Professional Documents
Culture Documents
Triage
Uploaded by
Sarah GuintoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Triage
Uploaded by
Sarah GuintoCopyright:
Available Formats
TRIAGE: - To sort - Medical needs and urgency of each individual patient - Sorting based on limited data acquisition - Consider
resource availability MILITARY VS CIVILIAN Military Priority is to get as many soldiers back into actions as possible serious wounds -> the first treatment priority
Civilian Priority is to maximize the survival of the greatest number of victims those with the most serious but realistically salvageable injuries are treated first
In both models, victims with lethal injuries or unlikely to survive even with extensive resource application are treated as the lowest priority ETHICAL JUSTIFICATION Utilitarian rule - Greater good of the greater number rather than particular good of the patient at hand. - Justified only because of clear necessity of general public welfare in a crisis Why should responders care about good triage? - Provides a way to draw organization out of chaos - Helps to get care to those who need it and will benefit from it the most - Helps in resource allocation - Provides an objective framework for stressful and emotional decisions Importance of Resources - Disaster is commonly defined as an incident in which patient care needs overwhelm local response resources - Daily emergency care is not usually constrained by resource availability Abundant resources relative to demand (R Patient) *Resources challenged Daily emergencies - do the best for each individual Disaster Settings - Do the greatest good for the greatest number. Maximize survival rate Triage is a dynamic process and id usually done more than once I. Primary Disaster Triage (PRIORITIZATION) Goal: - to sort patients based on probable needs for immediate care - To recognize futility Assumptions: - Medical needs outstrip immediately available resources - Additional resources will become available with time Triage based on physiology: - How well the patient is able to utilize their own resources to deal with their injuries - Which conditions will benefit the most from the expenditure of limited resources
The most commonly used adult tool in US and Canada is START tool (Simple Triage and Rapid Treatment) The only recognized pediatric MCI primary triage tool is the JumpSTART tool Other tools exist but are used for small
Basic Disaster Life Support www.dmou.org MASS Triage (Move, Assess, Sort, Send) - Assessment guidelines - Pediatric considerations - No MCI primary triage tool validated II. Secondary Disaster Triage (ALLOCATING RESOURCES) Goal: to nest match patients current and anticipated needs with available resources Incorporates - A reassessment of physiology - Assess Physical injuries - Initial treatment and assessment of patient response - Further knowledge of resource availability SAVE Tool (Secondary Assessment of Victim Endpoint) California EMS NATO Guidelines (Traffic lights) Red - Immediate priority - Airway obstructions, Cardiorespiratory failure, significant ext hemorrhage, shock, sucking chest wound, burns of face and neck Yellow - Delayed - Open thoracic wound, penetrating abdominal wound, severe eye injury, avascular limb fractures, significant burns other than face, neck or perineum Green - Minor, Walking wounded - Minor lacerations, contusions, sprains, superficial burns, partial thickness burns less 20% BSA Black - Expectant or dead, No vital signs - Head injury with GCS less 8, burns 85% BSA, multisystem trauma, massive blood loss - Provide comfort care Secondary Triage Goal: Identify victims - Needing life saving treatment, can only be provided in hospital settings - Need life saving treatment initially available on scene - With moderate non-life threatening, at risk for delayed complications - With minor injuries III. Tertiary Disaster Triage
