified. The interval between cleaning and sterilization of components, bulk-product containers, and equipment, as well as between their sterilization and use, is as short as possible and subject to a time-limit appropriate to the validated storage conditions.
8.72
9.73
10.74 The time between the start of the preparation of a solution and its sterilization or filtration through a bacteria-retentive filter is as short as possible. A maximum permissible time is validated for each product, taking into account its composition and the prescribed method of storage. 11.75 Water used in the preparation of parenterals is tested for endotoxins and complies with its approved specifications. 12.76 Water used for the final rinsing of container components that are used for parenteral drugs is tested for endotoxins unless such components are depyrogenated subsequently. 13.77 Any gas that is used to purge a solution or to blanket a product passes through a sterilizing filter. Compressed air and gases that come in direct contact with the product/container primary surfaces must be of appropriate chemical, particulate and microbiological purity, free from oil, and must be filtered through a sterilizing filter at the point of use. 14.78 The microbiological contamination of products (bioburden) is minimal prior to sterilization. The maximum acceptable bioburden is established on a product by product basis, and should be founded on adequate product/process design and control. Acceptable bioburden levels are further demonstrated through the execution of validation studies. This limit is related to the efficiency of the method to be used and to the risk of pyrogens (endotoxins), which are not removed by sterilization. The bioburden should be monitored before sterilization. All solutions, particularly large-volume parenterals, are passed through a bacteria-retentive filter; if possible, this filtering
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 86
Health Canada / Health Products and Food Branch Inspectorate
2721 2722 2723 2724 2725 2726 2727 2728 2729 2730 2731 2732 2733 2734 2735 2736 2737 2738 2739 2740 2741 2742 2743 2744 2745 2746 2747 2748 2749 2750 2751 2752
occurs immediately before the filling process. Where aqueous solutions are held in sealed vessels, any pressure-release outlets are protected (e.g., by hydrophobic microbial air filters). 15.79 Documented evidence that establishes the validation and validity of each sterilization process is available. The validation and validity of the sterilization process are verified at scheduled intervals, at least annually, and also whenever significant modifications or changes are made to the equipment. Loading patterns for all sterilization processes are established and validated. 1579.1 Sterilization by heat Chemicals or biological indicators may also be used, but should not take the place of physical measurements. 1579.1.1 Sufficient time is allowed for the whole load to reach the required temperature before measurement of the sterilizing time-period begins. This time is determined for each type of load to be processed. After the high-temperature phase of a heat sterilization cycle, precautions are taken to prevent contamination of a sterilized load during cooling.
1579.1.2
1579.2 Sterilization by moist heat 1579.2.1 Both temperature and pressure controls are used to monitor the process. Control instrumentation is independent from both monitoring instrumentation and recording charts. Where automated controls and monitoring systems are used for these applications, they are fully validated to ensure that the critical process requirements are met. System and cycle faults are registered by the system and observed by the operator. The reading of the independent temperature indicator is periodically monitored. For sterilizers fitted with a drain at the bottom of the chamber, it may also be necessary to record the temperature at this position throughout the sterilization period. There are frequent leak tests on the chamber when a vacuum phase is part of the cycle. The items to be sterilized, other than products in sealed containers, are wrapped, if necessary, in a material that allows the removal of air and the penetration of steam but that prevents re-contamination after sterilization. All parts of the load are in contact with the sterilizing agent at the required temperature and pressure for the required time. Clean steam is used for sterilization and does not contain additives at a level that could cause contamination of product or equipment.
1579.2.2
1579.2.3
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 87
Health Canada / Health Products and Food Branch Inspectorate
2753 2754 2755 2756 2757 2758 2759 2760 2761 2762 2763 2764 2765 2766 2767 2768 2769 2770 2771 2772 2773 2774 2775 2776 2777 2778 2779 2780 2781 2782 2783 2784 2785 2786 2787
1579.3 Sterilization by dry heat 1579.3.1 The process used includes air circulation within the chamber and the maintenance of a positive pressure to prevent the entry of non-sterile air. Any air admitted passes through a HEPA filter.
1579.4 Sterilization by radiation 1579.4.1 The radiation dose is measured during the sterilization procedure. For this purpose, dosimetry indicators that are independent of dose rate are to be used, giving a quantitative measurement of the dose received by the product itself. Dosimeters are inserted into the load in sufficient number and close enough together to ensure that there is always a dosimeter in the irradiator. Where plastic dosimeters are used, they are within the time limit of their calibration. Dosimeter absorbencies are read within a specified time period after exposure to radiation. Biological indicators may be used as an additional control. Materials handling procedures are designed so as to prevent mix-up between irradiated and non-irradiated materials. Radiation-sensitive colour disks are used on each package to differentiate between packages that have been subjected to irradiation and those that have not. The total radiation dose is administered within a predetermined time span.
1579.4.2 1579.4.3
1579.4.4
1579.5 Sterilization with Ethylene Oxide (EtO) 1579.5.1 Direct contact between gas and microbial cells is essential; precautions are taken to avoid the presence of organisms likely to be enclosed in such material as crystals or dried protein. The nature and quality of packaging materials can significantly affect the process. Before exposure to gas, materials are brought into equilibrium with the humidity and temperature required by the process. The time required for this is balanced against the opposing need to minimize the time before sterilization. Each sterilization cycle is monitored with suitable biological indicators, using the appropriate number of test pieces distributed throughout the load. The information so obtained is part of the batch record. For each sterilization cycle, records are made of the time taken to complete the cycle, the pressure, the temperature and the humidity within the chamber during the process, the gas concentration, and total amount of gas used. The pressure and temperature are recorded throughout the cycle on a chart. The readings are part of the batch record.
1579.5.2
1579.5.3
1579.5.4
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 88
Health Canada / Health Products and Food Branch Inspectorate
2788 2789 2790 2791 2792 2793 2794 2795 2796 2797 2798 2799 2800 2801 2802 2803 2804 2805 2806 2807 2808 2809 2810 2811 2812 2813 2814 2815 2816 2817 2818 2819 2820 2821 2822 2823 2824 1779.6
1579.5.5
After sterilization, the load is stored in a controlled manner under ventilated conditions to allow residual gas and reaction products to reduce to the defined level. This process is validated.
Biological indicators are considered only as an additional method for monitoring the sterilization, except in the case of ethylene oxide sterilization, where they are a normal part of the monitoring criteria. If they are used, strict precautions are taken to avoid transferring microbial contamination from them. Records are available indicating that the requirements for each sterilization cycle have been met. These records include all recording charts (e.g., time/temperature). A clear visual means is used for differentiating products that have not been sterilized from those that have been sterilized. Each basket, tray, or other carrier of products or components is should be clearly labelled with the name of the material, its batch number, and an indication of whether or not it has been sterilized. Such indicators as autoclave tape or radiation sensitive colour disks may be used, where appropriate, to indicate whether or not a batch (or sub-batch) has passed through a sterilization process. These visual means but they do not give a reliable are not intended to give an indication that the lot is in fact sterile. Note: Refer to Health Canadas P process V validation G guidelines for further guidance on these processes.
18.79.7
19.79.8
1680. Aseptic Filling Operations A written standard designed to test the efficiency of the overall aseptic filling operation is maintained. This standard includes a requirement to perform normal aseptic filling operations using sterile media. 1680.1 The use of nutrient media that support microbial growth in trials to simulate aseptic operations (i.e., sterile media fills, "broth fills") is a valuable part of the overall validation of an aseptic process. Such trials have the following characteristics: 1680.1.1 The trials simulate actual operations as closely as possible and also take into consideration worst case conditions. The medium or media selected are capable of growing a wide spectrum of microorganisms, including those that would be expected to be found in the filling environment. Each batch of media used for process simulation must be tested for its growth promotion capabilities. The trials include a sufficient number of units of production to give a high degree of assurance that low levels of contamination, if present, would be detected.
1680.1.2
1680.1.3
1680.2 A statistically valid number of containers is are filled during each broth-fill trial. The target is zero positives growth. Any positive unit indicates a potential problem regardless of the
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 89
Health Canada / Health Products and Food Branch Inspectorate
2825 2826 2827 2828 2829 2830 2831 2832 2833 2834 2835 2836 2837 2838 2839 2840
run size. All positives should be identified, and should result in a thorough, documented investigation and corrective action implemented. One acceptable method is to determine the contamination rate as an absolute value (e.g. 0.1%). Another acceptable method is a statistical based on the Poisson distribution of contaminated filled units. A contamination rate of less than 0.1% with a 95% confidence limit is acceptable. Any contamination is investigated, and records of such investigations are maintained. Broth fills are repeated at regular intervals, as well as whenever a significant alteration in the product, premises, equipment, or process warrants re-validation. Normally process simulation test should be repeated twice a year per shift and process. All personnel who enter into the aseptic area during product filling should take part in media fills at least once a year.
Observed number of failures Upper 95% confidence limit
10
4 . 7 4
6.3
7 . 7 5
9 . 1 5
1 0. 5 1
1 1. 8 4
1 3. 1 5
1 4. 4 3
1 5. 7 1
16 .9 6
2841 2842 2843 2844 2845 2846 2847 2848 2849 2850 2851 2852 2853 2854 2855 2856 2857 2858 2859
Contamination Rate %=
Upper 95% Confidence Limit Number of Filled Units
X 100
Contamination Rate= (Upper 95% Confidence Limit/ Number of Filled Units) x 100 Example 1: If 3,000 units were filled and two contamination units observed, the upper 95% confidence limit for the contamination rate would be not more than (6.3/3,000) x 100 = 0.21%. This rate is higher than the required value (of less than 0.1%) and therefore would be unacceptable. Example 2: If 3,000 units were filled and no contaminated unit was observed, the upper 95% confidence limit for the contamination rate would be not more than (3/3,000) x 100 = 0.1%. If batches smaller than 3,000 units are produced filled, the minimum number of containers used for process simulation with sterile nutrient media should be equal to the maximum commercial batch size and no contaminated unit should be found after the incubation period. 80.3 A process matrix may be developed for each filling line, and should include elements such as the type of products filled, size of lots, container and closure configuration, fill volume, line speed, filling line configuration and components, and sterile hold times.
