Professional Documents
Culture Documents
Is Besifloxacin Ophthalmic Suspension 0.6% Safe and Effective For Bacterial Conjunctivitis
Uploaded by
Mu'allim HawaryOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Is Besifloxacin Ophthalmic Suspension 0.6% Safe and Effective For Bacterial Conjunctivitis
Uploaded by
Mu'allim HawaryCopyright:
Available Formats
Philadelphia College of Osteopathic Medicine
DigitalCommons@PCOM
Physician Assistant Studies Student Scholarship Student Dissertations, Theses and Papers
1-1-2011
Is Besifloxacin Ophthalmic Suspension 0.6% Safe And Effective For The Treatment Of Bacterial Conjunctivitis?
Hetal R. Desai PA-S
Philadelphia College of Osteopathic Medicine, hetalde@pcom.edu
Recommended Citation
Desai, Hetal R. PA-S, "Is Besifloxacin Ophthalmic Suspension 0.6% Safe And Effective For The Treatment Of Bacterial Conjunctivitis?" (2011). Physician Assistant Studies Student Scholarship. Paper 38. http://digitalcommons.pcom.edu/pa_systematic_reviews/38
This Selective Evidence-Based Medicine Review is brought to you for free and open access by the Student Dissertations, Theses and Papers at DigitalCommons@PCOM. It has been accepted for inclusion in Physician Assistant Studies Student Scholarship by an authorized administrator of DigitalCommons@PCOM. For more information, please contact etheldrat@pcom.edu.
Is Besifloxacin Ophthalmic Suspension 0.6% Safe And Effective For The Treatment Of Bacterial Conjunctivitis?
Hetal R. Desai A SELECTIVE EVIDENCE-BASED MEDICINE REVIEW In Partial Fulfillment of the Requirements For The Degree of Master of Science In Health Sciences- Physician Assistant Department of Physician Assistant Studies Philadelphia College of Osteopathic Medicine Philadelphia, Pennsylvania
December 17, 2010
ABSTRACT OBJECTIVE: The objective of this systematic review is to determine whether or not besifloxacin ophthalmic suspension 0.6% is safe and effective for the treatment of bacterial conjunctivitis. STUDY DESIGN: Review of three trials in the English language, all published in 2009. DATA SOURCES: Randomized, double masked, multicenter parallel group studies comparing besifloxacin to a vehicle suspension or moxifloxacin were found using Ovid MEDLINE, and Cochrane databases. OUTCOME MEASURED: Resolution of bacterial conjunctivitis through reduced or eliminated signs or symptoms, the microbial eradication of the bacteria responsible for the disease, and the safety of the medication used in terms of adverse events while treating bacterial conjunctivitis with besifloxacin. RESULTS: All three double blinded RCTs demonstrated that besifloxacin was more safe and effective in treating bacterial conjunctivitis when compared with a vehicle suspension. When besifloxacin was compared with moxifloxacin, it was concluded that besifloxacin is not inferior to moxifloxacin for the treatment of bacterial conjunctivitis. CONCLUSIONS: The results of the RCTs demonstrate that besifloxacin for the treatment of bacterial conjunctivitis is safe and effective. More studies are needed comparing other drug treatments, different strengths, the safety and efficacy in children versus adults and the duration of the medicine adminitaration. Future studies will help to determine the best medicinal option in treating bacterial conjunctivitis safely and effectively. KEY WORDS: Besifloxacin, Bacterial Conjunctivitis
Desai, Besifloxacin & Bacterial Conjunctivitis 1
Introduction Bacterial conjunctivitis, whether acute or chronic is the most common eye disorder that nearly everyone will face at least once in their lifetime. Bacterial conjunctivitis is a disease that is symptomatically defined by a copious purulent discharge, mild eye discomfort due to sticky eyelids, redness and ocular irritation. The most common organisms to cause bacterial conjunctivitis are Staphylococci, Streptococci, Haemophilus, Pseudomonas, and Moraxella. In many cases, bacterial conjunctivitis is obtained from upper respiratory infections that have spread to the eye, although there are other ways of transmitting the disease. Many bacterial conjunctivitis cases are also due to transmission from an infected person to another through infected areas and close personal contact. Moreover, conjunctivitis can also exist due to viruses. Viral conjunctivitis is distinguished from bacterial conjunctivitis due to its characteristic clear discharge.1 This eye disease is of great importance to primary care patients due to the high