Professional Documents
Culture Documents
Stoke Pathophysiology 1228539935337551 8
Uploaded by
Mark Anthony Taña GabiosaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Stoke Pathophysiology 1228539935337551 8
Uploaded by
Mark Anthony Taña GabiosaCopyright:
Available Formats
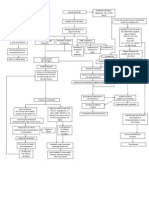
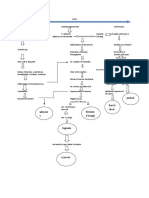
PATHOPHYSIOLOGY
Precipitating Factors: Hypertension Hyperlipidemia Diabetes Mellitus Heart Diseases Atherosclerosis Arteriosclerosis Thrombosis Severe dehydration Predisposing Factors: Life style (sedentary) Vices (Alcohol, smoke) Age Diet Sex Heredity Self-medication
VASOCONSTRICTION
Blockage of the blood vessel Embolism Lack of oxygen & nutrients supply
High blood pressure, smoking, heart diseases, diabetes, narrowing of arteries supplying the brain, high cholesterol and an unhealthy lifestyle.
Ischemic Stroke
Cerebral Ischemia
Hypoxia Subarachnoid Hemorrhage
High blood pressure, smoking, and a family history of burst aneurysms.
- Cell death - Decreased Oxygen level Intracerebral hemorrhage
Altered cerebral metabolism Venous Stroke Decreased cerebral perfusion Large Artery Strokes
Severe dehydration, severe infection in the sinuses of the head and medical or genetic conditions that increase a persons tendency to form blood clots.
Hypertension, diabetes, smoking and high cholesterol levels.
P A R A L Y S I S
Local Acidosis Transient Ischemic Attack Same with Ischemic stroke
Cytotoxic Edema
Aneurysm Rupture
Small Artery Stroke
Hypertension, diabetes and smoking.
Embolic strokes
Irregular heart beat (atrial fibrillation), a heart attack (myocardial infarction), heart failure or a small hole in the heart called a PFO (Patent Foramen Ovale).
Brain tissue Necrosis
A stroke is caused by a blocked or bleeding artery in the brain. Most strokes are due to Severe Cases D E A blood to the brain and are called ischemic strokes. Strokes due to blocked arteries that supply T H bursting of brain blood vessels are called hemorrhagic strokes. Intracerebral hemorrhage is caused by bleeding into the brain itself, while subarachnoid hemorrhage is due to bleeding around the base of the brain. A TIA (transient ischemic attack) is caused by a temporary blockage of blood flow to a
blood vessel to the brain lasting less than 24 hours. Another, rarer, form of stroke can occur when a vein (that drains blood out of the brain) is blocked. This is called a venous stroke. Ischemic Stroke This type of stroke is caused by blockage of a blood vessel (artery) supplying the brain. Brain tissue that no longer receives its blood supply can die within a few hours unless something is done to stop the damage. The blockage of arteries can occur in large arteries in the neck or the base of the brain, or in small arteries inside the brain itself. A blood clot can form in the brain or it can form elsewhere and be carried to the brain by an artery and after having an ischemic stroke and the majority of survivors have some long term disability. There are many conditions that increase a person's risk of ischemic stroke. These include high blood pressure, smoking, heart diseases, diabetes, narrowing of arteries supplying the brain, high cholesterol and an unhealthy lifestyle. Treating these conditions can decrease stroke risk. Intracerebral Hemorrhage This type of stroke is caused by the bleeding of a blood vessel within the brain. As a result of the bleeding a blood clot forms in the brain, which puts pressure on the brain and damages it. Although intracerebral hemorrhage is less common than ischemic stroke and it is more serious. The most common cause of intracerebral hemorrhage is high blood pressure. Another cause, especially in younger people with intracerebral hemorrhages, is abnormally formed blood vessels in the brain (vascular malformations or aneurysms). Subarachnoid Hemorrhage Subarachnoid hemorrhage results from the bleeding of an artery around the base of the brain. It is the least common stroke type, accounting for about 5% of all strokes. The most frequent cause of subarachnoid hemorrhage is bleeding from an aneurysm. An aneurysm is a weakening and ballooning of a short portion of an artery (similar to a bubble on the side of an old hose). The factors that can increase a persons risk of this type of stroke include high blood pressure, smoking, and a family history of burst aneurysms. TIA (Transient Ischemic Attack) A TIA is like a temporary ischemic stroke. An artery is temporarily blocked, preventing blood from reaching a part of the brain. This lack of blood flow causes that part of the brain to stop functioning. The symptoms of a TIA are the same as symptoms of an ischemic stroke. In a TIA, the blood vessel opens up again, before any permanent injury to the brain occurs and the patient
recovers completely. Most TIA symptoms last less than 30 minutes. People who suffer TIAs are at HIGH RISK OF STROKE soon thereafter. A TIA should lead to immediate medical evaluation to determine its cause and a treatment plan to prevent a stroke from following soon after. Venous Stroke Venous stroke is caused by a blood clot blocking the veins that allow blood to drain out of the brain. (All other strokes are caused by abnormalities of arteries carrying blood to the brain). Venous stroke causes a back pressure effect that leads to the stroke. These strokes can be either ischemic or hemorrhagic. Some causes of venous stroke include severe dehydration, severe infection in the sinuses of the head and medical or genetic conditions that increase a persons tendency to form blood clots.
