Professional Documents
Culture Documents
Case Study Ortho
Uploaded by
joshua_santiago_5Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Study Ortho
Uploaded by
joshua_santiago_5Copyright:
Available Formats
New Era University College of Nursing
In Partial Fulfillment for the Requirements in Philippine Orthopedic Center
A Case Study on Septic ankle left
Submitted by: Santiago, Joshua M
BSN Group. 3 A.Y. 2011-2012
Introduction Swelling of the feet and ankles can occur as a result of conditions involving the local extremities as well as systemic conditions (diseases and conditions that affect the entire body). Localized processes such as injuries and infections may lead to a swollen foot and/or ankle only on the involved side. Swelling of the ankle on one side is often a result of sprains or strains. Sometimes diseases that affect the entire body, such as heart disease and kidney or liver failure, can result in excess fluid buildup (edema) that is often concentrated in the legs and feet, leading to swelling not only of the ankles but also of the feet and lower legs. This can also occur with obstruction of the venous system, as may occur with pregnancy and obesity. Diseases of the joints, such as arthritis, can also affect the joints of the ankle and foot, leading to swelling of the involved areas. Treatments for swollen ankles and feet depend on the particular cause, but antiinflammatory medications are often used to manage the pain associated with strains and sprains Infection is an unusual cause of ankle swelling. Infections can either occur in the soft tissues around the ankle joint (cellulitis) or in the joint itself (septic joint). Infections can often be treated with medications alone, but may also require surgery.
II.
BIOGRAPHIC DATA Name: J.B.I Address: Bulacan Age: 2 years old Gender: male Race: Filipino Marital Status: Single Religious Orientation: Roman Catholic Date of Admission: October 1, 2011 at 10:00pm
III.
CHIEF COMPLAINT OR REASON FOR VISIT Left ankle swelling
IV.
NURSING HISTORY History of Present Illness 14 days prior to admission, Patient had chicken pox infection associated with progression of left ankle swelling. It was noted to be warm and tender to touch. Patient was also noted to have difficulty in bearing weight on left lower extremities. Fever was also noted 10 days prior to admission. Patient prompted consult with local hospital wherein oral antibiotics were given and provided relief of fever only 1 day prior to admission, there is still persistent symptoms where they consulted with another hospital where in doctor diagnosed this as to consider septic bone left. Patient was advised arthrotomy ankle but not done due to financial problem History of past illness Patient has chicken pox. No known allergies to food and medications Family history There are known hypertension in their family according to the grandmother of the patient
Anatomy and physiology The ankle and foot are incredibly complex, with a variety of connecting bones, ligaments, tendons and muscles. The ankle is made up of two joints: The ankle joint and the subtalar joint. The ankle joint includes two bones (the tibia and the fibula) that form a joint that allows the foot to bend up and down. Two bones of the foot (the talus and the calcaneus) connect to make the subtalar joint that allows the foot to move side to side. The tarsal bones connect to the 5 long bones of the foot - the metatarsals. Ligaments and Tendons The large Achilles tendon is the most important tendon for walking, running and jumping. It attaches the calf muscles to the heel bone to allow us to puch off and up on the toes. There are
another 12 tendons that cross the ankle. They are responsible for movements of the ankle, foot, and toes; some of these tendons also help support the arches of the foot. Muscles The muscles of the foot are classified as intrinsic and extrinsic. The intrinsic muscles are located within the foot and cause movement of the toes and are flexors (plantar flexors), extensors (dorsiflexors), abductors, and adductors of the toes. Several intrinsic muscles also help support the arches of the foot. The extrinsic muscles are located outside the foot, in the lower leg. The gastrocnemius muscle (calf) is the largest. They have long tendons that cross the ankle, to attach on the bones of the foot and assist movement.