Goal: Optimize individual outcome Incorporates: - Sophisticated assessment and treatment - Further assessment of available medical resources - Determination of best venue for definitive care MCI Triage Key points: - Resources and patient number acuity are limiting factors - No definite tool used
START TRIAGE
RPM R 30 P 2 M Can do Modification for nonambulatory children - Developmentally unable to walk and disabled do not force to walk (-_-) Duh of course. - Assess using JumpSTART - Tag depending on the applicable criteria Green, Yellow, Red, Black
What about WMD (Weapons of Mass Destruction) There is no widely recognized civilian MCI triage tool used in the US for any NRBC agents Must consider decontamination: - Who goes first? - What stage does triage take place? - Difficulty of conducting patient assessment and care with responders in protective gear WMD Triage Challenges (Weapons of Mass Destruction) - Agents of attack may be mixed. How do you triage victims who have injuries from a conventional attack in addition to a chemical or radiological/nuclear exposure? - NIological agents may impact fiel triage mostly in choice of destination facility (quarantine hospital) - Patterns of EMS calls may assist in identification of a occult biological agent attack or natural epidemic - Biosurveillance tool - Some agents cause toxindromes that allow or prediction of outcome based on presenting symptoms and signs - Agent-specific triage is dependent upon identification or strong suspicion of agents use - Very difficult to train and maintain readiness with multiple agent-specific triage schemes
Chemical Toxindrome Examples Nerve Agent: - Red: severe distress, seizure, signs in two or more systems (neuro, GI, respi excluding eyes and nose) - Black: pulseless or apneic, unless intensive resources are available Phosgene and vesicants: - Red: moderate to sever RD, only when intensive resources are immediately available - Black: burns >50% BSA form liquid exposure, signs of more than minimal pulmonary involvement, when intensive resources are available Cyanide Displaces oxygen hypoxia - Red: active seizure, recent onset of apnea with preserved circulation - Black: no palpable pulse http://www.bordeninstitute.army.mil/cwbw/CH14.pdf Key points about MCI triage - anything that can help organize the response to an MCI is a good thing - MCI triage Is different than daily triage, in both field and ED settings - Resource availability is the limiting factor to consider in MCI triage - All victims must have equal importance at the time of primary triage, this includes children - Disaster research agendas should include efforts to validate and improve existing triage tools www.jumpstarttriage.com Managing MCI - Loss of lives results from inefficient mobilization of resources - The community is the first to provide emergency assistance during emergencies and disasters resulting in large number of injuries - Attention was given to the training for emergency personnel in first aid or first responders - First responders were trained to provide victims with basic triage and field care before evacuation to the nearest health facility Ozone Disco Tragedy 1996 Lung Center Fire 1998 Manor Hall incident 200MCI defined as an event resulting in a bumber of victims large enough to disrupt the normal course of emergency and health care services - Low impact - High impact - Terrorism The most sophisticated approach, including pre-established procedures for resource mobilization, field management and hospital reception Impact Zone Field/Pre-hospital management (utilize resource mobilization) Hospital Reception and Management
