Professional Documents
Culture Documents
Abdominal Pain
Uploaded by
sammy_d6Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abdominal Pain
Uploaded by
sammy_d6Copyright:
Available Formats
Abdominal Pain
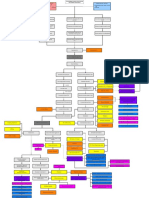
Anatomy GI Tract (oesophag us, stomach, small bowel, large bowel) Cause Gastroenteritis (gastric flu) Clinical Features Diffuse pain Usually associated with nausea/vomiting and diarrhoea May be associated with dehydration, fever, headaches, haematochezia Acute symptoms (lasts 1-6 days) May be associated with improperly prepared foods, contaminated water or travel to area of poor sanitation Diffuse umbilical pain in early stages Moves to RIF later (McBurneys point 1/3 between right ASIS and umbilicus) Pain may be in right flank, right hypochondrium, epigastric or umbilical depending on site and size of appendix May be associated with reduced appetite, nausea, vomiting, fever Peritonitis (guarding, rebound tenderness, percussion tenderness, Rovsings sign) often present Rare prior to age 2, most common age 10-30 May be asymptomatic Important Investigations Dx on history and examination Stool M/C/S if fever, haematochezia or diarrhoes lasting > 2 weeks (for Clostrium difficile, Salmonella, Shigella, Campylobacter, E. coli, parasites, ova, cysts) If symptoms inconclusive, rule out other causes (see conditions below) Management Usually self-limiting Treat dehydration if present o Replace fluids and electrolytes (orally if possible) Anti-emetics if needed Antibiotics if bacterial (must be proven with stool sample) Analgesia Fluid rescusitation IV antibiotics (gram negative and anaerobes) Antiemetics if needed Appendicectomy (lap or open) ASAP
Acute appendicitis (rarely chronic)
Gastritis
Dx on history and examination FBE raised WCC U&E if severe vomiting bHCG rule out ectopic pregnancy CRP - raised Urinalysis to exclude UTI Blood type and crossmatch (possibly need surgery) If needed: o Abdo CT in adults o Abdo ultrasound (free fluid collection in RIF; better in kids)
FBE anaemia?
Depends on cause
Epigastric or left hypochondrium pain (vague or sharp) Associtated with loss of appetite, nausea and vomiting May be associated with malaena or haematemesis Can be acute or chronic
LFT, U&E, lipase to rule out other aetiology H. pylori tests (blood, stool, biopsy) Abdo xray rule out other aetiology Stool sample faecol occult blood Endoscopy +/- biopsy
Oesophagitis and Gastrooesophageal reflux disease (GORD)
Epigastric pain radiating up towards the throat after eating (heartburn & regurgitation) Burning sensation after certain foods/drinks Pain worse when lying flat Commonly dysphagia May be odynophagia, water brash, nausea
Endoscopy +/- biopsy differentiate between infectious causes, look for oesophageal strictures, hiatus hernia, inflammation, Barretts oesophagus, adenocarcinoma Barium swallow x-ray FBE anaemia? 24 hr oesophageal pH monitoring
FBE raised WCC CRP - raised Abdo CT usually diagnostic Blood type and crossmatch (if surgery likely)
Diverticulitis
Sigmoid diverticulitis left flank or LIF pain (most common) Caecal diverticulitis has RIF or right flank pain (rarer) Associated with bloating, fever, nausea and vomiting, loss of appetite, diarrhoea/constipation
Cease causative medication o Reduce alcohol Antacids H2 antagonists (tidine) PPIs (prazole) o Depends on severity Lifestyle o Limit alcohol and smoking o Small regular meals, dont eat late at night o Weight loss o Dont sleep lying flat Antacids H2 antagonists (tidine) PPIs (prazole) Surgery lap fundoplication to strenthgen LOS Analgesia Bowel rest (nil by mouth) Antibiotics Surgery (if complicated or recurring attacks) usually done 6 weeks
Meckels diverticulitis (2% population, 2 feet from ileocaecal valve, 2 inches long, 2% symptomatic, 2 years age onset, 2x more boys) Crohns disease (IBD) any part of GI tract mouth to anus, patchy RIF, LIF, right flank, left flank, umbilical pain Pain may be diffuse Usually chronic picture May be associated with diarrhoea, haematochezia, malaena, bloating, steatorrhoea Other possible signs: perianal skin tags, anal pain/itchiness, aphthous mouth ulcers, growth failure in kids, FBE raised WCC, anaemia? U&E, coags, glucose for any GI bleed Abdo x-ray (other causes, obstruction) Stool M/C/S to rule out other bleeding causes Technetium-99m pertechnetate scan (shows gastric cells distal to stomach) Barium enema if unsure Blood type and crossmatch (possibly need surgery) FBE and film anaemia? Thrombocytosis? U&E effects of chronic diarrhoea (low K and Mg) B12 if anaemic CRP and ESR Abdo x-ray look for obstruction Urinalysis Stool M/C/S rule out infectious causes
RIF pain Age around 2 years Painless malaena May mimic acute appendicitis May be associated with reduced appetite, nausea, vomiting, fever May be bowel obstruction, volvulus, intussesception
after acute attack; or as emergency procedure in rupture; resection and anastomosis, or resection with colostomy (lifethreatening cases, Hartmanns) Once healed, increase fibre intake to reduce further attacks Surgery resection of MD (along with adjacent bowel segment in complicated cases)
Antibiotics (acute phase) Aminosalicylates (mesalazine) and corticosteroids (acute phase) Surgery for complications (e.g. fistula, stricture) Immune modulators
fever, weight loss, loss of appetite, uveitis, episcleritis, seronegative arthritis, skin lesions, DVT, PE, clubbing, osteoporosis, anaemia
Mesenteric adenitis (inflammation of mesenteric LN RIF pain but may be more diffuse More likely in children and adolescents
Ulcerative colitis (IBD) starts in rectum, goes proximally
LIF, left flank, umbilical pain Pain may be diffuse Usually chronic picture Usually diarrhoea mixed with mucous and blood May be weight loss, joint pain, tenesmus (ineffective and painful straining), fever, growth failure in kids, aphthous mouth ulcers, iritis, uveitis, episcleritis, seronegative arthritis, skin lesions, DVT, PE, clubbing, osteoporosis, anaemia, primary sclerosing cholangitis
Colonoscopy and biopsy (diagnostic) transmurual inflammation, patchy, cobblestones, granulomas Capsule endoscopy (if proximal to distal small bowel) Barium enema x-ray for seeing strictures, fistulas ASCA and ANCA antibodies positive ASCA, IgG, IgA; negative atypical ANCA FBE and film anaemia? Thrombocytosis? U&E effects of chronic diarrhoea (low K and Mg) LFTs bile duct involvement? CRP and ESR Abdo x-ray look for toxic megacolon, obstruction Urinalysis Stool M/C/S rule out infectious causes Flexible sigmoidoscopy and biopsy (diagnostic) distorted crypts, crypt inflmmation, shallow, mucosal Colonoscopy if dx unclear ASCA and ANCA antibodies positive atypical ANCA, negative ASCA Blood type and crossmatch (if surgery likely) FBE raised WCC U&E if severe vomiting CRP raised
long term Lifestyle: o Stop smoking o Proper diet, hydrate, low fibre No cure
Depends on severity and extent Aminosalicylates (mesalazine) Corticosteroids (acute phase) Immune modulators Nicotine patch?! Surgery (curative) in severe cases and complications colectomy with ileostomy or colectomy with ileal-anal pouch Lifestyle: o Proper diet, hydrate, low fibre o Broad spectrum antibiotics Supportive care
in abdomen)