Pathophysiology
Modifiable Factors Trauma
Non-Modifiable Factors Physical active persons
Trauma or open wound
Microorganism gain entry
Immunity response
Increased WBC
White blood cells attack microorganisms through phagocytosis
Inflammatory response
Redness, localized pain and swelling
Formation of localized dead cells
White blood cells still recognized this as foreign object
Laboratory Name of test HEMATOLOGY hemoglobin October 11,2011 Date done October 5 ,2011 Indication The Hb determination is part of a CBC. It is used to screen for disease associated with anemia, to determine the severity of anemia, to monitor the response to treatment for anemia, and to evaluate polycythemia. (A manual of laboratory and diagnostic test p74) Iron deficiency, thalassemia, pernicious anemia, hemoglobinopathies (A manual of laboratory and diagnostic test p7475) 93 gms/L Result 80 gms/L Normal 127183gms/L Significance Decreased Hb levels are found in anemia states (a condition in which there is a reduction of Hb, Hct, and/or RBC values)
HCT
October 5 ,2011
The Hct test is part of the CBC. This test indirectly measures the RBC mass. It is
.25gms/L
0.37-0.54 gms/L
Decreased Hct values are an indicator of anemia, a condition in which there is a reduction in the PVC. An Hct <30% (<0.30) means that the patient is moderately to severely anemic. Decreased values
October 11,2011
an important measurement in the determination of anemia or polycythemia. (A manual of laboratory and diagnostic test p69)
.28 gms/L .
also occur in the following conditions: Acute and chronic blood loss Hemolytic reaction (A manual of laboratory and diagnostic test p72) Leukocyte count October 5 ,2011 The WBC serves as a useful guide to the severity of the disease process. Specific October 11,2011 patterns of leukocyte response can be expected in various types of diseases as determined by the differential count (percentages of the different types of leukocytes). (A manual of laboratory and diagnostic test p48) Segmenters October 5 ,2011 0.60 0.50-0.70 7.20x109L 9.10x109L 4.510x109L The findings are normal
October 11,2011 LYMPHOCYTES October 5 ,2011 This test measures the number of lymphocytes in the peripheral blood October 11,2011 (A manual of laboratory and
0.32 0.30 0.20-0.40 Lymphopenia Aplastic anemia 0.55 (A manual of
diagnostic test p60)
laboratory and diagnostic test p61)
Monocytes
October 5 ,2011
October 11,2011
This test counts monocytes, which circulate in certain specific conditions such as tuberculosis, subacute bacterial endocarditis, and the recovery phase of acute infections.
0.08
0.00-0.07
The findings are normal
0.07
Eosinophils
October 5 ,2011
October 11,2011
This test is used to diagnose allergic infections, assess severity of infestations with worms and other large parasites, and monitor response to treatment.
0.02
0.00-0.05
Increased eosinophils: allergic states, drug sensitivity
0.06
reaction, skin disorders, tissue invasion by parasites, periarteritis nodosa, hypersensitivity response to malignancy (e.g. Hodgkin's disease), pulmonary infiltrative disease, disseminated eosinophilic hypersensitivity disease.
Platelet
October 5 ,2011
A platelet count is a test to measure how many platelets you have in your blood.
363
150400X109/L
The findings are normal
October 11,2011
Platelets help the blood clot. They are smaller than red or
353
white blood cells. MCV October 5 ,2011 Average volume of the red cell is measured by automated instrument, by electrical October 11,2011 impedance or by light scatter. 78 77 82-92 fl Decreased in: Iron deficiency, thalassemia; decreased or normal in anemia of chronic disease. MCH October 5 ,2011 MCH calculated from measured values of Hb and RBC; ie, MCH = Hb/RBC. A October 11,2011 low MCH can mean hypochromia or microcytosis or both. A high MCH is evidence of macrocytosis MCHC October 5 ,2011 MCHC describes how fully the erythrocyte volume is filled with hemoglobin and is October 11,2011 calculated from measurement of hemoglobin (Hb), mean corpuscular corpuscular volume (MCV) and red cell count (RBC); ie, MCHC = Hb/MCV x RBC. 33 32 32-38% 26 Aplastic anemia (A manual of laboratory and diagnostic test p61) 25 28-32 pg Lymphopenia
The findings are normal
WOUND GRAM STAINING AND CULTURE SENSITIVITY TEST GS: RBC-- ++, NO MICROORGANISM SEEN AFB: NO ACID FAST BACILLI SEEN
DRUG ORDER (Generic name, dosage, route, frequency, etc.) PARACETAMOL NSAIDS 200mg/ml IV q4 TID
TRADE / BRAND NAME
PHARMACOLOGIC ACTION OF DRUG
INDICATIONS AND CONTRAINDICATION S
ADVERSE EFFECTS OF THE DRUG
DESIRED ACTION ON YOUR CLIENT The patients fever will return to the normal range of temperature
NURSING RESPONSIBILITIES/ PRECAUTIONS Note prescribed dosage and expected outcomes Monitor CBC, liver and renal function studies Document presence of fever, onset and the duration Check for urine for occult blood
paracetamol
Decreases fever by INDICATIONS ahypothalamic effect Control of pain due to leading to sweating headache, earache, and vasodilation and To reduce fever in inhibits the effect of bacterial or viral pyrogens on the infections hypothalamic heatCONTRAINDICATION regulating centers. S May cause analgesia Renal insufficiency, by inhibiting CNS anemia. Clients with prostaglandin cardiac or pulmonary synthesis; however, disease are more due to minimal effects susceptible to on peripheral acetominophen toxicity prostaglandin synthesis, acetaminophen has no anti-inflammatory or uricosuric effects. Does not cause any anticoagulant effect or ulceration of the GI tract. antipyretic and analgesic effects are comparable to those of aspirin.