prevalence of the disease. Due to its ability to affect anyone in all age groups, bacterial conjunctivitis is important to treat and prevent. Although it is a self limiting disease in most cases, the use of antibiotics for its treatment has ultimately led to reduced transmission, quicker recovery time, shorter duration of the disease and reduced complications from long standing disease.2 Prevention of bacterial conjunctivitis is also possible through management of associated diseases such as acute otitis media and bacterial pneumonia, which can result in bacterial conjunctivitis if untreated.1 Currently, methods that are used to treat bacterial conjunctivitis include topical antibiotics such as sulfacetamide 10%, polymixin-bacitracin-neomycin, and trimethoprimpolymixin. Broad spectrum topical antibiotics are sufficient to treat the disease and cultures of
Desai, Besifloxacin & Bacterial Conjunctivitis 2
the ocular discharge are done to determine antibiotic resistance or in cases refractory to medicinal treatment. The total direct and indirect cost of treating bacterial conjunctivitis in the United States in 2005 was estimated to be $589 million.2 Costs include primary care visits and the cost of medicinal treatment, primarily topical broad spectrum antibiotics. Besifloxacin is another topical antibiotic that can be used as an option to treat those who have been affected by bacterial conjunctivitis. Besifloxaxin is a fluoroquinolone that has fairly good broad spectrum antibiotic activity. It is an FDA approved drug for the treatment of bacterial conjunctivitis, that has shown success in treating bacterial conjunctivitis as well as preventing complications and reducing transmission as well as duration of the disease. Objective The goal of this review is to determine whether or not besifloxacin ophthalmic suspension 0.6% is safe and effective for the treatment of bacterial conjunctivitis. Previous randomized controlled trials that have been published on besifloxacin ophthalmic suspension 0.6% for the treatment of bacterial conjunctivitis have shown that besifloxaxin is a safe and effective treatment and can be used as an alternative to other topical antibiotics for the treatment of bacterial conjunctivitis. Methods The studies that were obtained for this analysis were RCTs that included patients over the age of 1 who were adequately diagnosed with bacterial conjunctivitis based on criteria set forth by the studies authors. The intervention that was utilized in each of these RCTs was besifloxacin ophthalmic suspension 0.6%. Comparisons to this intervention included moxifloxaxin ophthalmic suspension 0.5%, another fluoroquinolone in the treatment of bacterial
Desai, Besifloxacin & Bacterial Conjunctivitis 3
conjunctivitis and a vehicle suspension that did not include besifloxacin. To gather information on these studies, databases such as the Cochrane Database of Systematic Reviews, MEDLINE, and the Ovid interface were used. All articles that were chosen were selected based on their importance of the outcomes to patients. Inclusion criteria that were placed for the selection of the studies were: 1) studies that were published in 1996 or later. 2) Studies associated with POEMS. 3) Studies published in the English language. 4) Studies that were randomized controlled trials. 4) Studies that were not previously used in meta-analyses or systematic reviews. Searching for randomized controlled studies in English using the keywords besifloxacin, and bacterial conjunctivitis helped to selectively limit articles that were necessary and were of importance to the study. The studies that were finalized and chosen were: 1) Randomized, prospective, double masked, vehicle controlled trial comparing besifloxacin suspension 0.6% to a vehicle formulation without besifloxacin. 2) Multicenter, randomized, double masked, parallel group study comparing besifloxacin ophthalmic suspension 0.6% to moxifloxacin ophthalmic solution 0.5%. and 3) Randomized, multicenter, double-masked, vehicle controlled study that compared besifloxacin ophthalmic suspension 0.6% to a vehicle suspension without besifloxacin. The characteristics of all the studies that were used in this analysis are displayed in Table 1. The three RCTs are similar in inclusion and exclusion criteria. Interventions are also similar in all the trials. The number of participants in each study varies greatly, as well as the number of withdrawals from the trials.
