Professional Documents
Culture Documents
Disturbed Sensory Perception
Uploaded by
Exia QuinagonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Disturbed Sensory Perception
Uploaded by
Exia QuinagonCopyright:
Available Formats
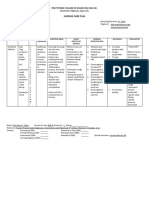
Disturbed Sensory Perception (Sensory Overload) related to change in environment, and hearing loss (as evidenced by disorientation to time
and place; restlessness; and altered behavior)
Provide a consistent physical environment and a daily routine. Provide access to familiar objects, when possible. Provide a low-stimulation environment for Mrs. Hagstrom because disorientation may be increased by overstimulation. Provide for adequate rest, sleep, and daytime naps. Use a calm and unhurried approach when interacting with Mrs. Hagstrom. Speak to the client in a slow, distinct manner with appropriate volume. Engage Mrs. Hagstrom in concrete here and now activities (that is, ADLs) that focus on something outside the self that is concrete and reality oriented.
Routine eliminates the element of surprise, overstimulation, and further confusion. Familiarity helps reduce confusion. A disruption in the quality or quantity of incoming stimuli can affect a person s cognitive status. Sensory overload blocks out meaningful stimuli. Reduces overstimulation and fatigue, which may be contributing factors to confusion. Promotes communication that enhances the person s sense of dignity. The client who has difficulty hearing will be better able to lip read and comprehend speech. Assists the individual to differentiate between own thoughts and reality. Hearing can be enhanced if the volume is appropriate and the hearing aid is consistently used. Effective listening is essential in a nurse client relationship. Poor listening skills can undermine trust and block therapeutic communication. Using simple terms and short sentences facilitates understanding and minimizes anxiety. Gaining the attention of a client with a hearing impairment is an essential first step toward effective communication. However, the client s personal space should be respected and permission to touch should be obtained.
Facilitate use of hearing aids, as appropriate. Listen attentively. Use simple words and short sentences, as appropriate. Obtain Mrs. Hagstrom s attention through touc
Nursing Diagnosis: Bathing hygiene Self care deficit NANDA Definition: Impaired ability to perform or complete bathing/hygiene activities for oneself Defining Characteristics: Inability to: wash body or body parts; obtain or get to water source; regulate temperature or flow of bath water; get bath supplies; dry body; get in and out of bathroom Impaired physical mobility-functional level classification: y Completely independent Requires use of equipment or device Requires help from another person for assistance, supervision, or teaching Requires help from another person and equipment or device Dependent does not participate in activity Related Factors: Decreased or lack of motivation; weakness and tiredness; severe anxiety; inability to perceive body part or spatial relationship; perceptual or cognitive impairment; pain; neuromuscular impairment; musculoskeletal impairment; environmental barriers NOC Outcomes (Nursing Outcomes Classification) Suggested NOC Labels Self-Care: Activities of Daily Living (ADLs) Self-Care: Bathing Self-Care: Hygiene Nursing Interventions and Rationales y Assess client's ability to bathe self through direct observation (in usual bathing setting only) and from client/caregiver report, noting specific deficits and their causes. Use of observation of function and report of function provide complementary assessment data for goal and intervention planning . y If in a typical bathing setting for the client, assess via direct observation using physical performance tests for ADLs. Observation of bathing performed in an atypical bathing setting may result in false data for which use of a physical performance test compensates to provide more accurate ability data . y Ask client for input on bathing habits and cultural bathing preferences. Creating opportunities for guiding personal care honors long-standing routines, increases control, prevents learned helplessness, and preserves self-esteem. Cultural preferences are respected. y Develop a bathing care plan based on client's own history of bathing practices that addresses skin needs, self-care needs, client response to bathing and equipment needs. Bathing is a healing rite and should not be routinely scheduled with a task focus. It should be a comforting experience for the client that enhances health.. y Individualize bathing by identifying function of bath , frequency required to achieve function, and best bathing form to meet client preferences, preserve client dignity, make bathing a soothing experience, and reduce client aggression. Individualized bathing produces a more positive bathing experience and preserves client dignity. Client aggression is increased with shower and tub bathing. Towel bathing increases privacy and eliminates need to move client to central bathing area; therefore it is a more soothing experience than either showering or tub bathing. y Request referrals for occupational and physical therapy. Collaboration and correlation of activities with interdisciplinary team members increases the client's mastery of self-care tasks. y Plan activities to prevent fatigue during bathing and seat client with feet supported. Energy conservation increases activity tolerance and promotes self-care. y Provide medication for pain 45 minutes before bathing if needed. Pain relief promotes participation in self-care. y Consider environmental and human factors that may limit bathing ability, such as bending to get into tub, reaching required for bathing items, grasping force needed for faucets, and lifting of self. Adapt environment by placing items within easy reach, lowering faucets, and using a handheld shower. Environmental factors affect task performance. Function can be improved based on engineering principles that adapt environmental factors to the meet the client's capabilities. y Use any necessary adaptive bathing equipment. Adaptive devices extend the client's reach, increase speed and safety, and decrease exertion.
