Professional Documents
Culture Documents
Premature Rupture of Membranes
Uploaded by
Mae SimborioOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Premature Rupture of Membranes
Uploaded by
Mae SimborioCopyright:
Available Formats
Premature Rupture of Membranes (PROM)
Definition Premature rupture of membranes (PROM) is an event that occurs during pregnancy when the sac containing the developing baby (fetus) and the amniotic fluid bursts or develops a hole prior to the start of labor. During pregnancy, the unborn baby (fetus) is surrounded and cushioned by a liquid called amniotic fluid. This fluid, along with the fetus and the placenta, is enclosed within a sac called the amniotic membrane. The amniotic fluid is important for several reasons. It cushions and protects the fetus, allowing the fetus to move freely. The amniotic fluid also allows the umbilical cord to float, preventing it from being compressed and cutting off the fetuss supply of oxygen and nutrients. The amniotic membrane contains the amniotic fluid and protects the fetal environment from the outside world. This barrier protects the fetus from organisms (like bacteria or viruses) that could travel up the vagina and potentially cause infection. Although the fetus is almost always mature at between 36-40 weeks and can be born without complication, a normal pregnancy lasts an average of 40 weeks. At the end of 40 weeks, the pregnancy is referred to as being term. At term, labor usually begins. During labor, the muscles of the uterus contract repeatedly. This allows the cervix to begin to grow thinner (called effacement) and more open (dilatation). Eventually, the cervix will become completely effaced and dilated. In the most common sequence of events (about 90% of all deliveries), the amniotic membrane breaks (ruptures) around this time. The baby then leaves the uterus and enters the birth canal. Ultimately, the baby will be delivered out of the mothers vagina. In the 30 minutes after the birth of the baby, the placenta should separate from the wall of the uterus and be delivered out of the vagina. Sometimes the membranes burst before the start of labor, and this is called premature rupture of membranes (PROM). There are two types of PROM. One occurs at a point in pregnancy before normal labor and delivery should take place. This is called preterm PROM. The other type of PROM occurs at 36-40 weeks of pregnancy. PROM occurs in about 10% of all pregnancies. Only about 20% of these cases are preterm PROM. Preterm PROM is responsible for about 34% of all premature births.
Causes The causes of PROM have not been clearly identified. Some risk factors include smoking, multiple pregnancies (twins, triplets, etc.), and excess amniotic fluid (polyhydramnios). Certain procedures carry an increased risk of PROM, including amniocentesis (a diagnostic test involving extraction and examination of amniotic fluid) and cervical cerclage (a procedure in which the uterus is sewn shut to avoid premature labor). A condition called placental abruption is also associated with PROM, although it is not known which condition occurs first. In some cases of preterm PROM, it is believed that bacterial infection of the amniotic membrane causes it to weaken and then break. However, most cases of PROM and infection occur in the opposite order, with PROM occurring first followed by an infection. Pathophysiology Numerous risk factors are associated with preterm PROM. Black patients are at increased risk of preterm PROM compared with white patients. Other patients at higher risk include those who have lower socioeconomic status, are smokers, have a history of sexually transmitted infections, have had a previous preterm delivery, have vaginal bleeding, or have uterine distension (e.g., polyhydramnios, multifetal pregnancy). Procedures that may result in preterm PROM include cerclage and amniocentesis. There appears to be no single etiology of preterm PROM. Choriodecidual infection or inflammation may cause preterm PROM. A decrease in the collagen content of the membranes has been suggested to predispose patients to preterm PROM. It is likely that multiple factors predispose certain patients to preterm PROM. Clinical Manifestation The main symptom of PROM is fluid leaking from the vagina. It may be a sudden, large gush of fluid, or it may be a slow, constant trickle of fluid. The complications that may follow PROM include premature labor and delivery of the fetus, infections of the mother and/or the fetus, and compression of the umbilical cord (leading to oxygen deprivation in the fetus). Labor almost always follows PROM, although the delay between PROM and the onset of labor varies. When PROM occurs at term, labor almost always begins within 24 