Page 90
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
2860 2861 2862 2863 2864 2865 2866 2867 2868 2869 2870
80.4
A process simulation run should be performed of sufficient duration to cover all routine manipulations and operations, various interventions known to occur during normal production, as well as worst case situations. A pre-defined list of all permitted interventions should be documented and incorporated into process simulation on a periodic basis. The process simulation test should simulate all the specific manufacturing steps, such as product transfer, sterile filtration, filling, transfer of semi-stoppered vials to the lyophilizer, the lyophilization cycle, and stoppering and crimping of vials. The process simulation test program incorporates a representative number, type, and complexity of normal interventions that occur with each run, as well as nonroutine interventions, and events (e.g., maintenance, stoppages, equipment, adjustments).
80.5
80.6
2871 2872 2873 2874 2875 2876 2877 2878 2879 2880 2881 2882 2883 2884 2885 2886 2887 2888 2889 2890 2891 2892 2893 2894 2895 2896 2897 2898 2899
80.7
The fill volume should be sufficient to assess potential microbial contamination, and to insure the complete contact with all sterile surfaces inside the container when the container is inverted and swirled. Consideration should be given to incubation of filled vials with media contact with the closure system (e.g. inverted storage). Incubation conditions should be suitable for recovery of bioburden and environmental isolates. Following the aseptic processing of the medium, the filled containers are incubated at 22.5 C 2.5 C or at 32.5 C 2.5 C. All media filled containers should be incubated for a minimum of 14 consecutive days. If two temperatures are used for incubation of media filled samples, then these filled containers should be incubated for at least 7 consecutive days at each temperature starting with the lower temperature. Initial qualification requires three successful process simulation tests. In the absence of observed issues with respect to environmental monitoring or sterility testing, requalification should take place on a regular basis or at least semi-annually with a minimum of a single process simulation.
80.8
80.9
80.10 Every person who is normally allowed to be in the filling room during aseptic filling operations must participate in the process simulation test, during which they must perform their normal assigned duties. Only trained and qualified personnel who have successfully participated in a process simulation test should be permitted to participate in aseptic processing. Records should be maintained. 81. Sterilization by Filtration 81.1 The sterilizing grade filter should be validated to reproducibly remove viable microorganisms from the process stream, producing a sterile effluent. Validation studies should consider factors that can affect filter performance, which generally include viscosity and surface tension of the solution to be filtered, pH, compatibility of the material or formulation components with the filter, pressures, flow rates, batch volume, maximum use time, temperature, osmolality, and the effects of hydraulic shock. The microorganism Brevundimonas diminuta (ATCC 19146) when properly harvested, grown and used, is a common challenge microorganism for sterilizing filters because of its
Page 91
81.2
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
2900 2901 2902 2903 2904 2905 2906 2907 2908 2909 2910 2911 2912 2913 2914 2915 2916 2917 2918 2919 2920 2921 2922 2923 2924 2925 2926 2927 2928 2929 2930 2931 2932 2933 2934 2935 2936 2937 2938 82. 81.5 81.3
size (0.3 m mean diameter). A challenge concentration of at least 107 organisms per cm2 of effective filtration area should generally be used, and should result in no passage of the challenge microorganism. Direct inoculation into the drug formulation is the preferred method because it provides an assessment of the effect of the drug product on the filter matrix and on the challenge organism (except for products with inherent bactericidal activity against this microbe, or oil-based formulations). Use of redundant sterilizing filters should be considered. This second filtration via a further sterilized micro-organism retaining filter, immediately prior to filling, should be carried out as close as possible to the filling point. When the use of one sterilizing filter has been validated to achieve sterilization of a specific product, then the sterilizing filter must satisfactorily pass integrity testing before and after use. When more than one sterilizing filters are used in the filter train, all filters must be tested before use. The secondary sterilizing filter does not require post-use integrity testing unless the primary sterilizing filter fails. In that case, the secondary sterilizing filter must satisfactorily pass integrity testing before and after use. If there are documented reasons for not being able to perform pre-filtration filter integrity testing of either filter in a series after sterilization, (e.g. if sterility downstream of the first filter may be compromised), the filters should be tested both prior to sterilization and after use. For aseptically filled vials, the filling / stoppering must be performed under Grade A conditions with a Grade B background. When this filling / stoppering is finished, the product is usually taken to a lower grade environment by means of a conveyor belt where the crimping is performed. Because complete integrity may not yet be achieved at this point, it is considered that a Grade C environment, when in operation, is the minimal grade to be used for the crimping operation. The following must also be considered: 81.5.1 81.5.2 the crimping should be done as soon as possible after the stoppering; the distance between the exit of the Grade A/B to the actual point of crimping in the lower environment should be kept as short as possible; procedures are in place to ensure that the stoppers are properly seated prior to the crimping operation; line stoppages and time lapses are documented; and stoppered vials which do not get crimped within the established time lapse are segregated and disposed of in accordance with SOPs.
81.4
81.5.3
81.5.4 81.5.5
Blow/ fill/ seal 82.1 Blow/ fill/ seal equipment used for aseptic production is fitted with an effective Grade A air shower and operated in at least a Grade C background environment. The background environment should comply with the viable and non viable limits at rest and viable limit when in operation.
Page 92
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
2939 2940 2941 2942 2943 2944 2945 2946 2947 2948 2949 2950 2951 2952 2953 2954 2955 2956 2957 2958 2959 2960 2961 2962 2963 2964 2965 2966 2967 2968 2969 2970 2971 2972 2973 2974 2975 2976 83.
82.2
Blow/ fill/ seal equipment used for the production of products that are terminally sterilized should be installed with at least a Grade D environment.
Isolator technology 83.1 The environmental cleanliness within an isolator is a Grade A located in at least a Grade D background. Decontamination procedures should ensure full exposure of all isolator surfaces to the chemical agent. Decontamination methods that render the inner surfaces of barrier and isolator systems free of viable microorganisms should be developed and validated. Residues from the decontamination process should not negatively impact product or primary contact surfaces. For sterilization of the filling line, where decontamination methods are used to render certain product contact surfaces free of viable organisms, a minimum of a six-log reduction should be demonstrated using a suitable biological indicator. When using Aseptic processing in isolators the integrity and seams of gloves and half suits should receive daily attention when in use and be addressed by a comprehensive preventative maintenance program. Replacement frequencies should be established in written standard operating procedures that will ensure that parts will be changed before they breakdown or degrade. Transfer systems, gaskets, and seals should be covered by a written maintenance program. Protection against potential ingress of any airborne particles from the environment surrounding the isolator must be a design feature. A breach of isolator integrity should normally lead to a decontamination cycle. Integrity can be affected by power failures, valve failure, inadequate overpressure, holes in gloves and seams, or other leaks. Air quality within the isolator should be monitored for microbiological quality and particulates during each shift.
83.2
83.3
83.4
83.5
83.6
20.84. Filled containers of parenteral products are inspected individually for the presence of particulates and other defects. When inspection is done visually, it takes place under suitable and controlled conditions of illumination, and background, and line speed. Operators doing the inspection pass regular eyesight checks, while wearing corrective lenses if such lenses are normally worn, and are allowed frequent breaks from inspection. Operators are subjected to routine checks for their efficiency in detecting defective units. Where other methods of inspection are used, the process is validated and the performance of the equipment is checked at intervals. 21.85. Filled ampules are subjected to a leaker test (e.g. dye immersion test). Samples of other containers closed by appropriately validated methods are checked for integrity of seal and/or maintenance of vacuum where applicable after an appropriate predetermined period. QUALITY CONTROL
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 93
Health Canada / Health Products and Food Branch Inspectorate
2977 2978 2979 2980 2981 2982 2983 2984 2985 2986 2987 2988 2989 2990 2991 2992 2993 2994 2995 2996 2997 2998 2999 3000 3001 3002 3003 3004 3005 3006
186.
Samples taken for sterility testing are representative of the whole of the batch, but in particular include samples taken from parts of the batch considered to be most at risk of contamination, for example: 186.1 For products that have been filled aseptically, samples include the first and last containers filled the last container filled, and those filled after any significant interruption. of work. 186.2 For products that have been heat-sterilized in their final containers, consideration is given to taking samples from the potentially coolest part of the load. Each sterilizer load is treated as a separate batch for sterility testing purposes.
2.
86.3
The validated sterility test applied to the finished product is only one measure taken to assure sterility. It is to be interpreted in conjunction with the environmental and batch processing records. Batches failing an initial sterility test are rejected unless a thorough investigation is carried out and the initial test is invalidated. The procedure for handling sterility test failures takes into account the guidance provided in official pharmacopeias (Schedule B to the Food and Drugs Act).
3.
86.4
4.87.
Where authorization for parametric release has been issued, after review of the submission which includes validation and monitoring of the process data pursuant to paragraph C.01.065(b)(ii), end product sterility testing is not required. Biological indicators used for routine monitoring of a sterilization process and when used in validation/ re-validation studies should be tested to verify the accuracy of the population count stated by the vendor. Media used for environmental monitoring should be tested for its growth promotion capability, in accordance with a formal written program. Microbial quantification must be based on scientifically sound methods. Because devices vary, the user should assess the suitability of their selected monitoring devices before they are placed into service. Such devices should be calibrated and used according to appropriate procedures. Environmental monitoring data generated in Grade A areas should be reviewed as part of product batch release. A written plan should be available that describes the actions to be taken when an environmental excursion occurs.
88.
89.
90.
91.