Chronic and even acute toxicity can develop after long symptom-free usage. Hematologic: methemoglobinemia, hemolytic anemia, neutropenia, thrombocytopenia, pancytopenia, leucopenia Allergic: urticarial and erythematous skin reactions, skin eruptions, fever. Miscellaneous: CNS stimulation, hypoglycemic coma, jaundice, drowsiness, glossitis. Possible liver damage in those who consume three or more alcoholic drinks daily
DRUG ORDER (Generic name, dosage, route, frequency, etc.)
TRADE / BRAND NAME
PHARMACOLOGIC ACTION OF DRUG
INDICATIONS AND CONTRAINDICATION S indication infections caused by sensitive staphylococci, streptococci, pneumococci, bacteroides, and other sensitive aerobic and anaerobic organisms. Contraindication -contraindicated in patients hypersensitive to drug or lincomycin -use cautiously in patients with renal or hepatic disease, asthma, history of GI disease, or significant allergies
ADVERSE EFFECTS OF THE DRUG
DESIRED ACTION ON YOUR CLIENT The patient will have a decrease signs of infections
NURSING RESPONSIBILITIES/ PRECAUTIONS -assess patients infection before and regularly throughout therapy -before giving first dose, obtain specimen for culture and sensitivity test, begin therapy pending results. -monitor renal, hepatic, and hematopoetic functions during prolonged therapy. -be alert for adverse reactions -tell patient to take entire amount prescribed even after he feels better. -tell patient receiving drug to report discomfort
Clindamycin antibiotic 100g IV q8H ANST
- inhibits bacterial protein synthesis by binding to 50S subunit of ribosome.
- hinders or kills susceptible bacteria.
CNS: headache CV: Thrombophlebitis EENT: pharyngitis GI: abdominal pain, Anorexia, bloody or tarry stools, constipation, diarrhea, dysphagia, esophagitis, flatulence, nausea, psuedomembranus colitis, unpleasant or bitter taste, vomiting. GU: UTI HEMATOLOGIC: Eosinophilia, thrombocytopenia, transient leukopenia SKIN: maculopapular rash, urticaria OTHER: anaphylaxis, erythema, pain (I.V. use), induration, pain; sterile abcess (I.M. use)
DRUG ORDER (Generic name, dosage, route, frequency, etc.)
TRADE / BRAND NAME
PHARMACOLOGIC ACTION OF DRUG
INDICATIONS AND CONTRAINDICATION S Indication To relieve bronchospasm associated with acute or chronic asthma,bronchitis, or other reversible obstructive airway diseases. Also used toprevent exerciseinduced bronchospas m. Contraindication Contraindicated in patients hypersensitive to drug or its ingredients.