Can mimic acute appendicitis Often preceded with sore throat, URTI Often fever May be diarrhoea, malaise, anorexia, nausea and vomiting Peritonitis (guarding, rebound tenderness, percussion tenderness) often present Acute presentation Diffuse crampy, intermittent pain central and mid-abdominal Often nausea and vomiting, may be constipation More acute presentation usually than LBO Diarrhoea (early sign) Abdominal distension Hyperactive bowel sounds early, hypoactive bowel sounds later Incarcerated hernia excluded May be fever or tachycardia if strangulation Often previous abdo surgery in history May be history of cancer (esp. ovarian or colonic) Peritionitis symptoms if perforation
Small bowel obstruction (adhesions, tumour, hernia, intussusceptio n (kids))
Serology to look for causative organisms Urinalysis to exclude UTI Blood M/C/S prior to prescribing ABx Abdo CT with contrast large LN, more widely distributed than appendicitis, normal appendix Abdo ultrasound excluding other aetiology such as enteritis Laparotomy LN specimen showing inflammation FBE WCC may be raised, raised haematocrit in dehydration Creatinine dehydration LDH Urinalysis Blood type and cross-match (possibly need surgery) LFTs exclude biliary/hepatic aetiology Chest xray (upright) air fluid levels perforation? Abdo x-ray (supine and upright) useful in simple obstruction airfluid levels, dilated SB loops, absent or minimal large bowel gas Barium swallow x-ray if plain xray normal, AVOID if perforation suspected (Ba causes peritonitis) Abdo CT if x-ray inconclusive, can differentiate many causes, used in very sick patients as first line
hydration, analgesia after excluding need for acute surgery Surgery if suppuration or abscess, or peritonitis, or if acute appendicitis cannot be excluded with certainty laparotomy, appendicectomy
Fluid resuscitation Analgesia Anti-emetics Antibiotics gram negative and anaerobes NG tube suction (decompress bowel) IDENTIFY CAUSE If pt not improving in 2-5 days, surgery may be needed to remove cause, or resection
Large bowel obstruction (adhesions, constipation, tumour, hernia, volvulus, intussusceptio n (kids), haemorrhoids, IBD)
Incarcerated (non-reducible) or strangulated (compromised blood supply) hernia
Colorectal cancer
Diffuse crampy, intermittent pain lower abdomen, central, spasms last longer Often constipation (absent flatus or bowel movement), may be nausea and vomiting Longer presentation usually than SBO Abdominal distension Abdomen hyper-resonant to percussion Hyperactive bowel sounds early, hypoactive bowel sounds later Incarcerated hernia excluded May be fever or tachycardia if strangulation Often previous abdo surgery in history May be history of cancer (esp. ovarian or colonic) Peritonitis symptoms if perforation Incarcerated: visible hernia (not obturator), non-reducible, may not be painful, sx of bowel obstruction (N&V, constipation) Strangulated: systemic toxicity, pain persists on reduction, pain out of proportion to exam findings, sx of bowel obstruction (N&V, constipation) Risk factors heavy lifting, obesity, male, very young or middle-aged, straining, COPD, ascites, FHx Change in bowel habit, tesesmus, haematemesis, mucous in stool,
FBE WCC may be raised, raised haematocrit in dehydration Creatinine dehydration LDH Urinalysis Blood type and cross-match (possibly need surgery) LFTs exclude biliary/hepatic aetiology Chest xray (upright) air fluid levels perforation? Abdo x-ray (supine and upright) useful in simple obstruction airfluid levels, dilated LB Barium enema x-ray if plain x-ray normal, AVOID if perforation suspected (Ba causes peritonitis)
Fluid resuscitation Analgesia Anti-emetics Antibiotics gram negative and anaerobes NG tube suction (decompress bowel) Surgery often needed to treat cause: carcinoma, diverticulitis, volvulus, intussusception
FBE raised WCC with left shift in strangulation U&E, creatinine if vomiting Urinalysis exclude urinary causes Chest x-ray (upright) free air = perforation Abdo x-ray (supine and upright) sns of SBO Ultrasound for obturator hernia
Analgesia Fluid resuscitation Surgical emergency reduce, repair weakness in muscle tissue, resection if necessary
Rectal examination mass, blood, mucous
Depends on stage Surgery polyp
Peptic/duoden al ulcer
Lactose intolerance Coeliac disease
faecal occult blood, malaena, sxs of bowel obstruction (N&V, constipation, abdo distension, pain), sxs of perforation (peritonitis), palpable mass, sns of anaemia, weight loss, decreased appetite, DVT, paraneoplastic syndromes, PUO Risk factors: increasing age, PHx polyps, PHx cancer, FHx, smoking, high meat, low veg diet, IBD, alcohol Epigastric pain radiating up towards the throat (heartburn & regurgitation) Food relieves duodenal ulcers, exacerbates gastric ulcers Pain whilst eating in gastric ulcer, pain 2-3 hrs after eating with duodenal ulcer Associated with bloating, waterbrash, nausea, copius vomiting, loss of appetite, loss of weight, haematemesis, malaena Perforation: sudden intense peritonitis pain Hx of GORD, heartburn or some medications (NSAIDS, COXI, glucocorticoids) Diffuse abdo pain Associated with bloating, flatulence, diarrhoea, nausea and acid reflux Pale, loose, greasy stool (steatorrhoea) and diarrhoea Weight loss or failure of weight
FBE anaemia? (Bleeding, iron deficiency, chronic disease) LFTs liver mets? Faecal occult blood test Colonoscopy with biopsy (stage 0IV)
removal, bowel resection Chemotherapy Radiotherapy
Dx often made on history and examination FBE anaemia? H. pylori tests (breath, urine, blood) Chest x-ray free air = perforation Gastroscopy - diagnostic Endoscopy +/- biopsy differentiate exclude cancer and if Rx unsuccessful after a few weeks Barium swallow x-ray
Non-acidic foods Antacids H2 antagonists (tidine) If H. pylori 2 antibiotics (clarithromycin, amoxicillin, tetracycline, metronidazole) + PPI (prazole) and sometimes bismuth compound Perforation = surgical emergency: repair of perforation Avoid lactose (dairy) Lactase supplements Gluten-free diet
Hydrogen breath test (overnight fast, lactose in morning) Lactose challenge tests FBE anaemia? Iron studies, folic acid, B12 Calcium, vitamin D
Irritable bowel syndrome
gain, fatigue Diffuse abdo pain with cramping, distension May be clubbing, mouth ulcers, osteopenia (calcium and vit D malabsorption), coagulation problems (vit K deficiency), recurrent miscarriage or unexplained infertility, abnormal LFTs Anaemia (iron deficiency, folic acid and B12 deficiency) May be other autoimmune disorders Chronic or acute onset (with infection) Diarrhoea and/or constipation Diffuse abdo pain May be urgency, tenesmus, bloating, GORD, genitourinary sx, chronic fatigue, psychiatric symptoms
Celiac serology and IgA (tissue transgluaminase antibody (tTG) and antiendomysial antibodies (EMA)) Endoscopy with biopsy (gold standard) reduced SB folds, mosaic mucosa, prominent submucosal blood vessels, nodular mucosa Thyroid function tests DXA scanning for osteoporosis
Gall bladder/bil e ducts
Acute cholecystitis
Right hypochondrium, occasionally epigastric pain, radiates around right side to back Constant, severe pain (biliary colic if obstruction of cystic duct) May be referred to right scapula May be worse after fatty foods May be associated with fever,
Diagnosis of exclusion Rule out: parasitic infection, lactose intolerance, celiac disease Stool M/C/S FBE, LFTs, ESR, serology for celiac disease Abdo ultrasound looking for gallstones and biliary tract disease Endoscopy with biopsy exclude peptic ulcer disease, celiac disease, IBD, malignancy Hydrogen breath testing exclude lactose and fructose intolerance LFTs may be raised ALP or bilirubin FBE high WCC CRP raised Lipase and amylase pancreatitis? Ultrasound of gallbladder and ducts (gall stones, sonographic Murphys sign, wall thickening >3mm,