3007 3008 3009 3010
MEDICAL GASES
REGULATION C.02.030 The provisions of C.02.025, C.02.027, and C.02.028 do not apply to medical gases.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 94
Health Canada / Health Products and Food Branch Inspectorate
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 95
Health Canada / Health Products and Food Branch Inspectorate
3011 3012 3013 3014 3015 3016 3017 3018 3019 3020 3021 3022 3023 3024 3025 3026 3027 3028 3029 3030 3031 3032 3033 3034 3035 3036 3037 3038 3039 Explanatory Note
ANNEX APPENDIX A INTERNATIONALLY HARMONIZED REQUIREMENTS FOR BATCH CERTIFICATION Content of the Fabricators/Manufacturers Batch Certificate for Drug/Medicinal Products Exported to Countries under the Scope of a Mutual Recognition Agreement (MRA)
In the framework of Mutual Recognition Agreements, the Sectoral Annex on Good Manufacturing Practices (GMP) requires a batch certification scheme for drug/medicinal products covered by the pharmaceutical Annex. The internationally harmonized requirements for the content of the batch certificate of a drug/medicinal product are attached. The importer of the batch is to receive and maintain the batch certificate issued by the fabricator/manufacturer. Upon request, the batch certificate has to be readily available to the regulatory authority of the importing country. This certification by the manufacturer regarding the conformity of each batch is essential to exempt the importer from re-control (re-analysis). Each batch shipped between countries having an MRA in force must be accompanied by a batch certificate issued by the fabricator/manufacturer in the exporting country. This certificate will be issued after a full qualitative and quantitative analysis of all active and other relevant constituents to ensure that the quality of the products complies with the requirements of the marketing authorization of the importing country. The certificate will attest that the batch meets the specifications and has been manufactured in accordance with the marketing authorization of the importing country; will detail the specifications of the product, the analytical methods referenced, and the analytical results obtained; and will contain a statement that the batch processing and packaging quality control records were reviewed and found in conformity with GMP. The batch certificate will be signed by the person responsible for releasing the batch for sale or supply/export at the fabrication/manufacturing recognized building. These harmonized requirements have been agreed on by the regulatory authorities of the following parties/countries: Australia, Canada, European Community, New Zealand, and Switzerland. EFTA Listed designated regulatory authorities are identified within section C.01A.019 of the Food and Drug Regulations. The most recent listing is available on the Health Canada website at the following address: http://www.hc-sc.gc.ca/dhp-mps/compli-conform/int/mra-arm/update-miseajour_tc-tm_e.html
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 96
Health Canada / Health Products and Food Branch Inspectorate
3040 3041
ANNEX A1 Designated regulatory authorities
3042 3043 1
Regulatory authority Swiss Agency for Therapeutic Products (Swissmedic), Bern, Switzerland
Drug or category of drugs Pharmaceuticals for humans or veterinary use Drugs listed in Schedules C and D to the Act.
Activities Fabricating, packaging/labelling, testing
3044
Regional Medicines Inspectorate of Northwestern Switzerland (RFS-NW), Basel, Switzerland
Pharmaceuticals for human or veterinary use. Drugs listed in Schedules C and D to the Act.
Fabricating, packaging/labelling, testing
3045
Regional Medicines Inspectorate of Eastern and Central Switzerland (RFSOZ), Zurich, Switzerland
Pharmaceuticals for human or veterinary use. Drugs listed in Schedules C and D to the Act.
Fabricating, packaging/labelling, testing
3046
Regional Medicines Inspectorate of Southern Switzerland (RFS-S), Ticino, Switzerland
Pharmaceuticals for human or veterinary use. Drugs listed in Schedules C and D to the Act.
Fabricating, packaging/labelling, testing
3047
Regional Medicines Inspectorate of Western Switzerland (RFS-W), Lausanne, Switzerland
Pharmaceuticals for human or veterinary use. Drugs listed in Schedules C and D to the Act.
Fabricating, packaging/labelling, testing
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 97
Health Canada / Health Products and Food Branch Inspectorate
3048 3049 3050 3051 3052 3053 3054 3055 3056 3057 3058 3059 3060 3061 3062 3063 3064 3065 3066 3067 3068 3069 3070 3071 3072 3073 3074 3075 3076 3077 3078 3079 3080 3081 1.
APPENDIX A1 Content of the Fabricators/Manufacturers Batch Certificate for Drug/Medicinal Products Exported to Countries under the Scope of a Mutual Recognition Agreement (MRA) [LETTERHEAD OF EXPORTING MANUFACTURER] Name of product. Proprietary, brand, or trade name in the importing country. Importing country. Marketing authorization number. The marketing authorization number of the product in the importing country should be provided. Strength/Potency. Identity (name) and amount per unit dose are required for all active ingredients/constituents. Dosage form (pharmaceutical form). Package size (contents of container) and type (e.g., vials, bottles, blisters). Lot/batch number. As related to the product. Date of fabrication/manufacture. In accordance with national (local) requirements. Expiry date. Name(s) of fabricator(s)/manufacturer(s) and address(es) of- manufacturing recognized building(s). All recognized buildings involved in the manufacture of the batch including packaging and quality control of the batch, should be listed. The name(s) and address(es) given must correspond to the information provided on the manufacturing authorization/establishment licence. Number(s) of manufacturing authorization(s)/licence(s) or certificate(s) of GMP compliance held by fabricator(s)/manufacturer(s). A number should be given for each recognized building listed under Item 10. Results of analysis. Should include the approved specifications, describe all results obtained, and refer to the analytical methods used (May refer to a separate certificate of analysis, which must be dated, signed, and attached). Comments/remarks. Any additional information that might be of value to the importer and/or inspector who must verify the compliance of the batch certificate (e.g., specific storage or transportation conditions).
Page 98
2. 3.
4.
5. 6. 7.
8.
9. 10.
11.
12.
13.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3082 3083 3084 3085 3086 3087 3088 3089 3090 3091 3092 3093 3094
14.
Certification statement. Should cover the fabrication/manufacturing, including packaging and quality control. The following text should be used: I hereby certify that the above information is authentic and accurate. This batch of product has been fabricated/manufactured, including packaging and quality control, at the above-mentioned recognized building(s) in full compliance with the GMP requirements of the local regulatory authority and with the specifications in the marketing authorization of the importing country. The batch processing, packaging, and analysis records were reviewed and found to be in compliance with GMP. Name and position/title of person approving the batch release. Must include the persons company/recognized building name and address, if more than one company is mentioned under Item 10. Signature of person approving the batch release. Date of signature.
15.
16. 17.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 99
Health Canada / Health Products and Food Branch Inspectorate
3095 3096
ANNEX B APPLICATION FOR ALTERNATE SAMPLE RETENTION
3097 3098 3099 3100 3101 3102 3103 3104 3105
1.
Name of importer/distributor: Address:
Telephone: Fax: 2. Name of product: DIN (if applicable): Name of fabricator: Address:
3.
3106 3107 3108 3109 4.
Telephone: Fax: Name of site where samples are to be retained: Address:
3110 3111 3112 3113 3114 3115 3116 3117 3118 3119 3120 3121 3122 5.
Contact person: Telephone: Fax: Criteria for assessment (complete as applicable) a. The testing of this product requires specialized product-specific methodology that is not available in Canada Yes 9 No 9
If yes, please specify (e.g., unique bioassay involving the use of cell lines or animals): b. This product is subject to Health Canadas lot release program: Yes 9 c. Estimated Canadian utilization: I. Approximate number of lots sold annually in Canada: ii. Approximate number of units sold annually in Canada: No 9
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 100
Health Canada / Health Products and Food Branch Inspectorate
3123 3124 3125 3126 3127 3128 3129 3130 3131 3132 3133 3134 3135 3136 3137 3138 3139 3140 3141 3142 3143 3144 3145 3146 3147 3148 3149 3150 3151 3152 3153 3154 3155 3156 3157 3158 7. 6.
d. e. f. g.
Average batch size imported to Canada: Approximate unit cost/value per sample: Shelf life of perishable drug: Radiopharmaceuticals: Yes 9 No 9
h.