ADVERSE EFFECTS OF THE DRUG
DESIRED ACTION ON YOUR CLIENT The patient will be able to loosen his/her secretions
NURSING RESPONSIBILITIES/ PRECAUTIONS Drug may decrease sensitivity of spirometry used for diagnosis of asthma. When switching patient from regular to extendedrelease tablets,remember that a regular 2-mg tablet every 6 hours is equivalent toan extended-release 4mg tablet every 12 hours. Syrup contains no alcohol or sugar and may be taken by children as young as age 2. In children, syrup may rarely cause erythema multiforme or Stevens-Johnson syndrome
salbutamol bronchodilator 1 neb + 1cc PNSS q6
reduce chemical mediator release from pulmonary mast cells and improve ability of cilia to clear mucus direct-acting agent that relaxes smooth muscle walls of the bronchi, uterus, and skeletal muscle vascular bed
CNS: tremor, nervousness, dizziness, insomnia, headache, hyperactivity, weakness, CNS stimulation, malaise. CV: tachycardia, palpitations, hypertension. EENT: dry and irritated nose and throat with inhaled form, nasal congestion, epistaxis, hoarseness. GI: heartburn, nausea, vomiting, anorexia, altered taste, increased appetite. Metabolic: hypokalemia. Musculoskeletal: muscle cramps. Respiratory: bronchospasm, cough, wheezing, dyspnea, bronchitis, increased sputum. Other: hypersensitivity reactions
DRUG ORDER (Generic name, dosage, route, frequency, etc.)
TRADE / BRAND NAME
PHARMACOLOGIC ACTION OF DRUG
INDICATIONS AND CONTRAINDICATION S Indication Prevention and treatment of iron deficiency anemias. Dietary supplement for iron. Contraindication Hypersensitivity Severe hypotension.
ADVERSE EFFECTS OF THE DRUG
DESIRED ACTION ON YOUR CLIENT The patient will have an increase of HGB and HCT
NURSING RESPONSIBILITIES/ PRECAUTIONS Advise patient to take medicine as prescribed. Caution patient to make position changes slowly to minimize orhtostatic hypotension. Instruct patient to avoid concurrent use of alcohol or OTC medicine without consulting the physician. Advise patient to consult physician if irregular heartbeat, dyspnea, swelling of hands and feet and hypotension occurs. Encourage patient to comply with additional intervention for hypertension like proper diet, regular exercise, lifestyle changes and stress management.
Ferrous sulfate
- Elevates the serum iron concentration which then helps to form High or trapped in the reticuloendothelial cells for storage and eventual conversion to a usable form of iron.
Dizziness Nasuea and vomiting Nasal Congestion Dyspnea Hypotension Muscle cramps Flushing
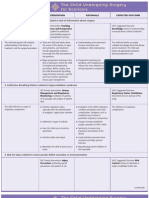
CUES
NURSING DIAGNOSIS
GOALS AND OBJECTIVES
NURSING INTERVENTIONS Evaluate current limitations/degree of deficit in light of usual status. Ascertain ability to stand and move about and degree of assistance necessary/use of equipment Adjust activities to prevent overexertion. Reduce intensity level or discontinue activities that cause undesired physiological changes. Plan care with rest periods between activities to reduce fatigue. Involve client/SO(s) in planning of activities as much as possible. Assist with activities and provide/monitor clients use of assistive
EVALUATION
Objective: Sitting in the wheel chair Limited leg movemen t
Impaired physical mobility of the lower extremity r/t surgical incision at the left leg
Goal After 1-2 days of nursing interventions, client will be able to demonstrates and verbalizes proper exercises of the lower extremities & can perform activities of daily living with Minimal assistance. Objectives: 1.participate willingly in the necessary activities 2. demonstrate a increase in physical mobility 3. Use identified techniques to enhance mobility
GOAL MET
After 1-2 days of nursing interventions, client was able to demonstrates and verbalizes proper exercises of the lower extremities & can perform activities of daily living with Minimal assistance as evidenced by: Using of wheel chair by himself Was able to perform simple activities such as eating and combing hair by himself
devices (crutches, walker, wheelchair, oxygen tank, etc.) to protect client from injury. Increase exercise/activity levels gradually; teach methods to conserve energy, such as stopping to rest for 3 minutes during a 10-minute walk, sitting down instead of standing to brush hair.