hours. Earlier in pregnancy, labor can be delayed up to a week or more after PROM. The chance of infection increases as the time between PROM and labor increases. While this may cause doctors to encourage labor in the patient who has reached term, the risk of complications in a premature infant may cause doctors to try delaying labor and delivery in the case of preterm PROM. The types of infections that can complicate PROM include amnionitis and endometritis. Amnionitis is an infection of the amniotic membrane. Endometritis is an infection of the innermost lining of the uterus. Amnionitis occurs in 0.5-1% of all pregnancies. In the case of PROM at term, amnionitis complicates about 3-15% of pregnancies. About 15-
23% of all cases of preterm PROM will be complicated by amnionitis. The presence of amnionitis puts the fetus at great risk of developing an overwhelming infection (sepsis) circulating throughout its bloodstream. Preterm babies are the most susceptible to this life-threatening infection. One type of bacteria responsible for overwhelming infections in newborn babies is called group B streptococci. Diagnostic Test Depending on the amount of amniotic fluid leaking from the vagina, diagnosing PROM may be easy. Some doctors note that amniotic fluid has a very characteristic musty smell. A pelvic exam using a sterile medical instrument (speculum) may reveal a trickle of amniotic fluid leaving the cervix, or a pool of amniotic fluid collected behind the cervix. One of two easy tests can be performed to confirm that the liquid is amniotic fluid. A drop of the fluid can be placed on nitrazine paper. Nitrazine paper is made so that it turns from yellowish green to dark blue when it comes in contact with amniotic fluid. Another test involves smearing a little of the fluid on a slide, allowing it to dry, and then viewing it under a microscope. When viewed under the microscope, dried amniotic fluid will be easy to identify because it will look feathery like a fern. Once PROM has been diagnosed, efforts are made to accurately determine the age of the fetus and the maturity of its lungs. Premature babies are at great risk if they have immature lungs. These evaluations can be made using amniocentesis and ultrasound measurements of the fetus size. Amniocentesis also allows the practitioner to check for infection. Other indications of infection include a fever in the mother, increased heart rate of the mother and/or the fetus, high white blood cell count in the mother, foul smelling or pus-filled discharge from the vagina, and a tender uterus. Medical Management Treatment of PROM depends on the stage of the patients pregnancy. In PROM occurring at term, the mother and baby will be watched closely for the first 24 hours to see if labor will begin naturally. If no labor begins after 24 hours, most doctors will use medications to start labor. This is called inducing labor. Labor is induced to avoid a prolonged gap between PROM and delivery because of the increased risk of infection. Preterm PROM presents more difficult treatment decisions. The younger the fetus, the more likely it may die or suffer serious permanent damage if delivered prematurely. Yet the risk of infection to the mother and/or the fetus increases as the length of time from PROM to delivery increases. Depending on the age of the fetus and signs of infection, the doctor must decide either to try to prevent labor and delivery until the fetus is more mature, or to induce labor and prepare to treat the complications of prematurity. However, the baby will need to be delivered to avoid serious risks to both it and the mother if infection is present, regardless of the risks of prematurity. Medications
CORTICOSTEROIDS Corticosteroids decrease perinatal morbidity and mortality after preterm PROM. A recent meta-analysis found that corticosteroid administration after preterm PROM, versus no administration, reduced the risk of respiratory distress syndrome (20 versus 35.4 percent), intraventricular hemorrhage (7.5 versus 15.9 percent), and necrotizing enterocolitis (0.8 versus 4.6 percent) without an increase in the risk of maternal or neonatal infection. Because corticosteroids are effective at decreasing perinatal morbidity and mortality, all physicians caring for pregnant women should understand the dosing and indications for corticosteroid administration during pregnancy. The most widely used and recommended regimens include intramuscular betamethasone (Celestone) 12 mg every 24 hours for two days, or intramuscular dexamethasone (Decadron) 6 mg every 12 hours for two days. The National Institutes of Health recommends administration of corticosteroids before 30 to 32 weeks gestation, assuming fetal viability and no evidence of