Professional Documents
Culture Documents
Wound Scale
Uploaded by
Humam SyriaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wound Scale
Uploaded by
Humam SyriaCopyright:
Available Formats
ACADEMIC EMERGENCY MEDICINE
June 1998, Volume 5, Number 6
683
DUCATION AND PRACTIC
An Assessment of Clinical Wound Evaluation Scales
JAMES QUINN, MD, GEORGE WELLS, MD V. A.
Abstract. Objective: To compare 2 clinical wound scales and to determine a minimal clinically important difference (MCID) on the visual analog cosmesis scale. Methods: Using data from 2 previously published clinical trials, 91 lacerations and 43 surgical incisions were assessed on the 2 scales; a 100-mm visual analog scale (VAS) (0 = worst possible scar, 100 = best possible scar) and a wound evaluation scale (WES) assessing 6 clinical variables (a score of 6 is considered optimal, while a score of 5 5 suboptimal). All wound assessments on the VAS were done by 2 cosmetic surgeons who rated photographs on 2 occasions. A cohort of wounds on the WES were assessed by a second observer. The difference of the mean optimal and suboptimal VAS scores for each study was used to determine a MCID on the VAS scale. Results:
The VAS scale yielded intraobserver agreements of 0.93 and 0.87(95% CI: 0.89-0.96 and 0.78-0.93)and interobserver agreements of 0.50 and 0.71 (95% CI: 0.32-0.65 and 0.52-0.84) for lacerations and incisions, respectively. Kappa coefficient measuring agreement on the WES was 0.79 (95% CI: 0.57-1.0). The mean (?SD) VAS scores of optimal wounds were 72 5 12 mm and 65 5 20 mm, while the mean scores of suboptimal wounds were 57 ? 17 mm and 50 2 23 mm for lacerations and incisions, respectively. Conclusions: A n MCID on the VAS cosmesis scale is 15 mm. Studies should be designed to have a sample size and power to detect this difference. Key words: wounds; lacerations; tissue adhesives; sutures; staples; infection; cosmetic appearance. ACADEMIC EMERGENCY MEDICINE 1998;5~583-586
ALJD, reliable outcome measures that can assess important clinical differences are essential tools for clinical trials.' Investigators have been interested in measuring important but subjective outcomes for some time. Outcome measures have been developed to evaluate subjective out~.~ comes such as quality of life, and ~ a i n .Recently there has been interest in clinical wound healing, and several scales have been developed to measure the cosmetic outcomes of healed lacerations and incisions.4~6 visual analog cosmesis scale, like the A visual analog pain scale, has become a desirable method of clinical evaluation because of its continuous nature, ability to measure small differences, reproducible results, and ease of use.
The difficulty with visual analog scales (VASs) is that although they can measure small changes and statistical differences between groups, the clinical relevance of the numerical results and important clinical differences on these scales are not i n t ~ i t i v e .To. ~ ~ improve the VAS scale as an outcome measure, the determination of minimal clinical important differences (MCIDs) is essential to their proper use. In addition, they should be combined with descriptive scales that can better define the numerical results of the VAS. To date, investigators have determined this MCID on VAS pain scales' and the VAS cosmesis scale has been combined and contrasted with descriptive scale^.^ This is the first study t o derive an MCID for the VAS cosmesis scale.