CUES
NURSING DIAGNOSIS
GOALS AND OBJECTIVES
NURSING INTERVENTIONS INDEPENDENT 1. Assess clients muscle strength gross and fine motor coordination
EVALUATION
Risk for injury Objective: Age: 2 yrs old
Goal After 1-2 days of nursing intervention the client will be free from injury. Objectives: After 2 hours of nursing intervention the client will be given instruction carefully to be able to reduce the risk for injury through attaining safe environment:
GOAL MET
2. Assess mood, coping abilities, personality styles ( e.g. temperament aggressions impulsive behavior, level of self- esteem )
After 1-2 days of nursing intervention the client was free from any injury as evidenced by: Always with support of the significant others Always insight of the significant others
3. Provide safe environment:
- padded side rails - watch door edges curbs and landing steps
pad side rails remove obstacles in the room
4. Discuss important of self monitoring of conditions / emotions
Discharge Plan The patient is instructed to take the following plan for discharge.
M-EDICATION, instruct patient to continuously drink medication as prescribe by Doctor E-XERCISES, instruct patient to conduct 15-20 minutes exercises morning and active ROM in extremities for about 5-10minutes every afternoon T-REATMENT, instruct patient to continuously stick to the regimen of drinking medication on time and reporting to physician for any signs of deviations H-EALTH TEACHING, instruct patient to exercise daily, increase fluid intake O-UT-PATIENT FOLLOW UP, Instruct patient to attend follow-up check-ups as recommended by the physician. D-IET, the patient will be place on diet as tolerated S-PIRITUAL, Encourage client to attend religious practices like attending the worship service
Treatment and management ARTHROTOMY The medical term arthrotomy means cutting into a joint. Also known as a synosteotomy, an arthrotomy can be performed for a variety of reasons, usually as part of a larger surgery which is intended to address a problem inside the joint or an issue with one or more of the bones which articulates at the joint. Procedures of this nature are usually performed by anorthopedic surgeon, a surgeon who specializes in surgeries involving the bones and joints. One reason to perform an arthrotomy is to gain access to the joint for the purpose of a joint repair or replacement surgery. Cutting into the joint may be necessary to access the surgical field and to make the interior of the joint visible to the physician. However, it also increases healing time. Historically, surgeons had to weigh the damage caused by an arthrotomy with the need for the surgery when making treatment recommendations to patients. Today, cutting into the joints is less necessary because surgeons can perform arthroscopicsurgery. In this type of surgery, cameras are inserted into the joint along with tools which can be used to perform manipulations inside the joint. This allows the surgeon to work within the surgical field without having to cut the joint open to do so. Minimally invasive surgery is safer for the patient, decreases the risk of complications, and shortens healing time considerably, making it an appealing choice when it is an available option. Cutting into a joint may also be necessary during an amputation or during exploratory surgery in which arthroscopic surgery is not an option. Arthroscopy may not be possible in some emergency situations, for example, or when a joint is badly crushed and thus the surgeon has difficulty understanding what is going on inside the surgical field without looking at it directly. When arthrotomy is required as part of a medical procedure, the surgeon uses specialized tools which have been designed for cutting quickly and efficiently into the joints while minimizing damage. The surgeon plans out the cuts ahead of time so that when the patient is on the table, the surgeon already has a plan in mind for performing the surgery. Patients should be aware that even routine surgeries can be accompanied
with complications, and a good surgeon will discuss the potential risks of a procedure before it begins so that the patient will be prepared ahead of time.
BLOOD TRANSFUSION A blood transfusion is the transfer of blood or blood products from one person (donor) into another person's bloodstream (recipient). This is usually done as a life saving maneuver to replace blood cells or blood products lost through severe bleeding, during surgery when blood loss occurs or to increase the blood count in an anemic patient. The following material is provided to all patients and/or their family members regarding blood transfusions and the use of blood products. Although in most situations the likelihood of a blood transfusion associated with surgery is uncommon, at times patients may require blood products. You are encouraged to discuss your particular need for transfusion as well as the risks of transfusion with your doctor. Your options may be limited by time and health factors, so it is important to begin carrying out your decision as soon as possible. For example, if friends or family members are donating blood for a patient (directed donors), their blood should be drawn several days prior to the anticipated need to allow adequate time for testing and labeling. The exact protocols are hospital and donor site specific. The safest blood product is your own, so if a transfusion is likely, this is your lowest risk choice. Unfortunately this option is usually only practical when preparing for elective surgery. In most other instances the patient cannot donate their own blood due to the acute nature of the need for blood. Although you have the right to refuse a blood transfusion, this decision may hold life-threatening consequences. If you are a parent deciding for your child, you as the parent or guardian must understand that in a lifethreatening situation your doctors will act in your child's best interest to insure your child's health and well being in accordance with standards of medical care regardless of religious beliefs. Please carefully review this material and decide with your doctor which option(s) you prefer.