Patient care management goal: to support the patients vital functions, restore cerebral blood flow, minimize neurologic deficits, and prevent progression 1. Maintain a patent airway to promote adequate oxygenation 2. Administer oxygen therapy with possible intubation andmechanical ventilation to ensure adequate tissue perfusion 3. Maintain bed rest to minimize metabolic requirements 4. Provide I.V. fluids to support blood pressure and maintain volume 5. Administer dexamethasone to reduce cerebral edema 6. Administer anticoagulants and antiplatelet drugs for thrombotic conditions after hemorrhage has been ruled out 7. Administer sedatives, such as Phenobarbital, to decrease metabolic requirements 8. Assess the patients neurologic status; observe for CVA progression and level of consciousness (LOC) change as evidenced by decreasing numerical score on the GLASGOW COMA SCALE. 9. Correct cardiovascular abnormalities, such as atrial fibrillation, that may be contributing factors 10. Consider surgical procedures to correct circulatory impairment, prevent repeated hemorrhage, or relieve cerebral pressure 11. Begin bedside range-of-motion exercise to preserve mobility and prevent deformities 12. Teach the patient to identify risk factors and necessary life-style modifications, such as diet, stress reduction, and smoking cessation 13. Direct the family to community groups that provide support or rehabilitation
In order to understand how stroke occurs and the damage it can cause, it is useful to understand the basic anatomy of the brain. The signs and symptoms of a stroke depend on which region of the brain is affected and how severely.
The brain has three primary components. Each is responsible for different functions: The Cerebrum: The cerebrum is the largest and most developmentally advanced portion of the brain. It controls a number of higher functions, including speech, emotion, the integration of sensory stimuli, initiation of the final common pathways for movement, and fine control of movement. It is divided into a left and a right hemisphere. The left hemisphere controls the majority of functions on the right side of the body, while the right hemisphere controls most of functions on the left side of the body. Thus, injury to the left cerebral hemisphere produces sensory and motor deficits on the right side, and vice versa. The cerebrum is composed of the frontal, parietal, temporal, and occipital lobes:
The frontal lobe is involved in planning, organizing, problem solving and selective attention. The portion known as the prefrontal cortex controls personality and various higher cognitive functions such as behavior and emotions. The back of the frontal lobe consists of the premotor and motor areas, which produce and modify movement. The left and right parietal lobes contain the primary sensory cortex, which controls sensation (touch and pressure), and a large association area that controls fine sensation (judgment of texture, weight, size, and shape). Damage to the right parietal lobe can cause visuo-spacial deficits, making it hard for the patient to find his/her way around new or even familiar places. Damage to the left parietal lobe may disrupt a patients ability to understand spoken and/or written language. The left and right temporal lobes, located around ear level, allow a person to differentiate smells and sounds. They also help in sorting new information and are believed to be
responsible for short-term memory. The right lobe is primarily involved in visual memory (i.e., memory for faces and pictures). The left lobe is primarily involved in verbal memory (i.e., memory for words and names). The occipital lobe processes visual information. It is mainly responsible for visual reception and contains association areas that help in the visual recognition of shapes and colors. Damage to this lobe can cause visual deficits.