MIC Management First Responders first medically trained responder to arrive on the scene Second Responders vital to the restoration of the disaster sites FIRST RESPONDERS - Bureau of Fire - National Security - Emergency Medical Services SECOND RESPONDERS - Skilled construction workers - Police - Fire - Volunteers - Other responders Characteristics: - Incorporates linkages between field and health care facilities through a command post GOAL: Good of the majority (utilitarianism) Challenges: - Availability of resources - Efficiency of responders LEGAL BASIS - Department of Health A.O. 155 2004 o Known as Implementing Guidelines for Managing Mass Casualty Incidents during Emergencies and Disasters o Reduce possible loss of life and prevent disability in cases of MCI o Components: Operations and Dispathc Field Management Safety Measures Victim Management MANAGING MASS GATHERINGS Preparing for Mass Gatherings 1. Risk Assessment 2. Surveillance (How will we know when it happens) 3. Response (what will we do when it happens) Establish partnerships
Mass gatherings can cause: - Increase in the level of existing risks - Pose entirely new risks Major anticipated health risks: - Heat or cold related illness - Foodborne and waterborne illnesses
Communicable diseases Accidents and Injuries INJURIES AND PANIC RELATED, Trauma GI Heart problem
Strategies to reduce risks - Mass gatherings make responding to illnesses and injuries more difficult - Challenges in risk reduction includes: o Greater than usual movement of people o More interaction among large numbers of people in confined areas o Greater impact and stress on local infrastructure systems o Higher levels of chaors and confusion
You might also like
- Uterine Myoma Case Study Group A FinalDocument88 pagesUterine Myoma Case Study Group A Finallowell cerezoNo ratings yet
- GROUP 3 - CASE STUDY - TraumaDocument5 pagesGROUP 3 - CASE STUDY - TraumaDinarkram Rabreca EculNo ratings yet
- Cushing's SyndromeDocument5 pagesCushing's SyndromesummerduskNo ratings yet
- Pathophysiology of Shock Sepsis and Organ Failure PDFDocument1,179 pagesPathophysiology of Shock Sepsis and Organ Failure PDFNotInterested100% (1)
- What Is TriagingDocument5 pagesWhat Is TriagingshairaNo ratings yet
- Metabolic EmergenciesDocument53 pagesMetabolic EmergenciesWengel Redkiss100% (1)
- NCP CvaDocument7 pagesNCP CvaEmerson SilverioNo ratings yet
- Anecdotal ReportDocument12 pagesAnecdotal ReportNikko PayawalNo ratings yet
- The human gastrointestinal system explainedDocument31 pagesThe human gastrointestinal system explainedEen AliNo ratings yet
- Nursing Diagnosis, Interventions, and Evaluation for AnxietyDocument6 pagesNursing Diagnosis, Interventions, and Evaluation for AnxietyShreshthi VermaNo ratings yet
- Gordon's health patternsDocument5 pagesGordon's health patternsnerlynNo ratings yet
- Acute Respiratory Distress Syndrome (ARDS): Causes, Symptoms and TreatmentDocument30 pagesAcute Respiratory Distress Syndrome (ARDS): Causes, Symptoms and TreatmentOya Zuraini KamalNo ratings yet
- Risk For Decreased Cardiac Tissue PerfusionDocument3 pagesRisk For Decreased Cardiac Tissue PerfusionKarina MadriagaNo ratings yet
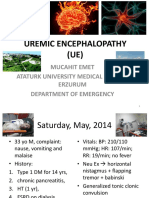
- Uremic EncephalophatyDocument48 pagesUremic EncephalophatySindi LadayaNo ratings yet
- Case Study Medical WardDocument4 pagesCase Study Medical WardFrancis Antonio Llenaresas QuijanoNo ratings yet
- DX Fracture PDFDocument8 pagesDX Fracture PDFSherree HayesNo ratings yet
- Sample Charting PDFDocument2 pagesSample Charting PDFjeffersonswallNo ratings yet
- Acute Pancreatitis - Practice Essentials, Background, PathophysiologyDocument18 pagesAcute Pancreatitis - Practice Essentials, Background, PathophysiologyInês BipNo ratings yet
- Patient Information From Your Surgeon & Sages Laparoscopic Gallbladder RemovalDocument5 pagesPatient Information From Your Surgeon & Sages Laparoscopic Gallbladder RemovalolarrozaNo ratings yet
- Hyperosmolar Hyperglycemic State (HHS)Document21 pagesHyperosmolar Hyperglycemic State (HHS)Malueth AnguiNo ratings yet
- Pregnancy and Newborn ReviewDocument3 pagesPregnancy and Newborn ReviewKATHERINE GRACE JOSENo ratings yet
- Lesson 3 Patient Classification SystemDocument22 pagesLesson 3 Patient Classification SystemTanya WilliamsNo ratings yet
- Thoracentesis Reflective EssayDocument2 pagesThoracentesis Reflective EssayAnjae GariandoNo ratings yet
- Film Analysis: in Health Care Ethics (NR-NUR127)Document5 pagesFilm Analysis: in Health Care Ethics (NR-NUR127)John MagtibayNo ratings yet