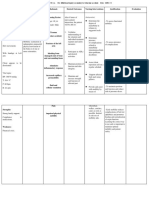
Table 1. Characteristics of Studies Included in the Systematic Review of Besifloxacin Ophthalmic Suspension 0.6% for the Treatment of Bacterial Conjunctivitis
Desai, Besifloxacin & Bacterial Conjunctivitis 4 Study Type
RCT, double masked
# Pts.
Age (yrs)
Inclusion Criteria
Minimum grade 1 for purulent conjunctival discharge, minimum grade 1 for either bulbar or palpebral conjunctival injection, pinhole visual acuity 20/200, negative pregnancy test
Exclusion Criteria
Hypersensitivity to fluroquinolones, besifloxacin, or any other ingredient used in the study, if a topical medication was used within 48 hours before or during study, if Abx were used w/in 72 hrs of the start of study, dx of viral/allergic conjunctivitis, hx of iritis, corneal erosion syndrome, ulcerative keratitis Use of ophthalmic solutions, ocular surgery within 6 weeks of start of study, viral/allergic conjunctivitis, ulcerative keratitis, corneal erosion syndrome, hypersensitivity to drug/drug class Use of systemic or topical Abx within 72 hrs, topical soln within 2 hours, anti-inflamm. agent within 48 hrs before or during the study, pregnant or nursing females, viral/allergic conjunctivitis, corneal erosion syndrome, ulcerative keratitis, immunocompromi sed, hypersensitivity to drug/drug class
W/D
Intervention
Besifloxacin ophthalmic suspension 0.6% given 3 times daily for 5 days
Karpecki, et.al., 2009
269
1+
13
McDonald ,et al., 2009
RCT, double masked
1161
1+
Healthy pts, grade 1 or more purulent discharge and injection, visual acuity of 20/200, agreement to d/c Abx agents, negative pregnancy test Visual acuity 20/200, method of contraception or negative pregnancy test, discontinued use of contact lenses
52
Besifloxacin ophthalmic suspension 0.6% given 3 times daily for 5 days
Tepedino, et al., 2009
RCT, double masked
957
1+
26
Besifloxacin ophthalmic suspension 0.6% applied 3 times daily for 5 days
Desai, Besifloxacin & Bacterial Conjunctivitis 5
Outcomes that were measured were POEMS such as the resolution of bacterial conjunctivitis through reduced or eliminated signs or symptoms, the microbial eradication of the bacteria that was the cause of the disease, and the safety of the medication used in treating bacterial conjunctivitis. Outcomes were measured using Cochran-Mantel-Haenszel (CMH), Pearson X2 test, Fisher exact test, individual safety outcomes assessments based on grading scales. Karpecki, DePaolis, Hunter, White, et al used 4 point scales for ocular discharge, bulbar conjunctival injection, where 0= absent, 1= mild, 2= moderate, and 3=severe. The clinical outcomes were then counted for each patient, and an overall score was determined. In the overall score, 0= scores for ocular discharge and bulbar conjunctival injection are 0, 1= improvement, current score less than day-1 score, 2= no change from baseline score, 3= worse, current score greater than day-1 score. In the study done by McDonald, Protzko, Brunner, Morris, et al, the investigators used a scale to determine global assessment of changes in clinical signs and symptoms where 0= cured, 1= improved, 2= no change from pretreatment, and 3= worse. Investigators Tepedino, Heller, Usner and Brunner, et al also used the same 0-3 rating scale for clinical outcomes where 0= resolution or cure, 1=improvement, 2= no change, and 3= worse. In all three RCTs, microbial eradication was measured through microscopy. Safety was measured in all studies using visual acuity and biomicroscopy for lids, limbus, conjunctiva, cornea, anterior chamber, lens and vitreous. Results Two RCTs compared besifloxacin with a vehicle suspension while another RCT compared besifloxacin with moxifloxacin, another topical ophthalmic antibiotic in the same drug class. Inclusion and exclusion criteria for each of the studies was fairly similar. Each study chose
Desai, Besifloxacin & Bacterial Conjunctivitis 6
participants who were above the age of 1 and healthy, non pregnant patients. The participants also had to have a minimum grade 1 for purulent ocular discharge and a minimum grade 1 for bulbar or palpebral conjunctival injection along with a pinhole visual acuity of greater than 20/200. The study excluded participants who had a hypersensitivity to fluoroquinolones, if the patients had used any topical medication on the eye within 48 hours of the start of the study, if antibiotics were used within 72 hours of the study or if the patient had a diagnosis of viral or allergic conjunctivitis. Patients with a history of corneal erosion syndrome, ulcerative keratitis, or iritis were also excluded from the studies. The results of the primary outcome, the treatment of bacterial conjunctivitis were presented in the articles as dichotomous data. All