The Cerebellum: The cerebellum is the second largest area of the brain. It controls reflexes, balance and certain aspects of movement and coordination. The Brain Stem: The brain stem is responsible for a variety of automatic functions that are critical to life, such as breathing, digestion and heart beat as well as alertness and arousal (the state of being awake).
Symptoms Point to Stroke Location
A stroke can occur anywhere in the brain or just outside it. The symptoms that a stroke victim experiences depend on which area(s) of the brain are involved. When a stroke occurs in the right hemisphere of the cerebrum, the result may be paralysis on the left side of the body, difficulty reasoning or thinking out solutions to even the simplest problem. A stroke in the left hemisphere can result in paralysis of the right side of the body and may disrupt the ability to speak. A stroke involving the cerebellum may result in a lack of coordination (ataxia), clumsiness and balance problems, shaking, or other muscular difficulties. This can interfere with a persons ability to walk, talk, eat and perform other self-care tasks. Brain stem strokes are the most devastating and life threatening because they can disrupt the involuntary functions essential to life. People who survive may remain in a vegetative state or be left with severe impairments.
Blood Flow to the Brain
The heart pumps oxygen- and nutrient-laden blood to the brain, face, and scalp via two major sets of vessels: the carotid arteries and the vertebral arteries. The jugular and other veins bring blood out of the brain.
The carotid arteries run along the front of the neck one on the left and one on the right. They are what you feel when you take your pulse just under your jaw. The carotid arteries split into external and internal arteries near the top of the neck. The external carotid arteries supply blood to the face and scalp. The internal carotid arteries supply blood to the front (anterior) three-fifths of cerebrum, except for parts of the temporal and occipital lobes. The vertebral arteries travel along the spinal column and cannot be felt from the outside. They join to form a single basilar artery (hence the name vertebrobasilar arteries) near the brain stem at the base of the skull. The arteries supply blood to the posterior two-fifths of the cerebrum, part of the cerebellum, and the brain stem. Because the brain relies on only two sets of major arteries for its blood supply, it is very important that these arteries are healthy. Often when an ischemic stroke occurs, the carotid or vertebral artery system is blocked with a fatty buildup called plaque, allowing little or no blood to flow to the brain. During a hemorrhagic stroke, an artery in or on the surface of the brain has ruptured or is leaking, causing bleeding and damage in or around the brain. These arteries that conduct blood to the brain the internal-carotid and vertebral arteries connect through the Circle of Willis, which loops around the brainstem at the base of the brain. From this circle, other arteries the anterior cerebral artery (ACA), the middle cerebral artery (MCA), and the posterior cerebral artery (PCA) arise and travel to all parts of the brain. Because the carotid and vertebrobasilar arteries form a circle, if one of the main arteries is blocked, the smaller arteries that the circle supplies can receive blood from the other arteries. This phenomenon is called collateral circulation. Collateral circulation is a process in which small (normally closed) arteries open up and connect two larger arteries or different parts of the same artery. They can serve as alternate routes of blood supply. Sometimes when an artery in the brain is blocked due to ischemic stroke or transient ischemic
attack (TIA), open collateral vessels can allow blood to "detour" around the blockage, restoring blood flow to the affected part of the brain. Everyone has collateral vessels, at least in microscopic form. These vessels normally aren't open. However, they grow and enlarge in some people with coronary heart disease or other blood vessel disease. While everyone has collateral vessels, they don't open in all people. The Circle of Willis has a downside, however. Cerebral aneurysms tend to occur at the junctions between the arteries that make up the Circle.