From the Department of Surgery, Division of Emergency Medicine CJVQ), University of Michigan, Ann Arbor, MI; and the Loeb Research Institute, Clinical Epidemiology Unit (GAW), University of Ottawa, Ontario, Canada. Received: August 26, 1997; revision received: November 17, 1997; accepted: December 14, 1997; updated: December 28, 1997. Presented at the SAEM annual meeting, Washington, DC, May 1997. The studies upon which this secondary analysis was performed were sponsored by Closure Medical Corporation. Address for correspondence and reprints: James V. Quinn, MD, Division of Emergency Medicine, The University of Michigan, TC B1354, Box 0303, 1500 East Medical Center Drive, Ann Arbor, MI 48109-0303. Fax: 313-936-9414; E-mail: jaquinn@ umich.edu
METHODS
Studg Design. We performed a retrospective analysis and comparison of 2 scales used to measure the cosmetic outcomes of healed lacerations and incisions of 2 previously published studies. Approval t o analyze the data from published studies using these scales was granted from the institutional review board at the University of Michigan. Population and Settings. The data from 2 prospective trials on laceration treatment8 and surgi-
584
WOUND SCALES
Quinn, Wells
CLINICAL WOUND EVALUATION SCALES
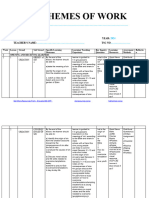
TABLE 1. Wound Evaluation Scale*
1. Stepoff borders (0for yes, 1 for no) 2 Contour irregularity-puckering . 3. Scar width-greater than 2 mm 4. Edge inversion-sinking, curling 5. Inflammation-redness, discharge 6. Overall cosmesis ( 0 = poor, 1 = acceptable)
*6/6 = optimal wound healing.
cyanoacrylate tissue adhesive. All wounds in this study had identical closures of the deep layer prior to skin closure. The average length of the incisions was 9.4 cm. The same 2 methods of wound evaluation (WES and VAS) were used, but were performed at 1 month rather than 3 months for the laceration study.
cal incisions treatment were used. The trials cornpared traditional suturing with the use of a new topical tissue adhesive. The laceration study included all facial lacerations as well as certain selected extremity and torso lacerations. The surgical incision study compared incisions from a wide variety of head and neck incisions.
Measurements. In the laceration study, patients were prospectively randomized to have the skin of their lacerations closed with either 5-0 monofilament suture or topical tissue adhesive. The average length of laceration in the study was 2.5 cm, and 12.5% of the lacerations required deep sutures. At 3 months the patients had a wound assessment done on a previously validated wound evaluation scale (WESh4 The score was assigned by a research nurse aware of the method of closure and validated by a second nurse blinded to the method of closure and unaware of previous wound scores. Nurses and physicians have been shown to .~ use the WES r e l i a b l ~The wound score addresses 6 clinical variables: absence of stepoff, contour irregularities, wound margin separation >2 mm, edge inversion, excessive distortion, and overall cosmetic appearance. Each of these categories is graded on a O-or-l-point scale. A total cosmetic score is derived by the addition of the scores of the 6 categorical variables. A score of 6 is considered optimal, while a score of 5 5 suboptimal (Table 1). At the same time the WES was determined, the patients had photographs of their healing wounds taken. The photographs were taken by the research assistant in a standard fashion using a 1:3 macro setting with a ring flash and using 100 Ektachrome slide film.1 These photographs were rated for cosmesis on a previously validated cosmesis scale. This VAS for cosmesis has been demonstrated to be reliable and valid.s The VAS cosmesis scale is a 100-mm line with worst scar at the right end (0 mm) and best scar at the left end (100 mm) (Figs. 1 and 2). The photographs were rated on 2 occasions by 2 cosmetic surgeons blinded to which method was used to close the wounds. The surgical incision study was a prospective, nonrandomized comparison study comparing the skin closures of various head and neck incisions with either 4-0 nylon subcuticular suture or octyl-
Data Analysis. The mean 2 SD of the VAS cosmesis scores for optimal and suboptimal wounds was determined for each study The MCID on the VAS was considered to be the distance between an average optimal Score and an average suboptimal score. Observer agreement of the cosmetic SUrgeons on their VAS scores was determined using the intraclass correlation coefficient. Agreement on the WES was determined using the kappa (K) coefficient. Confidence interval estimates for the agreement coefficients were calculated.
RESULTS
There were 91 patients in the laceration group, 67 with optimal scores and 24 with suboptimal scores. In the incision study, there were 43 patients, 23 with optimal and 20 with suboptimal wound scores. The mean difference in VAS cosmesis scores in both the laceration and incision studies was 15 mm (Figs. 1and 2). The VAS scale yielded intraobserver agreements of 0.93 and 0.87 (95% CI: 0.89-0.96 and 0.78-0.93) and interobserver agreements of 0.50 and 0.71 (95% CI: 0.32-0.65 and 0.52-0.84) for lacerations and incisions, respectively. The K coefficient measuring agreement on the WES was 0.79 (95% CI: 0.57-1.0).
