Professional Documents
Culture Documents
Clinical Teaching On Neurological Assessment
Uploaded by
Fiyas BiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Teaching On Neurological Assessment
Uploaded by
Fiyas BiCopyright:
Available Formats
CLINICAL TEACHING ON NEUROLOGICAL ASSESSMENT
SUBMITEED BY: Fiyas .BI 1st yr MSc Nursing Govt:college of nursing Trivandrum
SUBMITTED BY: Mrs:Prathiba Asst:professor Govt:college of nursing Trivandrum
INTRODUCTION The nervous system is one of the bodys control systems; by means of electrochemical impulses, we are able to detect changes and feel sensations, initiate appropriate responses to changes, and organize and store information for future use. Some of this is conscious activity, but much of it is reflexive in nature and happens without our awareness Staff nurses in many types of practice settings encounter patients with altered neurologic function. Disorders of the nervous system can occur at any time during the life span and can vary from mild, self-limiting symptoms to devastating, life-threatening disorders. The nurse must be skilled in the assessment of the neurologic system whether the assessment is generalized or focused on specific areas of function. Assessment in either case requires knowledge of the anatomy and physiology of the nervous system and an understanding of the array of tests and procedures used to diagnose neurologic disorders. Knowledge about the nursing implications and interventions related to assessment and diagnostic testing is also essential. METHOD OF NEUROLOGICAL ASSESSMENT A) LOCATE THE LESION
The first priority is to identify the region of the nervous system that is likely to be responsible for the symptoms. Can the disorder be mapped to one specific location, is it multifocal, or is a diffuse process present? Are the symptoms restricted to the nervous system, or do they arise in the context of a systemic illness? Is the problem in the central nervous system (CNS), the peripheral nervous system (PNS), or both? If in the CNS, is the cerebral cortex, basal ganglia, brainstem, cerebellum, or spinal cord responsible? Are the pain-sensitive meninges involved? If in the PNS, could the disorder be located in peripheral nerves and, if so, are motor or sensory nerves primarily affected, or is a lesion in the neuromuscular junction or muscle more likely? Deciding "where the lesion is" accomplishes the task of limiting the possible etiologies to a manageable, finite number. In addition, this strategy safeguards against making serious errors. Once the question, "Where is the lesion?" is answered, then the question, "What is the lesion?" can be addressed. B) DEFINE THE PATHOPHYSIOLOGY
Clues to the pathophysiology of the disease process may also be present in the history. Primary neuronal (gray matter) disorders may present as early cognitive disturbances, movement disorders, or seizures, whereas white matter involvement produces predominantly "long tract" disorders of motor, sensory, visual, and cerebellar pathways NEUROLOGICAL HISTORY 1) COURSE OF ILLNESS
It is important to determine the precise time of appearanceand rate of progression of the symptoms experienced by the patient. The rapid onset of a neurologic complaint, occurring within seconds or minutes, usually indicates a vascular event,a seizure, or migraine. The onset of sensory symptoms located in one extremity that spread over a few seconds to adjacent portions of that extremity and then
to the other regions of the body suggests a seizure. A more gradual onset and less well localized symptoms point to the possibility of a transient ischemic attack (TIA). A similar but slower temporal march of symptoms accompanied by headache, nausea, or visual disturbance suggests migraine. The presence of "positive" sensory symptoms (e.g., tingling or sensations that are difficult to describe) or involuntary motor movements suggests a seizure; in contrast, transient loss of function (negative symptoms) suggests a TIA.
PATIENTS DESCRIPTION OF COMPLAINT The same words often mean different things to different patients. "Dizziness" may imply impending syncope, a sense of disequilibrium, or true spinning vertigo. "Numbness" may mean a complete loss of feeling, a positive sensation such as tingling, or paralysis. "Blurred vision" may be used to describe unilateral visual loss as in transient monocular blindness, or diplopia. The interpretation of the true meaning of the words used by patients to describe symptoms becomes even more complex when there are differences in primary languages and cultures. 3) CORROBORATION OF HISTORY BY OTHERS It is almost always helpful to obtain additional information from family, friends, or other observers to corroborate or expand the patient's description. Memory loss, aphasia, loss of insight, intoxication, and other factors may impair the patient's capacity to communicate normally with the examiner or prevent openness about factors that have contributed to the illness. Episodes of loss of consciousness necessitate that details be sought from observers to ascertain precisely what has happened during the event 4) FAMILY HISTORY Many neurologic disorders have an underlying genetic component. The presence of a Mendelian disorder, such as Huntington's disease or Charcot-Marie-Tooth neuropathy, is often obvious if family data are available. More detailed questions about family history are often necessary in polygenic disorders such as MS, migraine, and many types of epilepsy. It is important to elicit family history about all illnesses, in addition to neurologic and psychiatric disorders. A familial propensity to hypertension or heart disease is relevant in a patient who presents with a stroke 5) MEDICAL ILLNESS Many neurologic diseases occur in the context of systemic disorders. Diabetes mellitus, hypertension, and abnormalities of blood lipids predispose to cerebrovascular disease. A solitary mass lesion in the brain may be an abscess in a patient with valvular heart disease, a primary hemorrhage in a patient with a coagulopathy, a lymphoma or toxoplasmosis in a patient with AIDS, or a metastasis in a patient with underlying cancer. Patients with malignancy may also present with a neurologic paraneoplastic syndrome (Chap. 97) or complications from chemotherapy or radiotherapy 6) DRUGS AND TOXINS It is essential to inquire about the history of drug use, both prescribed and illicit. Aminoglycoside antibiotics may exacerbate symptoms of weakness in patients with disorders of neuromuscular transmission, such as myasthenia gravis, and may cause dizziness secondary to ototoxicity. Vincristine and other antineoplastic drugs can cause peripheral neuropathy, and immunosuppressive agents such as cyclosporine can produce encephalopathy. Excessive vitamin ingestion can lead to disease; for example vitamin A and pseudotumor cerebri, or pyridoxine and peripheral neuropathy. Many patients are unaware that over-the-counter sleeping pills, cold
2)
preparations, and diet pills are actually drugs. Alcohol, the most prevalent neurotoxin, is often not recognized as such by patients, and other drugs of abuse such as cocaine and heroin can cause a wide range of neurologic abnormalities. 