You might also like
- Stroke PathophysiologyDocument3 pagesStroke PathophysiologyMaureen EricaNo ratings yet
- Pathophysiology CVD InfarctDocument1 pagePathophysiology CVD InfarctElisa KerrNo ratings yet
- Pathophysiology of StrokeDocument4 pagesPathophysiology of StrokeACe JAyNo ratings yet
- Sepsis Is The Consequence of A Dysregulated Inflammatory Response To An Infectious InsultDocument11 pagesSepsis Is The Consequence of A Dysregulated Inflammatory Response To An Infectious InsultShrests SinhaNo ratings yet
- Pathophysiology of CVADocument1 pagePathophysiology of CVAChristine Joy Ilao PasnoNo ratings yet
- Pathophysiology CVADocument1 pagePathophysiology CVANenette Aquino100% (2)
- Pathophysiology ErDocument3 pagesPathophysiology ErAlexa A. AldayNo ratings yet
- Pathophysiology in Liver CirrhosisDocument4 pagesPathophysiology in Liver CirrhosisCyrus Ortalla RobinNo ratings yet
- Pa Tho Physiology of Hemorrhagic StrokeDocument2 pagesPa Tho Physiology of Hemorrhagic StrokeMerlash MerlaNo ratings yet
- Heart Failure COncept MapDocument2 pagesHeart Failure COncept MapJrBong SemaneroNo ratings yet
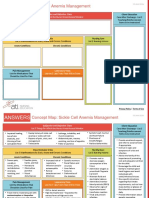
- NCC-SickleCellAnemiaManagement ConceptMap InteractivePDFDocument2 pagesNCC-SickleCellAnemiaManagement ConceptMap InteractivePDFLoggerz Arck100% (1)
- Pathophysiology and Schematic Diagram of Typhoid FeverDocument3 pagesPathophysiology and Schematic Diagram of Typhoid FeverCyrus De AsisNo ratings yet
- PathophysiologyDocument34 pagesPathophysiologyeunams_1195% (20)
- Pathophysiology CHFDocument2 pagesPathophysiology CHFPerry Oliver AlvarezNo ratings yet
- Pathophysiology HPN CvaDocument1 pagePathophysiology HPN Cvatresdos09No ratings yet
- Pathophysiology: Precipitating FactorDocument6 pagesPathophysiology: Precipitating FactorMark Anthony YabresNo ratings yet
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Client Centered PathophysiologyDocument3 pages"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Client Centered PathophysiologyCarl Elexer Cuyugan Ano50% (2)
- CellulitisDocument39 pagesCellulitisMary Jhane Villanueva50% (4)
- Stroke PathophysiologyDocument2 pagesStroke PathophysiologyJaessa Feliciano100% (2)
- Cholecystitis Nursing Care PlanDocument4 pagesCholecystitis Nursing Care PlanMDCITY83% (6)
- Schematic Pathophysiology CVADocument10 pagesSchematic Pathophysiology CVAheiyu100% (5)
- Guillain Barre Syndrome PathophysiologyDocument4 pagesGuillain Barre Syndrome Pathophysiologykathy100% (13)
- Drug Study Case 1Document37 pagesDrug Study Case 1Maria Charis Anne IndananNo ratings yet
- Age Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat IntakeDocument3 pagesAge Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat Intakenursing concept mapsNo ratings yet
- Angina Pectoris PathophysiologyDocument2 pagesAngina Pectoris PathophysiologyALIANA KIMBERLY MALQUESTONo ratings yet
- Qtsoi Concept MapDocument5 pagesQtsoi Concept MapGenella BabantoNo ratings yet
- Pathophysiology of TiaDocument1 pagePathophysiology of Tiaabbeeyy100% (1)
- Concept MapDocument1 pageConcept MapChristine Marie Barce Martinez100% (2)
- Case On Intracranial HemorrhageDocument17 pagesCase On Intracranial HemorrhageLorebell100% (2)
- Pathophysiology of Congestive Heart FailureDocument3 pagesPathophysiology of Congestive Heart Failuretinayko100% (1)
- Final patho-HCVDDocument2 pagesFinal patho-HCVDAlvin RamirezNo ratings yet