Non-prescription drugs (see Category IV product monographs): Yes 9 (specify) No 9
9 Acne therapies 9 anti-caries products containing fluoride 9 Anti dandruff products 9 Antiperspirants 9 Antiseptic skin cleansers 9 Athletes foot treatments 9 Medicated skin care products 9 Sunburn protectants I. 9 Hard-surface disinfectants
We have formally arranged with the storage site to maintain sufficient numbers of samples of lots under the storage conditions indicated on the label, with the same container-closure sold in Canada, and to allow access to those samples by all pertinent regulatory authorities including Health Canada. Yes 9 No 9
We have a written commitment with the responsible person at the storage site that samples will be provided within 48 hours of receiving a request from Health Canada. Signature of responsible officer: Title: Emergency telephone number:
Mail, e-mail or fax application to France Dansereau Manager, Inspection Unit Health Products and Food Branch Inspectorate National Coordination Centre 11 Holland Avenue, Tower A, 2nd Floor Holland Cross P.L. 3002C Ottawa, Ontario, K1A 0K9 Fax 613-952-9805 E-Mail: france_dansereau@hc-sc.gc.ca
Page 101
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3159 3160 3161 3162 3163 3164 3165 3166 3167 3168 3169 3170 3171 3172 3173 3174 3175 3176 3177 3178 3179 3180 3181 3182 3183 3184 3185 3186 3187 ACRONYMS API:
APPENDIX B
Active Pharmaceutical Ingredient
CoC: Certificate of Compliance DIN: Drug Identification Number GMP: Good Manufacturing Practices ICH: International Conference on Harmonization HPFBI:Health Products and Food Branch Inspectorate NOC: Notice of Compliance MPD: Master Production Documents MRA: Mutual Recognition Agreement OOS: Out of specification PIC/S: Pharmaceutical Inspection Cooperation/Scheme VICH: Veterinary International Conference on Harmonisation WFI: Water for Injection WHO: World Health Organization GLOSSARY OF TERMS The definitions given below apply to the terms used in these guidelines, they also apply to the terms used in the annexes unless otherwise specified therein. Definitions quoted from other documents are identified in brackets at the end of the definition. ACTIVE PHARMACEUTICAL INGREDIENT (ingrdient pharmaceutique actif) - Any substance or mixture of substances that is intended to be used in the manufacture of a drug (medicinal) product and that, when used in the production of a drug, becomes an active ingredient of the drug product. Such substances are intended to furnish pharmacological activity or other direct effect in the diagnosis, cure, mitigation, treatment, or prevention of disease or to affect the structure and function of the body. (ICH, Q7A, step 5) AIRLOCK (sas) - An enclosed space with two or more doors, that is interposed between two or more rooms, usually of differing classes of cleanliness, for the purpose of controlling the airflow between those rooms when either people or goods need to enter or leave them.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 102
Health Canada / Health Products and Food Branch Inspectorate
3188 3189 3190 3191 3192 3193 3194 3195 3196 3197 3198 3199 3200 3201 3202 3203 3204 3205 3206 3207 3208 3209 3210 3211 3212 3213 3214 3215 3216 3217 3218 3219 3220 3221 3222
ALTERNATE SAMPLE RETENTION (ASR) SITE (site alternatif pour la conservation des chantillons) - An alternate location specified on a Drug Establishment Licence for the storage of samples pursuant to section C.02.025 (1) of the Food and Drug Regulations. ASEPTIC AREA (aire aseptique) - A zone or zones within a clean area where Grade A or B (see table in Section C.02.029 of these guidelines) conditions are maintained. ASEPTIC PROCESS (procd aseptique) - A method of producing a sterile product in which sterile bulk drug or sterile raw materials are compounded and assembled with sterile packaging components under Grade A or B conditions (see table in Section C.02.029 of these guidelines). BATCH (lot de fabrication) - A quantity of drug in dosage form, a raw material, or a packaging material, homogeneous within specified limits, produced according to a single production order and as attested by the signatories to the order. In the case of continuous manufacture, a batch corresponds to a defined fraction of the production, that is characterized by its intended homogeneity. It may sometimes be necessary to divide a batch into a number of sub-batches, which are later brought together to form a final homogeneous batch. BATCH CERTIFICATE (certificat de lot) A certificate issued by the fabricator of a lot or batch of a drug that is exported within the framework of a mutual recognition agreement and in which the fabricator (a) identifies the master production document for the drug and certifies that the lot or batch has been fabricated, packaged/labelled and tested in accordance with the procedures described in that document; provides a detailed description of the drug, including (I) a statement of all properties and qualities of the drug, including the identity, potency and purity of the drug, and (ii) a statement of tolerances for the properties and qualities of the drug; ) identifies the analytical methods used in testing the lot or batch and provides details of the analytical results obtained; sets out the addresses of the buildings at which the lot or batch was fabricated, packaged/labelled and tested; and certifies that the lot or batch was fabricated, packaged/labelled and tested in accordance with the good manufacturing practices of the regulatory authority that has recognized those buildings as meeting its good manufacturing practices standard. (C.01A.001)
(b)
(d)
(e)
(The certificates content is also described in Appendix A). BATCH NUMBER (numro de lot de fabrication) - A distinctive combination of numbers and/or letters that specifically identifies a batch. The batch number appears on the batch records, certificates of analysis, etc.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 103
Health Canada / Health Products and Food Branch Inspectorate
3223 3224 3225 3226 3227 3228 3229 3230 3231 3232 3233 3234 3235 3236 3237 3238 3239 3240 3241 3242 3243 3244 3245 3246 3247 3248 3249 3250 3251 3252 3253 3254 3255 3256 3257 3258 3259 3260 3261 3262 3263 3264
BIOLOGICAL DRUG (drogue biologique) - A drug that is listed in Schedule D to the Food and Drugs Act. BRACKETING (mthode des extrmes) - The design of a stability schedule such that only samples on the extremes of certain design factors (e.g., strength, package size) are tested at all time points as in a full design. The design assumes that the stability of any intermediate levels is represented by the stability of the extremes tested. Where a range of strengths is to be tested, bracketing is applicable if the strengths are identical or very closely related in composition (e.g., for a tablet range made with different compression weights of a similar basic granulation, or a capsule range made by filling different plug fill weights of the same basic composition into different sized capsule shells). Bracketing can be applied to different container sizes or to different fills in the same container closure system. (ICH, Q1A)) BULK DRUG (drogue en vrac) - A drug in dosage form that is not in its final packaging, usually in quantities larger than the largest commercially available package size. BULK PROCESS INTERMEDIATE (produit intermdiaire en vrac) - Any intermediate form of a Schedule C or D drug (e.g., final bulk intermediate, bulk material, bulk concentrate, drug substance) which must undergo further processing before it becomes a final product. They are usually characterized by a holding time, storage conditions and the application of in-process tests. CAMPAIGN PRODUCTION (production conscutive) - Sequential processing of material, either more than one product in a multi-product facility or more than one lot of the same product in a dedicated facility, over a defined period of time. Campaign production could occur at any point in a production process where common rooms/suites and/or equipment are reused for multiple products/lots. CERTIFICATE OF ANALYSIS (CoA) (Certificat danalyse) - A document containing the name and address of the laboratory performing the test(s), name and specifications of the material(s), test(s) performed, test method(s) used, actual numerical results, approval date(s), signature of approver, and any other technical information deemed necessary for its proper use. CERTIFICATE OF COMPLIANCE (CoC) (Certificat de conformit (CC)) - A certificate issued by a Regulatory Authority attesting to the GMP compliance of a recognized building in that country. In Canada, the CoC is issued by the HPFB Inspectorate. CERTIFICATE OF MANUFACTURE (certificat de fabrication) - A document issued by a vendor to a distributor or importer that attests that a specific lot or batch of drug has been produced in accordance with its master production documents. Such certificates include a detailed summary of current batch documentation, with reference to respective dates of revision, manufacture, and packaging, and are signed and dated by the vendors quality control department. For drugs that are fabricated, packaged/labelled and tested in MRA countries, the batch certificate is considered to be equivalent. CERTIFICATE OF PHARMACEUTICAL PRODUCT (CPP) (Certificat de produit pharmaceutique) - A certificate issued by the Inspectorate establishing the status of the pharmaceutical, biological, radiopharmaceutical or veterinary product listed and the GMP status of the fabricator of the product. This certificate is in the format recommended by the WHO.
Page 104
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3265 3266 3267 3268 3269 3270 3271 3272 3273 3274 3275 3276 3277 3278 3279 3280 3281 3282 3283 3284 3285 3286 3287 3288 3289 3290 3291 3292 3293 3294 3295 3296 3297 3298 3299 3300 3301 3302
CHANGE CONTROL (contrle des changements) - A written procedure that describes the action to be taken if a change is proposed (a) to facilities, materials, equipment, and/or processes used in the fabrication, packaging, and testing of drugs, or (b) that may affect the operation of the quality or support system. CHANGEOVER PROCEDURE (procdure de conversion) - A logical series of validated steps that ensures the proper cleaning of suites and equipment before the processing of a different product begins. CLEAN AREA (aire propre) - A room or suite of rooms where Grade C or D conditions (see table in Section C.02.029 of these guidelines) are required. The rooms have a defined environmental control of particulate and microbial contamination and are constructed, maintained, and used in such a way as to minimize the introduction, generation, and retention of contaminants. COMMITMENT BATCHES (lots de fabrication viss pour des essais systmatiques) Production batches of a drug product for which the stability studies are initiated or completed post approval through a commitment made in the registration application. (ICH Q1A (R2)) COMPUTERIZED SYSTEMS (systmes informatiss) - Consists of all components, including but not limited to hardware, software, personnel, and documentation, necessary to capture, process, transfer, store, display, and manage information. CONCURRENT PRODUCTION CONTAINMENT (confinement) - Total isolation of one or more steps of a manufacturing process to prevent cross-contamination of the product, or staff, from all other steps of the process. CONTRACTOR (entrepreneur) - Legal entity carrying out activities on behalf of a company pursuant to a written agreement. This includes other sites within the same corporate structure. CRITICAL AREA (aire critique) - Area in which the sterilized drug product, containers, and closures are exposed to environmental conditions that must be designed to maintain product sterility. This critical area is termed as a Grade A area. Activities conducted in this area include manipulations, such as aseptic connections, sterile ingredient additions, filling and closing operations. CRITICAL PROCESS (procd critique) - A process that if not properly controlled may cause significant variation in the quality of the finished product. DATE OF FABRICATION (date de fabrication) - Unless otherwise defined in the Food and Drug Regulations, this is the date when any active ingredient, excipient, anti-oxidant, preservative, or air/oxygen scavenger is first added to the lot being processed. DILUTE DRUG PREMIX (prmlange mdicamentaeux dilu) - A drug for veterinary use that results from mixing a drug premix with a feed as defined in section 2 of the Feed Regulations, 1983, with the lowest approved dosage level of the drug. (C.01.A.001) DIRECTOR (directeur) - The Assistant Deputy Minister, Health Products and Food Branch, of the Department of Health. (A.01.010)
Page 105
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3303 3304 3305 3306 3307 3308 3309 3310 3311 3312 3313 3314 3315 3316 3317 3318 3319 3320 3321 3322 3323 3324 3325 3326 3327 3328 3329 3330 3331 3332 3333 3334 3335 3336 3337 3338 3339 3340
DISTRIBUTOR (distributeur) or MANUFACTURER (fabricant) - A person, including an association or partnership, who under their own name, or under a trade, design or word mark, trade name or other name, word, or mark controlled by them, sells a food or drug. (A.01.010) Divisions 1A and 2 to 4 apply to the following distributors (C.01A.003): (a) a distributor of a drug listed in Schedule C or D to the Act or in Schedule F to these Regulations, a controlled drug as defined in subsection G.01.001 (1) or a narcotic as defined in the Narcotic Control Regulations who does not hold the drug identification number for the drug or narcotic; and a distributor of a drug for which that distributor holds the drug identification number.