7) FORMULATE AN IMPRESSION OF PATIENT Use the opportunity while taking the history to form an impression of the patient. Is the information forthcoming, or does it take a circuitous course? Is there evidence of anxiety, depression, hypochondriasis? Are there any clues to defects in language, memory, insight, or inappropriate behavior? The neurologic assessment begins as soon as the patient comes into the room and the first introduction is made CLINICAL MANIFESTATIONS The clinical manifestations of neurologic disease are as varied as the disease processes themselves. Symptoms can be subtle or intense,fluctuating or permanent, an inconvenience or devastating. The common presenting complaints of a patient with neurological disorder are:a) PAIN: Pain can sbe acute or chronic. In general, acute pain lasts for a relatively short period of time and remits as the pathology resolves. In neurologic disease, this type of pain is often associated with spinal disc disease, trigeminal neuralgia, or other neuropathic pathology (eg, postherpetic neuralgia, or painful neuropathies). In contrast, chronic pain extends for long periods of time and may represent a low level of pathology. This type of pain might also occur with discogenic disease. b) SEIZURES: The alteration may be short, as in a blank stare lasting only a second, or of longer duration, such as a tonic-clonic grand mal seizure that can last several minutes. The type of seizure activity is a direct result of the area of the brain affected. Seizures can occur as isolated events, such as when induced by a high fever, alcohol or drug withdrawal, or hypoglycemia. A seizure may also be the first obvious sign of a brain lesion. c) DIZZINESS: Dizziness is an abnormal sensation of imbalance or movement. It is fairly common in the elderly and one of the most common complaints encountered by health professionals. Dizziness can have a variety of causes, including viral syndromes, hot weather, roller coaster rides, and middle ear infections, to name a few. One difficulty confronting health care providers when assessing dizziness is the vague and varied terms patients use to describe the sensation. d) VISUAL DISTURBENCES: Normal vision depends upon functioning visual pathways through the retina and optic chiasm and the radiations into the visual cortex in the occipital lobes. Lesions of the eye itself (eg, cataract), lesions along the pathway (eg, tumor), or lesions in the visual cortex (from stroke) interfere with normal visual acuity. Abnormalities of eye movement (as in the nystagmus associated with multiple sclerosis) can also compromise vision by causing diplopia or double vision. e) WEAKNESS: Weakness, specifically muscle weakness, is a common manifestation of neurologic disease. Weakness frequently coexists with other symptoms of disease and can affect a variety of muscles, causing a wide range of disability. Weakness can be sudden and permanent, as in stroke, or
progressive, as in many neuromuscular diseases such as amyotrophic lateral sclerosis. Any muscle group can be affected. f) ABNORMAL SENSATIONS: Numbness, abnormal sensation, or loss of sensation is a neurologic manifestation of both central and peripheral nervous system disease. Altered sensation can affect small or large areas of the body. It is frequently associated with weakness or pain and is potentially disabling. Both numbness and weakness can significantly affect balance and coordination. NEUROLOGICAL EXAMINATION . The neurologic examination is challenging and complex; it has many components and includes a number of skills that can be mastered only through repeated use of the same techniques on a large number of individuals with and without neurologic disease. There is no single, universally accepted sequence of the examination that must be followed, but most clinicians begin with assessment of mental status followed by the cranial nerves, motor system, sensory system, coordination, and gait. Whether the examination is basic or comprehensive, it is essential that it be performed in an orderly and systematic fashion to avoid errors and serious omissions 1) MENTAL STATUS EXAMINATION The mental status examination is underway as soon as the physician begins observing and talking with the patient. If the history raises any concern for abnormalities of higher cortical function or if cognitive problems are observed during the interview, then detailed testing of the mental status is indicated. The patient's ability to understand the language used for the examination, cultural background, educational experience, sensory or motor problems, or co-morbid conditions need to be factored into the applicability of the tests and interpretation of results. Individual elements of the mental status examination can be subdivided into level of consciousness, orientation, speech and language, memory, fund of information, insight and judgment, abstract thought, and calculations. a)Level of consciousness: is the patient's relative state of awareness of the self and the environment, and ranges from fully awake to comatose. When the patient is not fully awake, the examiner should describe the responses to the minimum stimulus necessary to elicit a reaction, ranging from verbal commands to a brief, painful stimulus such as a squeeze of the trapezius muscle. Responses that are directed toward the stimulus and signify some degree of intact cerebral function (e.g., opening the eyes and looking at the examiner or reaching to push away a painful stimulus) must be distinguished from reflex responses of a spinal origin (e.g., triple flexion responseflexion at the ankle, knee, and hip in response to a painful stimulus to the foot). b): Orientation is tested by asking the person to state his or her name, location, and time (day of the week and date); time is usually the first to be affected in a variety of conditions. c)Speech: is assessed by observing articulation, rate, rhythm, and prosody (i.e., the changes in pitch and accentuation of syllable and words). d) Language: is assessed by observing the content of the patient's verbal and written output, response to spoken commands, and ability to read. A typical testing sequence is to ask the patient to name successively more detailed components of clothing, a watch or a pen; repeat the phrase "No ifs, ands, or buts"; follow a three-step, verbal command; write a sentence; and read and respond to a written command e) Memory: should be analyzed according to three main time scales: (1) immediate memory can be tested by saying a list of three items and having the patient repeat the list immediately, (2) short term memory is assessed by asking the patient to recall the same three items 5 and 15 min later, and (3)
long-term memory is evaluated by determining how well the patient is able to provide a coherent chronologic history of his or her illness or personal events. f) Fund of information: is assessed by asking questions about major historic or current events, with special attention to educational level and life experiences. g)Abnormalities of insight and judgment: are usually detected during the patient interview; a more detailed assessment can be elicited by asking the patient to describe how he or she would respond to situations having a variety of potential outcomes (e.g., "What would you do if you found a wallet on the sidewalk?"). h) Abstract thought: can be tested by asking the patient to describe similarities between various objects or concepts (e.g., apple and orange, desk and chair, poetry and sculpture) or to list items having the same attributes (e.g., a list of four-legged animals). i) Calculation ability : is assessed by having the patient carry out a computation that is appropriate to the patient's age and education (e.g., serial subtraction of 7 from 100 or 3 from 20; or word problems involving simple arithmetic). CRANIAL NERVE ASSESSMENT The cranial nerves (CN) are best examined in numerical order, except for grouping together CN III, IV, and VI because of their similar function. A)Cranial nerve I ( olfactory ): Testing is usually omitted unless there is suspicion for inferior frontal lobe disease (e.g., meningioma). With eyes closed, ask the patient to sniff a mild stimulus such as toothpaste or coffee and identify the odorant. B)Cranial nerve II ( optic): Check visual acuity (with eyeglasses or contact lens correction) using a Snellen chart or similar tool. Test the visual fields by confrontation, i.e., by comparing the patient's visual fields to your own. As a screening test, it is usually sufficient to examine the visual fields of both eyes simultaneously; individual eye fields should be tested if there is any reason to suspect a problem of vision by the history or other elements of the examination, or if the screening test reveals an abnormality. Face the patient at a distance of approximately 0.61.0 m (23 ft) and place your hands at the periphery of your visual fields in the plane that is equidistant between you and the patient. Instruct the patient to look directly at the center of your face and to indicate when and where he or she sees one of your fingers moving. Beginning with the two inferior quadrants and then the two superior quadrants, move your index finger of the right hand, left hand, or both hands simultaneously and observe whether the patient detects the movements. A single small-amplitude movement of the finger is sufficient for a normal response. Focal perimetry and tangent screen examinations should be used to map out visual field defects fully or to search for subtle abnormalities. Optic fundi should be examined with an ophthalmoscope, and the color, size, and degree of swelling or elevation of the optic disc noted, as well as the color and texture of the retina. The retinal vessels should be checked for size, regularity, arterial-venous nicking at crossing points, hemorrhage, exudates, etc. c) cranial nerves III,IV,VI (occulomotor, trochlear, abducense): Describe the size and shape of pupils and reaction to light and accommodation (i.e., as the eyes converge while following your finger as it moves toward the bridge of the nose). To check extraocular movements, ask the patient to keep his or her head still while tracking the movement of the tip of your finger. Move the target slowly in the horizontal and vertical planes; observe any paresis, nystagmus, or abnormalities of smooth pursuit (saccades, oculomotor ataxia, etc.). If necessary, the relative position of the two eyes, both in primary and multidirectional gaze, can be assessed by comparing the reflections of a bright light off both pupils. However, in practice it is typically more useful to determine whether the patient describes diplopia in any direction of gaze; true diplopia should almost always resolve with one eye closed. 1)