Soluble fibre supplementation Stool softeners and laxatives in constipation-dominant Anti-diarrhoeals in diarrhoea-dominant Serotonin agonists (C)/antagonists (D) Antispasmodics Antidepressants
Analgesia Fluid rescusitation IV antibiotics (broad spectrum and anaerobes) Antiemetics if needed Cholecystectomy (lap or open) ASAP
Chronic cholecystitis
diarrhoea, nausea, vomiting, steatorrhoea, jaundice Murphys sign positive Risk factors: fs Nausea, belching, diarrhoea Vague abdominal pain Risk factors: fs
Choledocholith iasis Right hypochondrium or epigastric pain Colicky pain (CBD obstruction) Obstructive jaundice Murphys sign positive Steatorrhoea NO fever (if present means ascending cholangitis) Risk factors: fs Charcots triad: RUQ pain, fever, jaundice May be low BP, confusion
pericholecystic fluid, gallbladder dilatation) CT cannot see non-calcified calculi LFTs may be raised ALP or bilirubin FBE high WCC CRP raised Lipase and amylase pancreatitis? Ultrasound of gallbladder and ducts (gall stones, sonographic Murphys sign, wall thickening >3mm, pericholecystic fluid, gallbladder dilatation) CT cannot see non-calcified calculi LFTs raised serum bilirubin, high conjugated bilirubin, raised GGT and ALP Lipase and amylase pancreatitis? Ultrasound gall bladder stones, ERCP, MRCP or intraoperative cholangiogram
Analgesia Fluid rescusitation IV antibiotics (broad spectrum and anaerobes) Antiemetics if needed Cholecystectomy (lap or open) ASAP
ERCP to remove stone and sphincterotomy Cholecystectomy once symptoms have resolved
Ascending cholangitis (infection of entire biliary tree usually due to bile duct obstruction)
LFTs ALT, AST, ALP and GGT raised, raised bilirubin FBE high WCC CRP raised Blood cultures Ultrasound dilated bile ducts, may find stones, differentiates btn cholangitis and cholecystitis ERCP or MRCP +/- bile culture
Medical emergency Fluid rescusitation IV antibiotics (broad spectrum and anaerobes) for 7-10 days ERCP unblockage of bile duct (remove strone) and
Chronic hepatitis (longer than 6 months) FBE may be raised WCC, haemolysis, pancytopaenia LFTs raised ALT, AST, raised bilirubin (GGT raised a lot more than ALP?) Albumin Coagulation screen (PT) Anti-HAV IgM, HBsAg, Anti-HBc, Anti-HBs, Anti-HCV Liver ultrasound if needed Liver biopsy if needed FBE may be raised WCC, haemolysis, pancytopaenia LFTs raised ALT, AST, raised bilirubin (GGT raised a lot more than ALP?) Albumin Coagulation screen (PT) Anti-HAV IgM, HBsAg, Anti-HBc, Anti-HBs, Anti-HCV Liver ultrasound if needed Liver biopsy if needed FBE raised WCC, anaemia of chronic disease LFTs low albumin, raised ALP, may be elevated AST/ALT or
Liver
Acute hepatitis (less than 6 months)
Liver abscess
Diffuse abdo pain Jaundice Anorexia (loss of appetite), aversion to smoking in smokers Tender hepatomegaly in 10% Non-specific: malaise, joint pain, muscle aches, fever, nausea, vomiting, diarrhoea, headache Hepatic encephalopathy or coma, bleeding (no vit K) if liver failure Risks: IVDU, sexual contact, travel history Non-specific: malaise, tiredness, weakness Often asymptomatic (dx on blood tests) Jaundice severe damage May be hepatomegaly Cirrhosis: bleeding, weight loss, peripheral oedema, ascites, oesophageal varices, hepatic encephalopathy, hepatorenal syndrome Risks: IVDU, sexual contact, travel history Right hypochondrium pain (common) or diffuse Steatorrhoea, dark urine, fever, chills, loss of appetite, nausea,
sphincterotomy +/stent Cholecystectomy once symptoms have resolved IDENTIFY CAUSE: hepatitis virus, alcohol, medications, plants, solvents, other infections, autoimmune Fluid rescusitation Antiemetics if needed Interferon or lamivudine for hep B, interferon for hep C Liver transplant in severe cases IDENTIFY CAUSE: hepatitis virus, alcohol, medications, plants, solvents, other infections, autoimmune Fluid rescusitation Antiemetics if needed Interferon or lamivudine for hep B, interferon for hep C Liver transplant in severe cases Antibiotics for 4-6 weeks Percutanous drainage of abscess or surgical
vomiting, weight loss, weakness, jaundice, cough due to diaphragm irritation, tender hepatomegaly, hepatic friction rub
Congestive hepatomegaly
Pancreas
Acute pancreatitis
Right hypochondrium pain with hepatomegaly Other signs of right-sided heart failure dyspnoea, wheezing, wet cough, ascites, peripheral oedema, prominent veins, oesophageal varices, abnormal heart sounds Jaundice, coagulopathy Pain can be diffuse, epigastric or left hypochondrium Pain radiates through to back (like stab wound) Associated with nausea and vomiting, sweating, increased HR and RR, increased BP, decreased BP if bleeding, ileus (absent bowel sounds), jaundice, malnutrition Sudden, lasts a few days Causes: idiopathic, gallstones, ethanol, trauma, steroids, mumps, autoimmune, scoprion sting,
bilirubin Blood cultures Chest x-ray basal atelectasis, right hemidiaphragm raised, right pleural effusion Abdo CT with contrast (95-100% sensitivity) well-demarcated hypodense area Abdo ultrasound (80-90% sensitivity) hypoechoic mass Gallium and technetium studies Percutaneous needle aspiration under CT - culture of abscess fluid (diagnostic) LFTs raised ALT, AST, bilirubin U&E Chest x-ray ECG Echocardiogram General full work up For diagnosis, 2 of: characteristic abdo pain, serum amylase or lipase > 3 times normal, characteristic CT findings Amylase Lipase (preferred) U&E LFTs Abdo CT or abdo ultrasound
removal
Treat underlying heart/lung problem
Analgesia (morphine) Fluid resuscitation (IV) Nil by mouth Monitor for complications ERCP in gallstone pancreatitis In necrotising pancreatitis, start imipenem or other Abx
Chronic pancreatitis
hypercalcaemia, hypertriglyceridaemia, hypothermia, ERCP, drugs (azathioprine, diuretics) Pain can be diffuse, epigastric or left hypochondrium May be worse with eating or drinking alcohol May be associated with chronic weight loss, loss of appetite, diarrhoea, nausea, vomiting, steatorrhoea Occurs over many years
Pancreatic abscess
Spleen
Splenic rupture
Abdominal mass Abdominal pain Chills, fever Loss of appetite Nausea and vomiting Hx of pancreatits Left hypochondrium pain, may be referred to left shoulder With free blood, may be diffuse abdo pain, peritonitis and rebound tenderness May be signs of shock: tachycardia, tachypnoea, restlessness, anxiety, decreased pulse pressure, decreased capillary return
For diagnosis, 2 of: characteristic abdo pain, serum amylase or lipase > 3 times normal, characteristic CT findings Amylase Lipase (preferred) Faecal fat test Serum IgG4 (autoimmune pancreatitis) Serum trypsinogen U&E LFTs Abdo CT Abdo ultrasound ERCP or MRCP FBE raised WCC Blood cultures Abdo CT Abdo MRI Abdo ultrasound FBE anaemia? Focussed abdominal sonographic technique (FAST) or Diagnostic peritoneal lavage (DPL) free intraperitoneal fluid? Abdo CT with contrast Exploratory laparotomy
Analgesia (morphine) Fluid resuscitation (IV) Nil by mouth Nasogastric sunctioning Insulin for diabetes ERCP in gallstone pancreatitis Pancreas may need to be removed
Antibiotics Percutanous drainage or surgery to drain and remove abscess