DISCUSSION
Until recently most treatments for wounds were evaluated and reported as case series.ll Objective comparison of treatments with a randomized trial was impossible because of the lack of valid, reliable, and clinically important outcome measures that could be assessed in a blinded fashion. Valid reliable scales such as the VAS cosmesis scale and the WES now make it possible to do this. Any good outcome measure should have 5 properties: it should measure an important outcome of the intervention, it should be reliable (i.e., the results should be reproducible), it should be valid (i.e., be a true measure of the outcome), one should be able to measure or determine clinically important differences on the scale, and it should be easy to use and understand. Several years ago we chose cosmesis as our outcome measure for clinical wound evaluation. We determined that it was the most important outcome for patients by informally surveying 75 pa-
ACADEMIC EMERGENCY MEDICINE
June 1998, Volume 5, Number 6
585
tients and parents of children with lacerations. While outcomes such as pain and time were very important, final cosmetic outcome (80% of the time) was the most important outcome to this group of surveyed parents and patients with facial lacerations. When considering other parts of the body i t was still important (39% of the time), but time spent waiting was considered more important for these wounds (46%),while pain was third (15%) (unpublished data, 1991). Other important outcomes such as infection and dehiscence were considered, but using them as a primary outcome measure is difficult because they are relatively rare, and measuring them is problematic because many cannot agree on what truly is a n infection.12J3We also believe that important infections and dehiscences will manifest themselves as poor cosmetic outcomes. As noted above, a good outcome measure must be reliable, i.e., reproducible. We have shown that if a cosmetic surgeon likes the scar the first time it is shown to him or her, and then the scar is shown to the same surgeon again some time later when he or she is unaware of the previous result, he or she will give the scar a very similar score (intraobserver reliability or agreement). Having 2 cosmetic surgeons agreeing on the score of the wound (interobserver agreement) not only gives it a measure of reliability, but also gives it a measure of validity. Not surprisingly, agreement of a surgeon with his or her own previous scores tends to be stronger than agreement between surgeons, and in this study one measurement was only 0.5, which is the lower acceptable boundary for such agreement. However, when analyzing the incisions in this study, the interobserver ageement was 0.71, which was more consistent with previous studies where the interobserver agreement consistently ranges from 0.71 to 0.75.6J4.15 There is no criterion standard with which to measure and test the validity of the VAS cosmesis scale. For that reason we believe it is important to help define the scale with descriptive measures or outcomes that can help to define numerical values of the scale and improve its validity. In these 2 studies we chose to combine it with the WES, which assesses various clinical variables when determining an optimal vs a suboptimal scar. In the past we combined the VAS cosmesis scale with a descriptive scale that classified wounds into 3 categories: excellent, acceptable, and poor, based on clinical d e s ~ r i p t o r s The importance of this is il.~ lustrated in the following example. If one were told that the average VAS cosmesis score of a group of traumatic lacerations was 68 mm, he or she would really have no idea what that means. I t may be possible to compare them with another group, but was the score from this group actually good or bad?
By knowing that the average optimal score of all traumatic wounds was 72 mm, one can be fairly confident that the outcomes in that group are good. In another attempt to improve validity, we chose to use cosmetic surgeons to evaluate the scars, because they are the ones who deal with scars on a daily basis and make decisions regarding revision. Doing so gives the VAS cosmesis scale a measure of face validity.
LIMITATIONSAND FUTURE QUESTIONS
This study is limited by its retrospective analysis of data from 2 studies, which, aside from using the same outcome measures, were very different in design. The study on lacerations was a prospective, randomized trial of traumatic lacerations, on a variety of sites of the body closed by 10 different physicians, with a 3-month blinded cosmetic evaluation. The study on incisions was a nonrandomized, prospective comparison of surgical incisions treated by 2 surgeons (1sutured a n d 1 applied tissue adhesive) with a 1-month blinded cosmetic evaluation. To deal with this limitation we did not attempt to combine the data of these studies when doing our analysis. However, the fact that both scales are reliable and produce similar MCIDs despite vastly different clinical scenarios leads us to
worst scar
VAS Cosmesis Scale 100 rn Optimal best
Suboptimal
scar
Figure 1. Average optimal and suboptimal scores for the laceration study. VAS = visual analog scale.