Horizontal nystagmus is best assessed at 45 and not at extreme lateral gaze (which is uncomfortable for the patient); the target must often be held at the lateral position for at least a few seconds to detect an abnormality d) Cranial nerve V (trigeminal) : Examine sensation within the three territories of the branches of the trigeminal nerve (ophthalmic, maxillary, and mandibular) on each side of the face. As with other parts of the sensory examination, testing of two sensory modalities derived from different anatomic pathways (e.g., light touch and temperature) is sufficient for a screening examination. Testing of other modalities, the corneal reflex, and the motor component of CN V (jaw clenchmasseter muscle) is indicated when suggested by the history. e) Cranial nerve VII ( facial ) : Look for facial asymmetry at rest and with spontaneous movements. Test eyebrow elevation, forehead wrinkling, eye closure, smiling, and cheek puff. Look in particular for differences in the lower versus upper facial muscles; weakness of the lower two-thirds of the face with preservation of the upper third suggests an upper motor neuron lesion, whereas weakness of an entire side suggests a lower motor neuron lesion. f) Cranial nerve VIII (acoustic) : Check the patient's ability to hear a finger rub or whispered voice with each ear. Further testing for air versus mastoid bone conduction (Rinne) and lateralization of a 512-Hz tuning fork placed at the center of the forehead (Weber) should be done if an abnormality is detected by history or examination. Any suspected problem should be followed up with formal audiometry g) Cranial nerve IX, X ( glossopharyngeal, vagus) : Observe the position and symmetry of the palate and uvula at rest and with phonation ("aah"). The pharyngeal ("gag") reflex is evaluated by stimulating the posterior pharyngeal wall on each side with a sterile, blunt object (e.g., tongue blade), but the reflex is often absent in normal individuals. h) Cranial nerve XI ( spinal accessory) : Check shoulder shrug (trapezius muscle) and head rotation to each side (sternocleidomastoid) against resistance. i) Cranial nerve XII ( hypoglossal ): Inspect the tongue for atrophy or fasciculations, position with protrusion, and strength when extended against the inner surface of the cheeks on each side. MOTOR EXAMINATION The motor examination includes observations of muscle appearance, tone, strength, and reflexes. Although gait is in part a test of motor function, it is usually evaluated separately at the end of the examination a) Appearance : Inspect and palpate muscle groups under good light and with the patient in a comfortable and symmetric position. Check for muscle fasciculations, tenderness, and atrophy or hypertrophy. Involuntary movements may be present at rest (e.g., tics, myoclonus, choreoathetosis), during maintained posture (pill-rolling tremor of Parkinson's disease), or with voluntary movements (intention tremor of cerebellar disease or familial tremor). b) Tone : Muscle tone is tested by measuring the resistance to passive movement of a relaxed limb. Patients often have difficulty relaxing during this procedure, so it is useful to distract the patient to minimize active movements. In the upper limbs, tone is assessed by rapid pronation and supination of the forearm and flexion and extension at the wrist. In the lower limbs, while the patient is supine the examiner's hands are placed behind the knees and rapidly raised; with normal tone the ankles drag along the table surface for a variable distance before rising, whereas increased tone results in an immediate lift of the heel off the surface. Decreased tone is most commonly due to lower motor neuron or peripheral nerve disorders. Increased tone may be evident as spasticity (resistance determined by the angle and velocity of motion; corticospinal tract disease), rigidity (similar resistance in all angles of 2)
motion; extrapyramidal disease), or paratonia (fluctuating changes in resistance; frontal lobe pathways or normal difficulty in relaxing). Cogwheel rigidity, in which passive motion elicits jerky interruptions in resistance, is seen in parkinsonism. c) Strength : Testing for pronator drift is an extremely useful method for screening upper limb weakness. The patient is asked to hold both arms fully extended and parallel to the ground with eyes closed. This position should be maintained for ~10 s; any flexion at the elbow or fingers or pronation of the forearm, especially if asymmetric, is a sign of potential weakness. Muscle strength is further assessed by having the patient exert maximal effort for the particular muscle or muscle group being tested. It is important to isolate the muscles as much as possible, i.e., hold the limb so that only the muscles of interest are active. It is also helpful to palpate accessible muscles as they contract. Grading muscle strength and evaluating the patient's effort is an art that takes time and practice. Muscle strength is traditionally graded using the following scale: 0 = no movement 1 = flicker or trace of contraction but no associated movement at a joint 2 = movement with gravity eliminated 3 = movement against gravity but not against resistance 4 = movement against a mild degree of resistance 4 = movement against moderate resistance 4+ = movement against strong resistance 5 = full power d) Reflexes : The motor reflexes are involuntary contractions of muscles or muscle groups in response to abrupt stretching near the site of the muscles insertion. The tendon is struck directly with a reflex hammer or indirectly by striking the examiners thumb, which is placed firmly against the tendon. Testing these reflexes enables the examiner to assess involuntary reflex arcs that depend on the presence of afferent stretch receptors, spinal synapses, efferent motor fibers, and a variety of modifying influences from higher levels. Common reflexes that may be tested include the deep tendon reflexes (biceps, brachioradialis, triceps, patellar, and ankle reflexes) and superficial or cutaneous reflexes (abdominal reflexes and plantar or Babinski response) Grading reflexes: 4+ - hyperactive response often indicating pathology 3+ - brisk reacting than average may be normal response or indicating pathology 2+ - average response or normal response 1+ - hypoactive 0 - absent y Biceps reflex: The biceps reflex is elicited by striking the biceps tendon of the flexed elbow. The examiner supports the forearm with one arm while placing the thumb against the tendon and striking the thumb with the reflex hammer. The normal response is flexion at the elbow and contraction of the biceps y Triceps reflex : To elicit a triceps reflex, the patients arm is flexed at the elbow and positioned in front of the chest. The examiner supports the patients arm and identifies the triceps tendon by palpating 2.5 to 5 cm (1 to 2 in) above the elbow. A direct blow on the tendon normally produces contraction of the triceps muscle and extension of the elbow y Brachio radialis reflex: With the patients forearm resting on the lap or across the abdomen, the brachioradialis reflex is assessed. A gentle strike of the hammer 2.5 to 5 cm (1 to 2 in) above the wrist results in flexion and supination of the forearm.