IV fluids Blood transfusion if needed Splenic angioembolisation (if available) Laparotomy and splenic repair or splenectomy in
Splenic abscess
Hypotension is a grave sign Left hypochondrium pain Fever Splenomegaly May be left shoulder pain, pleuritic chest pain at left lung base, malaise, dyspnoea, dullness at left lung base, elevated left hemidiaphragm, left basal crackles FBE raised WCC, with left shift, anaemia of chronic disease Blood cultures and sensitivities Chest x-ray basal atelectasis, left hemidiaphragm raised, left pleural effusion Abdo x-ray gas under left hemidiaphragm, abnormal soft tissue density Abdo CT with contrast (best) welldemarcated hypodense area Abdo ultrasound hypoechoic mass Percutaneous needle aspiration under CT - culture of abscess fluid (diagnostic) Urinalysis signs of UTI (nitrite, WBCs) FBE raised WCC Urine M/C/S (MSU) If kidney stone suspected, KUB xray Abdo ultrasound if anatomical abnormality suspected
haemodynamically unstable Antibiotics for 4-6 weeks (anti-fungal if needed) Percutanous or open drainage of abscess or splenectomy (open or laparoscopic)
Renal and urinary
Pyelonephritis
Cystitis
Right or left flank pain radiating to the back (may be RIF, LIF, umbilical or suprapubic depending on kidney site) High fever, dysuria May be vomiting Chronic pyelonephritis may cause fever, flank pain, weight loss, malaise, decreased appetite, dysuria, haematuria Pain in costovertebral angle on back Suprapubic pain or pressure Dysuria, polyuria, urinary urgency, nocturia
Antibiotics specific to cultures done (e.g. fluoroquinolone, cephalosporin, aminoglycoside) IV fluid resuscitation if needed
Urinalysis signs of UTI (nitrite, WBCs, RBCs) FBE raised WCC Urine M/C/S (MSU)
Antibiotics specific to cultures done (e.g. fluoroquinolone, cephalosporin, aminoglycoside)
Renal calculi or bladder or kidney tumour causing obstruction
Right or left loin to groin pain, may also be in back Colicky pain with a background pain Strong pain Urinary urgency, restlessness, haematuria, sweating, nausea, vomiting Pain in costovertebral angle on back
Urinalysis signs of UTI (nitrite, WBCs, RBCs), urinary casts, crystals FBE raised WCC U&E renal function Calcium renal function Urine M/C/S (MSU) 24 hr urine collection: urine volume, Mg, Na, uric acid, Ca, citrate, oxalate, phosphate KUB x-ray calcium-containing stones (60%) Non-contrast abdo CT (best) Kidney ultrasound hydronephrosis, radiolucent stones
Urinary retention
Suprapubic pain or pressure Poor urinary stream, straining, incomplete voiding, hesitancy, nocturia, urinary incontinence, frequency Bladder distended on percussion Anuria is a medical emergecny
Urinalysis signs of UTI? Serum PSA U&E and creatinine kidney failure? Bladder ultrasound slow flow rate, retention, distension (before and after urinating) Cytoscopy of bladder Prostate biopsy
Female reproducti ve
Pelvic inflammatory disease
Suprapubic pain Fever, new or different discharge, dyspareunia, irregular menstrual bleeding May be asymptomatic
Hard to diagnose STI screen Pelvic ultrasound dilated fallopian tubes, abscess? Laparoscopy +/- biopsy (diagnostic)
Many stones pass spontaneously Analgesia (NSAIDS, opioids) Medical expulsive therapy alpha adrenergic blockers, CCB, corticosteroids Extracorporeal shock wave lithotripsy (ESWL) to fragment uncomplicated stones Ureterscopic surgery +/- stent placement Surgery +/chemotherapy & radiotherapy for tumour if neoplastic Indwelling catheter Prostatic stent IDENTIFY CAUSE (BPH, nerve dysfunction, constipation, infection, medication, prostate cancer) o Prostatectomy, TURP5-alphareductase inhibitor No cure once damage done Antibiotics Treating partners for STIs
Ovarian torsion
Hx of PID, recent sexual contact, recent onset of menses, IUD, partner has an STI RIF or LIF pain, sudden onset, severe, may radiate to back, thigh or pelvis, may be bilateral Associated with nausea and vomiting, fever (necrosis) Onset often during exercise or agitating movement Any age, but usually early reproductive years Suprapubic, RIF or LIF or pelvic pain midway through menstrual cycle, cramping, sharp, may switch sides each month Can last hours, or until next cycle Suprapubic pain, cramping. May be bilateral, in lower back and rectal area, down thighs and legs Typically in reproductive years May be associated with infertility, dysmenorrhoea, dyspareunia, dysuria May be constipation, chronic fatigue, long/heavy periods, fever, headaches, depression, diarrhoea Suprapubic pain or discomfort Abnormal gynaecological bleeding, heavy or painful periods, abdo bloating, painful defication, back ache, urinary frequency or retention, and sometimes infertility
Mittelschmerz (mid-cycle pain with ovulation)
Endometriosis (ectopic endometrial cells)
Urine and serum bHCG rule out ectopic pregnancy Urinalysis, blood cultures rule out other causes Doppler ultrasound blood flow, ovarian enlargement, impaired venous/lymphatic drainage, ovarian cyst? Abdo CT ruling out other causes Laparoscopy Diagnosis made if mid-cycle and no pelvic abnormalities Pelvic examination Abdo ultrasound Pelvic ultrasound free fluid, endometrial cysts, large endometrial areas Pelvic MRI free fluid, endometrial cysts, large endometrial areas Laparoscopy with biopsy (gold standard)
Analgesia Antiemetics if needed Fluid rescucitation if prolonged vomiting Laparoscopy uncoiling of ovary with surgical fixation to pelvic wall Ovary resection if necrosis has occurred Analgesia Hormonal contraception to prevent ovulation Analgesia Surgical removal of endometrial tissue Hormones to suppress natural cycle Fertility medication/IVF
Uterine fibroids (benign myometrial tumour)
FBE anaemia? Iron studies iron deficiency? Pelvic examination can feel large fibroids Pelvic ultrasound focal mass with heterogenous texture, causing
Not treated unless symptomatic Medications to control symptoms or shrink tumour NSAIDS, OCP, IUD, hormonal
May cause miscarriage, bleeding, premature birth in pregnancy May be asymptomatic Rarely grow in women before puberty or after menopause In 30-40% women over 40, mostly asymptomatic
shadowing Pelvic MRI can also be used Hysteroscope Malignant uterine leiomyosarcomas are very rare, therefore fibroids are usually assumed to be benign unless theres fast growth after menopause, or obvious invasion Uncertainty after ultrasound and MRI, surgery is indicated
Ovarian cyst
Ovarian cancer
RIF, LIF, vaginal, suprapubic pain dull aching or sudden sharp pain or discomfort; may radiate to back or thighs; may be constant or intermittent Abdominal bloating/distension May be associated with breast tenderness, irregular periods, abnormal uterine bleeding or spotting, menstrual pain, urinary changes, constipation, weight gain, nausea and vomiting, fatigue, infertility May be asymptomatic Most common during childbearing years May be RIF, LIF, suprapubic or pelvic pain or discomfort May be abdominal mass, bloating/ascites, back pain, urinary urgency, constipation tiredness,
Pelvic ultrasound or pelvic CT Biopsy if FHx of ovarian cancer
Ultrasound fibroid destruction Surgical methods to reduce blood supply to fibroid arterial embolisation Myomectomy (fibroid removal) Hysterectomy Antibiotics if infection Blood transfusion if severe anaemia Iron supplements if needed Analgesia paracetamol, NSAIDS, narcotics Warm bath, heat pads OCP to regulate cycle
Pelvic examination FBE U&E Urine and serum bHCG pregnancy?