VAS Cosmesis Scale
Optimal Suboptimal
100
worst scar
best scar
Fiaure 2. Average optimal and suboptimal scores for the
incision study. VAS = visual analog scale.
686
WOUND SCALES
Quinn,Wells
CLINICAL WOUND EVALUATION SCALES
believe that our conclusions can be generalized to most clinical settings. We also assumed that an important clinical difference corresponded t o the difference between an optimal and a suboptimal W S score. The assumption that a scar is clinically less desirable because it fails to score on all 6 clinical variables may be debated, although the majority of wounds score either a 4-516 (suboptimal) or 6/6 (optimal). Only the occasional wound scores less than 4/6. Finally, it can be argued that the satisfaction of patients with regard t o assessment of their own wounds is the most important outcome. Although we have considered the MCID that physicians are willing t o accept, we have not addressed the MCID that patients are willing to accept. Singer et al. have shown good concordance between physician and patient assessments of wounds.l6 However, using patients to assess their wounds has methodologic problems. It is impossible t o blind patients to the treatment of their wounds and when patients are not blinded, they are more likely t o bias their assessments to please the investigators (Hawthorne effect).17The VAS used by patients, unlike the VAS cosmesis scale, has not yet been validated as an outcome measure. Prospective, randomized trials using blinded validated outcome measures should be the design of choice for clinical wound studies, and future rigorously designed studies should similarly evaluate patient assessment of cosmesis.
RMerences
1 Streiner DL, Norman GR. Health Measurement Scales: A . Practical Guide to Their Development and Use, ed 1. New York Oxford University Press, 1991, pp 1-3, 8. 2. Huskisson EC. Visual analogue scales. In: Melzack R. Pain Measurement and Assessment, New York: Raven Press, 1983, pp 33-7. 3 Guyatt GH, Berman LB, Townsend M, et al. A measure for . quality of life in clinical trials for chronic lung disease. Thorax. 1987; 42:773-8. 4. Hollander JE,Singer AJ, Valentine S, m o d e HC Jr, Henry MC. Wound registry: development and validation. Ann Emerg Med. 1995; 25675-85. 8. Quinn JV,Drzewiecki AE,Stiell IG, Elmslie TJ. Appearance scales to measure the cosmetic outcomes of healed lacerations. Am J Emerg Med. 1995; 13:229-31. 6. Wells GA, Tugwell P, Kraag GR, et a . Minimum important l difference between patients with rheumatoid arthritis: the patient's perspective. J Rheumatol. 1993; 20:567-60. 7. Todd KH, Funk KG, Funk JP,Bonacci R. The clinical significance of reported changes in pain severity. Acad Emerg Med. 1995; 2:369-70. 8. Quinn J, Wells G, Sutcliffe T, et al. A randomized trial comparing octylcyanoacrylate tissue adhesive and sutures in the management of lacerations. JAMA. 1997; 277:1527-30. 9. Maw JL, Quinn JV,Wells GA, et al. A prospective comparison of octylcyanoacrylate tissue adhesive and sutures for the closure of head and neck incisions. J Otolaryngol. 1997; 26: 26-30. 1 . Storrow AB, Stack LB, Peterson P. An approach to emer0 gency department photography. Acad Emerg Med. 1994; 1: 454-62. 11. Watson DP. Use of cyanoacrylate tissue adhesive for closing facial lacerations in children. Br Med J. 1989; 299:1014. 1 . Thomson PD, Smith DJ. What is infection? Am J Surg. 2 1994; 167(1A ~~pplk7S-lOS. 13. Quinn JV,Maw JL, Ramotar K, et al. Octylcyanoacrylate tissue adhesive wound repair versus suture wound repair in a contaminated wound model. Surgery. 1997; 122:69-72. 14. Bruns TB, Simon HK, McLario DJ, et al. Laceration repair using a tissue adhesive in a children's emergency department. Pediatrics. 1996; 98:673-5. 1 . Quinn JV,Drzewiecki AE, Li MM, et al. A randomized, 8 controlled trial comparing a tissue adhesive with suturing in the repair of pediatric facial lacerations. Ann Emerg Med. 1993; 22:1130-5. 1 . Singer AJ, Church AL, Forrestal K, et al. Comparison of 6 patient satisfaction and practitioner satisfaction with wound appearance after traumatic wound repair. Acad Emerg Med. 1997; 4~133-7. 17. Fletcher RH, Fletcher SW, Wagner EH. Clinical Epidemiology: The Essentials, ed 2. Baltimore: Williams and Wilkins, 1988, p 137.