- Managing Hypertension to Prevent ComplicationsDocument10 pagesManaging Hypertension to Prevent ComplicationsArabylle Maranca AbuelNo ratings yet
- 13 Areas Patient Assessment UnconsciousDocument3 pages13 Areas Patient Assessment UnconsciousChristiany Racho SalduaNo ratings yet
- Altered Urinary Elimination - ADPCN Resource UnitDocument5 pagesAltered Urinary Elimination - ADPCN Resource UnitChillette FarraronsNo ratings yet
- Risk For SuicideDocument3 pagesRisk For SuicidepamfiestaNo ratings yet
- Growth and DevelopmentDocument5 pagesGrowth and DevelopmentGabrielLopezNo ratings yet
- NCP - Self-Concept RT Body Image (Pott's Dse)Document3 pagesNCP - Self-Concept RT Body Image (Pott's Dse)yanny03No ratings yet
- Glasgow Coma ScaleDocument13 pagesGlasgow Coma ScaleDanna Christine Gumboc PaguntalanNo ratings yet
- Gastrointestinal SystemDocument17 pagesGastrointestinal SystempreetNo ratings yet
- Disaster Nursing - Icn Position and Recommendation - Rotone, Lycah v. - BSN 4yb-4Document3 pagesDisaster Nursing - Icn Position and Recommendation - Rotone, Lycah v. - BSN 4yb-4Lycah RotoneNo ratings yet
- Moira Mae B. Balite BSN 2A: Post Partum Care DefinitionDocument5 pagesMoira Mae B. Balite BSN 2A: Post Partum Care DefinitionMoiraMaeBeridoBaliteNo ratings yet
- Medical-Surgical Nursing 3Document2 pagesMedical-Surgical Nursing 3Charissa Magistrado De LeonNo ratings yet
- De Sagun, Leila Camille, A. NCMB312-RLE BSN3Y1-1B Course Task #1Document1 pageDe Sagun, Leila Camille, A. NCMB312-RLE BSN3Y1-1B Course Task #1Carl SantosNo ratings yet
- Urgent Care Clinic Improves Patient Flow by 30 MinutesDocument2 pagesUrgent Care Clinic Improves Patient Flow by 30 MinuteselonaNo ratings yet
- Dr. H. Achmad Fuadi, SPB-KBD, MkesDocument47 pagesDr. H. Achmad Fuadi, SPB-KBD, MkesytreiiaaNo ratings yet
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodDocument5 pagesTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellNo ratings yet
- NCP 1Document3 pagesNCP 1kat2111993No ratings yet
- NCP - Impaired Gas Exchange (COPD)Document3 pagesNCP - Impaired Gas Exchange (COPD)Karen Joy ItoNo ratings yet
- NCM 118 Medsurg EndtermDocument25 pagesNCM 118 Medsurg EndtermJmarie Brillantes PopiocoNo ratings yet
- Pathophysiology of Diabetes MellitusDocument2 pagesPathophysiology of Diabetes MellitusShelly_Ann_Del_9959No ratings yet
- Compre Ho PsychDocument114 pagesCompre Ho PsychRyan Mae Tutor GarciaNo ratings yet
- Leptospirosis CaseDocument29 pagesLeptospirosis CaseJp RectraNo ratings yet
- Patho Sheet For Hypovolemic ShockDocument3 pagesPatho Sheet For Hypovolemic ShockAnnie JohnsonNo ratings yet
- St. Ferdinand College Provides Education on Musculoskeletal DisordersDocument12 pagesSt. Ferdinand College Provides Education on Musculoskeletal DisordersSteve EstebanNo ratings yet
- PRC Form (Minor Operation)Document1 pagePRC Form (Minor Operation)mawelNo ratings yet
- Nursing Care Plans for Fever, Rashes & Knowledge DeficitDocument10 pagesNursing Care Plans for Fever, Rashes & Knowledge DeficitRobin HaliliNo ratings yet
- NCPDocument9 pagesNCPLeolene Grace BautistaNo ratings yet
- Management of Acute Gastroenteritis in ChildrenDocument14 pagesManagement of Acute Gastroenteritis in ChildrenYayaNo ratings yet
- Q A 1Document48 pagesQ A 1ChannelGNo ratings yet
- VerA Ok-Prelim Ncm104 (Autosaved) VeraDocument30 pagesVerA Ok-Prelim Ncm104 (Autosaved) Verajesperdomincilbayaua100% (1)
- Sample PSADocument4 pagesSample PSAjudssalangsangNo ratings yet
- Hemorrhagic Cerebro Vascular DiseaseDocument37 pagesHemorrhagic Cerebro Vascular Diseasejbvaldez100% (1)
- Aplastic Anemia: Rare Blood Disorder Causes FatigueDocument11 pagesAplastic Anemia: Rare Blood Disorder Causes FatigueToni Shiraishi-Aque RuizNo ratings yet
- Case Report GBSDocument31 pagesCase Report GBSAde MayashitaNo ratings yet
- TRIAGE PRINCIPLES FOR MASS CASUALTY INCIDENTSDocument8 pagesTRIAGE PRINCIPLES FOR MASS CASUALTY INCIDENTSdeaaannnnnnNo ratings yet
