Professional Documents
Culture Documents
Quiz 2 Review
Uploaded by
Kelsey BissellOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Quiz 2 Review
Uploaded by
Kelsey BissellCopyright:
Available Formats
QUIZ #2 REVIEW Preoperative Evaluation #1 1) Discuss a general overview of preoperative assessment.
a) Goals of preoperative assessment i) Optimize patient care, satisfaction, comfort and convenience ii) Minimize perioperative morbidity and mortality by accurately identifying risk of anesthetics or might alter the planned technique iii) Minimize surgical delays or preventable cancellations iv) Determine appropriate post op disposition of the patient (where is procedure best performed?) v) Evaluate the patients health status, determining which if any preop consultations are required vi) Formulate a plan for the most appropriate perianesthetic care and post op patient care. vii) Communicate patient management issues effectively among care providers viii) Ensure time-efficient and cost-effective patient evaluation b) Preanesthesia Assessment Clinic i) Permit patient registration ii) Obtain a medical history and perform a physical examination iii) Promote patient teaching iv) Meet or schedule appointments with medical consultants v) Complete any required preoperative diagnostic testing
2)
Outline purpose and benefits of thorough chart review. a) Purpose i) To provide the basis for and direction of the patient interview and physical assessment. b) Benefits i) Alerts anesthesia provider to unusual conditions (ie. MH, atypical plasma cholinesterase surgical delay to get surgical/anesthetic records to provide information about patient care (ie. avoidance of succs, trigger-free anesthetic_ increasing safety for patient ii) Reviews and verifies patient name, date, and proposed surgery to decrease errors iii) Medical tx, Rx, I&O, diagnostic tests, H&Ps help to alert anesthesia provider to additional need for consultation, dx tests, or more questioning iv) Baseline social data (ie. culture, coping, limitations) can be obtained help to focus patient interview
(1)
3)
Examine key considerations in the Patient Interview/History, with emphasis in the following areas: a) Objectives of Preop Interview i) Ensure that goals of preop assessment are met ii) Provide preop education to patient and family iii) Obtain consent iv) Acquaint patient and family to surgical process v) Evaluate the patients social situation vi) Motivate the patient to comply with preventive care ie. smoking cessation, improvement of cardiovascular fitness. b) Surgical history i) Patients often have a hard time remembering surgical hx. ii) It is important to specifically ask about complications in the past ie. peripheral nerve injury, uncontrolled bleeding c) Anesthetic history i) Often not included in surgical hx ii) Possible adverse reactions: prolonged n/v, difficult airway, MH, post-op delirium, anaphylaxis, cardiopulmonary collapse)
d)
(1) Knowing adverse reactions allows alteration of the anesthetic plan reducing incidence of them iii) Take special note if a surgery was aborted and for what reason ie. difficult airway iv) Vague reports of fever or seizure/convulsion might = MH v) Familial anesthetic complications? (1) MH, atypical plasma cholinesterase, porphyria, glycogen storage diseases Drug history i) Helps to focus assessment ii) Patient with HTN or angina might need recent consult iii) Adverse drug effects/interactions may happen with anesthetics. (1) Sufficient time should be given for unwanted Rx to metabolize completely, usually 3-5 half lives. iv) Drug allergies (1) Understand which rx have side effects and which are true allergies (2) If a true allergy, it is absolutely contraindicated and other drugs of the same class should be avoided. v) Prescriptions (Table 20-1)
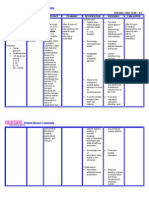
Intraoperative concerns w/ or w/out BP HR, intolerance to hypovolemia Management Optimize hydration, moderate vasopressor dose Discontinuation Issues Brief interruption is welltolerated, continuation may regional blood flow/O2 delivery and preserve renal fx, consider holding if pt. taking amio, >3 antihypertensive, or those that brief is unacceptable, omit BP AM dose day of surgery -blockers should be continued if they are used to treat angina, symptomatic arrhythmias or hypertension
Drug category Drugs affecting CV system ACE inhibitors
-blockers
d/c may CV morbidity and development of withdrawal sx (HR, nausea, MI, anxiety, headache)
Optimize hydration
Ca-channel blockers
SVR and BP d/t peripheral vasodilation, negative inotropic/chronotropic effect Hypokalemia, hypovolemia Cardiac depression, prolonged NMB, amio- BP, atropine resistant HR requiring v-pacing
Optimize hydration, phenylephrine prn to maintain atrial pressure Monitor K levels preop, maintain hydration Monitor serum drug levels, amio-lg doses of vasopressors or inotropes and pacemaker capability
Diuretics Antiarrhytmics
Drugs Affection Hemostasis Antiplatelets/NSAIDS