Surgical excision of tumour unilateral oophorectomy, bilateral oophorectomy,
weight loss, vaginal bleeding May be subtle
CA-125 & OVA1 marker AFP, LDH in young patients malignant germ cell tumour? Transvaginal ultrasound Pelvic CT Laparotomy or laparoscopy with biopsy to confirm dx and stage
Ectopic pregnancy
Typically symptoms at 5-8 weeks RIF, LIF or suprapubic pain Early signs: may be pain, dysuria, vaginal bleeding, pain with defication Later signs: pelvic pain and bleeding (internal and external); may be shoulder pain, back pain, cramping
Male reproducti ve Testicular torsion Acute onset (<6hrs), severe testicular pain or suprapubic, RIF or LIF pain (referred from testes) Nausea and vomiting Testicle positioned higher than normal Abnormal/absent cremasteric reflex
Urine and serum bHCG FBE if bleeding U&E and LFTs kidney, liver function, electrolyte imblanace? Serum lactate if shock Urinalysis UTI? Blood group and hold, Rh factor if needed Pelvic examination Transabdominal and transvaginal pelvic ultrasound intrauterine pregnancy? Ectopic pregnancy? Failed intrauterine pregnancy? Pelvic MRI (no radiation) if theres uncertainty Laparotomy or laparoscopy if needed to confirm Testicular dopplar ultrasound if low suspicion avascular, distinguishes from epididymitis If high suspicion on history and examination, proceed to surgery
salpingectomy (fallopian tubes), hysterectomy, or debulking surgery Chemotherapy IV or IP (intraperitoneal) - for more advanced or aggressive Radiotherapy avoided in advanced stages Potential medical emergency Methotraxate if unruptured, haemodynamically stable, and normal liver, kidney and blood tests Laparoscopy or laparotomy to remove pregnancy only or tube and pregnancy
Surgical emergency Analgesia Surgery ASAP detorsion (manual, rotate outward and medial to lateral), orchiplexy, possible
Epididymitisis (acute, subacute, chronic)
Swollen testis Most common in adolescent males, but consider in all 12-30 year-olds Testicular pain, may radiate to abdomen Testicle may be warm or red Usually gradual onset
orchiectomy (testicle removal) if necrosis Urinalysis (may be abnormal) UTI? Testicular doppler ultrasound increased blood flow STI screen Urine M/C/S Syphilis, HIV tests FBE raised WCC Serum lactate - raised Abdo x-ray to exclude other aetiology, or obstruction Abdo CT greater sensitivity and specificity if SBO also present mesenteric oedema, bowel dilatation, bowel wall thickening, intramural gas, mesenteric stranding Angiography if possible (not acutely ill pt) Endoscopy with light spectroscopy to analyse capillary oxygen level Antibiotics azithromycin and cefixime (cover gonorrhoea and Chlamydia), or others based on sensitivities Analgesia Scrotal elevation and support Ischaemic coloitis can be life-threatening Fluid resuscitation if needed Oxygen if needed Analgesia (opioids) Antibiotics (broad spectrum) Surgical resection of necrotic bowel if peritonitis present Intra-arterial papaverine during angiography opioid derivative to relax vascular smooth muscle Arterial embolus embolectomy, papaverine infusion, or intra-arterial thrombolysis Arterial thrombosis
Blood vessels
Mesenteric ischaemia (small bowel ischaemia) acute or chronic
Early phase severe diffuse pain, bloody stools, nausea, vomiting, diarrhoea, tachycardia Pain progresses, more widespread, decreased bowel motility, bloating, absent bowel sounds Final shock phase metabolic acidosis, dehydration, low BP, tachycardia, confusion Chronic mesenteric ischaemia postprandial pain, weight loss Typically in older patients
FBE raised WCC Serum lactate - raised Abdo x-ray to exclude other aetiology Abdo CT other diagnoses? Complications? Angiography if possible (not acutely ill pt) Colonoscopy or flexible sigmoidoscopy with biopsy and with light spectroscopy to analyse capillary oxygen level
Ischaemic colitis (large bowel ischaemia)
Splenic infarction (thromboembol ism in splenic artery)
Diffuse abdo pain or left-sided pain out of proportion to physical findings limited focal tenderness Early phase severe diffuse pain, bloody stools, diarrhoea, fever Pain progresses, more widespread, decreased bowel motility, bloating, absent bowel sounds Final shock phase metabolic acidosis, dehydration, low BP, tachycardia, confusion Chronic mesenteric ischaemia postprandial pain, weight loss Typically in older patients Severe left hypochondrium or epigastric pain, may radiate to the left shoulder May be fevers and chills, nausea, vomiting, pleuritic chest pain May be asymptomatic Risk factors: malignancy, hypercoaguable states, sickle cell, endocarditis, AF, prosthetic valves, HIV, autoimmune collagen disorder, others
FBE anaemia? Raised WCC? Abdo CT or MRI with contrast wedge-shaped infarct Angiography if vascular lesion suspected as cause
papaverine infusion and grafting Non-occlusive papaverine Venous thrombosis heparin/warfarin, possible surgery Chronic angioplasty +/- stent, or surgical revascularisation Often resolves spontaneously Fluid resuscitation Bowel rest, nil orally Cardiac function and oxygenation optimised NG tube if ileus present Antibiotics in moderate-severe cases If worsens surgery: lapatomy and bowel resection Analgesia (NSAIDs, narcotics) Observation Splenectomy or partial splenectomy if persistent symptoms or complications (haemorrhage, abscess, rupture, persistent pseudocyst)
Aortic dissection Type A ascending aorta Type B descending aorta
Sudden onset, severe, tearing chest pain May radiate to back, thorax, flank, abdomen or groin May be syncope or stroke, peripheral nerve damage, Horners syndrome, hoarse voice, dyspnoea, haemoptysis, dysphagia, fever, anxiety Hx of hypertension
FBE may be raised WCC, anaemia? U&E - Blood-urea-nitrogen and creatinine may be raised (renal involvement) Troponin T may be raised ECG mimic AMI Urinalysis renal involvement? LDH raised Chest x-ray may be mediastinal widening, tracheal deviation or pleural effusion Chest CT with contrast (in haemodynamically stable) diagnostic TOE echo (in haemodynamically unstable) diagnostic
Abdominal aortic aneurysm 90% infrarenal
Often asymptomatic Umbilical pain, pulsates, radiates through to back, chest or scrotum Palpable, expansile abdominal mass Bruits may be present if renal or visceral artery stenosis Ruptured AAA: excruciating pain of lower back, flank, abdomen and groin; hypovolaemic shock (low BP,
FBE transfusion requirements, WCC infection? U&E surgical risk LFTs surgical risk Blood group and hold Urinalysis UTI? ECG surgical risk Arterial blood gases surgical risk Chest x-ray cardiac/lung state Abdo ultrasound size of