CONCLUSION
The MCID on the VAS cosmesis scale is 15 mm. Studies should be designed with a sample size t o have the power to determine this difference. Studies that have a large sample size may have the power to determine statistical differences less than this, but the clinical relevance of such smaller differences is uncertain.
You might also like
- Study On Pressure UlcerDocument219 pagesStudy On Pressure UlcerThein Ko Oo100% (1)
- Nueva Escala de VancouverDocument8 pagesNueva Escala de VancouverMargit MuñozNo ratings yet
- Values of A Patient and Observer Scar Assessment SDocument9 pagesValues of A Patient and Observer Scar Assessment SDesrainy InhardiniNo ratings yet
- Rcse9004 326Document6 pagesRcse9004 326Casian TripacNo ratings yet
- Jurnal Visual Analog ScaleDocument10 pagesJurnal Visual Analog ScaleFachri MubarokNo ratings yet
- 32Document12 pages32Amina GoharyNo ratings yet
- 551Document7 pages551dilkulNo ratings yet
- UntitledDocument21 pagesUntitledOmair HawkNo ratings yet
- Mauck 2014Document13 pagesMauck 2014I Made DuniaNo ratings yet
- Wound Image Analysis Classifier For Efficient Tracking of Wound Healing StatusDocument13 pagesWound Image Analysis Classifier For Efficient Tracking of Wound Healing Statussipij100% (1)
- 668-Article Text-1030-1-10-20181101Document4 pages668-Article Text-1030-1-10-20181101burhanNo ratings yet
- (ADC-KI-67) Correlation Between Apparent Diffusion Coefficient and The Ki-67 Proliferation Index in Grading Pediatric GliomaDocument7 pages(ADC-KI-67) Correlation Between Apparent Diffusion Coefficient and The Ki-67 Proliferation Index in Grading Pediatric Gliomaafdhal.888980No ratings yet
- Columna Paper Anato 2Document7 pagesColumna Paper Anato 2Claudio Cofré MansillaNo ratings yet
- ' Premio Publicación Indexada 2Document7 pages' Premio Publicación Indexada 2Francisco Álvarez MarcosNo ratings yet
- Eginton2003 - A Prospective Randomized Evaluation of Negative-Pressure Wound Dressings For Diabetic Foot WoundsDocument5 pagesEginton2003 - A Prospective Randomized Evaluation of Negative-Pressure Wound Dressings For Diabetic Foot WoundsburhanNo ratings yet
- Anzarut 2009Document8 pagesAnzarut 2009Salomón León Beaumont-BlancoNo ratings yet
- Comparing Running Vs Interrupted Sutures For Skin ClosureDocument11 pagesComparing Running Vs Interrupted Sutures For Skin Closureluisrmg91No ratings yet
- Pitcher 2017Document6 pagesPitcher 2017anhca4519No ratings yet
- PIIS000709121730212XDocument6 pagesPIIS000709121730212Xmansoormanu2929No ratings yet
- DG MRotDocument12 pagesDG MRotVictor Andrés Olivares IbarraNo ratings yet
- EJPRS - Volume 43 - Issue 2 - Pages 339-343Document5 pagesEJPRS - Volume 43 - Issue 2 - Pages 339-343mm7bc6wfqdNo ratings yet
- C - SpineDocument10 pagesC - SpineCharly MontielNo ratings yet
- Surgery For Unruptured Arteriovenous Malformations of The Brain Is Better Than Conservative Management For Selected Cases: A Prospective Cohort StudyDocument13 pagesSurgery For Unruptured Arteriovenous Malformations of The Brain Is Better Than Conservative Management For Selected Cases: A Prospective Cohort StudyAmina GoharyNo ratings yet