(b)
DOSAGE FORM (forme posologique) - A drug product that has been processed to the point where it is now in a form in which it may be administered in individual doses. DRUG (drogue) - Any substance or mixture of substances manufactured, sold, or represented for use in (a) the diagnosis, treatment, mitigation, or prevention of a disease, a disorder, an abnormal physical state, or the symptoms thereof, in humans or animals, (b) restoring, correcting, or modifying organic functions in humans or animals, or (c) "disinfection" in premises in which food is manufactured, prepared, or kept. (Section 2 of the Food and Drugs Act) In Division 1A and Division 2 of the Food and Drug Regulations, "drug" means a drug in dosage form, or a drug that is a bulk process intermediate that can be used in the preparation of a drug listed in Schedule C to the Act or in Schedule D to the Act that is of biological origin. It does not include a dilute drug premix, a medicated feed as defined in Section 2 of the Feeds Regulations, 1983, a drug that is used only for the purposes of an experimental study in accordance with a certificate issued under Section C.08.015 or a drug listed in Schedule H to the Act. (C.01A.001(2)) DRUG ESTABLISHMENT LICENCE (licence dtablissement pour les produits pharmaceutiques) - A licence issued to a drug establishment in Canada which has been inspected and assessed as being in compliance with the applicable requirements of Divisions 2 to 4 of the Food and Drug Regulations. DRUG IDENTIFICATION NUMBER (drogue: identification numrique) - A number assigned to each drug in dosage form under the Food and Drug Regulations with the exception of blood and blood components and radiopharmaceuticals. DRUG PREMIX (prmlange mdicamenteux) - a drug for veterinary use to which a drug identification number has been assigned, where the directions on its label specify that it is to be mixed with feed as defined in Section 2 of the Feeds Act. (C.01A.001) EXPIRY DATE (date limite dutilisation) - Means the earlier of (a) the date, expressed at minimum as a year and month, up to and including which a drug maintains its labelled potency, purity and physical characteristics, and (b) the date, expressed at minimum as a year and month, after which the manufacturer recommends that the drug not be used; C.01.001) EXPORT CERTIFICATE (under Section 37 of the Food and Drugs Act) (Certificat d'exportation (en vertu de l'article 37 de la Loi sur les aliments et drogues)) - A certificate signed
Page 106
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3341 3342 3343 3344 3345 3346 3347 3348 3349 3350 3351 3352 3353 3354 3355 3356 3357 3358 3359 3360 3361 3362 3363 3364 3365 3366 3367 3368 3369 3370 3371 3372 3373 3374 3375 3376
by the fabricator and a Commissioner for Taking Oaths to attest that the drug for which the certificate is prepared is not manufactured or sold for consumption in Canada and that its package and the contents do not contravene any known requirement of the law of the country to which it is or is about to be consigned. FABRICATE (manufacturer) - To prepare and preserve a drug for the purpose of sale. (C.01A.001) FABRICATORS BATCH CERTIFICATE (Certificat de fabrication dun lot) - A certificate delivered under the scope of a mutual recognition agreement for a lot or batch of a drug. (The certificates content is described in Annex A). Please refer to regulation C.01A.001 (1) for a complete definition of batch certificate. FILLING (remplissage) - Transferring a bulk drug into its final container and enclosing it in the container. FINISHED PRODUCT (produit fini) - A product that has undergone all stages of production, including packaging in its final container and labelling. FORMULATING (transformation) - Preparing components and combining raw materials into a bulk drug. For sterile products, this includes such steps as cleaning, rinsing, sterilizing, aerating, flushing, and filtering. GROUP 2 PRODUCTS (produits du groupe 2) - Drugs listed in Schedule D to the Act and subject to Health Canadas lot release programme which require the highest level assessment after the notice of compliance (NOC) has been issued. This assessment includes targeted testing, protocol review, and written approval for sale of each lot in Canada in the form of a release letter. GROWTH PROMOTION (stimulation de la croissance) - A test in which prepared media is challenged with pre-selected organisms to assure that the media is capable of supporting growth. IMPORT (importer) - To import into Canada a drug for the purpose of sale (C.01A.001) IN-PROCESS CONTROL (contrle en cours de fabrication ) - Checks performed during production in order to monitor and, if necessary, to adjust the process to ensure that the finished product conforms to its specifications. The control of the production environment or equipment may also be regarded as a part of in-process control. IN-PROCESS DRUG (drogue semi-finie) - Any material or mixture of materials that must, to become a drug in dosage form, undergo further processing. IN-PROCESS TESTING (analyse en cours de fabrication) - The examination or testing of any material or mixture of materials during the manufacturing process. INSTALLATION QUALIFICATION (qualification d'installation) - The documented act of demonstrating that process equipment and ancillary systems are appropriately selected and correctly installed.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 107
Health Canada / Health Products and Food Branch Inspectorate
3377 3378 3379 3380 3381 3382 3383 3384 3385 3386 3387 3388 3389 3390 3391 3392 3393 3394 3395 3396 3397 3398 3399 3400 3401 3402 3403 3404 3405 3406 3407 3408 3409 3410 3411 3412 3413 3414 3415
LABEL (tiquette) - Includes any legend, word, or mark attached to, included in, belonging to, or accompanying any food, drug, cosmetic, device, or package (Section 2 of the Act). The inner and outer drug product labels must contain the information described in Section C.01.004 of the Food and Drug Regulations. As described in package/label, the action of labelling refers to affixing the inner or outer label to the drug. (C.01A.001) LONG TERM TESTING (analyses long terme) - Stability studies under the recommended storage condition, for the re-test period or shelf life proposed (or approved) for labelling. (ICH, Q1A)) LOT (lot) - A quantity of any drug in dosage form, a raw material, or a packaging material, homogeneous within specified limits, constituting all or part of a single batch and identified by a distinctive lot number that appears on the label of the finished product. LOT FAILURE (lot dfectueux) - A lot or batch that has been rejected due to failure to meet in process or final product release specifications. LOT NUMBER (numro de lot) - Any combination of letters, figures, or both, by which any food or drug can be traced in manufacture and identified in distribution. (A.01.010) MANUFACTURER (fabricant) or DISTRIBUTOR (distributeur) - See definition under distributor. MANUFACTURING BATCH DOCUMENT RECORD (fiche de lot de fabrication) Instructions that outline in detail the materials and procedures required to fabricate, prepare, and preserve a single lot or batch of a drug in dosage form. Records demonstrating that the batch of a drug was fabricated in accordance with the approved master production documents. MARKETING AUTHORIZATION (autorisation de mise en march) - A legal document issued by Health Canada, authorizing the sale of a drug product in Canada; it includes a Notice of Compliance (NOC) or a Drug Identification Number (DIN). and/or Natural Health Product number (NPN). A legal document issued by Health Canada, authorizing the sale of a drug or a device based on the health and safety requiremenets of the Food and Drug Act and its associated Regulations. The marketing authorization may be in the form of a Drug Identification Number (DIN), a device licence for classes II, III and IV medical devices, or a natural health product licence (NPN or DINHM). MASS BALANCE (somme des masses) - The process of adding together the assay value and levels of degradation products to see how closely these add up to 100% of the initial value, with due consideration of the margin of analytical error. (ICH, Q1A)) MASTER FORMULA (formule-type) - A document or set of documents specifying the raw materials with their quantities and the packaging materials, together with a detailed description of the procedures and precautions required to produce a specified quantity of a finished product as well as the processing instructions, including the in-process controls. MASTER PRODUCTION DOCUMENTS (MPD) (document-type de production) - a Documents that includes specifications for raw material, for packaging material and for packaged
Page 108
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3416 3417 3418 3419 3420 3421 3422 3423 3424 3425 3426 3427 3428 3429 3430 3431 3432 3433 3434 3435 3436 3437 3438 3439 3440 3441 3442 3443 3444 3445 3446 3447 3448 3449 3450 3451 3452
dosage form; master formula (including composition and instructions as described in the definition above), sampling procedures, and critical processing related SOPs, whether or not these SOPs are specifically referenced in the master formula. MATRIXING (mthode de la matrice) - The design of a stability schedule such that a selected subset of the total number of possible samples for all factor combinations is tested at a specified time point. At a subsequent time point, another subset of samples for all factor combinations is tested. The design assumes that the stability of each subset of samples tested represents the stability of all samples at a given time point. The differences in the samples for the same drug product should be identified as, for example, covering different batches, different strengths, different sizes of the same container closure system, and possibly in some cases, different container closure systems. (ICH, Q1A)) The concept of matrixing may also apply in other areas such as validation. MEDICAL GAS (gaz mdical) - Any gas or mixture of gases manufactured, sold or represented for use as a drugC.02.002) MRA COUNTRY (pays participant un ARM) - A country that is a participant to a mutual recognition agreement with Canada. (C.01A.001). MUTUAL RECOGNITION AGREEMENT (MRA) (accord de reconnaissance mutuelle (ARM)) An international agreement that provides for the mutual recognition of compliance certification for Good Manufacturing Practices for drugs. (C.01A.001) OPERATIONAL QUALIFICATION (qualification oprationelle) - The documented action of demonstrating that process equipment and ancillary systems work correctly and operate consistently in accordance with established specifications. PACKAGE (emballer) - As described in package/label, the action of packaging refers to putting a drug in its immediate container. C.01A.001) PACKAGE/LABEL (emballer/tiqueter) - To put a drug in its immediate container or to affix the inner or outer label to the drug. (C.01A.001) PACKAGING (emballage) - Operations required to package and label a single lot or batch of a drug in dosage form. PACKAGING BATCH DOCUMENT RECORD (fiche d'emballage de lot de fabrication) Instructions that outline in detail the materials and special procedures required to package and label a single lot or batch of a drug in dosage form. Records demonstrating that the batch of a drug was packaged in accordance with the approved master production documents. PACKAGING MATERIAL (matriel d'emballage) - Labels, printed packaging materials and those components in direct contact with the dosage form. (refer to C.02.002) PARENTERAL USE (usage parentral) - Administration of a drug by means of hypodermic syringe, needle or other instrument through or into the skin or mucous membrane. C.01.001)