intra-amniotic infection. Use of corticosteroids between 32 and 34 weeks is controversial. Administration of corticosteroids after 34 weeks gestation is not recommended unless there is evidence of fetal lung immaturity by amniocentesis. Multiple courses are not recommended because studies have shown that two or more courses can result in decreased infant birth weight, head circumference, and body length. ANTIBIOTICS Giving antibiotics to patients with preterm PROM can reduce neonatal infections and prolong the latent period. A meta-analysis showed that patients receiving antibiotics after preterm PROM, compared with those not receiving antibiotics experienced reduced postpartum endometritis, chorioamnionitis, neonatal sepsis, neonatal pneumonia, and intraventricular hemorrhage. Another meta-analysis found a decrease in neonatal intraventricular hemorrhage and sepsis. A number of antibiotic regimens are advocated for use after preterm PROM. The regimen studied by the National Institute of Child Health and Human Development trial uses an intravenous combination of 2 grams of ampicillin and 250 mg of erythromycin every six hours for 48 hours, followed by 250 mg of amoxicillin and 333 mg of erythromycin every eight hours for five days. Women given this combination were more likely to stay pregnant for three weeks despite discontinuation of the antibiotics after seven days. It is advisable to administer appropriate antibiotics for intrapartum group B streptococcus prophylaxis to women who are carriers, even if these patients have previously received a course of antibiotics after preterm PROM. TOCOLYTIC THERAPY Limited data are available to help determine whether tocolytic therapy is indicated after preterm PROM. As described above, corticosteroids and antibiotics are beneficial when administered to patients with preterm PROM, but no studies of these therapies combined with tocolysis are available. Tocolytic therapy may prolong the latent period for a short time but do not appear to improve neonatal outcomes. In the absence of data, it is not unreasonable to administer a short course of tocolysis after preterm PROM to allow
initiation of antibiotics, corticosteroid administration, and maternal transport, although this is controversial. Long-term tocolytic therapy in patients with PROM is not recommended; consideration of this should await further research. Management Based on Gestational Age 34 TO 36 WEEKS When preterm PROM occurs at 34 to 36 weeks ges-tation, physicians should avoid the urge to prolong pregnancy. Studies have shown that labor induction clearly is beneficial at or after 34 weeks gestation. One study showed that conservative management between 34 and 36 weeks gestational age resulted in an increased risk of chorioamnionitis and a lower average umbilical cord pH. Another study of 430 women with preterm PROM revealed that there was no improvement in major or minor neonatal morbidity after 34 weeks gestation. Although corticosteroids are not indicated after 34 weeks gestation, physicians should prescribe appropriate antibiotics for group B streptococcus prophylaxis and should consider maternal transport to a facility skilled in caring for premature neonates, if possible. Preterm PROM is not a contraindication to vaginal delivery. 32 TO 33 WEEKS For patients with preterm PROM at 32 or 33 weeks gestation with documented pulmonary maturity, induction of labor and transportation to a facility that can perform amniocentesis and care for premature neonates should be considered. Prolonging pregnancy after documentation of pulmonary maturity unnecessarily increases the likelihood of maternal amnionitis, umbilical cord compression, prolonged hospitalization, and neonatal infection. There are few data to guide the care of patients without documented pulmonary maturity. No studies are available comparing delivery with expectant management when patients receive evidence-based therapies such as corticosteroids and antibiotics. Physicians must balance the risk of respiratory distress syndrome and other sequelae of premature delivery with the risks of pregnancy prolongation, such as neonatal sepsis and cord accidents. Physicians should administer a course of corticosteroids and antibiotics to patients without documented fetal lung maturity and consider delivery 48 hours later or perform a careful assessment of fetal well-being, observe for intra-amniotic infection, and deliver at 34 weeks, as described above. Consultation with a neonatologist and physician experienced in the management of preterm PROM may be beneficial. Patients with amnionitis require broad-spectrum antibiotic therapy, and all patients should receive appropriate intrapartum group B streptococcus prophylaxis, if indicated.