To assure a safe transfusion make sure your healthcare provider who starts the transfusion verifies your name and matches it to the blood that is going to be transfused. Besides your name, a second personal identifier usually is used as your birthday. This assures the blood is given to the correct patient. If during the transfusion you have symptoms of shortness of breath, itching, fever or chills or just not feeling well, alert the person transfusing the blood immediately.
You might also like
- Case Study ObcsDocument41 pagesCase Study ObcsKrischelle Abella Sabordo100% (1)
- Case StudyDocument5 pagesCase StudyEdward Jeremy ParasNo ratings yet
- Nursing Case Study Orthopedic FractureDocument15 pagesNursing Case Study Orthopedic FracturenursingdocNo ratings yet
- Case Study On Fracrure Tibial Fracture Apa FormatDocument7 pagesCase Study On Fracrure Tibial Fracture Apa Formatjawn09euclidNo ratings yet
- Ijser: A Case Study On CholelithiasisDocument2 pagesIjser: A Case Study On CholelithiasisRuby Cubionalanting100% (1)
- Acute Gastroenteritis With Severe DehydrationDocument22 pagesAcute Gastroenteritis With Severe DehydrationCess Dunwan100% (1)
- Case Study Ugib.Document19 pagesCase Study Ugib.Mary Ann Garcia100% (1)
- Final Case StudyDocument13 pagesFinal Case StudyJen Gacula OsinNo ratings yet
- Nontoxic Nodular GoiterDocument9 pagesNontoxic Nodular GoiterKayshey Christine ChuaNo ratings yet
- Final CholelithiasisDocument36 pagesFinal CholelithiasisRalph Pelegrino100% (2)
- Case Study PHDDocument42 pagesCase Study PHDJoy AntonetteNo ratings yet
- Stomach CancerDocument7 pagesStomach CancerSyazmin KhairuddinNo ratings yet
- Closed Fracture HumerusDocument35 pagesClosed Fracture HumerusEryn Farahin ZainalNo ratings yet
- Care Study OsteomyelitisDocument23 pagesCare Study OsteomyelitisJake Pitos100% (1)
- Case Report - Juliet - Closed Fracture Middle of The Left FemurDocument28 pagesCase Report - Juliet - Closed Fracture Middle of The Left FemurGupiesNo ratings yet
- Case Presentation Meyke Liechandra C11109130 Fracture ClavicleDocument24 pagesCase Presentation Meyke Liechandra C11109130 Fracture ClavicleWahyunita IlhamNo ratings yet
- Sample Charting PDFDocument2 pagesSample Charting PDFjeffersonswallNo ratings yet
- Acute Gastro Enteritis 1Document42 pagesAcute Gastro Enteritis 1MichaelKimDugenia0% (1)
- Post Op Case Studies StudentsDocument19 pagesPost Op Case Studies StudentsRenie SerranoNo ratings yet
- Cs AGNDocument177 pagesCs AGNMa Rafaela Rosales PalomponNo ratings yet
- NURSING CARE PLAN The Child Undergoing Surgery For ScoliosisDocument3 pagesNURSING CARE PLAN The Child Undergoing Surgery For ScoliosisscrewdriverNo ratings yet
- Grand Case Study FinalDocument34 pagesGrand Case Study FinalFenina S. CalmaNo ratings yet
- NCP ScoliosisDocument4 pagesNCP ScoliosisCharley DegamoNo ratings yet
- FINAL CHOLE,,,Sa Wakas TpozDocument64 pagesFINAL CHOLE,,,Sa Wakas TpozakatzkiNo ratings yet
- Case Presentation (Age) NG Grp. A2 FinalDocument43 pagesCase Presentation (Age) NG Grp. A2 Finaljean therese83% (6)
- Care of Older Persons With Dementia and DepressionDocument28 pagesCare of Older Persons With Dementia and DepressionAnthony RiggsNo ratings yet
- Dyspepsia (Gastritis) Case StudiesDocument9 pagesDyspepsia (Gastritis) Case StudiesJessica Nurin Graman100% (1)