- Journal Homepage: - : IntroductionDocument5 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Jarbo OJSM Lever TestDocument7 pagesJarbo OJSM Lever Testashlyn granthamNo ratings yet
- Laporan Evaluasi Diri DiahDocument3 pagesLaporan Evaluasi Diri DiahVTry AL Ma'fhyNo ratings yet
- Jowc 2023 32 4 229Document6 pagesJowc 2023 32 4 229Sr Gabriel iNo ratings yet
- 1 s2.0 S0360301609016228Document2 pages1 s2.0 S0360301609016228andresNo ratings yet
- Determination of Minimum Clinically Important Difference in Pain, Disability, and Quality of Life After Extension of Fusion For Adjacent-Segment DiseaseDocument7 pagesDetermination of Minimum Clinically Important Difference in Pain, Disability, and Quality of Life After Extension of Fusion For Adjacent-Segment DiseasewilsonwqaNo ratings yet
- Jurnal New1Document5 pagesJurnal New1Nurul Qomariah TNo ratings yet
- 10 1016@j Jse 2018 11 025Document2 pages10 1016@j Jse 2018 11 025hari vijayNo ratings yet
- Comparison of Running Cutaneous Suture VS Spacing SutureDocument6 pagesComparison of Running Cutaneous Suture VS Spacing Sutureluisrmg91No ratings yet
- Kuhn2013 PDFDocument9 pagesKuhn2013 PDFNati GallardoNo ratings yet
- ContentServer AspDocument7 pagesContentServer AspCoralonNo ratings yet
- Ahn 2019 PDFDocument8 pagesAhn 2019 PDFMiguel Martín LandroveNo ratings yet
- 88 FullDocument10 pages88 Fullmarcus souzaNo ratings yet
- [Journal of Neurosurgery_ Spine] A points-based algorithm for prognosticating clinical outcome of Chiari malformation Type I with syringomyelia_ results from a predictive model analysis of 82 surgically managed adult patientsDocument10 pages[Journal of Neurosurgery_ Spine] A points-based algorithm for prognosticating clinical outcome of Chiari malformation Type I with syringomyelia_ results from a predictive model analysis of 82 surgically managed adult patientsdrpraveenkumarNo ratings yet
- 1547 5654 Article p80Document12 pages1547 5654 Article p80wilsonwqaNo ratings yet
- TMP 8 B86Document5 pagesTMP 8 B86FrontiersNo ratings yet
- Chron I SubduralDocument9 pagesChron I Subduralelton fidelisNo ratings yet
- Ekin 2018Document3 pagesEkin 2018barbaramcoelho7No ratings yet
- Prospective, Randomized, Controlled Trial Comparing A Tissue Adhesive (Dermabond™) With Adhesive Strips (Steri-Strips™) For The Closure of Laparoscopic Trocar Wounds in ChildrenDocument4 pagesProspective, Randomized, Controlled Trial Comparing A Tissue Adhesive (Dermabond™) With Adhesive Strips (Steri-Strips™) For The Closure of Laparoscopic Trocar Wounds in ChildrenluishelNo ratings yet
- Surgical Site Infection and Analytic Morphometric Assessment of Body Composition in Patients Undergoing Midline LaparotomyDocument9 pagesSurgical Site Infection and Analytic Morphometric Assessment of Body Composition in Patients Undergoing Midline LaparotomyJose Manuel Luna VazquezNo ratings yet
- ANZ Journal of Surgery - 2021 - Yang - Outcomes of Patients With Metastatic Cutaneous Squamous Cell Carcinoma To The Axilla PDFDocument8 pagesANZ Journal of Surgery - 2021 - Yang - Outcomes of Patients With Metastatic Cutaneous Squamous Cell Carcinoma To The Axilla PDFRong LiuNo ratings yet
- 117 1445002005 PDFDocument7 pages117 1445002005 PDFChristianWicaksonoNo ratings yet
- Circir 22 90 Supl-1 084-091Document8 pagesCircir 22 90 Supl-1 084-091Gustavo Adolfo Nato VázquezNo ratings yet