24 TO 31 WEEKS Delivery before 32 weeks gestation may lead to severe neonatal morbidity and mortality. In the absence of intra-amniotic infection, the physician should attempt to prolong the pregnancy until 34 weeks gestation. Physicians should advise patients and family members that, despite these efforts, many patients deliver within one week of preterm PROM. Contraindications to conservative therapy include chorioamnionitis, abruptio placentae, and nonreassuring fetal testing. Physicians should administer a course of corticosteroids and antibiotics and perform an assessment of fetal well-being by fetal monitoring or ultrasonography. After transport to a facility able to care for patients with preterm PROM before 32 weeks gestation, patients should receive daily (or continuous, if indicated) fetal monitoring for contractions and fetal well-being. Umbilical cord compression is common (32 to 76 percent)7 with preterm PROM before 32 weeks gestation; therefore, at least daily fetal monitoring is indicated. In addition, the physician should observe closely for fetal or maternal tachycardia, oral temperature exceeding 100.4F (38C), regular contractions, uterine tenderness, or leukocytosis, which are possible indicators of amnionitis. Corticosteroid administration may lead to an elevated leukocyte count if given within five to seven days of PROM. Evidence suggests that prolonged latency may increase the risk of intra-amniotic infection. A retrospective analysis of 134 women with preterm PROM at 24 to 32 weeks gestation who received steroids and antibiotics found a nonsignificant trend toward intrauterine inflammation in patients with a latency period longer than one week. Delivery is necessary for patients with evidence of amnionitis. If the diagnosis of an intrauterine infection is suspected but not established, amniocentesis can be performed to check for a decreased glucose level or a positive Gram stain and differential count can be performed. For patients who reach 32 to 33 weeks gestation, amniocentesis for fetal lung maturity and delivery after documentation of pulmonary maturity, evidence of intraamniotic infection, or at 34 weeks gestation should be considered. BEFORE 24 WEEKS The majority of patients will deliver within one week when preterm PROM occurs before 24 weeks gestation, with an average latency period of six days. Many infants who are delivered after previable rupture of the fetal membranes suffer from numerous long-term problems including chronic lung disease, developmental and neurologic abnormalities, hydrocephalus, and cerebral palsy. Previable rupture of membranes also can lead to Potters syndrome, which results in pressure deformities of the limbs and face and pulmonary hypoplasia. The incidence of this syndrome is related to the gestational age at which rupture occurs and to the level of oligohydramnios. Fifty percent of infants with rupture at 19 weeks gestation or earlier are affected by Potters syndrome, whereas 25 percent born at 22 weeks and 10 percent after 26 weeks gestation are affected. Patients should be counseled about the outcomes and benefits and risks of expectant management, which may not continue long enough to deliver a baby that will survive normally.
Physicians caring for patients with preterm PROM before viability may wish to obtain consultation with a perinatologist or neonatologist. Such patients, if they are stable, may benefit from transport to a tertiary facility. Home management of patients with preterm PROM is controversial. A study of patients with preterm PROM randomized to home versus hospital management revealed that only 18 percent of patients met criteria for safe home management. Bed rest at home before viability (i.e., approximately 24 weeks gestation) may be acceptable for patients without evidence of infection or active labor, although they must receive precise education about symptoms of infection and preterm labor, and physicians should consider consultation with experts familiar with home management of preterm PROM. Consider readmission to the hospital for these patients after 24 weeks gestation to allow for close fetal and maternal monitoring. Prognosis The prognosis in PROM varies. It depends in large part on the maturity of the fetus and the development of infection. Prevention The only controllable factor associated with PROM is smoking. Cigarette smoking should always be discontinued during a pregnancy. Reference Davidson, Susan. Diseases Causes & Diagnosis Current Therapy Nursing Management Patient Education (Educational Publishing House. 