Left untreated, high mortality rate Admit to ICU: arterial blood pressure monitoring with arterial line, central venous pressure monitoring with central catheter, cardiac performance filling pressures, urine output monitoring Analgesia Negative ionotropes (beta blockers, calcium channel blockers if contraindicated) Hypotensives nitroprusside, labetolol, calcium channel blocker Surgery: always in type A aortic arch repair and stent, sometimes stents inserted for type B Symptomatic aneurysm = surgery o Open repair o Endovascular aneurysm repair (EVAR) Quit smoking Anti-hypertensives
tachycardia, cyanosis, altered mental state); 90% mortality Abdomina l muscles Abdominal muscle strain or trauma Abdominal or psoas abscess Site depends on site of pathology Hx of straining, exercise or trauma May be muscle spasm, oedema, bruising RIF, LIF, suprapubic or umbilical pain (depending on muscle) Fever, prolonged ileus (abdominal abscess) May be sepsis low BP, tachycardia, metabolic acidosis
aneurysm, free fluid (bad in obese, bowel gas) Abdo CT 100% sensitivity for AAA, helps surgery planning Angiography or MRI angio surgical planning Based on history and examination
Abdomina l wall
Herpes zoster (shingles, caused by varicella zoster virus VZV)
Usually single dermatomal pain burning, throbbing, stabbing Pain preceeds rash by 48-72 hours, then vesicles, bullae, crusting; resolve by 10-15 days May involve multiple dermatomes in immunocompromised
FBE raised WCC, anaemia, abnormal platelets? LFTs abnormal? Chest x-ray subphrenic or subhepatic may cause pleural effusion, elevated hemidiaphragm, atelectasis Abdo x-ray other causes, ileus, free gas, displaced viscera, mottled soft tissue masses, air-fluid levels? Abdo ultrasound Abdo CT (best) Abscess M/C/S Usually diagnosed on history and examination In complication pts, do: Tzanck smear of base of fresh vesicle multinucleated giant cells (negative test deosnt rule out VZV) Direct immunoflueorescence and PCR (can differentiate HSV and VZV) Diagnosed on history and
Apply ice Avoid causing pain to muscles Gentle stretching Antibiotics broad spectrum until sensitivities obtained Percutaneous CTguided abscess drainage Surgical drainage if needed
Usually self-limiting Analgesia Antivirals (acyclovir) Corticosteroids
Radiculitis
Dermatomal pain, numbness, pins
Rest, ice
and needles radiated from the spine due to nerve irritation
examination
Abdominal wall haematoma
Acute, sharp abdominal pain that develops over hours, worse with movement, often unilateral Palpable abdominal mass, firm, non-pulsatile Fever, nausea, vomiting, anorexia, diarrhoea, constipation, bladder irritability May be peritonitis (e.g. rebound tenderness) May be hypovolemic shock: low BP, tachycardia, confusion, pallor 2-3 times more common in females Hx of blunt trauma, surgical procedure, coughing, sneezing, constipation, exercise, anticoagulant use
FBE anaemia? Platelet count, raised WCC? Coagulation profile Blood gases if shocked Abdo CT (first line) Abdo ultrasound first line when CT contraindicated, or used to monitor in everyone Abdo MRI in chronic haematomas can differentiate from tumour Intraluminal bladder pressure measurement if abdominal compartment syndrome suspected
Analgesia NSAIDs, paracetamol Spinal manipulation May need epidural steroidal injection Treat CAUSE (disc herniation, lumbar spinal stenosis, disc disease): o Chiro/physio/m assage/yoga Haemodynamically stable: o Rest o Analgesia o Haemoatoma compression o Ice pack o Treat predisposing condition o Reversal of anticoagulation if needed o IV fluids Haemodynamically unstable: o Anticoagulatio n reversal phytonadione + FFP o Blood transfusion o Arterial embolisation
Referred from elsewhere
Lower lobe pneumonia
Pulmonary embolism
May present as right or left hypochondrium pain Associated with productive cough, fever, chills, dyspnoea, chest pain, confusion, increased RR May be vomiting, diarrhoea, central cyanosis, decreased consciousness, weight loss, night sweats Bronchial breathing, basal crackles, dullness to percussion May present as sharp right or left hypochondrium pain Associated with sudden onset of dyspnoea, tachypnoea, pleuritic chest pain, cough, haemoptysis May be cyanosis, collapse, sudden death May be pleural friction rub, pleural effusion (dull percussion), raised JVP, loud P2, fever, jaundice, ascites (R heart failure) Risk factors: proximal leg DVT, immobilisation, pregnancy, obesity, cancer, OCP, thrombophilia May present as epigastric, left or right hypochondrium pain Exertional (angina) or sudden (AMI)
Chest x-ray - consolidation FBE WCC raised U&E CRP raised LFTs Non-responders/ immunocompromised: blood and sputum cultures
Operative exploration Oral antibiotics for most IV antibiotics for hospital-acquired Antivirals if viral cause Corticosteroids in aspiration pneumonia
Ischaemic heart disease (AMI, angina)
Wells score based on clinical criteria D-dimer normal rules out PE FBE platelets, WCC Coagulation profile ESR, U&E, LFT screening Troponin T Chest x-ray rule out other causes ECG S1Q3T3, other causes CT pulmonary angiography (gold standard) V/Q scan pregnant, contrast allergy Leg Doppler ultrasound DVT? ECG Chest x-ray FBE U&E LFTs Echocardiography Coronary angiogram
Thrombolysis for massive PE Anticoagulation heparin, LMW heparin Changed to warfarin for 3-6 months or lifelong if previous DVTs or PEs
Anti-anginals Revascularistion CABG, angioplasty Address modifiable risk factors (cholesterol, BP, diabetes, smoking, diet)
Pericarditis (acute or chronic)
Systemic
Sickle cell disease crisis (genetic HbS)
May present as sudden epigastric, or left hypochondrium pain radiating to the base of left scapula Relieved by sitting up and leaning forward, worse on inspiration May be cough, fever, fatigue, anxiety Friction rub at lower left sternal border Diffuse or site specific pain (with peritonitis) due to vaso-occlusive crisis (microcirculation occlusion) Can effect any body part Hx of sickle cell disease (screening at birth)
Cardiac stress test ECG non-specific ST elevation in all leads Troponin T may be raised TOE tamponade? Aspirin or NSAIDs for viral Severe cases may need: pericardiocentesis, antibiotics, steroids, colchicine, surgery
Diabetic ketoacidosis
Polydipsia, polyuria, malaise, weakness, fatigue, nausea and vomiting, diffuse abdo pain, decreased appetite, anorexia, sweating, weight loss May be fruity breath May be altered consciousness