data from the studies were analyzed with the intention to treat, excluding those who were excluded from the study. In the investigation done by Karpecki et al, the clinical resolution of bacterial conjunctivitis was 43.1% and 73.3% in the control and besifloxacin groups respectively. The relative benefit increase (RBI) was 70.0%, and the absolute benefit increase (ABI) was 30.2%. The number needed to treat (NNT) was 4 patients. The difference in the control and experimental groups is statistically significant with the p-value less than 0.001.3 In the study done by McDonald et al, the clinical resolution of bacterial conjunctivitis was 84% in the moxifloxacin group, and 84.5% in the besifloxacin group. The relative benefit increase and absolute benefit increase was 0.60% and 0.5% respectively. The number needed to treat was 200 patients. All data was included in a 95% confidence interval for RBI and ABI.4 The investigation done by Tepedino et al in comparing a vehicle suspension with besifloxacin ophthalmic suspension 0.6% yielded a clinical resolution and microbial eradication
Desai, Besifloxacin & Bacterial Conjunctivitis 7
of bacterial conjunctivitis of 69.1% in the control group, and 84.4% in the besifloxacin group. The relative risk benefit and absolute benefit increase is 22% and 15.3% respectively. The number needed to treat was 7 patients. All data was statistically significant with a p-value of 0.0011.5 Table 2 shows a summary of all three studies and the results for the clinical resolution of bacterial conjunctivitis in each study. Table 2. Clinical Resolution of Bacterial Conjunctivitis with Besifloxacin Suspension 0.6% Study Besifloxacin Control group group resolution resolution of illness of illness 73.3% 43.1% p-value Odds Ratio (95% CI) RBI ABI NNT
Karpecki, <0.0001 NR 70.0% 30.2% 4* 2009 McDonald, 84.5% 84% NR (-5.6%0.60% 0.5% 200* 2009 6.75%) Tepedino, 84.4% 69.1% 0.0011 NR 22% 15.3% 7* 2009 CI= Confidence Interval, RBI= Relative Benefit Increase, ABI= Absolute Benefit Increase, NNT= Number Needed to Treat, NR= Not Reported * The outcome that was measured was the clinical resolution of bacterial conjunctivitis. The NNT means that for every 4/200/7 patients who participated and received besifloxacin treatment, there was one more resolution of bacterial conjunctivitis than in the group of patients taking the vehicle suspension or the moxifloxacin suspension. Each study also calculated the incidence of adverse effects in terms of safety of besifloxacin ophthalmic suspension 0.6%. In the study done by Karpecki et al, the incidence of adverse events for besifloxacin group was 50.4%, and was 53% for the control group. The relative risk increase (RRI) was -4.9%, and the absolute risk increase (ARI) was -3.0%. The number needed to harm is -34 patients. In the study completed by McDonald et al, the incidence of ocular adverse events was 12% in the besifloxacin group and 14% in the control group with moxifloxacin. The relative risk increase was -14.3% and the absolute risk increase was -2.0%. The number needed to harm was
Desai, Besifloxacin & Bacterial Conjunctivitis 8
-50 patients.4 Tepedino et al completed a study between a vehicle suspension and besifloxacin ophthalmic suspension 0.6% in which the incidence of adverse events for the besifloxacin group was 9.2% and the adverse events for the control group, or the vehicle suspension without besifloxacin was 13.9%. The relative risk increase was calculated to be 33.8% and the absolute risk increase was calculated as -4.7%. The number needed to harm in this study was -22 patients. The data in this study was statistically significant with a p-value of 0.0047. Table 3 shows a summary of the incidence of adverse events in patients with besifloxacin and in the control group for each study performed.5 Table 3- Incidence of Adverse Events of Besifloxacin and Control Groups Study Besifloxacin Incidence of Adverse Events Control Group Incidence of Adverse Events 53% p-value RRI ARI NNH
Karpecki, 50.4% NR -4.9% -3.0% -34* 2009 McDonald, 12% 14% NR -14.3% -2.0% -50* 2009 Tepedino, 9.2% 13.9% 0.0047 -33.8% -4.7% -22* 2009 RRI= Relative Risk Increase, ARI= Absolute Risk Increase, NNH= Number Needed to Harm, NR= Not Reported * Since the outcome measured were adverse events in those participants receiving besifloxacin ophthalmic suspension 0.6%, the values mean that for every -34/-50/-22 patients treated with besifloxacin, there was one fewer incidence of adverse events experienced than in the group receiving the vehicle solution. In all three studies performed with besifloxacin, the most common adverse event that was reported was ocular irritation. Patients reported itching of the eyes or irritation after administration of the medication. However, in all three studies, the incidence of adverse events