Continue chronic Ca-channel blockers in pts with normal or slightly impaired CV function; caution in pts w/ L ventricular dysfunction (EF<40%) Rarely symptomatic if AM dose withheld, might be good for pts treated for chronic renal failure d/c rarely recommended, amio life is 58 d so impractical to d/c, withhold concurrent meds ie. ACE inhibitors ASA d/cd 7-10d prior to high risk surgery. NSAIDs up to AM of surgery ok if pt not at risk for bleeding. If NSAIDs dcd short acting: 1d, long acting 23d Hep: dc IV 6h prior and check PTT Coumadin: dc 3-5d prior and check PT/INR LMWH: dc 12 h prior d/c usually not option (acute MI, PE) AM dose withheld or Withhold AM of surgery Older MAOIs: dc 2w w/risk of psych consequences or provide MAOI-safe anesthesia Newer MAOIs: dc AM of surgery If taking older MAOI, consider switching to newer MAOI weeks before surgery and then only withholding AM dose DC gradually over 2 weeks prior, obtain baseline EKG, if continued, take precautions to SE DC 72h prior
Impaired plt fx; altered renal fx, GI bleed
Anticoagulants (heparin, Coumadin)
Increased hemorrhage
Heparin reversed w/ protamine Coumadin reversed w/vit K or FFP Antifibrinolytic agent (aprotinin) may be used Monitor BG, use insulin protocol Monitor BG, avoid dehydration Avoid triggers such as Demerol, pentazocine, dextromethorphan, indirectacting sympathomimetic agents (ephedrine)
Fibrinolytic Drugs (TPA, streptokinase) Hypoglycemic agents Insulin PO hypoglycemic Drugs affecting CNS MAO Inhibitors
Hemorrhage Hyperglycemia; hypoglycemia Hyper/hypoglycemic HTN d/t sympathomimetic Rxs causing release of NE, excitatory state or depressive phenomena d/t opioid administration
Tricyclic antidepressants
Lithium
adrenergic blocking activity and potential to block NE arrhythmias or BP, lowers seizure threshold T-wave smoothing, V arrhythmias, myocarditis, sinus dysfunction-extreme atropine resistant HR, dehydrationserum lithium
NE vasopressor of choice
Optimize hydration
vi)
Herb Echinacea
Herbals (Table 20-2) Relevant Pharmacologic Effects Activation of cell-mediated immunity Perioperative Concerns Allergic reactions; effectiveness of immunosuppressives ie corticosteroids/cyclosporine; potential of immune suppression w/chronic use; inhibition of hepatic microsomal enzymes drg toxicity of drugs metabolized by liver ie phenytoin, rifampin, phenobarbital Risk of MI, stroke d/t HR/BP, V arrhythmias w/ halothane, chronic use depletes endogenous catecholamines intraop hemodynamic instability, life-threatening interaction with MAOIs risk for bleeding risk for bleeding Preoperative Discontinuation No data
Ephedra
BP/HR
>24h prior
Garlic Ginko
Inhibition of platelet aggregation; fibrinolysis, antiHTN Inhibition of platelet-activating
>7d prior >36h prior
Ginseng Kava
factor Lowers BG, inhibition of platelet aggregation, PT-PTT in animals, many others Sedation, anxiolysis
St. Johns Wort
Inhibition of neurotransmitter reuptake, MAOI unlikely
Valerian
Sedation
Hypoglycemia, risk for bleeding, anticoagulation effect of warfarin sedative effect of anesthetics, potential for addiction, tolerance and withdrawal Induction of cytochrome P-450 enzymes, affecting cyclosporine, warfarin, steroids, protease inhibitors, benzos, Ca-channel blockers; dig levels sedative effect of anesthetics, potential for addiction, tolerance and withdrawal; potential to anesthetic requirement w/long-term use
>7d prior >24h prior
>5d prior
No data
e)
Social History i) Tobacco
(1) (2) (3)
ii)
Nicotine affects the CV system by HR/BP/O2 consumption/PVRimpaired coronary blood flow and O2supply/demand ratio CO occupies O2 binding site on Hbg O2 transport and perfusion
life of nicotine: 40-60m (4) life of CO: 130-190 m (5) Patient should stop smoking at least 12 h before surgery ETOH (1) Testing tools (a) Alcohol Use Disorders Identification Test (AUDIT) (b) CAGE (>2 + = alcoholic)
(i) Do you feel you should Cut down on your ETOH consumption? (ii) Have people Annoyed you by criticizing your drinking habits? (iii) Have you felt Guilty about drinking? (iv) Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover?
Eye-opener (2) Has the pt experienced withdrawal symptoms? (3) Chronic ETOH = tolerance to CNS depressants (4) Acute intoxication/advanced ETOH = exaggerated response to anesthetics iii) Illicit Drug Use (Box 20-4) (1) Cocaine and marijuana most common (2) Most patients dont want to say (a) Evidence of drug injection (b) Opthalmologic changes (pupil constriction/dilation/nystagmus) (c) Lymphadenopathy (d) Malnourishment in amphetamine users (e) Poor dental care and bruxism for amphetamine users (f) Nasal perforation for cocaine users Patient teaching Informed consent i) Options for anesthesia given ii) Consent for general should always be done if other methods are not sufficient Diagnostic Testing i) Pregnancy test (1) If pt uncertain, pg test should be done If pregnant, elective surgery should wait until after 1st trimester CXR (1) Of little predictive importance, unless assessment requires (2) Risk outweighs benefit iii) EKG (1) Baseline EKG should be done if pt >50yo (2) Questions about cost-effectiveness of baseline EKG iv) Lab draws (1) K within 7 d of surgery if on diuretics or dig (2) BG Am of surgery Fasting considerations i) Risk of aspiration complications relatively low ii) Studies seem to indicate more liberal fasting guidelines ok iii) Long pre-op fasting can cause: (1) Dehydration, hypoglycemia (in sm children), hypovolemia, increased irritability, increased anxiety, reduced compliance with fasting orders, thirst, hunger, headache ii)
f) g) h)
(2)
i)