FBE with reticulocyte count, raised WCC U&E, LFTs Serum lactate - raised Abdo x-ray to exclude other aetiology Abdo CT with contrast infarction? other diagnoses? Complications? Angiography if possible (not acutely ill pt) Colonoscopy or flexible sigmoidoscopy or endoscopy etc with biopsy and with light spectroscopy to analyse capillary oxygen level (depends on where occlusion is) Blood glucose (fingerprick while waiting) regularly U&E regularly Blood, urea, nitrogen ABGs and bicarbonate as necessary Urinalysis glucose and ketones
Analgesia Fluid resuscitation Consider hydroxyurea if recurrent episodes Consult with patients haematologist
Medical emergency Fluid resuscitation Insulin Correct electrolyte disturbances, esp. potassium loss Correct acid-base
May be intercurrent infection fever, dysuria, coughing, malaise, chills, chest pain, dyspnoea, joint pain More common in pts younger than 19, but may be at any age Hx of diabetes with failure to comply with insulin therapy
Alcoholic ketoacidosis
Diffuse abdo pain, nausea, vomiting, dyspnoea, dizziness, muscle pain, diarrhoea, syncope, seizure, haematemesis or malaena May signs of chronic alcohol use hepatosplenomegaly, peripheral neuropathy, gynaecomastia, testicular atrophy, palmar erythema May be fruity breath May be tachypnoea from acidosis Differentiate from alcohol gastritis or pancreatitis Hx of chronic alcohol abuse with abrupt cessation 1-2 days prior to presentation
Typhoid fever
Non-specific febrile illness, fever rises during day, peaks and troughs Diffuse abdo pain, may be fierce right colicky hypochondrial pain May be constipation, dry cough,
Serum beta-hydroxybutyrate (ketone) FBE raised WCC Urine and blood cultures infection? Phosphate, Ca, Mg Chest x-ray infection? MRI brain if altered consciousness cerebral oedema? ECG DKA may cause cardiac event ABGs and bicarbonate Blood glucose (fingerprick while waiting) U&E regularly Blood, urea, nitrogen Urinalysis glucose and ketones Serum beta-hydroxybutyrate (ketone) FBE raised WCC Urine and blood cultures infection? Phosphate, Ca, Mg LFTs, amylase, lipase, LDH exclude other causes Alcohol levels Chest x-ray oesophageal rupture, aspiration? Abdo CT other causes Diagnosis mainly on history and examination Blood, bone marrow (most sensitive), vomitus, or stool culture of S typhi (repeat for confirmation)
balance (sodium bicarb) Antibiotics if infection Long-term management
Thiamine Fluid resuscitation (dextrose and saline) Correct electrolyte disturbances, esp. potassium loss Correct acid-base balance (sodium bicarb) Benzodiazepines for alcohol withdrawal if needed Long-term management
Broad spectrum antibiotics started if suspected, narrowed once diagnsosis made Oral rehydration
dull frontal headache, delerium and increasing malaise As progresses red spots, distension, splenomegaly, weight loss, conjunctivitis, pea soup rd diarrhoea, psychosis (3 week) Hx of exposure to Salmonella typhi (7-14 days before symptoms) endemic area, food prepared by someone carrying typhoid
Exclude malaria, dysentery and pneumonia FBE anaemia? WCC? Platelets? ESR, CRP raised Coagulation profile LFTs raised AST, ALT, bilirubin U&E mild low Na, K Serum ALT to LDH ratio (less than 9:1 supports typhoid hepatitis) KUB x-ray bowel perforation?
therapy if needed Contact isolation during acute phase
You might also like
- Chart - WBC DisordersDocument1 pageChart - WBC DisordersSamuel RothschildNo ratings yet
- HEART MURMURS by NISHDocument41 pagesHEART MURMURS by NISHurtikikeNo ratings yet
- ACLS Drug TherapyDocument8 pagesACLS Drug TherapySahrensNo ratings yet
- Amboss Hemolytic AnemiaDocument16 pagesAmboss Hemolytic AnemiaAhmed Ali100% (2)
- Common BleepsDocument1 pageCommon BleepsShannon RamsumairNo ratings yet
- Hepatobiliary Notes 2.0Document18 pagesHepatobiliary Notes 2.0Sri VathanahNo ratings yet
- 9 Week Usmle Study ScheduleDocument3 pages9 Week Usmle Study ScheduleChewyNo ratings yet
- DDX Gastrointestinal Disorders ChartDocument20 pagesDDX Gastrointestinal Disorders ChartDavid UribeNo ratings yet
- Acls Pharmacology OverviewDocument11 pagesAcls Pharmacology OverviewzoyaligNo ratings yet
- House MD Notes Handbook PrototypeDocument78 pagesHouse MD Notes Handbook PrototypeBea Samonte100% (2)
- 60 ItemsDocument8 pages60 Itemsdylan143No ratings yet
- Med Geeks Clinical Lab GuideDocument17 pagesMed Geeks Clinical Lab GuideHuy Hoang100% (1)
- The Intern Pocket Card Surviving GraysDocument2 pagesThe Intern Pocket Card Surviving GraysKathleen Grace ManiagoNo ratings yet
- Acute AbdomenDocument47 pagesAcute AbdomenDani LeeNo ratings yet
- Abnomalites of ECGDocument81 pagesAbnomalites of ECGgrreddy8364320No ratings yet
- GI Signs and SymptomsDocument40 pagesGI Signs and SymptomsJohnny BeeNo ratings yet
- General Surgery: (Acute Abdomen)Document1 pageGeneral Surgery: (Acute Abdomen)MattNo ratings yet
- Accordion Sign-Appearance (C. Difficile)Document41 pagesAccordion Sign-Appearance (C. Difficile)Andra HijratulNo ratings yet
- Chest RadiographyDocument19 pagesChest RadiographyClaraMonet PalomoNo ratings yet
- Chapter 41: Genitourinary Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument6 pagesChapter 41: Genitourinary Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- Examination of The AbdomenDocument2 pagesExamination of The Abdomenkenners100% (13)
- Acute Abdomen: Medic Curses A MopDocument50 pagesAcute Abdomen: Medic Curses A MopSharaz AhmedNo ratings yet
- Abdul Rahim Bin Mohamad Nor C 111 10 871: Prof - Dr.Peter Kabo, PHD, SPFK, SPJP (K), Fiha, FasccDocument38 pagesAbdul Rahim Bin Mohamad Nor C 111 10 871: Prof - Dr.Peter Kabo, PHD, SPFK, SPJP (K), Fiha, FasccAis KonorasNo ratings yet
- Preventive Health: Based On The USPSTF 2014Document42 pagesPreventive Health: Based On The USPSTF 2014Louella CarpioNo ratings yet
- Alarm Symptoms of Hematoonco in Pediatrics: Dr. Cece Alfalah, M.Biomed, Sp.A (K) Pediatric Hematology and OncologyDocument22 pagesAlarm Symptoms of Hematoonco in Pediatrics: Dr. Cece Alfalah, M.Biomed, Sp.A (K) Pediatric Hematology and OncologyMuhammad ArifNo ratings yet
- Mo Intern Handbook - FinalDocument37 pagesMo Intern Handbook - FinalGideon K. MutaiNo ratings yet
- Pathology Mcqs (4th Year)Document9 pagesPathology Mcqs (4th Year)usmandumassar100% (7)
- MNT in Diseases of Kidney and UrinaryDocument38 pagesMNT in Diseases of Kidney and UrinaryJosephine A. Bertulfo100% (1)
- Renal UltrasoundDocument179 pagesRenal UltrasoundJuhar AhamedNo ratings yet
- Assessment Test 3Document40 pagesAssessment Test 3Nathan BarrerasNo ratings yet