Desai, Besifloxacin & Bacterial Conjunctivitis 9
in the besifloxacin group were significantly lower than the incidence of adverse events in the control group, whether it be a vehicle suspension without besifloxacin or moxifloxacin. The most common adverse events that were reported in each of the studies was eye irritation, blurred vision and ocular pruritis. Karpecki and associated analyzed ocular adverse events in the experimental and control groups. They determined that the overall ocular adverse event rate in the eyes that were treated with besifloxacin was 34.7%, whereas the ocular adverse event rate in the eyes that were treated with vehicle suspension not containing besifloxacin was 38.8%. Table 3 displays the results of the ocular adverse events that occurred during the Karpecki et al study on besifloxacin.3 Table 3. Incidence of Ocular Adverse Events in Besifloxacin and Vehicle Suspension Groups Ocular Adverse Event Eye Pain Blurred Vision Eye Irritation n= number of participants Discussion In the double masked RCT that was conducted by Karpecki and associates, the results displayed success for the besifloxacin intervention. The clinical resolution of bacterial conjunctivitis was 73.3% for the besifloxacin experimental group whereas the resolution of bacterial conjunctivitis was 43.1% for the vehicle suspension group. Both interventions were administered similarly 3 times a day for 5 days.3 McDonald et al determined in their double blinded RCT that moxifloxacin and besifloxacin were similar in efficacy due to their similar properties. The clinical resolution for besifloxacin and moxifloxacin was 58.3% and 59.4% respectively. The solutions were also used three times daily for a total of 5 days. The study also Besifloxacin (n=190) 20 (10.5%) 20 (10.5%) 14 (7.4%) Vehicle (n=188) 13 (6.9%) 22 (11.7%) 23 (12.2%)
Desai, Besifloxacin & Bacterial Conjunctivitis 10
noted that the 95% Confidence Interval of the clinical resolution rates showed that besifloxacin was not inferior to moxifloxacin despite a difference in their success rates.4 The administration of besifloxacin and a vehicle suspension for three times daily for five days in the Tepedino et al double blinded study also yielded results in favor of the besifloxacin intervention. The clinical resolution of bacterial conjunctivitis in the besifloxacin group and in the vehicle group without besifloxacin was 45.2% and 33.0% respectively.5 All three of the RCTs included a patient population over the age of 1. However, there is no information on the results of clinical resolution and adverse events of besifloxacin between children and adults. More information is needed on the efficacy of the medication between the two groups as well as the strength and the administration of the medication that can be given to children versus adults. This information will likely allow primary care providers to determine if besifloxacin is safe and effective for children also. Authors of the RCT also mentioned that besifloxacin, a fluoroquinolone was effective in eradicating the bacteria that are the most likely causes for bacterial conjunctivitis. Fluroquinolones cover Gram positive bacteria as well as Gram negative bacteria, and the efficacy of besifloxacin in the microbial resolution of the bacterial conjunctivitis is vital information on treating most cases of bacterial conjunctivitis. A limitation of each study was the comparison of clinical resolution rates between treating bacterial conjunctivitis symptomatically with no medication and using besifloxacin for treating bacterial conjunctivitis from Day 1. There is no information on how the outcome of the disease would have been in regards to duration of the disease if besifloxacin was not used for five days to treat the illness. A study comparing the duration of the disease in using besifloxacin
Desai, Besifloxacin & Bacterial Conjunctivitis 11
versus no medication would be helpful to determine if bacterial conjunctivitis is a disease to be treated with medications or not. Conclusions The trials that were reviewed established that besifloxacin is safe and effective in treating bacterial conjunctivitis. Since besifloxacin suspension was only studied using one strength, 0.6%, there was a limitation in knowing the efficacy at different strengths of the medication. Future studies should be designed to include different classes of drugs that can be used to treat bacterial conjunctivitis. The length of the administration of the medication should also vary to determine the recommended duration of treatment. The results of these future studies will help to determine the best medicinal option in the treatment of bacterial conjunctivitis.