y Patellar reflex: The patellar reflex is elicited by striking the patellar tendon just below the patella. The patient may be in a sitting or a lying position. If the patient is supine, the examiner supports the legs to facilitate relaxation of the muscles. Contractions of the quadriceps and knee extension are normal responses y Ankle reflex: To elicit an ankle (Achilles) reflex, the foot is dorsiflexed at the ankle and the hammer strikes the stretched Achilles tendon. This reflex normally produces plantar flexion. If the examiner cannot elicit the ankle reflex and suspects that the patient cannot relax, the patient is instructed to kneel on a chair or similar elevated, flat surface. This position places the ankles in dorsiflexion and reduces any muscle tension in the gastrocnemius.The Achilles tendons are struck in turn, and plantar flexion is usually demonstrated. y Superficial reflexes: The major superficial reflexes include corneal, gag or swallowing, upper/lower abdominal, cremasteric (men only), plantar, and perianal. These reflexes are graded differently than the motor reflexes and are noted to be present () or absent (-). Of these, only three are tested commonly. The corneal reflex is tested carefully using a clean wisp of cotton and lightly touching the outer corner of each eye on the sclera. The reflex is present if the action elicits a blink. Conditions such as a cerebrovascular accident or coma might result in loss of this reflex, either unilaterally or bilaterally. Loss of this reflex indicates the need for eye protection and possible lubrication to prevent corneal damage. The gag reflex is elicited by gently touching the posterior pharynx with a cotton-tipped applicator; first on one side of the uvula and then the other. Positive response is an equal elevation of the uvula and gag with stimulation. Absent response on one or both sides can be seen following a cerebrovascular accident and requires careful evaluation and treatment of the resultant swallowing dysfunction to prevent aspiration of food and fluids into the lungs. The plantar reflex is elicited by stroking the lateral side of the foot with a tongue blade or the handle of a reflex hammer.Stimulation normally causes toe flexion. Toe fanning (positive Babinski) is an abnormal response 3) SENSORY EXAMINATION The sensory system is even more complex than the motor system because sensory modalities are carried in different tracts located in different portions of the spinal cord. The sensory examination is largely subjective and requires the cooperation of the patient Assessment of the sensory system involves tests for tactile sensation, superficial pain, vibration, and position sense (proprioception). During the sensory assessment, the patients eyes are closed. Simple directions and reassurance that the examiner will not hurt or startle the patient encourage the cooperation of the patient. Tactile sensation is assessed by lightly touching a cotton wisp to corresponding areas on each side of the body. The sensitivity of proximal parts of the extremities is compared with that of distal parts. Pain and temperature sensations are transmitted together in the lateral part of the spinal cord, so it is unnecessary to test for temperature sense in most circumstances. Determining the patients sensitivity to a sharp object can assess superficial pain perception. The patient is asked to differentiate between the sharp and dull ends of a broken wooden cotton swab or tongue blade; Vibration and proprioception are transmitted together in the posterior part of the cord. Vibration may be evaluated through the use of a low-frequency (128- or 256-Hz) tuning fork. The handle of the vibrating fork is placed against a bony prominence, and the patient is asked whether he or she feels a sensation and is instructed to signal the examiner when the sensation ceases. Common locations used to test for vibratory sense include the distal joint of the great toe and the proximal thumb joint. If the
patient does not perceive the vibrations at the distal bony prominences, the examiner progresses upward with the tuning fork until the patient perceives the vibrations Position sense or proprioception may be determined by asking the patient to close both eyes and indicate, as the great toe is alternately moved up and down, in which direction movement has taken place. Integration of sensation in the brain is evaluated next. This may be performed by testing two-point discriminationwhen the patient is touched with two sharp objects simultaneously, are they perceived as two or as one? If touched simultaneously on opposite sides of the body, the patient should normally report being touched in two places. If only one site is reported, the one not being recognized is said to demonstrate extinction. Another test of higher cortical sensory ability is stereognosis. The patient is instructed to close both eyes and identify a variety of objects (eg, keys, coins) that are placed in one hand by the examiner 4) COORDINATION AND BALANCE Cerebellar influence on the motor system is reflected in balance control and coordination. Coordination in the hands and upper extremities is tested by having the patient perform rapid, alternating movements and point to-point testing. First, the patient is instructed to pat his or her thigh as fast as possible with each hand separately. Then the patient is instructed to alternately pronate and supinate the hand as rapidly as possible. Lastly, the patient is asked to touch each of the fingers with the thumb in a consecutive motion. Speed, symmetry, and degree of difficulty are noted. Point-to-point testing is accomplished by having the patient touch the examiners extended finger and then his or her own nose. This is repeated several times. This assessment is then carried out with the patients eyes closed. Coordination in the lower extremities is tested by having the patient run the heel down the anterior surface of the tibia of the other leg. Each leg is tested in turn. The Romberg test is a screening test for balance. The patient stands with feet together and arms at the side, first with eyes open and then with both eyes closed for 20 to 30 seconds. The examiner stands close to reassure the patient of support if he or she begins to fall. Slight swaying is normal, but a loss of balance is abnormal and is considered a positive Romberg test. Additional cerebellar tests for balance in the ambulatory patient include hopping in place, alternating knee bends, and heel-to-toe walking (both forward and backward). 5) GAIT Watching the patient walk is the most important part of the neurologic examination. Normal gait requires that multiple systemsincluding strength, sensation, and coordinationfunction in a highly integrated fashion. Unexpected abnormalities may be detected that prompt the examiner to return, in more detail, to other aspects of the examination. The patient should be observed while walking and turning normally, walking on the heels, walking on the toes, and walking heel-to-toe along a straight line. The examination may reveal decreased arm swing on one side (corticospinal tract disease), a stooped posture and short stepped gait (parkinsonism), a broad-based unstable gait (ataxia), scissoring (spasticity), or a high-stepped, slapping gait (posterior column or peripheral nerve disease), or the patient may appear to be stuck in place (apraxia with frontal lobe disease). INVESTIGATIONS a) X RAY EXAMINATION Spinal x-ray examinations are done to determine the status of individual vertebrae and their relationship to one another. If the patient experiences pain with certain movements, he or she may be asked to flex and extend the area of the spine being examined while the radiographs are taken. This allows detection of abnormal movement of the vertebrae. If the patient has possibly sustained trauma to the spine, particularly the cervical spine, radiographs are taken before immobilizing devices are
removed. Skull radiographs may be taken to detect skull fractures or foreign bodies. No special nursing care is required.
b) C.T. SCAN A computed tomographic (CT) scan is used for diagnosing neurological disorders of the brain or the spine. Some of the disorders that can be detected by CT are hemorrhage, ventricle size, cerebral atrophy, tumors, skull fractures, andabscesses. CT is used when MRI is contraindicated because of metal aneurysm clips or other metal implants. The scan may be performed with or without radiopaque contrast material to enhance the clarity of the images that are recorded. If contrast material is used, a series of images is filmed, and then the contrast material is given intravenously and another series of images is filmed. The patient should be questioned about any allergies to contrast material, iodine, or shellfish. The blood urea nitrogen (BUN) and creatinine levels should be checked before administration of contrast material because it is excreted through the kidneys. Patients with elevated BUN and creatinine or known renal disease may be unable to tolerate the contrast material. Contrast material is most commonly used if a tumor is suspected or following surgery in the area to be scanned. CT scans are commonly used in emergency evaluations because they can be done quickly, an important consideration if the patient is ventilated or unstable. NURSING CONSIDERATIONS: Essential nursing interventions include preparation for the procedure and patient monitoring. Preparation includes teaching the patient about the need to lie quietly throughout the procedure. A review of relaxation techniques may be helpful for claustrophobic patients. Sedation can be used if agitation, restlessness, or confusion will interfere with a successful study. Ongoing patient monitoring during sedation is necessary. If a contrast agent is used, the patient must be assessed before the CT scan for an iodine/shellfish allergy, as the