1990) Kumar. Robbins & Cotran Pathologic Basis of Disease (Elsevier Saunders Inc. 7th edition. 2005) Huether. Understanding Pathophysiology (Mosby, Inc. 2nd edition. 2000)
You might also like
- Premature Rupture of MembranesDocument33 pagesPremature Rupture of MembranesSarang Lee100% (1)
- The Pathophysiology of PPROMDocument2 pagesThe Pathophysiology of PPROMNano KaNo ratings yet
- Gestational Diabetes Case PresentationDocument102 pagesGestational Diabetes Case Presentationkitten garciaNo ratings yet
- Understanding Ectopic Pregnancy: Causes, Symptoms and TreatmentDocument11 pagesUnderstanding Ectopic Pregnancy: Causes, Symptoms and TreatmentPrincess BalloNo ratings yet
- Abruptio PlacentaDocument5 pagesAbruptio PlacentaJuan Carlo Z. SolidumNo ratings yet
- Fetal DistressDocument111 pagesFetal DistressSakariye SuleimanNo ratings yet
- Diagnosis of PregnancyDocument26 pagesDiagnosis of PregnancyMounikaNo ratings yet
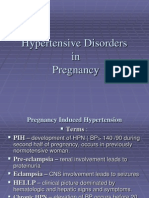
- Pregnancy Induced HypertensionDocument3 pagesPregnancy Induced HypertensionDiane Kate Tobias Magno100% (1)
- Thyroid Disease in PregnancyDocument17 pagesThyroid Disease in Pregnancydaniel100% (1)
- Obgyn Anemia in Pregnancy For UG ClassDocument35 pagesObgyn Anemia in Pregnancy For UG ClassimranNo ratings yet
- Multifetal Pregnancy: Amr Nadim, MDDocument36 pagesMultifetal Pregnancy: Amr Nadim, MDsharenNo ratings yet
- Management of Pregnancy Related BleedingDocument75 pagesManagement of Pregnancy Related BleedingChuah Wei Hong100% (1)
- Premature Rupture of MembranDocument21 pagesPremature Rupture of MembranMarfu'ah HariyaniNo ratings yet
- Ectopic PregnancyDocument26 pagesEctopic PregnancysandhyakrishnanNo ratings yet
- Antepartum HaemorrhageDocument57 pagesAntepartum HaemorrhageLady350z100% (3)
- 001hypertensive Disorders in Pregnancy PDFDocument23 pages001hypertensive Disorders in Pregnancy PDFRosechelle Bas SamsonNo ratings yet
- Hypertension in PregnancyDocument68 pagesHypertension in PregnancyAbdul MoizNo ratings yet
- PROM Care PlanDocument2 pagesPROM Care PlanMariagmzNo ratings yet
- CVS Procedure ExplainedDocument5 pagesCVS Procedure ExplainedpriyankaNo ratings yet
- Obstetric Nursing Care PlanDocument14 pagesObstetric Nursing Care Planlilchristina0178% (9)
- Hypertension in Pregnancy CompiledDocument67 pagesHypertension in Pregnancy CompiledRaiza Love Caparas-PablicoNo ratings yet
- Neonatal SepsisDocument44 pagesNeonatal SepsisIsabel Barredo Del MundoNo ratings yet
- Jaundice in Pregnancy: Causes, Types, and ManagementDocument32 pagesJaundice in Pregnancy: Causes, Types, and ManagementManoj Sankaranarayana100% (2)
- Vulvitis, Vaginitis, Bartholin's Cyst and CervicitisDocument56 pagesVulvitis, Vaginitis, Bartholin's Cyst and CervicitisSushma Thakuri100% (1)
- Ectopic Pregnancy - CSDocument14 pagesEctopic Pregnancy - CSMASII100% (1)
- Malpresentation and Malposition - PostmaturityDocument29 pagesMalpresentation and Malposition - PostmaturityNishaThakuriNo ratings yet
- Post Partum HemorrhageDocument12 pagesPost Partum HemorrhageCristinaCaprosNo ratings yet
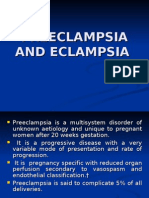
- Preeclampsia and EclampsiaDocument23 pagesPreeclampsia and Eclampsiaapi-3705046100% (6)
- Diabetes in PregnancyDocument88 pagesDiabetes in PregnancyKathleenZunigaNo ratings yet
- Ectopic PregnancyDocument3 pagesEctopic PregnancyMary Anne Yap100% (1)
- CPD, Dystocia, Fetal Distress OutputDocument8 pagesCPD, Dystocia, Fetal Distress OutputJohn Dave AbranNo ratings yet