- Tendinitis Calcificante en Hombro. Comparación Ondas Choque Vs AgujaDocument7 pagesTendinitis Calcificante en Hombro. Comparación Ondas Choque Vs AgujaAJ CésarNo ratings yet
- Pillai2016 PDFDocument35 pagesPillai2016 PDFmehak malhotraNo ratings yet
- (10920684 - Neurosurgical Focus) Impact of Preoperative Endovascular Embolization On Immediate Meningioma Resection OutcomesDocument7 pages(10920684 - Neurosurgical Focus) Impact of Preoperative Endovascular Embolization On Immediate Meningioma Resection OutcomesBedussa NuritNo ratings yet
- Clinically Significant Outcomes After Meniscectomy 2019Document12 pagesClinically Significant Outcomes After Meniscectomy 2019asmaNo ratings yet
- Development_and_Validation_of_the_Scoring_System_of_AppendicitisDocument8 pagesDevelopment_and_Validation_of_the_Scoring_System_of_AppendicitisKUTLUHAN YILMAZ Prof DrNo ratings yet
- Quilting after mastectomy reduces seromaDocument5 pagesQuilting after mastectomy reduces seromabeepboop20No ratings yet
- Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests For Subacromial ImpingementDocument6 pagesReliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests For Subacromial ImpingementGiovanniNo ratings yet
- Skin Staples HectingDocument5 pagesSkin Staples HectingdesyNo ratings yet
- 31 McMahon - A New Method Keratoconus PDFDocument7 pages31 McMahon - A New Method Keratoconus PDFSetiawan Arif WibowoNo ratings yet
- J Neurosurg Article p693Document8 pagesJ Neurosurg Article p693ابراهيم ساميNo ratings yet
- Original Article: B Richardson, L Shepstone, F Poland, M Mugford, B Finlayson, N ClemenceDocument6 pagesOriginal Article: B Richardson, L Shepstone, F Poland, M Mugford, B Finlayson, N ClemenceZackyNo ratings yet
- Clinical Diagnosis of Uncomplicated, Acute Appendicitis Remains An Imperfect ScienceDocument3 pagesClinical Diagnosis of Uncomplicated, Acute Appendicitis Remains An Imperfect ScienceHector ReinozoNo ratings yet
- Skin Cancer!Document8 pagesSkin Cancer!HudiansyahNo ratings yet
- Managing Common and Uncommon Complications of Aesthetic Breast SurgeryFrom EverandManaging Common and Uncommon Complications of Aesthetic Breast SurgeryJohn Y.S. KimNo ratings yet
- Case-Study WiproDocument23 pagesCase-Study WiproSamir PradhanNo ratings yet
- Form 4: MT Pleasant HIGHDocument4 pagesForm 4: MT Pleasant HIGHEmmanuel ThilliNo ratings yet
- Computer Form 4 Schemes of Work - Term 1Document14 pagesComputer Form 4 Schemes of Work - Term 1api-158285296No ratings yet
- Simple Interest Lesson PlanDocument2 pagesSimple Interest Lesson Planapi-401904683No ratings yet
- Format - 4: Eligibility Certificate For Appearing at All India Trade Test AlongwithDocument2 pagesFormat - 4: Eligibility Certificate For Appearing at All India Trade Test AlongwithPradeep KumarNo ratings yet
- Employee AbsenteesiumDocument12 pagesEmployee AbsenteesiumBalaji RamalingamNo ratings yet
- Job Vacancy: PT Orbit Terminal MerakDocument1 pageJob Vacancy: PT Orbit Terminal MerakqiqiNo ratings yet
- Civil Service Test QuestionsDocument8 pagesCivil Service Test QuestionsMS. RB RACELISNo ratings yet
- Myth and Education by Ted HughesDocument15 pagesMyth and Education by Ted Hughesapi-426885520% (3)