contrast agent is iodine-based. An intravenous line for injection of the contrast agent and a period of fasting (usually 4 hours) are required prior to the study. Patients who receive an intravenous or inhalation contrast agent are monitored during and after the procedure for allergic reactions and other side effects, including flushing, nausea, and vomiting. c) M.R.I. SCAN: Magnetic resonance imaging (MRI) gives a more detailed picture of soft tissue than a CT scan. It is not as useful when looking for bony abnormalities. MRI is used for diagnosis of degenerative diseases such as multiple sclerosis, arteriovenous malformations, small tumors, hemorrhages, and cerebral and spinal cord edema. An MRI of the mediastinal cavity will determine if the thymus gland is enlarged and facilitate the diagnosis of myasthenia gravis. It is a longer procedure and may be difficult for unstable, disoriented, or ventilated patients. As with a CT scan, the MRI can be done with or without contrast material. Some facilities have the capability to perform magnetic resonance angiograms (MRAs). This test allows visualization of blood vessels and assessment of blood flow without being as invasive as a traditional angiogram. NURSING CONSIDERATIONS: Because of the magnetic fields being used, there are restrictions placed on patients undergoing an MRI and the health-care personnel who work within the MRI facility. Individuals with pacemakers or any type of metallic prosthesis are not able to undergo MRI or be in the room when one is performed. This is because the magnetic field is so strong that it could dislodge the prosthesis or pacemaker. Patientsare asked to remove all metal objects, such as jewelry or hair clips, before the
procedure. Individuals who may have accidentally acquired metallic foreign bodies (e.g., metal slivers in the eye or shrapnel that was not removed) may need an xray examination to determine the presence or absence of such objects. Even permanent make-up and tattoos can cause problems because of the metallic salts in the dyes. Other contraindications include gross obesity, claustrophobia, agitation and inability to cooperate, and inability to lie flat. It may be difficult for the patient to lie in one position for a prolonged period. The patients need for pain medication should be assessed before the procedure. Use of pillows for positioning may improve comfort. The narrow, tunnel-like structure of the MRI unit causes claustrophobia in some patients; some patients may require use of sedatives or open MRI units. Warn the patient that the procedure involves a noisy knocking sound. Encourage the use of deep breathing, guided imagery, and other relaxation techniques . d) POSITRON EMISSION TOMOGRAPHY: Positron emission tomography (PET) is a computer-based nuclear imaging technique that produces images of actual organ functioning. The patient either inhales a radioactive gas or is injected with a radioactive substance that emits positively charged particles. When these positrons combine with negatively charged electrons (normally found in the bodys cells), the resultant gamma rays can be detected by a scanning device that produces a series of two-dimensional views at various levels of the brain. This information is integrated by a computer and gives a composite picture of the brain at workThis test is useful in showing metabolic changes in the brain (Alzheimers disease), locating lesions (brain tumor, epileptogenic lesions), identifying blood flow and oxygen metabolism in patients with strokes, evaluating new therapies for brain tumors, and revealing biochemical abnormalities associated with mental illness. NURSING CONSIDERATIONS: Key nursing interventions include patient preparation, which involves explaining the test and teaching the patient about inhalation techniques and the sensations (eg, dizziness, lightheadedness, and headache) that may occur. The intravenous injection of the radioactive substance produces similar side effects. Relaxation exercises may reduce anxiety during the test. e) SINGLE PHOTON EMISSION COMPUTED TOMOGRAPHY: Single photon emission computed tomography (SPECT) is a three-dimensional imaging technique that uses radionuclides and instruments to detect single photons. It is a perfusion study that captures a moment of cerebral blood flow at the time of injection of a radionuclide. Gamma photons are emitted from a radiopharmaceutical agent administered to the patient and are detected by a rotating gamma camera or cameras; the image is sent to a minicomputer. This approach allows areas behind overlying structures or background to be viewed, greatly increasing the contrast between normal and abnormal tissue. It is relatively inexpensive, and the duration is similar to that of a CT scan. NURSING CONSIDERATIONS: The nursing interventions for SPECT primarily include patient preparation and patient monitoring. Teaching about what to expect before the test can allay anxiety and ensure patient cooperation during the test. Premenopausal women are advised to practice effective contraception before and for several days after testing, and the woman who is breastfeeding is instructed to stop nursing for the period of time recommended by the nuclear medicine department. The nurse may need to accompany and monitor the patient during transport to the nuclear medicine department for the scan. Patients are
monitored during and after the procedure for allergic reactions to the radiopharmaceutical agent. In a few institutions nurses with special education and training inject the contrast agent before a SPECT scan f) MYELOGRAM: A myelogram is an x-ray examination of the spinal canal and its contents. Following a lumbar puncture, cerebrospinal fluid is removed and sent for laboratory analysis. Contrast material is then injected into the subarachnoid space. The patient is moved into various positions and radiographs are taken. Compression of nerve roots, herniation of intravertebral disks, and blockage of cerebrospinal fluid circulation may all be detected by myelogram. NURSING CONSIDERATIONS: Following the procedure, the patient is kept on bedrest with the head elevated. This lessens the possibility of the contrast material getting into the cerebral cerebrospinal fluid circulation. The contrast material used for myelograms can lower the seizure threshold in some patients. Any patient with a known seizure disorder should have serum levels of anticonvulsants evaluated and be carefully observed for signs of seizures. Because of their invasive nature, a separate informed consent form may be required for the lumbar puncture and myelogram. The physician performing the test explains the risks, benefits, and possible complications of the examination. Patients who need these diagnostic procedures may have cognitive deficits; therefore, it may be necessary to obtain consent from the legal next of kin. g) ANGIOGRAM: An angiogram is an x-ray study of blood vessels that is used when an abnormality of cerebral or spinal blood vessels is suspected or to obtain information about blood supply to a tumor. Following injection of a local anesthetic, a catheter is inserted through the femoral artery and advanced until contrast material can be injected into the appropriate vessels. The dye then shows the vessels on the radiograph and provides information about the structure of specific vessels, as well as overall circulation to the area.
NURSING CONSIDERATIONS: Before an angiogram, the patient receives a clear liquid diet and has an intravenous needle in place. Informed consent must be obtained. BUN and creatinine levels are evaluated because the contrast material is excreted through the kidneys. Potential for bleeding is assessed by prothrombin time and partial thromboplastin time tests because a puncture is being made in a large artery. Typically, the patient receives some type of sedation before being transported to the angiography suite. During the injection of the contrast material, the patient may complain of severe heat sensations and a metallic taste in the mouth. The patient must lie still while the radiographs are being taken, and so should be told about the sensations he or she may experience. Patients who are disoriented or agitated may require sedation to complete the test. Following the procedure, pressure is maintained on the catheter insertion site and the patient is kept flat in bed for 6 to 8 hours to prevent bleeding from the insertion site. The patient may turn from side to side but must keep the affected leg straight. In addition to assessing vital signs, evaluate the catheter insertion site and the presence and quality of the popliteal and pedal pulses in the affected leg. Decreas or loss of the pedal pulse may indicate a clot in the femoral artery and should be reported to the physician immediately. Patients should be encouraged to increase oral intake in addition to the intravenous fluids that are administered to aid in the excretion of the contrast material. h) NON INVASIVE CAROTID FLOW STUDIES:
Noninvasive carotid flow studies use ultrasound imagery and Doppler measurements of arterial blood flow to evaluate carotid and deep orbital circulation. The graph produced indicates blood velocity. Increased blood velocity can indicate stenosis or partial obstruction. These tests are often obtained before arteriography, which carries a higher risk of stroke or death. Carotid Doppler, carotid ultrasonography, oculoplethysmography, and ophthalmodynamometry are four common noninvasive vascular techniques that permit evaluation of arterial blood flow and detection of arterial stenosis, occlusion, and plaques. i) TRANS CRANIAL DOPPLER: Transcranial Doppler uses the same noninvasive techniques as carotid flow studies except that it records the blood flow velocities of the intracranial vessels. Flow velocities of the basal artery can be measured through thin areas of the temporal and occipital bones of the skull. A hand-held Doppler probe emits a pulsed beam; the signal is reflected by the moving red blood cells within the blood vessels. Transcranial Doppler sonography is a noninvasive technique that is helpful in assessing vasospasm (a complication following subarachnoid hemorrhage), altered cerebral blood flow found in occlusive vascular disease or stroke, and other cerebral pathology. NURSING CONSIDERATIONS: When a carotid flow study or transcranial Doppler is scheduled, the procedure is described to the patient. The patient is informed that this is a noninvasive test, that a hand-held transducer will be placed over the neck and orbits of the eyes, and that some type of water-soluble jelly is used on the transducer. Either one of these low-risk tests can be performed at the patients bedside. j) ELECROENCEPHALOGRAM: An electroencephalogram (EEG) represents a record of the electrical activity generated in the brain. It is obtained through electrodes applied on the scalp or through microelectrodes placed within the brain tissue. It provides a physiologic assessment of cerebral activity. The EEG is a useful test for diagnosing and evaluating seizure disorders, coma, or organic brain syndrome. Tumors, brain abscesses, blood clots, and infection may cause abnormal patterns in electrical activity. The EEG is also used in making a determination of brain death. Electrodes are applied to the scalp to record the electrical activity in various regions of the brain. The amplified activity of the neurons between any two of these electrodes is recorded on continuously moving paper; this record is called the encephalogram. For a baseline recording, the patient lies quietly with both eyes closed. The patient may be asked to hyperventilate for 3 to 4 minutes and then look at a bright, flashing light for photic stimulation. These activation procedures are performed to evoke abnormal electrical discharges, such as seizure potentials. A sleep EEG may be recorded after sedation because some abnormal brain waves are seen only when the patient is asleep. If the epileptogenic area is inaccessible to conventional scalp electrodes, nasopharyngeal electrodes may be used. NURSING CONSIDERATIONS: To increase the chances of recording seizure activity, it is sometimes recommended that the patient be deprived of sleep on the night before the EEG. Antiseizure agents, tranquilizers, stimulants, and depressants should be withheld 24 to 48 hours before an EEG because these medications can alter the EEG wave patterns or mask the abnormal wave patterns of seizure disorders.Coffee, tea, chocolate, and cola drinks are omitted in the meal before the test because of their stimulating effect. The meal is not omitted, however, because an altered blood glucose level can also cause changes in the brain wave patterns. The patient is informed that the standard EEG takes 45 to 60 minutes, 12 hours for a sleep EEG. The patient is assured that the
procedure does not cause an electric shock and that the EEG is a diagnostic test, not a form of treatment. An EEG requires patient cooperation and ability to lie quietly during the test. Sedation is not advisable as it may lower the seizure threshold in patients with a seizure disorder and alter brain wave activity in all patients. Patients with seizures do not stop taking their antiseizure medication prior to testing. Routine EEGs use a water-soluble lubricant for electrode contact, which at the conclusion of the study can be wiped off and removed by shampooing. Sleep EEGs involve the use of collodion glue for electrode contact, which requires acetone for removal. k) EVOKED POTENTIAL STUDIES In evoked potential studies, electrodes are applied to the scalp and an external stimulus is applied to peripheral sensory receptors to elicit changes in the brain waves. Evoked changes are detected with the aid of computerized devices that extract the signal, display it on an oscilloscope, and store the data on magnetic tape or disk. These studies are based on the concept that any insult or dysfunction that can alter neuronal metabolism or disturb membrane function may change evoked responses in brain waves. In neurologic diagnosis, they reflect conduction times in the peripheral nervous system. In clinical practice, the visual, auditory, and somatosensory systems are most often tested. This test is used to detect a deficit in spinal cord conduction and to monitor spinal cord function during operative procedures. Because myelinated fibers conduct impulses at a higher rate of speed, nerves with an intact myelin sheath record the highest velocity. Demyelination of nerve fibers leads to a decrease in speed of conduction, as found in GuillainBarr syndrome, multiple sclerosis, and polyneuropathies. NURSING CONSIDERATIONS: There is no specific patient preparation other than to explain the procedure and to reassure the patient and encourage him or her to relax. The patient is advised to remain perfectly still throughout the recording to prevent artifacts (signals not generated by the brain) that interfere with the recording and interpretation of the test. l) ELECTROMYOGRAPHY: An electromyogram (EMG) is obtained by introducing needle electrodes into the skeletal muscles to measure changes in the electrical potential of the muscles and the nerves leading to them. The electrical potentials are shown on an oscilloscope and amplified by a loudspeaker so that both the sound and appearance of the waves can be analyzed and compared simultaneously. An EMG is useful in determining the presence of a neuromuscular disorder and myopathies. They help to distinguish weakness due to neuropathy (functional or pathologic changes in the peripheral nervous system) from weakness due to other causes. NURSING CONSIDERATION: The procedure is explained and the patient is warned to expect a sensation similar to that of an intramuscular injection as the needle is inserted into the muscle. The muscles examined may ache for a short time after the procedure. m) NERVE CONDUCION STUDIES Nerve conduction studies are performed by stimulating a peripheral nerve at several points along its course and recording the muscle action potential or the sensory action potential that results. Surface or needle electrodes are placed on the skin over the nerve to stimulate the nerve fibers. This test is useful in the study of peripheral neuropathies. n) LUMBAR PUNCTURE AND C.S.F. ANALYSIS: A lumbar puncture (spinal tap) is carried out by inserting a needle into the lumbar subarachnoid space to withdraw CSF. The test may be performed to obtain CSF for
examination, to measure and reduce CSF pressure, to determine the presence or absence of blood in the CSF, to detect spinal subarachnoid block, and to administer antibiotics intrathecally (into the spinal canal) in certain cases of infection. The needle is usually inserted into the subarachnoid space between the third and fourth or fourth and fifth lumbar vertebrae. Because the spinal cord divides into a sheaf of nerves at the first lumbar vertebra, insertion of the needle below the level of the third lumbar vertebra prevents puncture of the spinal cord. A successful lumbar puncture requires that the patient be relaxed; an anxious patient is tense, and this may increase the pressure reading. CSF pressure with the patient in a lateral recumbent position is normally 70 to 200 mm H2O. Pressures of more than 200 mm H2O are considered abnormal. A lumbar puncture may be risky in the presence of an intracranial mass lesion because intracranial pressure is decreased by the removal of CSF, and the brain may herniate downward through the tentorium and the foramen magnum A lumbar manometric test (Queckenstedts test) may be performed by compressing the jugularveins on each side of the neck during the lumbar puncture. The increase in pressure caused by the compression is noted; then the pressure is released and pressure readings are made at 10-second intervals. Normally, CSF pressure rises rapidly in response to compression of the jugular veins and returns quickly to normal when the compression is released. A slow rise and fall in pressure indicates a partial block due to a lesion compressing the spinal subarachnoid pathways. If there is no pressure change, a complete block is indicated. This test is not performed if an intracranial lesion is suspected. The CSF should be clear and colorless. Pink, blood-tinged, or grossly bloody CSF may indicate a cerebral contusion, laceration, or subarachnoid hemorrhage. Sometimes with a difficult lumbar puncture, the CSF initially is bloody because of local trauma but then becomes clearer. Usually, specimens are obtained for cell count, culture, and glucose and protein testing. The specimens should be sent to the laboratory immediately because changes will take place and alterthe result if the specimens are allowed to stand.
NURSING CONSIDERATIONS: PRE-PROCEDURE:1. Determine whether written consent for the procedure has been obtained. 2. Explain the procedure to the patient and describe sensations that are likely during the procedure (ie, a sensation of cold as the site is cleansed with solution, a needle prick when local anesthetic is injected). 3. Determine whether the patient has any questions or misconceptions about the procedure; reassure the patient that the needle will not enter the spinal cord or cause paralysis. 4. Instruct the patient to void before the procedure. PROCEDURE:1 The patient is positioned on one side at the edge of the bed or examining table with back toward the physician; the thighs and legs are flexed as much as possible to increase the space between the spinous processes of the vertebrae, for easier entry into the subarachnoid space 2 . A small pillow may be placed under the patients head to maintain the spine in a horizontal position; a pillow may be placed between the legs to prevent the upper leg from rolling forward.