- Excess Amniotic Fluid Causes and DiagnosisDocument2 pagesExcess Amniotic Fluid Causes and DiagnosisAde Yonata100% (1)
- Hypertensive Disorders in PregnancyDocument81 pagesHypertensive Disorders in PregnancyarunshreerajendranNo ratings yet
- Antepartum HaemorrhageDocument48 pagesAntepartum HaemorrhageDuncan JacksonNo ratings yet
- Fetal DistressDocument33 pagesFetal DistressYara H QaisiNo ratings yet
- Caring for Mothers with Pregnancy-Induced HypertensionDocument4 pagesCaring for Mothers with Pregnancy-Induced HypertensionCatherine PradoNo ratings yet
- Bleeding in Early PregnancyDocument39 pagesBleeding in Early PregnancyIdiAmadouNo ratings yet
- Gestational Diabetes: Dr. Oyeyiola Oyebode Registrar Obstetrics and Gynaecology Ola Catholic Hospital, Oluyoro IbadanDocument40 pagesGestational Diabetes: Dr. Oyeyiola Oyebode Registrar Obstetrics and Gynaecology Ola Catholic Hospital, Oluyoro Ibadanoyebode oyeyiolaNo ratings yet
- Immediate Physiological Changes in New BornDocument7 pagesImmediate Physiological Changes in New BornLahunWanniangNo ratings yet
- Gestational Diabetes Screening Case StudiesDocument50 pagesGestational Diabetes Screening Case Studiesdiabetes asia100% (1)
- Placenta PreviaDocument11 pagesPlacenta PreviaHomerNo ratings yet
- Preeclampsia and EclampsiaDocument24 pagesPreeclampsia and Eclampsialeeseol20yahoo.comNo ratings yet
- Case Study On Preterm LaborDocument81 pagesCase Study On Preterm Laborkarl montanoNo ratings yet
- PartographDocument33 pagesPartographKathrynne Mendoza100% (1)
- Post Abortion CareDocument35 pagesPost Abortion CareNatukunda DianahNo ratings yet
- Nursing Seminar on Management of Third and Fourth Stages of LaborDocument39 pagesNursing Seminar on Management of Third and Fourth Stages of LaborSravanthi Karingula100% (1)
- Antenatal Assessment of Foetal Wellbeing.Document30 pagesAntenatal Assessment of Foetal Wellbeing.Kavya S MohanNo ratings yet
- Lesson Plan on Causes and Management of Intrauterine Fetal DeathDocument21 pagesLesson Plan on Causes and Management of Intrauterine Fetal DeathBupe LwitaNo ratings yet
- Menstrual disorders: causes, symptoms and treatmentsDocument47 pagesMenstrual disorders: causes, symptoms and treatmentsKiranNo ratings yet
- Rh Factor and Pregnancy: Understanding Rh IncompatibilityDocument22 pagesRh Factor and Pregnancy: Understanding Rh IncompatibilityDrPreeti Thakur ChouhanNo ratings yet
- Hypertensive Disorder in PregnancyDocument56 pagesHypertensive Disorder in PregnancyESCA GabrielNo ratings yet
- Assisted Vaginal DeliveryDocument26 pagesAssisted Vaginal Deliveryapi-3705046100% (5)
- Premature Rupture of MembraneDocument6 pagesPremature Rupture of MembraneSabna AjasNo ratings yet
- Preterm LaborDocument9 pagesPreterm LaborMelonie VINo ratings yet
- Case DR Priolapse - Preterm, Iufd, PromnDocument15 pagesCase DR Priolapse - Preterm, Iufd, PromnAL-Neil AntonioNo ratings yet
- PROM: Premature Rupture of MembranesDocument41 pagesPROM: Premature Rupture of MembranesWidya Rahayu33% (3)
- Premature Rupture of Membrane (PROM) : Submitted By: Joel Antolin Bsn4C Group 10Document3 pagesPremature Rupture of Membrane (PROM) : Submitted By: Joel Antolin Bsn4C Group 10Joel AntolinNo ratings yet
- Ruptured Uterus: Causes, Symptoms and TreatmentDocument3 pagesRuptured Uterus: Causes, Symptoms and TreatmentJB JuneNo ratings yet
- Premature Rupture of MembranesDocument8 pagesPremature Rupture of MembranesGladie Ann Dela RosaNo ratings yet
- Premature Rupture of MembranesDocument5 pagesPremature Rupture of MembranesJoselyn San MiguelNo ratings yet
- 03 Biochemistry PLE 2019 RatioDocument72 pages03 Biochemistry PLE 2019 RatioMae SimborioNo ratings yet
- AMBOSS Study Guide for PLE Exam PreparationDocument77 pagesAMBOSS Study Guide for PLE Exam PreparationFhai Escio100% (1)
- Gold 2019 Pocket GuideDocument49 pagesGold 2019 Pocket GuideJhonnathan RodriguezNo ratings yet
- Ethics in SirDocument4 pagesEthics in SirMae SimborioNo ratings yet
- Philippine CPG-2013-uti in Adults-Part1 PDFDocument82 pagesPhilippine CPG-2013-uti in Adults-Part1 PDFVirginia AbalosNo ratings yet