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 109
Health Canada / Health Products and Food Branch Inspectorate
3453 3454 3455 3456 3457 3458 3459 3460 3461 3462 3463 3464 3465 3466 3467 3468 3469 3470 3471 3472 3473 3474 3475 3476 3477 3478 3479 3480 3481 3482 3483 3484 3485 3486 3487 3488 3489
PHARMACEUTICAL (produit pharmaceutique) - A drug other than a drug listed in Schedule C or D to the Act. (C.01A.001). POTENCY (teneur) - The activity or amount of active moiety, or any form thereof, indicated by label claim to be present. PRIMARY BATCHES (lots primaires) - A batch of a drug product used in a formal stability study, from which stability data are submitted in a registration application for the purpose of establishing a re-test period or shelf life, respectively. (ICH Q1A (R2)) PROCESS QUALIFICATION (qualification de procd) - The phase of validation dealing with sampling and testing at various stages of the manufacturing process to ensure that product specifications are met. PROCESS VALIDATION (validation du procd) - Establishing documented evidence with a high degree of assurance, that a specific process will consistently produce a product meeting its predetermined specifications and quality characteristics. Process validation may take the form of Prospective, Concurrent or Retrospective Validation and Process Qualification or Re-validation. PRODUCTION (production) - All operations involved in the preparation of a finished product, from receipt of materials, through processing and packaging, to completion of the finished product, including storage. PURIFIED WATER (eau purifie) - As defined in any standard listed in Schedule B to the Food and Drugs Act. PURITY (puret) - The extent to which a raw material or a drug in dosage form is free from undesirable or adulterating chemical, biological, or physical entities as defined by specifications. QUALIFIED AUTHORITY (autorit qualifie) - An authorityA member of the Pharmaceutical Inspection Cooperation/Scheme (PIC/S) or the United States Food and Drug Administration (USFDA). QUALIFIED PERSONNEL (personnel qualifi) - Individuals who have the appropriate education, training and experience to perform their duties. QUALITY CONTROL DEPARTMENT (service du contrle de la qualit) - A separate and distinct operation function maintained by a manufacturer fabricator, packager/labeller, distributor, or an importer, that is responsible only to management, and that monitors the quality of production operations and exercises control over the quality of materials required for and resulting from those operations. QUARANTINE (quarantaine) - Effective restriction of the availability of material or product for use (physically or by system), until released by the quality control department. RADIOPHARMACEUTICAL (drogue radiopharmaceutique) - A drug that exhibits spontaneous disintegration of unstable nuclei with the emission of nuclear particles or photons. C.03.201)
Page 110
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3490 3491 3492 3493 3494 3495 3496 3497 3498 3499 3500 3501 3502 3503 3504 3505 3506 3507 3508 3509 3510 3511 3512 3513 3514 3515 3516 3517 3518 3519 3520 3521 3522 3523 3524 3525 3526
RAW MATERIAL (matire premire) - Any substance, other than in-process drug or packaging material, intended to be used in the manufacture of drugs, including those that appear in the master formula but that do not appear in the drug such as solvents and processing aids. RECOGNIZED BUILDING (btiment reconnu) - In respect of the fabrication, packaging/labelling or testing of a drug, a building that a regulatory authority that is designated under subsection C.01A.019(1) in respect of that activity has recognized as meeting its Good Manufacturing Practices standards in respect of that activity for that drug. (C.01A.001) RECONCILIATION (bilan comparatif) - A comparison, making due allowance for normal variation, between the amount of product or materials theoretically produced or used and the amount actually produced or used. RECOVERY (rcupration) - The introduction of all or part of previous batches of the required quality into another batch at a defined stage of manufacture. REGULATORY AUTHORITY (autorit rglementaire) - A government agency or other entity in an MRA country that has a legal right to control the use or sale of drugs within that country and that may take enforcement action to ensure that drugs marketed within its jurisdiction comply with legal requirements. RE-PACKAGING / RE-LABELLING (remballer/rtiqueter) - Replacement of packaging or labelling of previously packaged and labelled products. REPROCESSING (retraitement) - Subjecting all or part of a batch or lot of an in-process drug, a bulk process intermediate (final biological bulk intermediate) or a bulk drug of a single batch/lot to a previous step in the validated manufacturing process due to failure to meet predetermined specifications. Reprocessing procedures are foreseen as occasionally necessary and are validated and pre-approved by the quality control department or as part of the marketing authorization. RE-TEST DATE (date de r-analyse) -The date when samples of a drug substance are reexamined to ensure that the material is still suitable for use. The date when a material should be re-examined to ensure that it is still suitable for use. (ICH Q7) RE-TEST PERIOD (priode de r-analyse) - The period of time during which a drug substance can be considered to remain within the specifications and therefore acceptable for use in the fabrication of a given drug product, provided that it has been stored under defined conditions; after this period, the batch is re-tested for compliance with specifications and then used immediately. (ICH, Q1A)) RETURNED PRODUCT (produit retourn) - Bulk drug or finished product sent back to the manufacturer or importer. REWORKING (reprise) - Subjecting an in-process drug, a bulk process intermediate (final biological bulk intermediate), or final product of a single batch/lot to an alternate manufacturing process due to a failure to meet predetermined specifications. Reworking is an unexpected occurrence and is not pre-approved as part of the marketing authorization. (WHO GMP)
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 111
Health Canada / Health Products and Food Branch Inspectorate
3527 3528 3529 3530 3531 3532 3533 3534 3535 3536 3537 3538 3539 3540 3541 3542 3543 3544 3545 3546 3547 3548 3549 3550 3551 3552 3553 3554 3555 3556 3557 3558 3559 3560 3561 3562
SELF-CONTAINED FACILITY (installation confine) - means a premises that provides complete and total separation of all aspects of the operation, including personnel and equipment movement, with well established procedures, controls and monitoring. This includes physical barriers and separate utilities such as as well as separate air handling systems. A self-contained facilities facility does not necessarily imply two a distinct and separate buildings. SELL (vendre) - Offer for sale, expose for sale, have in possession for sale, and distribute, regardless of whether the distribution is made for consideration. (Section 2 of the Food and Drugs Act) SHELF LIFE / EXPIRATION DATING PERIOD - (dure de conservation/priode de premption) - The time interval during which a drug product is expected to remain within the approved specification provided that it is stored under the conditions defined on the label and in the proposed containers and closure. SPECIFICATIONS (spcifications) - Means a detailed description of a drug, the raw material used in a drug, or the packaging material for a drug and includes: (a) a statement of all properties and qualities of the drug, raw material or packaging material that are relevant to the manufacture, packaging, and use of the drug, including the identity, potency, and purity of the drug, raw material, or packaging material, a detailed description of the methods used for testing and examining the drug, raw material, or packaging material, and a statement of tolerances for the properties and qualities of the drug, raw material, or packaging material. C.02.002.)
(b)
STANDARD OPERATING PROCEDURE (SOP) - (procdure opratoire normalise (PON)) A written procedure giving instructions for performing operations not necessarily specific to a given product or material but of a more general nature (e.g., equipment operation, maintenance and cleaning; validation; cleaning of premises and environmental control; sampling and inspection). Certain SOPs may be used to supplement product-specific master and batch production documents. STERILE (strile) - Free from viable microorganisms. STERILIZING FILTER (filtre strilisant) - A filter used to render a material sterile. Sterilizing filters have a rated pore size of 0.2 m or less. SYSTEM (systme) - A regulated pattern of interacting activities and techniques that are united to form an organized whole. TERMINAL STERILIZATION (strilisation en phase terminale) - Sterilizing a drug in its final closed container. TEST (analyser) - To perform the tests, including any examinations, evaluations, and assessments, as specified in the Division 2 of the Food and Drug Regulations.