iv) New fasting guidelines (1) No gum or candy after MN (2) Clear liquids 2h prior (3) Breast milk 4h prior (4) Formula, milk or light meal >6h prior (5) Prescribed meds w/ sip of water 1h prior Preoperative Evaluation #2
4)
Formulate a system of quick and efficient patient evaluation. Focus on the following systems: a) Airway. Prediction of difficult airway (Table 20-3, 20-5) i) Should always be performed regardless of anesthetic plan ii) Tests for prediction of difficult intubation (1) Mallampati classification (a) Pt to stick out tongue and open mouth, but not phonate (b) Criticized for not being sensitive or reliable predictor of airway difficulty (c) I: visualization of soft palate, tonsillar fauces and pillars, uvula (d) II: visualization of soft palate, tonsillar fauces, uvula (e) III: visualization of soft palate, uvula (f) IV: soft palate not visualized (2) Thyromental distance (a) Neck fully extended w/mouth closed, measure distance between prominence of thyroid cartilage and chin. (b) <3 fingerbreadths or 7 cm = difficult intubation (3) Interincisor distance (a) Degree of mouth opening (b) <2 lg fingerbreadths or 4 cm = difficult intubation (4) Head/Neck movement (5) Mandibular Mobility (a) Ability to move the jaw forward and bite their lip iii) Dentition evaluation (1) Dental injuries are the most common reason for anesthesia-related claims b) Musculoskeletal i) Obesity (Box 20-6, 20-7) (1) Ideal body weight (a) Male=105 lb + 6 lbs/in >5 (b) Female = 100 lb + 5 lb/in>5 (c) 20% > IBW obesity (d) 2x IBW morbidly obese (2) BMI Weight in kg/height in m2 (b) 25-29.9: overweight (c) 30-34.9: moderate obesity (d) 35-39.9: severely obese (e) >40: morbidly obese (3) Cardiopulmonary (a) Asymptomatic patients should be screened for coronary disease if (i) Abnormal baseline EKG (ii) Hx of CAD/valve dz (iii) >50 yo w/metabolic syndrome, DM, HTN, smoking, dyslipidemia or family hx of CAD (4) Sleep apnea (a) Preop sleep study (5) Airway (a) Failed attempts 1:20 vs. 1:2200 (6) Question use of weight loss drugs ie amphetamines, Schedule IV appetite suppressants and antidepressants Ankylosing spondylitis and RA (1) Assess for NSAID/ASA, corticosteroid use (2) Severe ankylosis might make IV starts and intubation difficult
(a)
ii)
c)
RA can cause cricoarytenoid arthritis tracheal stenosis or decreased vocal cord movement (a) Sx: hoarseness, stridor, painful speech, dysphagia (4) Lung dz, effusions and cardiac conduction abnormalities may be present Neurological System i) Assess (1) Motor function (ie. gait) (2) Sensory system (ie. pain, touch, vibration) (3) Reflexes (4) CN abnormalities (5) Mental status and speech (6) Signs and sx of increasing ICP (a) Papilledema, unilateral mydriasis, HA made worse by coughing, n/v, slurred speech, disorientation, altered LOC, hemiplegia, neck rigidity (7) Hypothalamic ischemia d/t SAH or MI (a) Q waves, deep inverted T waves, prolonged QT intervals, and ST segment (8) GCS d/t TBI (a) <8 coma (b) Pre-op CT (0.5 cm midline shift of the brain) (9) Vertebral artery involvement
(3)
d)
(a) Do not (i) Extremes in head flexion, extension, rotation (b) Get 12 lead for carotid endarectomy Cardiovascular i) Assess (1) NYHA functional classification of heart dz (a) I: pt with cardiac dz, but have no functional limitations (b) II: pt with cardiac dz who are comfortable at rest, but experience fatigue, palpitation, dyspnea or angina with ordinary activity
(c)
III: pt w/ cardiac dz marked limitations to physical activity, comfortable at rest, but <ordinary activity causes sx
(d) IV: pt w/cardiac dz inability to carry on any physical activity w/out discomfort, sx at rest (2) Diagnostic tests (a) Stress test (b) Pharmacologic stress test (i) Echo or radionuclide scintigraphy are used with adenosine/dipyridamole (no inotropic stress) or dobutamine (inotropic stress) (c) Cardiac cath (i) Indicated for NYHA II or IV undergoing high risk surgery (ii) 3 identifiable findings that indicate poor ventricular function 1. CI<2.2 2. LV EDP >18 3. EF <40% (iii) Note wall motion abnormalities (3) Preexisting cardiac disease (a) HTN (i) >140/>90 (ii) If uncontrolled Stage III (>180/>110) and/or target-organ damage, surgery may be postponed until BP controlled (iii) What meds? (iv) c/o syncope or dizziness (b) Ischemic Heart dz (i) Risk factors 1. Age, smoking, DM, HTN, pulmonary disease, previous MI, LV wall dysfunction, PVD (ii) Sx should be determined at rest and w/activity (iii) Angina 1. Stable angina (predictable pain relieved by rest or NTG within 15 min) is no higher risk for intra-op MI than no angina
Unstable angina (new within 2mo, progressively worse, increased freq, intensity, or duration, less responsible to meds, occurs at rest or >30 minutes, transient ST or T changes or enzyme elevation) = risk of peri-op MI (iv) ACC/AHA guidelines: wait >4-6 w after MI for elective surgery (c) LV dysfunction (i) EF <35% = post op heart failure and death (ii) CHF sx Hx CHF, pulm edema, nocturnal dyspnea, bilateral rales, S3, CXR showing pulmonary vascular redistribution (iii) Elective surgery should be postponed until optimal ventricular performance can be achieved. (iv) Preop eval should be done within 12 mo of surgery (d) Valvular Heart dz (i) Rheumatic heart disease is most common cause of VHD (ii) Normal valves can accommodate 7x CO (iii) Identify type of valvular lesion before surgery
2.
1.