References 1. Riordan-Eva P. Chapter 7. Disorders of the Eyes & Lids. In: McPhee SJ PM, ed. CURRENT Medical Diagnosis and Treatment. 50th ed. The McGraw Hill Companies; 2011 2. Smith, A. F., Waycaster, C. Estimate of the direct and indirect annual cost of bacterial conjunctivitis in the United States. BMC Ophthalmology. 2009;9(13). 3. Karpecki P, Depaolis M, Hunter JA, et al. Besifloxacin ophthalmic suspension 0.6% in patients with bacterial conjunctivitis: A multicenter, prospective, randomized, doublemasked, vehicle-controlled, 5-day efficacy and safety study. Clin Ther. 2009;31(3):514526. 4. McDonald MB, Protzko EE, Brunner LS, et al. Efficacy and safety of besifloxacin ophthalmic suspension 0.6% compared with moxifloxacin ophthalmic solution 0.5% for treating bacterial conjunctivitis. Ophthalmology. 2009;116(9):1615-1623.e1. 5. Tepedino ME, Heller WH, Usner DW, et al. Phase III efficacy and safety study of besifloxacin ophthalmic suspension 0.6% in the treatment of bacterial conjunctivitis. Current Medical Research & Opinion. 2009;25(5):1159-1169.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- AbstractDocument1 pageAbstractMu'allim HawaryNo ratings yet
- Anterior UveitisDocument23 pagesAnterior UveitisRidy Ishvara PNo ratings yet
- Alur ApkDocument1 pageAlur ApkMu'allim HawaryNo ratings yet
- 15-Clinical Pathway Audit Tools A Systematic Review - Cari RefDocument20 pages15-Clinical Pathway Audit Tools A Systematic Review - Cari RefKang Heru Angon PitekNo ratings yet
- 1 Care Plan For 1 MalaysiaDocument47 pages1 Care Plan For 1 MalaysiaJoel LamNo ratings yet
- Anxiety Disorder GuidelinesDocument30 pagesAnxiety Disorder GuidelinesAlina Isabela CurtNo ratings yet
- Buku Saku Faq BPJS PDFDocument134 pagesBuku Saku Faq BPJS PDFFadli NugrahaNo ratings yet
- 2012 Speaker PL5 Ali Ghufron MuktiDocument7 pages2012 Speaker PL5 Ali Ghufron MuktiMu'allim HawaryNo ratings yet
- 15-Clinical Pathway Audit Tools A Systematic Review - Cari RefDocument20 pages15-Clinical Pathway Audit Tools A Systematic Review - Cari RefKang Heru Angon PitekNo ratings yet
- ADA Guidelines 2012Document53 pagesADA Guidelines 2012Jones PessoaNo ratings yet
- GAD AlgorithmDocument24 pagesGAD AlgorithmMu'allim HawaryNo ratings yet
- PeripartumDocument6 pagesPeripartumactininaNo ratings yet
- Risk Factors of Emergency HemodialysisDocument7 pagesRisk Factors of Emergency HemodialysisMu'allim HawaryNo ratings yet
- Crit Care Nurse 2010 Smithburger 24 30Document9 pagesCrit Care Nurse 2010 Smithburger 24 30Mu'allim HawaryNo ratings yet
- HerniaDocument31 pagesHerniaRahayu Tri NuritasariNo ratings yet
- Go No RheaDocument11 pagesGo No RheaMu'allim HawaryNo ratings yet
- Diarrhea AlgorithmDocument1 pageDiarrhea AlgorithmMarwan M.No ratings yet
- American Diabetes Association (ADA) gUIDELINESDocument43 pagesAmerican Diabetes Association (ADA) gUIDELINESSamuel Rudolf Maranatha JulioNo ratings yet
- Antihypertensive Drugs: Types, Side Effects and AdviceDocument3 pagesAntihypertensive Drugs: Types, Side Effects and AdviceMu'allim HawaryNo ratings yet
- Proton Pump Inhibitor Therapy For Peptic Ulcer BleedingDocument11 pagesProton Pump Inhibitor Therapy For Peptic Ulcer BleedingMu'allim HawaryNo ratings yet