- Mass Casualty IncidentDocument41 pagesMass Casualty IncidentCristel De TorresNo ratings yet
- Republic of The Philippines Professional Regulation Commission ManilaDocument20 pagesRepublic of The Philippines Professional Regulation Commission Manilawallyboy_casugaNo ratings yet
- The Aquino Health Agenda: Achieving Universal Health Care For All FilipinosDocument9 pagesThe Aquino Health Agenda: Achieving Universal Health Care For All FilipinosAlbert DomingoNo ratings yet
- Nursing Leadership and ManagementDocument283 pagesNursing Leadership and ManagementRuth Jazelle MendozaNo ratings yet
- Jose P. Laurel and Wartime PhilippinesDocument28 pagesJose P. Laurel and Wartime PhilippinesSarah GuintoNo ratings yet
- TMC Cadi Press Release RFID Baby TaggingDocument4 pagesTMC Cadi Press Release RFID Baby TaggingmeboniteerNo ratings yet
- 197 SiPAP BrochureDocument2 pages197 SiPAP BrochureAndrei IonutNo ratings yet
- Schizophrenia and Biblical Counseling Notes Doc-DrDocument4 pagesSchizophrenia and Biblical Counseling Notes Doc-DrJulio Cezar de Pinho Jr.No ratings yet
- Management of Surgical HemostasisDocument71 pagesManagement of Surgical HemostasisbogdanotiNo ratings yet
- Spina Bifida OCCULTADocument1 pageSpina Bifida OCCULTArebelswanteddot_comNo ratings yet
- SV300 Service Training-Basic V1.0Document82 pagesSV300 Service Training-Basic V1.0WALTER HUGO GOMEZNo ratings yet
- Schizophrenia TreatmentDocument6 pagesSchizophrenia TreatmentMichNo ratings yet
- Beltran, Justin KyleDocument4 pagesBeltran, Justin KyleKYLENo ratings yet
- Self Medication Bagi PasienDocument12 pagesSelf Medication Bagi PasienrychieqNo ratings yet
- Approach To Hypoglycemia in Infants and Children - UpToDateDocument19 pagesApproach To Hypoglycemia in Infants and Children - UpToDateOmar Nayef TaaniNo ratings yet
- FibromyalgiaDocument85 pagesFibromyalgiamariuscornel100% (1)
- Sarnat 1976Document10 pagesSarnat 1976João Paulo RaposoNo ratings yet
- Patient Safety Incident Report Form SummaryDocument9 pagesPatient Safety Incident Report Form SummaryJhun SantiagoNo ratings yet
- Beck Depression InventoryDocument2 pagesBeck Depression InventorySami Ullah Khan Niazi100% (1)
- AP Psych Midterm Study Guide 09-10 ObjDocument4 pagesAP Psych Midterm Study Guide 09-10 Objmrsaborges0% (1)
- Comparison of Icd 10 and DSM 5: BY Anitha J I Mphil Clinical PsychologyDocument102 pagesComparison of Icd 10 and DSM 5: BY Anitha J I Mphil Clinical Psychologyanitha1118No ratings yet
- Hyperkalemia Approach AND Management: Dr. Renuka RayanaDocument38 pagesHyperkalemia Approach AND Management: Dr. Renuka RayanaSap ModulesNo ratings yet
- Resume ChelDocument3 pagesResume ChelChristine Joy Ilao PasnoNo ratings yet
- SchizophreniaDocument4 pagesSchizophreniaapi-315897191No ratings yet
- Book 44 - Non VerbalDocument103 pagesBook 44 - Non VerbalcamcromanceNo ratings yet
- Perinatal AuditDocument11 pagesPerinatal AuditGladys SusantyNo ratings yet
- HW 1 PathoDocument4 pagesHW 1 PathoBryan RallomaNo ratings yet
- ASA Statement on Anesthesia DocumentationDocument3 pagesASA Statement on Anesthesia DocumentationAzaria WNo ratings yet
- Endocrinology Part 1Document131 pagesEndocrinology Part 1LucjaNo ratings yet
- Board Exam Compilation Book 2Document163 pagesBoard Exam Compilation Book 2Aaron Cy Untalan100% (6)
- Recommendation For Management of Diabetes During Ramadan:: How To Achieve Glycemic Control and SafetyDocument45 pagesRecommendation For Management of Diabetes During Ramadan:: How To Achieve Glycemic Control and SafetyLilianPrasetyaNo ratings yet
- Drug Dosage Calculations: Abbreviations Commonly Used in DosageDocument3 pagesDrug Dosage Calculations: Abbreviations Commonly Used in DosageShannen Kix OrtegaNo ratings yet
- Resume Only 2018Document2 pagesResume Only 2018api-430903191No ratings yet
- Treating Tetanus with InterventionDocument2 pagesTreating Tetanus with InterventionChristopher John Aguelo100% (3)
- DAFTAR HARGA PRODUK OGB DEXADocument3 pagesDAFTAR HARGA PRODUK OGB DEXAklinik medikamuliaNo ratings yet