(iv) Severe aortic stenosis greatest risk = 14x greater perioperative sudden death elective surgery
should be postponed until CT consult (e) Arrhythmias (i) EKG, BMP, Rx levels, CXR before surgery (ii) Ventricular arrhythmia class 1. Benign ventricular arrhythmias (PVCs) 2. Potentially malignant V arrhythmias (Heart dz w/anti-arrhythmia meds) 3. Malignant V arrhythmias (heart dz, hemodynamic compromise and family hx of sudden death) (iii) Pacemaker (4) Disease severity, stability, prior tx (5) Comorbidity (DM, PVD, chronic pulmonary dz, social risk factors) (6) Type of surgery to be performed Respiratory i) Surgical site (thoracic and aortic) is most important risk factor for post-op pulmonary complications ii) Emphysema and chronic bronchitis (1) Elective surgery postponed if (a) Severe dyspnea, wheezing, pulmonary congestion, CO2>50
e)
(2)
iii)
Best way to intra-op pulmonary complications = stop smoking at least 8 weeks (3) Diagnostic tests (a) ABG, CXR (emphysema), PFT (poor indicator of post-op complications) Asthma
f) g)
h)
i)
(1) Meds should be continued on day of surgery (2) Stress dose of steroids might be needed throughout surgery (3) Anti-anxiety meds given because anxiety can be a trigger for asthma (4) Ensure adequate hydration iv) URTI (1) Consider postponing elective surgery if signs of active infection, but proceed if chronic condition (2) Lower respiratory infections are indication for postponement of surgery 4-6w GI i) n/v, diarrhea, GI bleed, abd pain, distention, palpable masses, GERD, dysphagia, fluid/electrolyte balance, weight loss, ulcers, hernia Hepatobiliary i) hepatobiliary problems can be difficult to dx d/t liver resilience ii) hepatic function may further decrease after anesthesia and surgery especially after abdominal procedures iii) All elective surgeries should be postponed in pt with advanced liver dz d/t increased morbidity and mortality (1) If emergency surgery is indicated, anesthetists should (a) Give FFP, cryo (b) Check frequent BG (c) ABG, LFT, BMP iv) AST, SGOT, ALT, SGPT and LDH are not always a good indication of liver failure v) Increased prothrombin time is one of the best indicators of acute hepatic injury vi) Cirrhosis and hepatitis common causes of liver failure in US Renal i) Assess (1) Fluid status, polyuria, incontinence/retention, hematuria, UTIs, dysuria, anuria ii) Tx and resolution of UTI should be performed prior to elective surgery esp before MVR or total hip iii) Creatinine clearance best lab to determine renal function or GFR (1) GFR = UV/P iv) Chronic renal failure management success should be measured on fluid/electrolyte balance (1) Measure K 6-8h prior to surgery v) Hbg prior to surgery vi) If coagulopathic, dialysis can correct bleeding times. vii) Administer antacids and drain peritoneal dialysate prior to surgery to decrease aspiration risk Endocrine i) DM (1) Most common endocrine disorder (2) 90-95% of DM patients are NOT dependent on insulin (3) Pts with DMII are more likely to have HTN, CAD, PVD (4) Major goal is to determine pre-op BG control and organ dysfunction (5) Assess (a) Diabetes: type, method of monitoring (b) Drugs (c) CV disease (d) Renal disease (e) Neuropathy (f) Airway (6) Postpone surgery if pt has severe hyperglycemia or ketoacidosis (7) Reglan should be given to increase motility and decrease aspiration risk (8) Surgery should be as early as possible to limit fasting time (9) Po hypoglycemic should be held AM prior or 48h prior depending on half life ii) Thyroid disorders (1) Hyperthyroidism (a) Graves disease, goiter, thyroid carcinoma and pituitary tumors (b) sx of a hypermetabolic state (c) antithyroids, beta-blockers, iodine are often used and should be continued intra-op (d) CBC w/plt should be done (e) Anticholinergics should be avoided d/t increased tachy-arrhythmias (2) Hypothyroidism (a) Hasimoto disease, chronic thyroiditis (b) T4/synthroid given iii) Adrenocortical disorders (1) Most commonly caused by chronic treatment with steroids
(2) (3)
Cushing syndrome: excess corticosteroids buffalo hump, HTN, moon face, easy bruising, osteoporosis, personality changes
j)
Addisons disease: adrenocortical insufficiencyskin hyperpigmentation, weight loss, hypotension, hypoglycemia, hyponatremia, hyperkalemia (4) Operative management: fluid/electrolyte balance, tx of coexisting disorders (ie. HTN), continue steroid use throughout surgery ASA status classification (Table 20-14) i) Class I: (1) Healthy patient ii) Class II (1) Milk to moderate systemic disease (2) Slightly limits physical activity: HTN, DM, anemia, obesity, age iii) Class III (1) Severe systemic disturbance
5)
(2) Limited activity d/t pulmonary or CV disease, poorly controlled HTN, DM with vascular complications, angina, hx of MI iv) Class IV (1) Severe systemic disturbance that is life threatening (a) CHF, persistent angina, advanced pulmonary, renal or hepatic dysfunction v) Class V (1) Moribund patient undergoing surgery as a resuscitative effort with minimal chance for survivial (a) Uncontrolled hemorrhage from AAA vi) Class E (1) Emergency surgery (2) Health 30 yo F requires a D&C for moderate but persistent hemorrhage is ASA IE Examine guidelines for prevention of operative errors (Box 20-18 may keep you out of court someday)
LECTURE 1. Goals of preop eval a. Identify risk i. Optimize patient care ii. Minimize mortality and morbidity iii. Minimize delays 1. Latex allergy preparation iv. Determine appropriate post-op disposition 1. ICU, home, PACU? v. Evaluate patients health status vi. Formulate plan vii. Communicate pt management issues with other medical staff viii. Frequently plans can change once pre-op assessment done 2. Chart Reivew a. Surgical consent b. Baseline data, height, weight, VS, I/O c. H&P d. Progress notes, consult reports (cath report, echo results, PFT, EF) e. MAR i. Abx schedule, dose, interval ii. Be familiar w/patients other meds iii. labs iv. Plavix: how long since last dose 1. Should be stopped 5-7d prior to surgery f. Keeps you looking professional 3. Patient interview a. Introductions b. In person best, over the phone will do c. We interview the patient, and they interview us d. Turn off TV e. Dont ignore the family f. Titles: CRNA, SNA i. Not nurse anesthesia resident g. Be sensitive, tactful, professional until patient is out 4. Patient Hx a. Jeffs questions i. Can I ask you some questions you may have already answered twice? 1. Allergies? 2. meds? a. Herbals? b. Prescription? 3. Any problems with heart? a. Murmurs, arrhythmias, HTN 4. lungs? a. Asthma, pneumonia, bronchitis 5. liver/kidneys? a. Hepatitis, diabetes 6. stomach? a. Heart burn, reflux? 7. back, neck, or spine? a. Any pain when you turn your head from side to side b. How about when you tilt your head back? 8. seizures or numbness 9. Any bleeding disorders a. Bloody nose lasting longer than 2 weeks? 10. Any illness of any kind? b. Probing, direct, open-ended questions c. Surgical/anesthetic history i. Any questions about anesthesia? ii. Any problems with anesthesia in the past? 1. Nausea/vomiting 2. Sore throat/difficult airway 3. Anaphylaxis 4. Difficulty waking up
d.
e.