Page 112
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3563 3564 3565 3566 3567 3568 3569 3570 3571 3572 3573 3574 3575
VALIDATION (validation) - The documented act of demonstrating that any procedure, process, and activity will consistently lead to the expected results. Includes the qualification of systems and equipment. VENDOR (vendeur) - The Person who is the fabricator of the item (raw material, packaging material, medicinal ingredients, reagents). VETERINARY DRUGS (drogues vtrinaires) - Drugs that are administered to food-producing and companion animals. WHOLESALE (vendre en gros) - To sell any of the following drugs, other than at retail sale, where the seller's name does not appear on the label of the drugs: (a) a drug listed in Schedule C or D to the Act or in Schedule F to these Regulations or a controlled drug as defined in subsection G.01.001 (1); or (b) a narcotic as defined in the Narcotic Control Regulations. (C.01A.001)
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 113
Health Canada / Health Products and Food Branch Inspectorate
3576 3577 3578 3579 3580 3581 3582 3583 3584 3585 3586 3587 3588 3589 3590 3591 3592 3593 3594 3595 3596 3597 3598 3599 3600 3601 3602 3603 3604 3605 3606 3607 3608 3609 3610 3611 3.1
ANNEX APPENDIX C
REFERENCES
Food and Drugs Act http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/acts_regs_e.html http://laws.justice.gc.ca/en/F-27/index.html Food and Drug Regulations http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/acts_regs_e.html http://laws.justice.gc.ca/en/F-27/C.R.C.-c.870/index.html Controlled Drugs and Substances Act http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/acts_regs_e.html http://laws.justice.gc.ca/en/C-38.8/index.html Conditions of Acceptance of Foreign Inspection Reports for Listing Foreign Sites on Canadian Establishment Licences (POL-0013) http://hc-sc.gc.ca/dhp-mps/compli-conform/licences/directives/pol_13_tc-tm_e.html Good Manufacturing Practices Interpretation Decision Record Guide http://www.hc-sc.gc.ca/hpb-dgps/therapeut/zfiles/english/guides/gmp/interpretation_guide_e.pdf GMP Questions and Answers http://hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/question/index_e.html Good Manufacturing Practices for Schedule C Drugs (GUI-0026) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/annex_sched_c_tc_e.html http://www.hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/docs/sched_c-annexe_c_tc-tm_e.html Good Manufacturing Practices for Schedule D Drugs, Part 1, Biological Drugs (GUI-0027) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/sched_d_part1_tc_e.html http://www.hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/docs/sched_d_part1-annexe_d_part1_t c-tm_e.html Good Manufacturing Practices for Schedule D Drugs, Part 2, Human Blood and Blood Components (GUI-0032) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/sched_d_part2_tc_e.html http://www.hc-sc.gc.ca/dhp-mps/compli-conform/info-prod/don/sched_d_part2-annexe_d_part2_t c-tm_e.html Risk classification of GMP observations (GUI0023) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/risk_clas_gmp_obs_tc_e.html http://hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/docs/gui_23_tc-tm_e.html Guidelines for Temperature Control of Drug Products during Storage and Transportation (GUI-0069) http://www.hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/docs/gui-0069_tc-tm_e.html
Page 114
4.2
2.3
4.
9.5
6.
7.
8.
199.
10.
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3612 3613 3614 3615 3616 3617 3618 3619 3620 3621 3622 3623 3624 3625 3626 3627 3628 3629 3630 3631 3632 3633 3634 3635 3636 3637 3638 3639 3640 3641 3642 3643 3644 3645 3646 3647
5.11
Good Manufacturing Practices for Medical Gases (GUI-0031) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/gmp_med_gases_tc_e.html http://www.hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/docs/gui_0031_tc-tm_e.html GMP Interpretation Decision Records for Medical Gases (GUI-0062) http://www.hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/docs/gui_62_tc-tm_e.html
12.
1813. Product Recall Procedures http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/recall_procedure_tc_e.html http://hc-sc.gc.ca/dhp-mps/compli-conform/recall-retrait/proces_e.html 1.14 Cleaning Validation Guidelines http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/clean_val_gui_tc_e.html http://www.hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/validation/cleaning-nettoyage_tc-tm_e. html
2315. Validation Guidelines for Pharmaceutical Dosage Forms (GUI-0029) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/pharm_dos_form_tc_e.html http://www.hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/validation/gui_29_tc-tm_e.html 2216. Validation Documentation Requirements and Responsibilities for Drug Fabricators, Packagers/Labellers, Distributors and Importers (GUI-0042) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/validation_guide_tc_e.html http://www.hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/validation/req_resp-exig_resp_e.html 17. Process Validation Guidelines: Moist Heat Sterilization for Pharmaceuticals (GUI-0010) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/moist_heat_ster_pharm_tc_e.html http://hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/validation/mhsp-schpp_tc-tm_e.html Irradiation Sterilization for Pharmaceuticals (GUI-0009) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/irra_ster_pharm_tc_e.html http://hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/validation/isp-sipp_tc-tm_e.html Gaseous Sterilization for Pharmaceuticals (GUI-0007) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/gaseous_2001_tc_e.html http://hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/validation/gsp-sgpp_tc-tm_e.html Form-Fill-Seal for Drugs (GUI-0008) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/form_fill_seal_drugs_tc_e.html http://hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/validation/ffsd-frsm_tc-tm_e.html Aseptic Processes for Pharmaceuticals (GUI-0006) http://www.hc-sc.gc.ca/hpfb-dgpsa/inspectorate/asep_proc_pharm_tc_e.html http://hc-sc.gc.ca/dhp-mps/compli-conform/gmp-bpf/validation/app-papp_tc-tm_e.html 1618. Pharmaceutical Inspection Convention (PIC) and
Page 115
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Health Canada / Health Products and Food Branch Inspectorate
3648 3649 3650 3651 3652 3653 3654 3655 3656 3657 3658 3659 3660 3661 3662 3663 3664 3665 3666 3667 3668 3669 3670 3671 3672 3673 3674 3675 3676
Pharmaceutical Inspection Cooperation Scheme (PIC/s) http://www.picscheme.org/index.htm 10.19 International Conference on Harmonisation (ICH) Topics and Guidelines, Quality Topics http://www.ifpma.org/ich5q.html http://www.ich.org/cache/compo/276-254-1.html 11.20 ICH Q1A(R2): Stability Testing of New Drug Substances and Products http://www.hc-sc.gc.ca/hpb-dgps/therapeut/zfiles/english/guides/ich/draft/q1a(r)_e.pdf http://www.ich.org/LOB/media/MEDIA419.pdf 12.21 ICH Q1C: Stability Testing for New Dosage Forms http://www.hc-sc.gc.ca/hpb-dgps/therapeut/zfiles/english/guides/ich/quality/q1c_e.html http://www.ich.org/LOB/media/MEDIA413.pdf 13.22 ICH Q2A: Text on Validation of Analytical Procedures ICH Q2(R1): Validation of Analytical Procedures: Text and Methodology http://www.hc-sc.gc.ca/hpb-dgps/therapeut/zfiles/english/guides/ich/quality/q2a_e.html http://www.ich.org/LOB/media/MEDIA417.pdf 14. ICH Q2B: Validation of Analytical Procedures: Methodology http://www.hc-sc.gc.ca/hpb-dgps/therapeut/zfiles/english/guides/ich/quality/q2b_e.html
1523. ICH Q7A: Good Manufacturing Practice Guide for Active Pharmaceutical Ingredients (draft) http://www.hc-sc.gc.ca/hpb-dgps/therapeut/zfiles/english/guides/ich/draft/q7a_step2_e.pdf http://www.ich.org/LOB/media/MEDIA433.pdf 24. ICH Q1B: Stability Testing: Photostability Testing of New Drug Substances and Products http://www.ich.org/LOB/media/MEDIA412.pdf
2025. Stability Requirements for Changes to Marketed New Drugs http://www.hc-sc.gc.ca/hpb-dgps/therapeut/zfiles/english/policy/issued/mkndpsta_e.html http://www.hc-sc.gc.ca/dhp-mps/prodpharma/applic-demande/pol/marnd_dncom_pol_e.html 2126. Stability Testing of Existing Drug Substances and Products http://www.hc-sc.gc.ca/hpb-dgps/therapeut/zfiles/english/guides/c_mguide/stabtest_e.html http://hc-sc.gc.ca/dhp-mps/prodpharma/applic-demande/guide-ld/chem/stabt_stabe_e.html
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 116
Health Canada / Health Products and Food Branch Inspectorate
3677 3678 3679 3680 3681 3682 3683 3684 3685 3686 3687 3688 3689 3690 3691 3692 3693 3694 3695 3696 3697 3698
Name France Dansereau, Chair Richard Ferland Francisco Fernandes Taras Gedz Denis Girard Raymond Giroux Alicja Kasina Daryl Krepps Stephen McCaul Mdic Ndayishimiye, Secretary Randy Stephanchew
GMP Committee members
Title / Office / Bureau Manager, Inspection Unit, National Coordination Centre, HPFBI* Location Ottawa, ON
MRA officer Drug Specialist, Ontario & Nunavut Operational Centre, HPFBI Bureau of Pharmaceutical Sciences, BPS** Scientific Assessment Advisor, VDD*** Drug Specialist, Quebec Operational Centre, HPFBI Drug Specialist, Atlantic Operational Centre, HPFBI Senior Regulatory Advisor, BGTD**** MRA Officer Compliance Officer, National Coordination Centre, HPFBI