- Collaborative Statistics Supplemental Course MaterialsDocument106 pagesCollaborative Statistics Supplemental Course MaterialsjojojNo ratings yet
- CE F241 Handout - MohanDocument3 pagesCE F241 Handout - MohanSai Kiran TulluriNo ratings yet
- Basketball Alternative Task 20131768 Attempt 2019-03-05-00-58-45 hlth3800 Physical Education Teaching Methods Liusaidh GilchristDocument2 pagesBasketball Alternative Task 20131768 Attempt 2019-03-05-00-58-45 hlth3800 Physical Education Teaching Methods Liusaidh Gilchristapi-401963473No ratings yet
- Smart Thinking - How To Think Conceptually, - Bryan GreethamDocument329 pagesSmart Thinking - How To Think Conceptually, - Bryan Greethamnj1508gmailcom100% (3)
- Tut 4 - QDocument3 pagesTut 4 - QLwk KheanNo ratings yet
- La Tierra Sin Mal Historia de Un Mito PDFDocument230 pagesLa Tierra Sin Mal Historia de Un Mito PDFbriceNo ratings yet
- ID Country Name Gender AgeDocument11 pagesID Country Name Gender AgeБазарбаев БолотбекNo ratings yet
- Catch Up Fridays - Orientation PresentationDocument21 pagesCatch Up Fridays - Orientation Presentationjannetfrancia.sorretaNo ratings yet
- Grade 8 Cre Schemes of Work Term 1 OxfordDocument32 pagesGrade 8 Cre Schemes of Work Term 1 OxfordMartin ThumbiNo ratings yet
- Teaching Competence AbstractDocument3 pagesTeaching Competence AbstractFarrah DeebaNo ratings yet
- Conruence TriangleDocument6 pagesConruence TriangleRenan PaculanangNo ratings yet
- Exxon Mobile Case StudyDocument4 pagesExxon Mobile Case StudyShaher ShaikNo ratings yet
- Outline 2018: Cultivating Professionals With Knowledge and Humanity, Thereby Contributing To People S Well-BeingDocument34 pagesOutline 2018: Cultivating Professionals With Knowledge and Humanity, Thereby Contributing To People S Well-BeingDd KNo ratings yet
- Lemonnier 1992a - Elements For An Anthropology of TechnologyDocument145 pagesLemonnier 1992a - Elements For An Anthropology of TechnologycarlosNo ratings yet
- 6th Grade Science SyllabusDocument3 pages6th Grade Science Syllabusapi-328938442No ratings yet
- Thesis Titles For Business Management StudentsDocument6 pagesThesis Titles For Business Management Studentsamberedmondsonnorman100% (2)
- Academic Qualifications: Curriculum Vitae DR (MRS) Madhulika DubeDocument18 pagesAcademic Qualifications: Curriculum Vitae DR (MRS) Madhulika DubeGopal Krishna TiwariNo ratings yet
- Why-Do-We-Have-Rules-Powerpoint Ver 1Document13 pagesWhy-Do-We-Have-Rules-Powerpoint Ver 1api-579429878No ratings yet
- NYC LSAT Tutor's Top 10 LSAT Tips and TricksDocument2 pagesNYC LSAT Tutor's Top 10 LSAT Tips and TricksSteve Schwartz50% (2)
- Brunei DarussalamDocument16 pagesBrunei DarussalamSalcalide SthorneNo ratings yet
- 3-Minute Korean S1 #1 Self: Lesson TranscriptDocument4 pages3-Minute Korean S1 #1 Self: Lesson TranscriptHafizah GhazaliNo ratings yet




































![[Journal of Neurosurgery_ Spine] A points-based algorithm for prognosticating clinical outcome of Chiari malformation Type I with syringomyelia_ results from a predictive model analysis of 82 surgically managed adult patients](https://imgv2-2-f.scribdassets.com/img/document/582906155/149x198/902c0eb201/1710564842?v=1)