5. Nerve injury? 6. Uncontrolled bleeding? Familial history i. Atypical plasma cholinesterase ii. MH iii. Porphyria Patient hx i. Meds 1. Benzo, pain, beta-blockers, anti-HTN, antivirals, steroids 2. Dosage, schedule, to d/c or not a. BP meds i. Take them unless they include a diuretic b. Diuretics i. dc c. antiarrhythmics i. take d. antiplatelets i. 5-7d prior e. Anticoagulants i. Heparin: IV infusion off prior ii. LMWH: dc 12 h prior iii. Coumadin: 3-5d, INR<1.5 f. Hypoglycemic i. PO: withhold AM prior ii. Insulin: AM dose, check sugar pre and post g. CNS drugs h. Steroids i. Stress dose given if any history ii. Herbal Drug hx 1. Echinancea: stimulates immune system. Potential hepatotoxicity 2. Ephedra: wt loss, increased energy. Sympathetic stimulation, HR and BP 3. The 3 Gs: inhibition of platelets, prolong PT, PTT 4. Kava: Anxiolysis, GAB mediated hypnotic effect. May change MAC levels 5. St. Johns Wort: Mood elevation, induces cytochrome P-450 6. Valerian: sleep aid, anxiolytic. GABA. May change MAC. BIS monitor? iii. Social hx 1. Tobacco a. Nicotine is a toxic alkaloid b. Naturally occurring pesticide i. 1 of >6000 other poisons c. You have a captive audience i. Teach, encourage
d.
e. f. g. h. i. 2. ETOH a. b. c. d. e.
Patients should be instructed to stop smoking 12h prior to surgery life of nicotine: 40-60m life of CO: 2-3h Many surgeons require total cessation Risks: i. Pneumonia, atelectasis, increased secretions, bronchospasm, decreased immune response Second hand smoke and kids i. Kids already have reactive airway ii. Second hand smoke increases asthmatic response and laryngospasm
3.
f.
Patient teaching i. Risks with anesthesia 1. Risk of broken teeth, bruised lip, sore throat, swelling, hoarseness
Accurate assessment may be difficult AUDIT and CAGE Benzos: drug of choice for prevention and treatment of withdrawals Depakote, tegretol are possibilities s/s of withdrawal i. tremors, sweating, tachycardia, HTN, anxiety, restlessness, n/v, anxiety, hallucinations, seizures f. preserve liver function i. use Rx that are not metabolized in the liver ie. cisatricurium Illicit drugs a. Scarring, needle tracks b. Opthalmological changes c. Lymphadenopathy d. Malnourishment, poor dentition e. Nasal perforation f. Acute abuse is worse i. Delay elective cases ii. We like predictable
2.
Aspiration, lung injury death
ii.
Allergic reactions: anaphylaxis Death 5. Nerve damage, blurred vision, blindness, blood-clots, IV infiltration, seizures, stroke, death 6. Awareness. Extremely rare Risks with spinal/epidural
3. 4. 1.
Changes in BP, HR, or rhythm death
Infection/hematoma paralysis 2. Back pain/nerve damage: persistent numbness, weakness, bowel/bladder dysfunction 3. Systemic toxicity: dizziness, unconsciousness, seizure, circulatory collapse, death 4. Spinal headache: how to tell if its just a caffeine headache. How its treated g. Informed consent i. Do you understand risks as explained? ii. Do you have any further questions? h. Diagnostic testing i. Rationale for routine labs 1. To detect asymptomatic modifiable conditions that could alter anesthetic care 2. To detect asymptomatic unmodifiable conditions that could alter anesthetic risk 3. Prevent medico legal issues ii. Abnormal test results potentially alter patient care only 0.22-0.56% of the time iii. Rationale to consider before ordering? 1. Is it cost-effective? a. Will the result pay for itself? 2. Positive benefit-risk ration a. Does benefit outweigh the risk of lab error 3. Are correctable prior to surgery? 4. Would common sense reveal the same results? 5. Are the results likely to alter patient care? iv. Rationale for day of surgery 1. Older than 6 mo, changes in patients health status justify the test 2. Results change more frequently than every 6 mo v. CXR 1. Rarely justified vi. EKG 1. Of limited value in asymptomatic patients 2. Rarely leads to changes in patient care 3. No evidence supports the value of baseline i. Fasting i. 3 variables 1. Time of scheduled surgery 2. Time at which patient retired for the night 3. Variability in gastric emptying for solids and fluids among individuals ii. Problems associated with prolonged pre-op fasting 1. Dehydration, hypoglycemia, hypovolemia 2. Irritability, pre-op anxiety, reduced compliance 3. Thirst, headache (caffeine), hunger iii. Conditions that increase regurg risk 1. Anxiety, esophageal surgery, mechanical obstruction, hiatal hernia, DM, pain, pregnancy, smoking Lecture 1.25.2012 Preop eval #2 5. Airway assessment a. The cornerstone of anesthetic practice i. Should be performed preoperatively on every patient regardless of the anesthetic plan ii. The most thorough airway assessment wont identify all difficult airways
iii.
Previous anesthetics are very helpful if available and accurate
It follows that your record needs to be accurate 2. Help the next poor soul iv. Crenellations: ridges on tongue from tongue not fitting well in mouth, might be indicative of sleep apnea v. Redundant tissue: tissue on the outside is most likely tissue on the inside, a good indicator of a difficult airway b. Mallampati airway assessment i. Class I: ii. Class II: no tonsillar pillars iii. Class III: iv. Class IV: only hard palate visible c. Sniffing position: aligning pharyngeal and laryngeal axis. d. Assess ROM to assess for possible AO injury e. Thyromental distance: where you displace the tongue during laryngoscopy. If no space, you will not be able to displace the tongue. i. >7 cm normal. ii. <6cm anterior airway f. Table 20-3 COMPONENTS OF THE PREOP AIRWAY PHYSICAL EXAM Airway exam component Cautionary finding Length of upper incisors Relatively long
1.