- Acute Gastroenteritis in Paediatrics 1Document43 pagesAcute Gastroenteritis in Paediatrics 1Imran FaisalNo ratings yet
- Dec 21 23 Case Study ModuleDocument7 pagesDec 21 23 Case Study ModuleKristian Karl Bautista Kiw-isNo ratings yet
- Case Presentation: Presented byDocument34 pagesCase Presentation: Presented byZahid AnwarNo ratings yet
- Upper GI Bleed - SymposiumDocument38 pagesUpper GI Bleed - SymposiumSopna ZenithNo ratings yet
- Fracture at Right Femur Orif Case StudyDocument16 pagesFracture at Right Femur Orif Case StudyLouie ParillaNo ratings yet
- Case Study of Hip FractureDocument2 pagesCase Study of Hip FractureBernardete Freitas Barros100% (1)
- Theoretical Framework of Nursing PracticeDocument18 pagesTheoretical Framework of Nursing PracticeIsrael AgrisNo ratings yet
- Case Study - CholecystitisDocument26 pagesCase Study - Cholecystitismeed02100% (2)
- Case Study Medical WardDocument4 pagesCase Study Medical WardFrancis Antonio Llenaresas QuijanoNo ratings yet
- Ongoing AppraisalDocument2 pagesOngoing AppraisalLouisa Marie MirandaNo ratings yet
- A Case Study of Acute GastroenteritisDocument42 pagesA Case Study of Acute GastroenteritisGelah DacanayNo ratings yet
- Case AGNDocument66 pagesCase AGNMohaima PanditaNo ratings yet
- Case Study of "Subtrochanteric Femur": Prepared By: John Ress A. Escobal Group 1Document11 pagesCase Study of "Subtrochanteric Femur": Prepared By: John Ress A. Escobal Group 1J.r. MercadoNo ratings yet
- (Olfu) Pediatrics Case Study: Post Streptococcal Glomerulo Nephritis (PSGN)Document20 pages(Olfu) Pediatrics Case Study: Post Streptococcal Glomerulo Nephritis (PSGN)MikaCasimiroBalunanNo ratings yet
- Diagnostics - Nursing ResponsibilitiesDocument9 pagesDiagnostics - Nursing ResponsibilitiesCarmellaDawn100% (3)
- JOb Description For SupervisorDocument2 pagesJOb Description For SupervisorJennelyn LumbreNo ratings yet
- CholelithiasisDocument3 pagesCholelithiasisMIlanSagittarius0% (1)
- Case PresentationDocument10 pagesCase PresentationWina Hanriyani0% (1)
- A Case Study On Mild Compression Deformity L1Document25 pagesA Case Study On Mild Compression Deformity L1JM UncianoNo ratings yet
- Case Study 1 FinalDocument28 pagesCase Study 1 Finalapi-3905968320% (1)
- Cast and TractionsDocument12 pagesCast and TractionsNoemi Nazareno MarceloNo ratings yet
- FractureDocument71 pagesFractureRegime San Juan AtienzaNo ratings yet
- Cholelithiasis 0232Document118 pagesCholelithiasis 0232Kz LonerNo ratings yet
- Nursing Process of A Client With CholelithiasisDocument21 pagesNursing Process of A Client With Cholelithiasisapi-3822508100% (6)
- Palatoplasty Case StudyDocument26 pagesPalatoplasty Case StudySometwo C. Hangal100% (1)
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezNo ratings yet
- Case Study or (PGO)Document10 pagesCase Study or (PGO)Nikki Navalta Dela CruzNo ratings yet
- Genitourinary Trauma 2Document46 pagesGenitourinary Trauma 2Maria100% (1)
- Case History Surgery Chole CystitisDocument23 pagesCase History Surgery Chole CystitisMardiana KamalNo ratings yet
- Paget Disease of BoneDocument17 pagesPaget Disease of Boneraghunandhakumar100% (1)
- Case 5-2009: A 47-Year-Old Woman With A Rash and Numbness and Pain in The LegsDocument10 pagesCase 5-2009: A 47-Year-Old Woman With A Rash and Numbness and Pain in The LegsRommel D-pNo ratings yet