- Concept MapDocument5 pagesConcept Mapmild_tea100% (1)
- Transient Ischemic AttackDocument7 pagesTransient Ischemic AttackJennifer DimapilisNo ratings yet
- Pathophysiology of Meniere FinalDocument1 pagePathophysiology of Meniere Final1S VILLEGAS GabrielNo ratings yet
- DB13 - Pathophysiology of AtherosclerosisDocument2 pagesDB13 - Pathophysiology of Atherosclerosisi_vhie03No ratings yet
- Ineffective Tissue Perfusion PDFDocument4 pagesIneffective Tissue Perfusion PDFgcodouganNo ratings yet
- Pathophysiology of Leptospirosis and Dengue FeverDocument5 pagesPathophysiology of Leptospirosis and Dengue FeverKenneth Lagman100% (1)
- CVA PathophysiologyDocument3 pagesCVA Pathophysiologyshmily_0810No ratings yet
- Pathophysiology Sickle Cell Anemia PDFDocument1 pagePathophysiology Sickle Cell Anemia PDFTine GuibaoNo ratings yet
- Acute Coronary SyndromeDocument2 pagesAcute Coronary SyndromeRenz Castañaday100% (1)
- Pathophysiology of DMDocument4 pagesPathophysiology of DMNicole Louise N. VillanuevaNo ratings yet
- Pathophysiology of Diabetes Mellitus Type 2Document1 pagePathophysiology of Diabetes Mellitus Type 2faula rocamora100% (3)
- Pathophysiology of Status EpilepticusDocument6 pagesPathophysiology of Status EpilepticusKysha Ruth SevillaNo ratings yet
- Cva NCPDocument2 pagesCva NCPSharewin PulidoNo ratings yet
- Pathophysiology Hemorrhagic StrokeDocument1 pagePathophysiology Hemorrhagic StrokeJeffrey Dela CruzNo ratings yet
- Stroke PathophysiologyDocument5 pagesStroke Pathophysiologycinnabon_heart9100% (3)
- Pathophysiology of AppendicitisDocument2 pagesPathophysiology of Appendicitis33342No ratings yet
- COPD PathophysiologyDocument1 pageCOPD Pathophysiologyaj ajNo ratings yet
- COPD PathophysiologyDocument1 pageCOPD PathophysiologyJustin Ahorro-Dionisio33% (3)
- Systemic Lupus Erythematosus (SLE) : Genetic Factors Environmental FactorsDocument5 pagesSystemic Lupus Erythematosus (SLE) : Genetic Factors Environmental Factorsjoyrena ochondraNo ratings yet
- Precipitating Factors Predisposing Factors Chronic Kidney DiseaseDocument3 pagesPrecipitating Factors Predisposing Factors Chronic Kidney DiseaseGrace Jane DionaldoNo ratings yet
- STROKE: Handbook with activities, exercises and mental challengesFrom EverandSTROKE: Handbook with activities, exercises and mental challengesNo ratings yet
- What Is A StrokeDocument5 pagesWhat Is A StrokeLintsuNo ratings yet
- Focus On StrokeDocument92 pagesFocus On StrokeDIAH RETNO WULAN100% (2)
- Case 1 FinalDocument70 pagesCase 1 FinalMaria Charis Anne IndananNo ratings yet
- Cerebrovascular Diseas1Document47 pagesCerebrovascular Diseas1Jenard Joniel OlivarNo ratings yet
- Cerebrovascular Accident: Silliman University Dumaguete City Resource Unit OnDocument18 pagesCerebrovascular Accident: Silliman University Dumaguete City Resource Unit OnCharles KevinNo ratings yet
- Cross StitchDocument1 pageCross StitchMark Anthony Taña GabiosaNo ratings yet
- Drug StudyDocument7 pagesDrug StudyMark Anthony Taña GabiosaNo ratings yet
- Differents Kind of Mountain and HillDocument8 pagesDifferents Kind of Mountain and HillMark Anthony Taña GabiosaNo ratings yet
- Longitude Is A Geographic Coordinate That Specifies The EastDocument1 pageLongitude Is A Geographic Coordinate That Specifies The EastMark Anthony Taña GabiosaNo ratings yet
- Agn PediaDocument5 pagesAgn PediaMark Anthony Taña GabiosaNo ratings yet