Relation of maxillary and mandibular incisors during normal jaw closure Relation of maxillary and mandibular incisors during voluntary protrusion of jaw Interincisor distance Visibility of uvula Shape of palate Complicance of mandibular space Thyromental distance Length of neck Thickness of neck ROM of head and neck
Prominent overbite Mandibular incisors infront of maxillary incisors <3cm Not visible when tongue is protruded with patient in sitting position (e.g. Mallampati class >II) Highly arched or very narrow Stiff, indurated, occupied by mass, not resilient <3 finger breadths or <6 cm Short Thick Pt cant touch tip of chin to chest or cant extend neck
g.
h. Conditions associated with difficult airway i. Facial abnomalities Mandibular hypoplasia, microgenia, micrognathia a. Pierre Robin syndrome b. Treacher Collins syndrome c. Cri du caht syndrome Mouth/Tongue anomalies 1. Congenital anomalies of the mouth/tongue
1.
ii.
iii. iv. v.
a. Freeman-sheldon (whistling face) Ludwig angina (swelling) a. Potentially life=threatening, rapidly expanding, diffuse inflammation of the submandibular and sublingual spaces. Usually caused by an abscessed tooth. i. Sx: severe neck pain, swelling, fever, malaise and dysphagia 1. Stridor suggests an impending airway crisis 2. Patient will be panicking ii. Tx: assessment and protection of the airway, IV antibiotics, surgical evaluation and if necessary operative decompression Thoracoabdominal 1. kyphoscoliosis Neck
2.
1.
Spine 1.
Webbed (Turner syndrome)
vi.
congenital a. limited c-spine mobility i. Klippel-Feil syndrome b. C-spine instability i. Down syndrome ii. Mobius syndrome iii. Larsen syndrome iv. Morquio syndrome 2. acquired a. RA Nasal pathology
6.
1. Choanal atresia vii. Tracheomalacia (Larsen syndrome) i. Dentition i. of all claims in the US ii. Documentation 1. Pre-op eval 2. Induction 3. Emergence iii. Can be a foreign body concern iv. People are proud of their teeth, even floppy teeth Latex allergy a. Chronic exposure to latex makes you more likely to have allergy i. Rubber industry, health care workers, pts requiring frequent catherization b. Spinal bifida c. >9 prior surgical procedures d. Allergy to food and tropical fruits or stone fruits i. Banana, avocado, kiwi, mango, peach, passion fruit, celery, chestnuts e. Hx of intraoperative anaphylaxis of unknown cause f. Atopic patients: placelessness, allergic to everything Musculoskeletal assessment a. IBW (male) i. 105lb + 6lb for each inch >5ft b. IBW (female) i. 100lb + 5lb for each inch >5ft c. BMI i.
BMI=weight (kg)/height m2
7.
d.
Issues i.
1. 2. 3. 4.
Overweight: 25-29.9 Moderate 30-34.9 Severe 35-39.9 Morbid: >40
Nothing worse than obesity for anesthesia >30 coexisting conditions 1. Wound infections 2. DVT 3. Positioning issues 4. DMII 5. CHRD 6. HTN Adversely effects every organ system Changes our anesthetic plan 1. Induction/emergence sequence Decreased FRC (functional residual capacity) faster intubation needed 3. Difficult airway/bag-mask 4. Drugs/gases 5. Positioning concern 6. Everything will be more difficult Conditions associated with obesity (box 44-1) 1. obstructive sleep apnea Ankylosing spondylitis Tolerance of positioning 2. Lots of pillows and blankets 3. Positioning injuries may not be preventable Medications (ASA, NSAIDs, steroids) Systemic problems are extensive during advances stages 1. Position, intubation (tracheal stenosis), difficult IV start 2. Restrictive lung disease (limited chest-wall movement) 3. Pericardial effusions, arrythmias
ii.
iii. iv.
2.
v. e. ROM?
i.
1.
ii. iii.
8.
Neuro a. b.
As a rule: Patients shouldnt wake up stupider than when they went to sleep Assess i. Gait, arm strength, grip, reflexes, CN ii. Mental status, speech, cognitive function iii. Sx of increased ICP 1. HA, n/v, slurred speech, ECG abnormalities 2. GCS (<8=coma, requires intubation) iv. Serum concentrations of anticonvulsants (ie. phenytoin and Phenobarbital) to determine if levels are therapeutic v. Preoperative CT/MRI with eval vi. Question use of succs if ICP is concern vii. Steroids: continue perioperatively, check glucoses
viii.
9.
Cardiovascular a. Evaluation performed to: i. Define risk 1. can this heart be stressed without failing? 2. exercise tolerance 3. increased risk associated with a. unstable angina, active CHF (cause?), recent MI (<30d=highest risk) b. HTN, SBP>140, DBP>90 c. Smoking (pack/yr hx), ETOH, caffeine, illicit drugs ii. Determine severity iii. Determine presence of co-morbidities 1. PVD, carotid disease, DM, silent MI iv. Determine if patient will benefit from further testing v. Form anesthetic plan 1. Emergency or elective? Wait 4-6 w after MI 2. GA, spinal, regional, local vi. Know difference between stable vs unstable angina b. Exam i. Overall: truncal obesity with purpura and striae suggestive of Cushings disease ii. VS: BP in both arms iii. Funduscopic examination: hypertensive retinopathy iv. Neck: carotid bruits, distended veins or enlarged thyroid gland v. Heart: abnormal rhythm or size, murmurs, or heart sounds vi. Lungs: rales or bronchospasm vii. Abd: bruits, masses, enlarged kidneys or abnormal aortic pulsation viii. Extremities: delayed or absent femoral pulses secondary to aortic coarctation; evidence of atherosclerosis, peripheral edema
Recognize potential for autonomic hyperrelexia : spinal cord injury and stimulation below the level of the lesion
c.
ix. Neurologic evaluation: see above LV dysfunction i. 3 findings that indicate poor LV function 1. CI <2.2 2. LVEDP > 18 3. EF <40% ii. Read cath report or echo results
d.
e.
iii. S3, gallop, JVD, peripheral edema Valvular disease i. May involve stenosis, incompetence or both ii. Rheumatic heart disease still the most common cause of adult valvular disease iii. Severe aortic stenosis associated with 14x incidence of perioperative death Why? Arrhythmias i.