- NMAT Practice Set Part 1 & Part 2 With Answer KeyDocument64 pagesNMAT Practice Set Part 1 & Part 2 With Answer KeyLucid LynxNo ratings yet
- Promise of TomorrowDocument5 pagesPromise of TomorrowMae SimborioNo ratings yet
- Pediatric Caseheet PDFDocument23 pagesPediatric Caseheet PDFAparna DeviNo ratings yet
- Effectiveness of Planned Teaching Programme On The Knowledge of Endotracheal Suctioning Among Staff Nurses Working in IcuDocument6 pagesEffectiveness of Planned Teaching Programme On The Knowledge of Endotracheal Suctioning Among Staff Nurses Working in IcuRizwan KhanNo ratings yet
- TCM Cases - PainDocument671 pagesTCM Cases - PainGeander G. Bacheti100% (5)
- The Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaDocument8 pagesThe Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaCristian Manuel Goicochea ChuqueNo ratings yet
- The Clinical Toxicology of Sulfur Mustard: Review ArticleDocument18 pagesThe Clinical Toxicology of Sulfur Mustard: Review ArticleGiany GausNo ratings yet
- Tuberculosis and Typhoid: Deadly Diseases in the PhilippinesDocument37 pagesTuberculosis and Typhoid: Deadly Diseases in the PhilippinesAriel FuentespinaNo ratings yet
- CIPHIDocument256 pagesCIPHIसदानंद देशपांडेNo ratings yet
- Correlation of Sound and Colour - Paul Foster CaseDocument30 pagesCorrelation of Sound and Colour - Paul Foster Casesrk777100% (7)
- The SCARE Statement Consensus-Based Surgical Case ReportDocument7 pagesThe SCARE Statement Consensus-Based Surgical Case ReportIhsan KNo ratings yet
- 30th Report Bogus Unregistered Deregistered HealthPract-1Document106 pages30th Report Bogus Unregistered Deregistered HealthPract-1Paul GallagherNo ratings yet
- Who Unicri Cocaine Project Study 1995Document75 pagesWho Unicri Cocaine Project Study 1995speedheartNo ratings yet
- VMC Customer Service Complaint and Letter of DemandDocument3 pagesVMC Customer Service Complaint and Letter of DemandJames Alan BushNo ratings yet
- Blessing IwezueDocument3 pagesBlessing Iwezueanon-792990100% (2)
- Tfios Mediastudyguide v4Document7 pagesTfios Mediastudyguide v4api-308995770No ratings yet
- OB Meds WorksheetDocument18 pagesOB Meds WorksheetrickyandsheenaNo ratings yet
- Wound Management ProcedureDocument51 pagesWound Management ProcedureSisca Dwi AgustinaNo ratings yet
- ECTDocument22 pagesECTRubz Bulquerin0% (1)
- Miocarditis Por Clozapina Ronaldson2017 Revisión SistematicaDocument19 pagesMiocarditis Por Clozapina Ronaldson2017 Revisión SistematicaAlejandro PiscitelliNo ratings yet
- Health Teaching Plan HTNDocument3 pagesHealth Teaching Plan HTNCarpz Darpz88% (8)
- Lower Limb ProstheticsDocument28 pagesLower Limb ProstheticsSomu VictorNo ratings yet
- WeeFIM Score Sheet (MS Word)Document4 pagesWeeFIM Score Sheet (MS Word)Siti Maryam Rosyidah0% (2)
- Breast, EndocrineDocument247 pagesBreast, EndocrineRajan VaithianathanNo ratings yet
- Patient Safety and TechnologyDocument5 pagesPatient Safety and TechnologyAditya Toga100% (1)
- MSA Testing Reveals Body's Energetic HealthDocument4 pagesMSA Testing Reveals Body's Energetic HealthDenise MathreNo ratings yet
- 10 0000@Www Quintpub Com@ejed@18638Document23 pages10 0000@Www Quintpub Com@ejed@18638Víctor Rodríguez67% (3)
- A Comparison of Muscle Strength and Flexibility Between The Preferred and Non Preferred Leg in English Soccer PlayersDocument10 pagesA Comparison of Muscle Strength and Flexibility Between The Preferred and Non Preferred Leg in English Soccer PlayersMalikiNo ratings yet
- Management of Intravascular Devices To Prevent Infection: LinicalDocument5 pagesManagement of Intravascular Devices To Prevent Infection: LinicalCristianMedranoVargasNo ratings yet
- ACCIDENT REPORTING AND INVESTIGATION PROCEDUREDocument23 pagesACCIDENT REPORTING AND INVESTIGATION PROCEDUREkirandevi1981No ratings yet
- Acterial Iseases: Prepared By: Dr. Rea CorpuzDocument63 pagesActerial Iseases: Prepared By: Dr. Rea CorpuzMedecine Dentaire100% (2)
- Levorphanol - The Forgotten Opioid PDFDocument6 pagesLevorphanol - The Forgotten Opioid PDFfchem11No ratings yet