- Diarrhea AlgorithmDocument1 pageDiarrhea AlgorithmMarwan M.No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- INNOVATIVE CARE LINEDocument4 pagesINNOVATIVE CARE LINEJose Luis Paez NeiraNo ratings yet
- Training of Top US Distance SwimmersDocument45 pagesTraining of Top US Distance SwimmersMel HarbourNo ratings yet
- Guava Soap Cures AcneDocument10 pagesGuava Soap Cures AcneAubrey VaflorNo ratings yet
- Hypnosis, Past Lives and NLPDocument8 pagesHypnosis, Past Lives and NLPZiad Cassim (anti-Sufi)100% (1)
- Narcotic Drugs: Opium Herion Codeine Tramadol MorphineDocument9 pagesNarcotic Drugs: Opium Herion Codeine Tramadol MorphineSyed renobaNo ratings yet
- Akf Stok 13Document67 pagesAkf Stok 13Grace Riani Pongsipulung TariganNo ratings yet
- 53 Vol. 6 Issue 7 IJPSR 2015 RA 4953Document9 pages53 Vol. 6 Issue 7 IJPSR 2015 RA 4953Dina AyupnNo ratings yet
- Disturbing Art Exposes Modern Culture AbsurditiesDocument15 pagesDisturbing Art Exposes Modern Culture Absurdities2aethicusNo ratings yet
- XxssDocument13 pagesXxssfkhunc07No ratings yet
- Psychology All Case Studies PDFDocument54 pagesPsychology All Case Studies PDFArmeen AmirNo ratings yet
- Types of Casts and Their IndicationsDocument3 pagesTypes of Casts and Their IndicationsPhylum ChordataNo ratings yet
- 13497-Texto Del Artículo-48998-1-10-20150925Document7 pages13497-Texto Del Artículo-48998-1-10-20150925Pipe Contecha BernatteNo ratings yet
- Farm NoteDocument3 pagesFarm NoteSreya Sanil50% (2)
- NCP OrthoDocument2 pagesNCP OrthoJeyser T. GamutiaNo ratings yet
- XZXZDocument4 pagesXZXZhenpupraNo ratings yet
- Master Tong-Style Acupuncturist Interview Part 1Document4 pagesMaster Tong-Style Acupuncturist Interview Part 1Anonymous uMnup2r100% (1)
- Medical Council of Inida Declaration Form 2010-2011for FacultyDocument9 pagesMedical Council of Inida Declaration Form 2010-2011for FacultydrtpkNo ratings yet
- Pathology of JointsDocument13 pagesPathology of JointswobblegobbleNo ratings yet
- Sample ResumeDocument3 pagesSample Resumeapi-380209683% (6)
- BUFFER STOK SO TGL 27des2021Document3 pagesBUFFER STOK SO TGL 27des2021Putu NindyaNo ratings yet
- Poster Competition Rules PDFDocument2 pagesPoster Competition Rules PDFZulfan ZulfanNo ratings yet
- Periodontal DressingDocument9 pagesPeriodontal DressingDilaC.FareshaNo ratings yet
- Edna K.huffman - Health Information Managemen 1994Document36 pagesEdna K.huffman - Health Information Managemen 1994gspot967% (6)
- Treponema Pallidum: Human PathogensDocument27 pagesTreponema Pallidum: Human PathogensGeorgeNecoarăNo ratings yet
- JAPAN-Flag-Standard Medical Chest MAR 2018 (Req)Document10 pagesJAPAN-Flag-Standard Medical Chest MAR 2018 (Req)shishir kumarNo ratings yet
- List of Firms Having Who (Own)Document1 pageList of Firms Having Who (Own)Ksusha ChernobrovaNo ratings yet
- Chronic Low Back Pain Good Clinical Practice GCPDocument341 pagesChronic Low Back Pain Good Clinical Practice GCPTru ManNo ratings yet
- Principles of Tooth PreparationsDocument14 pagesPrinciples of Tooth PreparationsMarrion Jules Sequitin MendozaNo ratings yet
- Ecg Quick Guide PDFDocument7 pagesEcg Quick Guide PDFansarijavedNo ratings yet
- September 15, 2016Document20 pagesSeptember 15, 2016CassieNo ratings yet