- Pekana European Remedy Guide: For Licensed Health Care PractitionersDocument68 pagesPekana European Remedy Guide: For Licensed Health Care PractitionersMegan Hughes100% (3)
- Valvular Heart DiseaseDocument10 pagesValvular Heart DiseaseEzyan SyaminNo ratings yet
- Source NotesDocument30 pagesSource NotesChris Jardine Li100% (1)
- 00 NephrologyDocument98 pages00 Nephrologyeryxsp0% (1)
- Pain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Document3 pagesPain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Ryan TurnerNo ratings yet
- Disorders of The BoneDocument2 pagesDisorders of The BoneRPh Krishna Chandra JagritNo ratings yet
- Cardiology Step 2 CK NotesDocument5 pagesCardiology Step 2 CK NotesVidur S SinghNo ratings yet
- Seizures in ChildrenDocument21 pagesSeizures in ChildrenTera SurbaktiNo ratings yet
- UrosepsisDocument22 pagesUrosepsisWita Ferani KartikaNo ratings yet
- Congenital Heart Defects Test Five Nursing FourDocument6 pagesCongenital Heart Defects Test Five Nursing FourTiffany D'Alessandro GordonNo ratings yet
- Nursing Care Plan PyelonephritisDocument2 pagesNursing Care Plan Pyelonephritisderic91% (33)
- Unit 8 Med Surg Study Guide NursingDocument5 pagesUnit 8 Med Surg Study Guide Nursingatl_nurse_student100% (7)
- An Approach To A Patient With JaundiceDocument48 pagesAn Approach To A Patient With JaundiceSuranga Lakshitha PereraNo ratings yet
- Gallbladder, Liver, Pancreas and SpleenDocument19 pagesGallbladder, Liver, Pancreas and Spleensarguss14100% (3)
- Urinary Tract InfectionsDocument44 pagesUrinary Tract Infectionstummalapalli venkateswara rao100% (2)
- CARAS SCUTSHEET 2nd EditDocument2 pagesCARAS SCUTSHEET 2nd EditFrances Katrina Siruno100% (1)
- Nur 111 Session 6 Sas 1Document12 pagesNur 111 Session 6 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Liver Nursing NotesDocument7 pagesLiver Nursing NotesHeather ShantaeNo ratings yet
- Hospital Follow Up Progress Note MedicalTemplateDocument1 pageHospital Follow Up Progress Note MedicalTemplatee-MedTools100% (18)
- IE - Antibiotic TableDocument5 pagesIE - Antibiotic TablemeganNo ratings yet
- Valvular Heart DiseaseDocument4 pagesValvular Heart DiseaseAfif Al BaalbakiNo ratings yet
- Ninja - Anemias PDFDocument1 pageNinja - Anemias PDFErica Hyeyeon LeeNo ratings yet
- Cystic FibrosisDocument203 pagesCystic FibrosisAren SongcoNo ratings yet
- PancreatitisDocument2 pagesPancreatitisMary GiuntiniNo ratings yet
- Step1 Review TopicsDocument32 pagesStep1 Review TopicsAsif AbidiNo ratings yet
- Urological History TakingDocument6 pagesUrological History TakingayuniNo ratings yet
- Biochemisty Cheat SheetsDocument4 pagesBiochemisty Cheat SheetsNatalie KingNo ratings yet
- Medicine Review 2018 1Document470 pagesMedicine Review 2018 1Norjetalexis Maningo CabreraNo ratings yet
- Antihypotensive Drugs: Roger Joseph Ii Ramos Jecino, RN, M.DDocument28 pagesAntihypotensive Drugs: Roger Joseph Ii Ramos Jecino, RN, M.DFranz Earl Niño AlbesaNo ratings yet
- Aquifer InternalMedicine11 - 45Document8 pagesAquifer InternalMedicine11 - 45JulieNo ratings yet
- Bone TumorsDocument15 pagesBone Tumorssarguss1450% (2)
- Notes For Clincal CasesDocument12 pagesNotes For Clincal CasesMandeepNo ratings yet
- Anemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDocument15 pagesAnemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDanielle FosterNo ratings yet
- DKA Draft 1 AM - Drawio 2Document1 pageDKA Draft 1 AM - Drawio 2Dud AccNo ratings yet
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Peptic UlcerDocument4 pagesPeptic UlcerEris Abdul AzizNo ratings yet
- Pre-Res Case Presentation: Jo Anne N. Ramos, MDDocument72 pagesPre-Res Case Presentation: Jo Anne N. Ramos, MDKah Mote KyuNo ratings yet
- Turkey Book 03 Internal Medicine PDFDocument47 pagesTurkey Book 03 Internal Medicine PDFPreaisNo ratings yet
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Renal Pathology: Kidney and The Urinary Collecting SystemDocument37 pagesRenal Pathology: Kidney and The Urinary Collecting Systemapplesncore100% (1)
- CL7 Urinary Tract Infection 20192020-20191212060056Document50 pagesCL7 Urinary Tract Infection 20192020-20191212060056Nur Ain IzzatiNo ratings yet
- Nitrofurantoin 50 and 100 MF UKPARDocument30 pagesNitrofurantoin 50 and 100 MF UKPARdivyenshah3No ratings yet
- Differential Diagnosis of Flank PainDocument43 pagesDifferential Diagnosis of Flank PainDrArish Mahmood78% (9)
- Dysplasia & Multicystic KidneyDocument8 pagesDysplasia & Multicystic KidneyShintia MalindaNo ratings yet
- Urinary Tract Infection Thesis PDFDocument8 pagesUrinary Tract Infection Thesis PDFdwrxjhgr100% (2)
- Section 1 Functional Disturbances and Diseases of Kidneys: DR - Damodar SedaiDocument82 pagesSection 1 Functional Disturbances and Diseases of Kidneys: DR - Damodar SedaiShreeya SharmaNo ratings yet
- Sandoz LTD Levofloxacin 500 MG Film-Coated Tablet: by Adeyanju Patrick at 4:19 PM, Sep 05, 2011Document8 pagesSandoz LTD Levofloxacin 500 MG Film-Coated Tablet: by Adeyanju Patrick at 4:19 PM, Sep 05, 2011afsala1982No ratings yet
- Med. Forum, Vol. 32, No.3 March, 2021Document185 pagesMed. Forum, Vol. 32, No.3 March, 2021jhoselinNo ratings yet
- World's Largest Science, Technology & Medicine Open Access Book PublisherDocument27 pagesWorld's Largest Science, Technology & Medicine Open Access Book PublisherAngela StellaNo ratings yet
- Candiduria: Evidence-Based Approach To Management, Are We There Yet?Document10 pagesCandiduria: Evidence-Based Approach To Management, Are We There Yet?ntnquynhproNo ratings yet
- LP PyleonephritisDocument7 pagesLP PyleonephritisAnonymous 0C4OZmRNo ratings yet
- Probiotics For Preventing Urinary Tract Infections in Adults and Children - Schwenger, EM - 2015 - Cochrane LibraryDocument21 pagesProbiotics For Preventing Urinary Tract Infections in Adults and Children - Schwenger, EM - 2015 - Cochrane LibraryMixcy MabatidNo ratings yet
- ACute Pylonephris Case PresentationDocument6 pagesACute Pylonephris Case PresentationbantilanNo ratings yet
- Referat UtiDocument20 pagesReferat UtiYeni Rosa SitohangNo ratings yet
- Resume MedisDocument4 pagesResume MedisJauhari AttabraniNo ratings yet
- Acute Pyelonephritis: Causes/ Risk FactorsDocument6 pagesAcute Pyelonephritis: Causes/ Risk FactorsShiraishiNo ratings yet
- Urology HX and ExamDocument31 pagesUrology HX and ExamMisbah KaleemNo ratings yet
- Aminoglycoside Guidance Document 20200424Document6 pagesAminoglycoside Guidance Document 20200424Marcelo UGNo ratings yet
- Guias NICE IVU QUICKDocument16 pagesGuias NICE IVU QUICKJorge Esteban Camacho TéllezNo ratings yet