- If Things DonDocument1 pageIf Things DonMark Anthony Taña GabiosaNo ratings yet
- If Things DonDocument1 pageIf Things DonMark Anthony Taña GabiosaNo ratings yet
- MefenamicDocument2 pagesMefenamicMark Anthony Taña GabiosaNo ratings yet
- 5 Biomechanics of Elbow JointDocument45 pages5 Biomechanics of Elbow JointJHINUK DASGUPTANo ratings yet
- Deep Tendon Reflex Steps On How To Assess The DTR: Normal Response: DTR GradingDocument2 pagesDeep Tendon Reflex Steps On How To Assess The DTR: Normal Response: DTR GradingElla EvangelistaNo ratings yet
- Properties of Cardiac Muscle PDFDocument38 pagesProperties of Cardiac Muscle PDFZaid RazaliNo ratings yet
- HOPE 2A MODULE 4 Badminton 2 PDFDocument19 pagesHOPE 2A MODULE 4 Badminton 2 PDFLeo Patrick100% (7)
- Circulatory SystemDocument3 pagesCirculatory Systemnacuamaryjoy123No ratings yet
- Lab Muscle ContractionDocument5 pagesLab Muscle ContractionAllan DuplaNo ratings yet
- Post Mastectomy ExerciseDocument4 pagesPost Mastectomy ExerciseKusum RoyNo ratings yet
- SkullDocument23 pagesSkullurjaNo ratings yet
- Interdigital (Morton's) Neuroma - Foot & Ankle - OrthobulletsDocument3 pagesInterdigital (Morton's) Neuroma - Foot & Ankle - OrthobulletsEmiel AwadNo ratings yet
- Tubular and Massif Organ: Problem Based Learning (PBL)Document18 pagesTubular and Massif Organ: Problem Based Learning (PBL)KEZIA CALISTA HERLIANINo ratings yet
- Ch. 4 TissuesDocument55 pagesCh. 4 TissuesBora YaNo ratings yet
- Keilhauer Sguig BrochureDocument11 pagesKeilhauer Sguig BrochureJeffrey MeltzerNo ratings yet
- Oral Anatomy Q&ADocument8 pagesOral Anatomy Q&AHanny CarinoNo ratings yet
- Untamed MDMW Home 1-2Document5 pagesUntamed MDMW Home 1-2Leena FranklinNo ratings yet
- Hormones: Test Yourself 15.1 (Page 287)Document3 pagesHormones: Test Yourself 15.1 (Page 287)leeNo ratings yet
- Riumachi 31Document7 pagesRiumachi 31tommy58No ratings yet
- Skin Flap Physiology PDFDocument25 pagesSkin Flap Physiology PDFTang Weng JunNo ratings yet
- Baza III Curs MedDocument117 pagesBaza III Curs MedIntekhabAtahar0% (1)
- Factores Macroesteticos en El Diseño de SonrisaDocument7 pagesFactores Macroesteticos en El Diseño de SonrisaJassel DurdenNo ratings yet
- Physiological Modeling - Final Project (Circulatory System)Document18 pagesPhysiological Modeling - Final Project (Circulatory System)Joshua DamianNo ratings yet
- Exclusive 42 BCS Solve SheetDocument272 pagesExclusive 42 BCS Solve SheetRezaul RazibNo ratings yet
- Case Study On Tos & Cervical Stenosis: by Faviola Bedoy, SPTADocument14 pagesCase Study On Tos & Cervical Stenosis: by Faviola Bedoy, SPTAapi-547954700No ratings yet
- Biomechanics of Knee JointDocument123 pagesBiomechanics of Knee JointSIBASIS PATTANAYAKNo ratings yet
- Ha&P - Semi ReviewerDocument71 pagesHa&P - Semi ReviewerLittle StuartNo ratings yet
- Gym PrinciplesDocument23 pagesGym PrinciplesKrešimir DodigNo ratings yet
- Spinal NervesDocument53 pagesSpinal Nervespearl joy holleroNo ratings yet
- Maxillary SinusDocument37 pagesMaxillary SinusSkAliHassan100% (2)
- Sensory Systems Lecture NotesDocument7 pagesSensory Systems Lecture Notesdevilstrill1605100% (1)
- Amphibian Anatomy and PhysiologyDocument10 pagesAmphibian Anatomy and PhysiologySilvi SiNo ratings yet
- Nursing Head-to-Toe Assessment Cheat Sheet PDFDocument7 pagesNursing Head-to-Toe Assessment Cheat Sheet PDFJoebert BangsoyNo ratings yet