3. The nurse assists the patient to maintain the position to avoid sudden movement, which can produce a traumatic (bloody) tap. 4. The patient is encouraged to relax and is instructed to breathe normally, because hyperventilation may lower an elevated pressure.. 5. The nurse describes the procedure step by step to the patient as it proceeds. 6. The physician cleanses the puncture site with an antiseptic solution and drapes the site. 7. Local anesthetic is injected to numb the puncture site, and then a spinal needle is inserted into the subarachnoid space through the third and fourth or fourth and fifth lumbar interspace. 8. A specimen of CSF is removed and usually collected in three test tubes, labeled in order of collection. A pressure reading may be obtained. The needle is withdrawn. 9. A small dressing is applied to the puncture site. 10. The tubes of CSF are sent to the laboratory immediately. POST PROCEDURE:1. Instruct the patient to lie prone for 2 to 3 hours to separate thealignment of the dural and arachnoid needle punctures in the meninges, to reduce leakage of CSF. 2. Monitor the patient for complications of lumbar puncture; notify physician if complications occur. 3. Encourage increased fluid intake to reduce the risk of postprocedure headache CONCLUSION Neurologic diseases are common and costly. Most patients with neurologic symptoms seek care from internists and other generalists rather than from neurologists. Because therapies now exist for many neurologic disorders, a skillful approach to diagnosis is essential. Errors commonly result from an overreliance on costly neuroimaging procedures and laboratory tests, which, while useful, do not substitute for an adequate history and examination. The proper approach to the patient with a neurologic illness begins with the patient and focuses the clinical problem first in anatomic and then in pathophysiologic terms; only then should a specific diagnosis be entertained. This method ensures that technology is judiciously applied, a correct diagnosis is established in an efficient manner, and treatment is promptly initiated. BIBILIOGRAPHY 1. Fauci braunwald and etal, HARRISONS PRINCIPLES OF INTERNAL MEDICINE , vol II, 17 th edition, Mc Graw Hill publications, United states, page no. 1689-1691 2. K. V. Krishna das, TEXTBOOK OF MEDICINE, 5th edition, jay pee publishers, New Delhi, page no. 928-935 3. Lewis and etal. MEDICAL SURGICAL NURSING 7th edition, mosby publications, Philadelphia, page no. 1758-1762 4. Black M.J. and etal, MEDICAL SURGICAL NURSING,7th edition, voliume 2, saunders publishers, Misouri. Pageno. 1694-1698. 5. Swash M., HUTCHINSONS CLINICAL METHODS, 21ST edition, saunders publishers, Misouri. Page no. 219-225.
6. 7. 8. 9.
www. Wikipedia. com www.nlm.nih.gov www.wisegeek.com www.britanica.com
You might also like
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- Mental Health Nursing Unit 1Document9 pagesMental Health Nursing Unit 1PihuNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Nursing Care of Head InjuryDocument1 pageNursing Care of Head InjuryRaveen mayiNo ratings yet
- 10 Nurses Proper Professional EtiquetteDocument1 page10 Nurses Proper Professional EtiquetteReva stevanaNo ratings yet
- Triage and Priority SettingDocument10 pagesTriage and Priority SettingekonurcahyaningrumNo ratings yet
- Nursing Careplan - Rectal CancerDocument5 pagesNursing Careplan - Rectal CancerdrugcardrefNo ratings yet
- Family Health Nursing: Ms - Neethu Vincent Asst Professor KVM College of NursingDocument9 pagesFamily Health Nursing: Ms - Neethu Vincent Asst Professor KVM College of NursingNeethu VincentNo ratings yet
- Neurological AssessmentDocument5 pagesNeurological AssessmentVIDYANo ratings yet
- F Discharge Plan 2019Document1 pageF Discharge Plan 2019Besael BaccolNo ratings yet
- Abdominal Paracentesis.Document4 pagesAbdominal Paracentesis.Sukh Preet100% (1)
- Plattischemic Stroke Lesson PlanDocument18 pagesPlattischemic Stroke Lesson Planapi-216258123100% (3)
- Newborn Care: Prepare The (Sterile) Hypo Tray-The Inner Side Is Considered SterileDocument5 pagesNewborn Care: Prepare The (Sterile) Hypo Tray-The Inner Side Is Considered Sterileallkhusairy6tuansiNo ratings yet
- Pain and Pain ManagementDocument7 pagesPain and Pain ManagementNatukunda DianahNo ratings yet
- History Taking FormatDocument10 pagesHistory Taking FormatMuskaan DeepNo ratings yet
- Sainath School of Nursing, GNM SyllabusDocument101 pagesSainath School of Nursing, GNM SyllabusFabin JoseNo ratings yet
- NCP Alcoholic NeuropathyDocument5 pagesNCP Alcoholic NeuropathyPeachy Marie Anca100% (1)
- NCLFNP - Mr. Robert McClelland CaseDocument4 pagesNCLFNP - Mr. Robert McClelland CaseAiresh Lamao50% (2)
- Drugs Used in CPR - Lesson PlanDocument12 pagesDrugs Used in CPR - Lesson Planmonika makwana100% (2)
- Guillan Barre Syndrome FinalDocument16 pagesGuillan Barre Syndrome FinalAswathy RCNo ratings yet
- PericarditisDocument45 pagesPericarditisBrenda WardshoneNo ratings yet
- Diphtheria SlideDocument11 pagesDiphtheria Slideandre andreNo ratings yet
- MHN, I (U), 6Document51 pagesMHN, I (U), 6akilaNo ratings yet
- The Education of Nurses On The Leading Edge of TransformationDocument31 pagesThe Education of Nurses On The Leading Edge of TransformationDip Ayan M100% (1)
- Critical Care NursingDocument2 pagesCritical Care NursingJyoti KathNo ratings yet
- Geriatric Considerations in Nursing: Priyanka. T M SC Nursing 1 YearDocument70 pagesGeriatric Considerations in Nursing: Priyanka. T M SC Nursing 1 Yearsanthiyasandy100% (1)
- Communication: DefinitionDocument18 pagesCommunication: Definitionannu panchalNo ratings yet
- Critical Care NursingDocument7 pagesCritical Care NursingShilpa JoshiNo ratings yet
- Shock Concept MapDocument2 pagesShock Concept MapElizabeth GarretsonNo ratings yet
- Abdominal Assessment VideoDocument4 pagesAbdominal Assessment VideoAmber Nicole HubbardNo ratings yet
- Teaching Plan 7Document61 pagesTeaching Plan 7dinman_rituraj1683No ratings yet
- Recreational TherapyDocument22 pagesRecreational TherapyKishore RathoreNo ratings yet
- Case Study About: Cardiac Failure and Pulmonary EdemaDocument32 pagesCase Study About: Cardiac Failure and Pulmonary EdemaIan Simon DorojaNo ratings yet
- Neurological DisordersDocument7 pagesNeurological Disordersomicspublishinggroup100% (1)
- Acute Renal FailureDocument17 pagesAcute Renal FailureDina Rasmita100% (1)
- Scope of Community Health Nursing PracticeDocument2 pagesScope of Community Health Nursing Practicechuniadsuar50% (2)