- Lupusand GIbleedDocument2 pagesLupusand GIbleedAshley Noonan SteereNo ratings yet
- Risk For Ineffective Tissue PerfusionDocument5 pagesRisk For Ineffective Tissue PerfusionElle Oranza100% (1)
- Footpri NTS: Inside This IssueDocument4 pagesFootpri NTS: Inside This IssueBhishman DesaiNo ratings yet
- 2020-08-06 St. Mary's County TimesDocument32 pages2020-08-06 St. Mary's County TimesSouthern Maryland OnlineNo ratings yet
- Immunohematology - Chapter 4Document14 pagesImmunohematology - Chapter 4Mohamed NourNo ratings yet
- RBC PreservationDocument23 pagesRBC PreservationLoiLoiChanNo ratings yet
- Must To Know MTLDocument15 pagesMust To Know MTLMae MacalandaNo ratings yet
- HCI Final ProjectDocument15 pagesHCI Final ProjectMʌɭɩĸ HʌɱʑʌNo ratings yet
- Quality Assurance in The Blood Transfusion LabDocument25 pagesQuality Assurance in The Blood Transfusion LabMichelle AnsahNo ratings yet
- 1 - EUBIS - Part - A - Manual - Edition - 1 - 0 - 1 - FN2016 NEW PDFDocument138 pages1 - EUBIS - Part - A - Manual - Edition - 1 - 0 - 1 - FN2016 NEW PDFGilbertmichyNo ratings yet
- Blood ProductDocument89 pagesBlood ProductSam0% (1)
- Blood DonationDocument24 pagesBlood DonationKris NNo ratings yet
- 0.1 Chapter 7 - Ethical Considerations On Community Health NursingDocument45 pages0.1 Chapter 7 - Ethical Considerations On Community Health NursingyounggirldavidNo ratings yet
- Blood BankDocument12 pagesBlood BankIda RaniNo ratings yet
- Medical - Teacher Book PDFDocument41 pagesMedical - Teacher Book PDFSarah Auckland50% (10)
- Design Project Proposal Proponent's NameDocument4 pagesDesign Project Proposal Proponent's NameJhonydel EscanillaNo ratings yet
- Abraham Tenaw 4 Power Point ProposalDocument32 pagesAbraham Tenaw 4 Power Point Proposalnahom fikaduNo ratings yet
- Parental Consent Blood Donation ENDocument2 pagesParental Consent Blood Donation ENDelaney MarieNo ratings yet
- Blood Donors List 2Document4 pagesBlood Donors List 2Tanzeel KhokharNo ratings yet
- SRSDocument4 pagesSRSSevleena B JoyNo ratings yet
- The Composition of Blood: Fact Sheet: Blood PlasmaDocument1 pageThe Composition of Blood: Fact Sheet: Blood PlasmaKoshkaNo ratings yet
- IntroductionDocument11 pagesIntroductionVikraman ThamotharanNo ratings yet
- Kotak Mahindra BankDocument23 pagesKotak Mahindra BankSai VasudevanNo ratings yet
- PE 005-3 (PICS GMP Guide For Blood Establishments)Document25 pagesPE 005-3 (PICS GMP Guide For Blood Establishments)William ChandraNo ratings yet
- Assignment BloodDocument7 pagesAssignment Bloodhusain albaqaliNo ratings yet
- BLOOD BANK MANAGEMENT SYSTEM DiagramsDocument19 pagesBLOOD BANK MANAGEMENT SYSTEM DiagramsChinamayi Chinmayi80% (5)
- World Blood Donor DayDocument10 pagesWorld Blood Donor DayNeeraj KumarNo ratings yet
- Capstone ProposalDocument8 pagesCapstone Proposalapi-253857430No ratings yet
- 3 IhDocument42 pages3 IhGennelyn Ross Delos ReyesNo ratings yet
- Shubham's Project ReportDocument27 pagesShubham's Project ReportShubham JainNo ratings yet
- Consti 2 CasesDocument275 pagesConsti 2 CasesJoseph AbadianoNo ratings yet
- Upcoming Atlanta Red Cross Blood DrivesDocument26 pagesUpcoming Atlanta Red Cross Blood DrivesJonathan RaymondNo ratings yet