Longueuil, QC Toronto, ON Ottawa, ON Ottawa, ON Longueuil, QC Halifax, NS Ottawa, ON Toronto, ON Ottawa, ON
Drug Specialist, Manitoba and Saskatchewan Operational Centre, HPFBI Drug Inspection Specialist, National Coordination Centre, HPFBI Drug Specialist, Western Operational Centre, HPFBI A/Manager, Policy and Regulations Division, NCC, HPFBI
Winnipeg, MB
Stphane Taillefer Sheila Welock Kim Dayman-Rutkus * ** *** ****
Ottawa, ON Burnaby, BC Ottawa, ON
Health Products and Food Branch Inspectorate Bureau of Pharmaceutical Sciences, Therapeutic Products Directorate Veterinary Drugs Directorate, Health Products and Food Branch Biologics and Genetic Therapies Directorate
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 117
Health Canada / Health Products and Food Branch Inspectorate
3699
List of contributors
Name To nino A ntonetti Drug GM P Inspection U nit, Compliance and E nforcement Coordination D ivision, H PFB Inspectorate Richard Ferland Quality and Inform ation M anagement Division, H PFB Inspectorate Francisco Fernandes Ontario O perational C entre, H PFB Inspectorate Taras Gedz Office of Clinical Trials, Therap eutic P roducts D irectorate Raymond G iroux Quebec Operational C entre, H PFB Inspectorate Paul Gustafson Manitob a and Saska tchewan O perational C entre, H PFB Inspectorate Tho H uynh Quebec Operational C entre, H PFB Inspectorate Louise Jodoin Drug GM P Inspection U nit, Compliance and E nforcement Coordination D ivision, HP FB Inspectorate Simon Jones Manufac turing and Chemical Ev aluation Division, V eterinary Dru gs Directorate Stephen M cCaul Quality and Inform ation M anagement Division, H PFB Inspectorate W ill Stevens Centre for B iologics Evaluation, Bio logics and G enetic T herap ies Directorate Johanne Vee nstra Drug GM P Inspection U nit, Compliance and E nforcement Coordination D ivision, H PFB Inspectorate Sheila Welock W estern O perational C entre, H PFB Inspectorate Location Ottawa, ON
3700 3701 3702 3703 3704 3705 3706 3707 3708 3709 3710 3711 3712 3713 3714 3715 3716 3717 3718 3719 3720 3721 3722 3723 3724 3725 3726 3727
Longueuil, QC
Toronto, ON
Ottawa, ON
Longueuil, QC Winnipeg, MB
Longueuil, QC
Ottawa, ON
Ottawa, ON
Scarborough, ON Ottawa, ON
Ottawa, ON
Burnaby, BC
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 118
Health Canada / Health Products and Food Branch Inspectorate
3728 3729
Health Products and Food Branch Inspectorate Operational Centres
NATIONAL COORDINATION CENTRE 11 H olland Avenue, T ower A, 2 nd Floor Holland Cross P.L. 3002C Ottawa, Ontario, K1A 0K9 Manager, Inspection Unit: France Dansereau T 613-957-1492 F 613-952-9805 ATLANTIC OPERATIONAL CENTRE 1505 Barrington Street, Suite 1625 Halifax, Nova Scotia, B2J 3Y6 Manager: Annette Daley T 902-426-5350 F 902-426-6676 QUEBEC OPERATIONAL CENTRE 1001 West St-Laurent Blvd. Longueuil, Qubec, J4K 1C7 Manager: Alain Brub T 450-646-1353 F 450-928-4455 ONTARIO AND NUNAVUT OPERATIONAL CENTRE 2301 M idland Avenue Scarborough, Ontario, M1P 4R7 Manager: Jean-Marc Charron T 416-973-1466 F 416-973-1954 MANITOBA AND SASKATCHEWAN OPERATIONAL CENTRE 510 Lagimodiere Blvd. Winnipeg, Manitoba, R2J 3Y1 Manager: Robert Scales T 204-983-5453 F 204-984-2155 BRITISH COLOMBIA AND YUKON OPERATIONAL CENTRE 3155 W illingdon Green Burnaby, B.C., V5G 4P2 Manager: Dennis Shelley T 604-666-3704 F 604-666-3149
3730 3731 3732 3733 3734 3735 3736 3737 3738 3739 3740 3741 3742 3743 3744 3745 3746 3747 3748 3749 3750 3751 3752 3753 3754 3755 3756 3757 3758 3759 3760 3761 3762 3763 3764 3765 3766
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 119
Health Canada / Health Products and Food Branch Inspectorate
3767 3768 3769 3770 3771 3772 3773 3774 3775 3776
Health Products and Food Branch Inspectorate - Operational Centres
ATLANTIC OPERATIONAL CENTRE Health Produ cts and Foo d B ranch Inspectorate 16 th floor, suite 1625 1505 Barrington Street Halifax, No va Scotia B3J 3Y6 Tel: (902) 426-2160 Fax: (902) 426-6676 E-mail: insp_aoc-coa@hc-sc.gc.ca
3777 3778 3779 3780 3781 3782 3783 3784
QUEBEC OPERATIONAL CENTRE Health Produ cts and Foo d B ranch Inspectorate 100 1 St-Laurent Street W est Longueuil, Qubec J4K 1C7 Tel: (450) 646-1353 Fax: (450) 928-4455 E-mail: QOC -COQ@ hc-sc.gc.ca
3785 3786 3787 3788 3789 3790 3791 3792
ONTARIO OPERATIONAL CENTRE Health Produ cts and Foo d B ranch Inspectorate 2301 M idland Avenue Scarborough, Ontario M1P 4R7 Tel: (416) 973-1600 Fax: (416) 973-1954 E-mail: insp_onoc-coon@hc-sc.gc.ca
3793 3794 3795 3796 3797 3798 3799 3800
MANITOBA AND SASKATCHEWAN OPERATIONAL CENTRE Health Produ cts and Foo d B ranch Inspectorate 510 Lagimo dire Blvd Winnipeg, Manitoba R2J 3Y1 Tel: (204) 984-1341 Fax: (204) 984-2155 E-mail: Insp_MSOC _COM S@hc-sc.gc.ca
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 120
Health Canada / Health Products and Food Branch Inspectorate
3801 3802 3803 3804 3805 3806 3807 3808 3809
WESTERN OPERATIONAL CENTRE Health Produ cts and Foo d B ranch Inspectorate 4 th Floor 4595 Canada W ay Burnaby, British-C olom bia V5G 1J9 Tel: (604) 666-3704 Fax: (604) 666-3149 E-mail: insp_woc-coo@hc-sc.gc.ca
3810 3811 3812 3813 3814 3815 3816 3817 3818 3819
IN SP EC TO R AT E O TT AW A Health Produ cts and Foo d B ranch Inspectorate Gra ham Spry B uilding, 2 nd Floor 250 Lanark A venue Address Locator #2002B Ottaw a, On tario K1A 0K9 Tel: (613) 957-1492 Fax: (613) 957-6709 E-mail: GM P_questions_BPF@ hc-sc.gc.ca
Good Manufacturing Practices (GMP) Guidelines - 2007 Edition - Draft for comments December 2002
Page 121
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Symbiosis Law School ICE QuestionsDocument2 pagesSymbiosis Law School ICE QuestionsRidhima PurwarNo ratings yet
- Aerospace Propulsion Course Outcomes and Syllabus OverviewDocument48 pagesAerospace Propulsion Course Outcomes and Syllabus OverviewRukmani Devi100% (2)
- St. Helen Church: 4106 Mountain St. Beamsville, ON L0R 1B7Document5 pagesSt. Helen Church: 4106 Mountain St. Beamsville, ON L0R 1B7sthelenscatholicNo ratings yet
- Pines City Colleges: College of NursingDocument2 pagesPines City Colleges: College of NursingmagisasamundoNo ratings yet
- Test Initial Engleza A 8a Cu Matrice Si BaremDocument4 pagesTest Initial Engleza A 8a Cu Matrice Si BaremTatiana BeileșenNo ratings yet
- Eng CBLDocument2 pagesEng CBLMengTangNo ratings yet
- NGOs Affiliated To SWCDocument2,555 pagesNGOs Affiliated To SWCMandip marasiniNo ratings yet
- Official Correspondence in English CompleteDocument55 pagesOfficial Correspondence in English Completeyadab rautNo ratings yet
- Council Of Architecture Scale Of ChargesDocument4 pagesCouncil Of Architecture Scale Of ChargesAshwin RajendranNo ratings yet
- Diagnostic Test in Mapeh 8: Department of EducationDocument4 pagesDiagnostic Test in Mapeh 8: Department of Educationcarl jayNo ratings yet
- Repeaters XE PDFDocument12 pagesRepeaters XE PDFenzzo molinariNo ratings yet
- Csd88584Q5Dc 40-V Half-Bridge Nexfet Power Block: 1 Features 3 DescriptionDocument26 pagesCsd88584Q5Dc 40-V Half-Bridge Nexfet Power Block: 1 Features 3 DescriptionJ. Carlos RGNo ratings yet
- Fernández Kelly - Death in Mexican Folk CultureDocument21 pagesFernández Kelly - Death in Mexican Folk CultureantoniadelateNo ratings yet
- Sar Oumad Zemestoun v01b Music Score سر اومد زمستون، نت موسیقیDocument1 pageSar Oumad Zemestoun v01b Music Score سر اومد زمستون، نت موسیقیPayman Akhlaghi (پیمان اخلاقی)100% (3)
- Slope StabilityDocument11 pagesSlope StabilityAhmed MohebNo ratings yet
- Chemistry The Molecular Science 5th Edition Moore Solutions Manual 1Document36 pagesChemistry The Molecular Science 5th Edition Moore Solutions Manual 1josephandersonxqwbynfjzk100% (27)
- Manoj KR - KakatiDocument5 pagesManoj KR - Kakatimanoj kakatiNo ratings yet
- Lived Experiences of Science Teachers of Pangasinan Ii in The New Normal Education: A Phenomenological StudyDocument10 pagesLived Experiences of Science Teachers of Pangasinan Ii in The New Normal Education: A Phenomenological StudyIJAR JOURNALNo ratings yet
- Magical Industrial RevolutionDocument156 pagesMagical Industrial RevolutionUgly Panda100% (12)
- Air India CpioDocument5 pagesAir India CpioVicky GautamNo ratings yet
- Commissioning Procedure for JTB-PEPCDocument17 pagesCommissioning Procedure for JTB-PEPCelif maghfirohNo ratings yet
- 3DO For IPDocument7 pages3DO For IPHannah Angela NiñoNo ratings yet
- Ict Lesson 2 Lesson PlanDocument3 pagesIct Lesson 2 Lesson Planapi-279616721No ratings yet
- The Art of Communication PDFDocument3 pagesThe Art of Communication PDFHung Tran JamesNo ratings yet
- HAF F16 ManualDocument513 pagesHAF F16 Manualgreekm4dn3ss86% (7)
- Mock-B1 Writing ReadingDocument6 pagesMock-B1 Writing ReadingAnonymous 0uBSrduoNo ratings yet
- Art 1207-1257 CCDocument5 pagesArt 1207-1257 CCRubz JeanNo ratings yet
- Bioorganic Chemistry: Yagyesh Kapoor, Kapil Kumar TDocument25 pagesBioorganic Chemistry: Yagyesh Kapoor, Kapil Kumar TAlexandru SavaNo ratings yet
- MR GMAT Combinatorics+Probability 6EDocument176 pagesMR GMAT Combinatorics+Probability 6EKsifounon KsifounouNo ratings yet