Determine severity and limitations
ii. iii.
malignant: all of the above with hemodynamic compromise and family history of sudden death. Ask: Does it limit your activity? Pacers 1. preop key points a. have the pacemaker or defibrillator interrogated by a competent authority shortly before the anesthetic b. Identify the magnet rate and rhythm if a magnet mode is present and magnet use is planned c. Disable antitachycardia therapy if the device is a defibrillator 2. intraop key points monitor cardiac rhythm/peripheral pulse with pulse oximeter or arterial waveform disable the artifact filter on the EKG monitor Avoid monopolar electrosurgery Use bipolar ESU if possible, if not, then pure cut is better than blend or coag setting Position ESU ground pad to prevent electricity from crossing the generator-heat circuit, even if the pad must be placed on the distal forearm and the wire covered with sterile drape Postop key points a. Parameters should be determined for pacer with interrogation b. The ICD patient must be monitored until the antitachycardia therapy is restored b. c. d. e.
1. 2. 3.
benign arrhytmias: unifocal PVC potentially malignant: known organic heart disease and antiarrhythmic therapy
a.
3.
10. Respiratory a. Site and type of surgery are strongest predictors of complications b. Risk increases as incision approaches the diaphragm
c.
d. e.
f. g. h.
i.
Length of procedure: time is the enemy Positioning: lateral, prone, trendelenburg Effects of anesthesia on the lungs i. Inhibition of mucociliary clearance. ii. Inhibition of surfactant production iii. Increased capillary permeability iv. Increased sensitivity of pulmonary vasculature to neurohumoral mediators Ask about exercise intolerance, chronic cough or unexplained dyspnea Listen for wheezing, rhonchi, decreased breath sounds, dullness to percussion, prolonged expiratory phase Asthma i. Preop management is the same as if the patient was not having surgery. Business as usual ii. May need steroid stress dose coverage iii. Metered dose inhalers prior to surgery iv. Ask about recent hospitalizations for asthma attacks 1. Triggers? Anxiety? Upper respiratory tract infection i. Particularly in kids 1. Usually the surgery is done to treat chronic URTI ii. Elective cases should be postponed in patients who will benefit from delay iii. Dont ask more of an already compromised immune system
iv.
11. GI a.
Lower respiratory tract involvement is of increased concern postpone 4-6 w
Assess for
i.
ii. iii. iv.
n/v/d 1. requires further eval of fluid and electrolyte status 2. RSI GI bleeding 1. h/h, type and cross, fluid resuscitation prior to induction 2. RSI Abd pain or distention 1. bowel obstruction is scary even with a functioning NG tube 2. RSI Dysphagia, esophageal or pyloric strictures 1. RSI
GERD 1. most common 2. RSI b. If in doubt, RSI! 12. Hepatobiliary a. Issues i. Liver has tremendous reserve ii. LFT are limited in their ability to refeclt extent of liver disease iii. Unexplained jaundice should be thoroughly investigated 1. postpone elective surgery iv. sx of worsening hepatobiliary disease 1. coagulopathy, jaundice, tremors, increased DTR, ascites, spider nevi, splenomegaly 2. hepatorrenal failure is usually fatal 3. high incidence of morbidity/mortality 13. Renal a. Issues i. Volume status 1. i/o if hospitalized 2. diuresis ii. Any suspected dysfunction should be investigated prior to surgery 1. creatinine level most common 2. most accurate is 24h creatinine clearance 3. presence of UTI (UA encouraged) 4. extent of renal failure 5. time of last dialysis 6. current hct/hgb 7. Serum K within 6-8h of surgery iii. Common procedures 1. stents, TURP, TURBT, Stone manipulation with laser iv. Renal failure considerations 1. IV access can be challenging 2. NIBP placement in strange places 3. Dose for effect a. Use drugs metabolized by other routes when possible b. Dose for effect, not by weight 4. Positioning (fragile skin)
v.
5.
6.
14. Endocrine a. Diabetes i. Degree of control ii. Organ involvement 1. renal, CV, neuropathic, airway (stiff AO joints d/t glycosylation) 2. special care in cases of non-compliance and newly diagnosed diabetes 3. autonomic neuropathy a. orthostasis, lack HR response to valsalva, delayed gastric emptying b. gastrokinetic agents are a good idea. iii. Maintain serum glucose <180 and >110 iv. Hold oral meds, take AM dose of insulin v. Positioning 1. assess ROM preop 2. allow patient to position self on OR table and asses comfort a. may affect how we dose Versed 3. Document a. Not all positioning injuries are preventable vi. CXR
IV with saline on microdrip hypotension can cause AV shunt to clot off
vii.
Prayer sign (Barash, page 1297)
1.
b.
Thyroid i. Hyperthyroidism 1. Excess secretion of T3 and T4 a. Graves disease, goiter, hypermetabolism 2. Goals a. Euthyroid state i. Methimazole, PTU, propranolol ii. Continue perioperatively 3. Possible esmolol infusion 4. avoid anticholinergics 5. may require higher dose of versed ii. hypothyroidism 1. synthroid common
a simple clinical test that may be used to detect limited joint mobility in the hands. Inability of the patient to completely close the gaps between opposed palms and fingers when pressing the hands together in a praying position constitutes a positive prayer sign. Improvement is seen in a patient after he received 4 months of aggressive glycemic control.