- Terminologies Used in Nursing Education 1Document11 pagesTerminologies Used in Nursing Education 1ramita sahNo ratings yet
- HistoryDocument16 pagesHistorySiri DevarapalliNo ratings yet
- NCP 1Document2 pagesNCP 1Roscelie KhoNo ratings yet
- Mental Helath Nursing ObjectivesDocument1 pageMental Helath Nursing ObjectivespgfhgfgfNo ratings yet
- Knowledge Regarding Skin Banking Among Student NursesDocument5 pagesKnowledge Regarding Skin Banking Among Student NursesAnonymous izrFWiQNo ratings yet
- 05 N293 33108Document23 pages05 N293 33108Arjay G ParaniNo ratings yet
- Concept, Philosophy, Aims & Objectives of Nursing EducationDocument12 pagesConcept, Philosophy, Aims & Objectives of Nursing EducationPruthviNo ratings yet
- Psychiatric EmergenciesDocument25 pagesPsychiatric EmergenciesAnnapurna DangetiNo ratings yet
- Kidney Stones: Kim Applebee Alex KaullenDocument26 pagesKidney Stones: Kim Applebee Alex KaullenPatrascu CristiNo ratings yet
- Chapter 004Document21 pagesChapter 004HannaNo ratings yet
- Lesson Plan of Health PromotionDocument8 pagesLesson Plan of Health Promotionsuman guptaNo ratings yet
- Care of Eye - FOOT AND NAILS NCPDocument12 pagesCare of Eye - FOOT AND NAILS NCPchaitali shankarNo ratings yet
- Cardiac AssessmentDocument7 pagesCardiac AssessmentElle ChasenNo ratings yet
- Colostomy CareDocument4 pagesColostomy CareRhenzes HaraNo ratings yet
- Av AidsDocument19 pagesAv AidsSachin SinghNo ratings yet
- Hebephrenic SchizophreniaDocument2 pagesHebephrenic SchizophreniaJanelle Matamorosa100% (1)
- NCP Acute Pain Related To Presence of Postoperative Surgical IncisionDocument2 pagesNCP Acute Pain Related To Presence of Postoperative Surgical IncisionAbdelmar SusulanNo ratings yet
- A Study to Assess the Knowledge Regarding Needle Stick Injuries among Staff Nurses in Selected Hospitals at Bangalore with a View to Develop an Information Booklet on Prevention of Needle Stick InjuriesDocument3 pagesA Study to Assess the Knowledge Regarding Needle Stick Injuries among Staff Nurses in Selected Hospitals at Bangalore with a View to Develop an Information Booklet on Prevention of Needle Stick InjuriesInternational Journal of Innovative Science and Research Technology100% (1)
- ChemotherapyDocument11 pagesChemotherapyRekha G.No ratings yet
- A Presentation On Hot Fomentation and Hot SpoonDocument21 pagesA Presentation On Hot Fomentation and Hot Spoongideon A. owusuNo ratings yet
- A Study To Assess The Effectiveness of Planned Teaching Program Regarding The Knowledge of Psycho Active Substance Abuse and Its Consequences On General Health Among The College STDocument5 pagesA Study To Assess The Effectiveness of Planned Teaching Program Regarding The Knowledge of Psycho Active Substance Abuse and Its Consequences On General Health Among The College STInternational Journal of Innovative Science and Research Technology100% (1)
- Introduction To Management: Mrs. G. S. ParanjpeDocument30 pagesIntroduction To Management: Mrs. G. S. Paranjpeshubham rathod0% (1)
- Lesson Plan SynopsisDocument19 pagesLesson Plan Synopsisshivani dasNo ratings yet
- Case Presentation On CAD-DVD: Lakhinana - Srilatha Y16PHD0813 V/V Pharm DDocument19 pagesCase Presentation On CAD-DVD: Lakhinana - Srilatha Y16PHD0813 V/V Pharm DAshu AmmuNo ratings yet
- Dazai OsamuDocument8 pagesDazai OsamuzamatinNo ratings yet
- Hepatitis BDocument61 pagesHepatitis BMichael AmandyNo ratings yet
- Dengue NS1 RDT Annex 5-6Document4 pagesDengue NS1 RDT Annex 5-6Ga B B Orlongan100% (1)
- The Preparation of The True Sulphur of AntimonyDocument20 pagesThe Preparation of The True Sulphur of AntimonyAlex BellNo ratings yet
- Central Nervous System StimulantsDocument6 pagesCentral Nervous System StimulantsNathalia CabalseNo ratings yet
- Parathyroid DisordersDocument19 pagesParathyroid DisordersmatrixtrinityNo ratings yet
- 1 - RF Report ?Document3 pages1 - RF Report ?مدى القحطانيNo ratings yet
- Pneumonia (Pulmonya)Document33 pagesPneumonia (Pulmonya)LopaoMedinaNo ratings yet
- Biliary Tract DiseaseDocument52 pagesBiliary Tract DiseaseAna Cotoman100% (1)
- Personality and Social DevelopmentDocument15 pagesPersonality and Social DevelopmentKri de AsisNo ratings yet
- Algoritma CKD PDFDocument2 pagesAlgoritma CKD PDFDesla Citra100% (1)
- CENE Course Outline On Psychiatric NursingDocument3 pagesCENE Course Outline On Psychiatric NursingJohn Ryan BuenaventuraNo ratings yet
- Speech DelayDocument16 pagesSpeech Delayian ismail100% (1)
- Planned Teaching On Occupational Health HazardsDocument8 pagesPlanned Teaching On Occupational Health HazardsgandhialpitNo ratings yet
- Case Study PresentationDocument21 pagesCase Study Presentationapi-272776993No ratings yet
- Mechanisms of Cataract Formation: Nicholas Phelps Brown MD, FRCS, FrcophthDocument7 pagesMechanisms of Cataract Formation: Nicholas Phelps Brown MD, FRCS, FrcophthQomariah RiaNo ratings yet
- InfectiousmeningitisDocument10 pagesInfectiousmeningitisHow ToNo ratings yet
- Cholinergic SyndromeDocument3 pagesCholinergic SyndromeEmman AguilarNo ratings yet
- Conjunctivitis A Systematic Review of Diagnosis and TreatmentDocument18 pagesConjunctivitis A Systematic Review of Diagnosis and TreatmentdasityarachmanNo ratings yet
- Physical Assessment For TABHSODocument10 pagesPhysical Assessment For TABHSOAqeel Al-MahdalyNo ratings yet
- Integrated Comprehensive Test IiiDocument14 pagesIntegrated Comprehensive Test IiiGhee Lardizabal0% (1)
- Revista Gastroenterologia Mexico: Scientific LetterDocument4 pagesRevista Gastroenterologia Mexico: Scientific LetterPriyanshu SinghNo ratings yet
- Graft Versus Host Disease..Document2 pagesGraft Versus Host Disease..Sakawath HosainNo ratings yet
- End Stage Renal Disease and DialysisDocument15 pagesEnd Stage Renal Disease and Dialysissome random dudeNo ratings yet
- Why Are Teens Eating So Badly?Document9 pagesWhy Are Teens Eating So Badly?Zaff Mat EfronNo ratings yet
- Physiological C-WPS OfficeDocument15 pagesPhysiological C-WPS OfficeGwagsiGlennNo ratings yet
- 5 6323480972671058006Document195 pages5 6323480972671058006Anonymous QOCn5dNo ratings yet
- Case Study CHNDocument23 pagesCase Study CHNKramer Dialola LacsonNo ratings yet
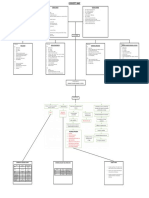
- IM-CAP Concept MapDocument1 pageIM-CAP Concept MapTrisNo ratings yet
- NCPDocument7 pagesNCPJulianne Jeamer FabroaNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4.5 out of 5 stars4.5/5 (6)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (254)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (60)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)