2.
not too scary
15. ASA status classification a. ASA I: healthy patient b. ASA II: mild to moderate disease c. d. e. f.
i. DM, Heart dz that SLIGHTLY limits activity, anemia, chronic bronchitis, morbid obesity ASA III: severe disease i. Heart dz that limits activity, uncontrolled HTN, BM w/vascular complications, angina, hx MI ASA IV: life threatening i. CHF, persistent angina, advanced pulmonary, renal or hepatic dysfunction ASA V: moribund, palliative or resuscitative w/ minimal chance of survival i. Uncontrolled hemorrhage ASA E: emergency surgery i. D&C of 30yo for moderate but persistent hemorrhage (ASA IE)
16. Universal protocol guidelines
17. Valley questions
Quiz #2
1. 2. 3. 4. 5.
6.
Which is not an important of the pt anesthetic history? Diabetes If MAC/light sedation is planned, consent for general anesthesia is not necessary- false Pt with complex medications should be evaluated at least (1 week) prior to an elective scheduled procedure Factors that are used to calculate BMI include all except____ weight in pounds Which statement is true concerning adverse and allergic reactions? An allergic reaction to a medication makes that medications an absolute contraindication Which statement indicated a true allergic reaction- morphine makes my throat swell Which of the following is true concerning criteria for preoperative chest x ray- the risk of performing a chest x ray on asymptomatic patients less than In general diagnostic results is relevant within 6 months Aspiration risk screening is always significant
7. 8.
9.
10. Morbid obesity is defined as- body weight that is double the ideal body weight.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Scoliosis, Lordosis, and KyphosisDocument40 pagesScoliosis, Lordosis, and KyphosisRati W. PaneseNo ratings yet
- Bacterial VaginosisDocument11 pagesBacterial VaginosisMuh. Idham RahmanNo ratings yet
- Viral Exanthem (Main)Document94 pagesViral Exanthem (Main)Starlet Rhonadez Bito-onon OrielNo ratings yet
- Complete Blood Count: at A GlanceDocument6 pagesComplete Blood Count: at A Glancecsy123No ratings yet
- Nursing Care Plan Urinary Tract Infection (UTI)Document2 pagesNursing Care Plan Urinary Tract Infection (UTI)deric95% (97)
- Increased Intracranial Pressure (IICP)Document2 pagesIncreased Intracranial Pressure (IICP)Giselle Chloe Baluya icoNo ratings yet
- Mood StabilizersDocument6 pagesMood StabilizersLan FdzNo ratings yet
- NCM 219 ReviewDocument32 pagesNCM 219 ReviewKeanu Win CatipayNo ratings yet
- Om Health Campus Affiliated To Purbanchal University Gopikrishnanagar, KathmanduDocument107 pagesOm Health Campus Affiliated To Purbanchal University Gopikrishnanagar, KathmanduAdditi SatyalNo ratings yet
- Breast Cancer Awareness - 13 October 2019Document4 pagesBreast Cancer Awareness - 13 October 2019Times MediaNo ratings yet
- 03 Enf. SistemicasDocument12 pages03 Enf. SistemicasAgustin BuryakNo ratings yet
- Entamoeba Coli: BackgroundDocument4 pagesEntamoeba Coli: BackgroundJam Pelario100% (1)
- Hereditary Hemorrhagic Telangiectasia (HHT)Document15 pagesHereditary Hemorrhagic Telangiectasia (HHT)MarshallNo ratings yet
- Ascites Causes Diagnosis and TreatmentDocument24 pagesAscites Causes Diagnosis and TreatmentrifkaNo ratings yet
- MRCS Practice Papers Part A: Paper 2 Emqs: Second EditionDocument28 pagesMRCS Practice Papers Part A: Paper 2 Emqs: Second Editionhina arsh0% (1)
- Acute Diarrhea LaDocument38 pagesAcute Diarrhea LaBane LtpNo ratings yet
- Pre Conception CareDocument58 pagesPre Conception CareMarkos MakishaNo ratings yet
- Male and Female Pattern Hair LossDocument15 pagesMale and Female Pattern Hair LossRahul SrivastavaNo ratings yet
- 06 Case SheetDocument10 pages06 Case Sheetshad mansooriNo ratings yet
- NCP (Actual)Document2 pagesNCP (Actual)Silinna May Lee SanicoNo ratings yet
- Research Paper HIV Awareness of The STEMDocument6 pagesResearch Paper HIV Awareness of The STEMJohn Dave LansangNo ratings yet
- Cauda Equina SyndromeDocument3 pagesCauda Equina SyndromepuchioNo ratings yet
- Meniere's DiseaseDocument2 pagesMeniere's DiseaseNoelyn BaluyanNo ratings yet
- Non Small-Cell Lung Cancer in A 15-Year-Old NonsmokerDocument2 pagesNon Small-Cell Lung Cancer in A 15-Year-Old Nonsmokertonirian99No ratings yet
- Med Term 3 (1) - 231209 - 003105Document30 pagesMed Term 3 (1) - 231209 - 003105Anushka KarthikeyanNo ratings yet
- WSDDocument13 pagesWSDhinatakunhinata75No ratings yet
- Good Shepherd Hospital (Swaziland) TB Infection Control Policy Dec 2014Document30 pagesGood Shepherd Hospital (Swaziland) TB Infection Control Policy Dec 2014COMDIS-HSDNo ratings yet
- Subcutaneous MycosesDocument22 pagesSubcutaneous MycosesCut Raihan100% (1)
- Pretest Surgery (3) 55Document8 pagesPretest Surgery (3) 55Hasan A AsFourNo ratings yet
- Krok 1 Stomatology 2012Document22 pagesKrok 1 Stomatology 2012Saaha ParmarNo ratings yet