Provide privacy: have only one caregiver providing bathing assistance, encourage a traffic-free bathing area, and post privacy signs. The client perceives less privacy if more than one caregiver participates or if bathing takes place in a central bathing area in a high-traffic location that allows staff to enter freely during care . y Keep client warmly covered. Clients, especially elderly clients, who are prone to hypothermia may experience evaporative cooling during and after bathing, which produces an unpleasant cold sensation . y Allow client to participate as able in bathing. Smile and provide praise for accomplishments in a relaxed manner. The client's expenditure of energy provides the caregiver the opportunity to convey respect for a well-done task, which increases the client's self-esteem. Smiling and being relaxed are associated with a calm, functional client response. y Inspect skin condition during bathing. Observation of skin allows detection of skin problems. y Use or encourage caregiver to use an unhurried, caring touch. The basic human need of touch offers reassurance and comfort. y If client is bathing alone, place assistance call light within reach. A readily available signaling device promotes safety and provides reassurance for the client. Risk for ineffective airway clearance related to aspiration of tube feeding N U R S I N G C A R E OF T H E P A T I E N T W I T H A N A S O G A S T R I C T U B E a. P r ovi de g o o d o r a l h y g i e n e at r e g u l ar a n d f r e q u e n t i n t er va l s. O f f e r w a t e r or m o u t h w a s h to r i n se t h e m o u t h e v e r y h o u r . Assi st t h e pa ti e nt to b r u s h h i s t e e t h at l e a st ever y 4 hours. b. K e e p t h e nostr i l s f r e e of a c c u m u l a t i o n s of dr ied sec r eti on s. c. If perm i ssi bl e, a p p l y l ub r i c a nt s u c h as Vasel i ne to t h e li ps a n d nostr i l s f o r t h e pati ent's c o m f or t . P ati ents may w e a r lipstick. d. E n c o u r a g e t h e p ati en t to s w a l l o w s al i va n a t u r a l l y ; t h e t u b e is a c o n s t a n t s o u r c e of a n n o y a n c e a n d t h e p at i en t may h a v e a t e n d e n c y to e xp ec tor at e e xc e s s i v el y . The p hy s i c i a n may a l l o w c h e w i n g gum or h a r d c a n d y to h e l p m ai n t a i n m o u t h m o i s t ur e a n d to e n c o u r a g e n o r m a l s w a l l o w i n g of s al i v a. Only c o n sc i o u s , r e s p o n si ve , a l e r t pati en ts s h o u l d be g i v e n t h e s e i tem s. C A U T I O N : R e m i n d t h e pa ti e nt to r e m o v e gum or c a n d y b ef or e m o u t h c a r e a n d s l e ep. e. R e p o r t c om p l a i n t s a n d s i g n s of n o s e or t h r o a t irri tation ( e xc e s si v e m u c u s , s o r e t h r o a t , or h o a r s en e s s ) . f. E n c o u r a g e t h e pa ti e nt to c h a n g e posi ti on f r e qu e n t l y , u s i n g c a r e n o t to p u l l on t h e t u b e a n d n o t to l i e on t h e dr ai nag e t u b i n g . g. F o l l o w diet or der s e x a c t l y . If w a t e r or c l ea r f l ui d s a r e a l l o w e d by m o u t h , be s u r e to c h e c k on a m o u n t to be g i v e n at o n e ti m e. K n o w e x a c t l y w h e t h e r or n o t t h e t u b e is to be c l a m p e d when f l ui d s a r e g i v e n a n d at w h a t t i m e i n te r v al in r el ati on to o r a l i n ta ke. F o r e x a m p l e , t h e or d er may be to c l a m p t h e dr ai nag e t u b e f o r 1 h o u r af te r i nt ak e to a l l o w s o m e abs or pti o n y
You might also like
- Assessing and Managing Risk of AspirationDocument6 pagesAssessing and Managing Risk of AspirationaianrNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care Planapi-309251523No ratings yet
- NCP PryllDocument6 pagesNCP PryllpjcolitaNo ratings yet
- Nursing Care PlanDocument1 pageNursing Care Planapi-38118511380% (10)
- NCP For StokeDocument5 pagesNCP For StokeMemedNo ratings yet
- Impaired Verbal CommunicationDocument6 pagesImpaired Verbal CommunicationLaura Sansonetti100% (1)
- As Needed.: Environmental Stimuli 6Document4 pagesAs Needed.: Environmental Stimuli 6Nicole GumolonNo ratings yet
- Nursing Care Plan For Special ChildrenDocument2 pagesNursing Care Plan For Special Childrenharas_dcsaisNo ratings yet
- Nursing Care PlansDocument4 pagesNursing Care Plansapi-19762967No ratings yet
- Nursing Interventions for SchizophreniaDocument1 pageNursing Interventions for SchizophreniaTalTal Balcera Beniten100% (1)
- Content: Outline Form Only Make A Separate Sheet For The Content. The Health Teaching Plan Should Focus On Home Care For Patients With Mood DisorderDocument4 pagesContent: Outline Form Only Make A Separate Sheet For The Content. The Health Teaching Plan Should Focus On Home Care For Patients With Mood DisorderRaffy Sebastian Seballos100% (1)
- NCP Disturbed Sensory PerceptionDocument3 pagesNCP Disturbed Sensory PerceptionEdmarkmoises ValdezNo ratings yet
- Nursing Care Plan for Client with Altered Thought ProcessDocument5 pagesNursing Care Plan for Client with Altered Thought ProcessOphelia Ross Omaña TutanesNo ratings yet
- NCP Alcoholic NeuropathyDocument5 pagesNCP Alcoholic NeuropathyPeachy Marie Anca100% (1)
- HTP of AsthmaDocument1 pageHTP of AsthmaMarland Faith Dela CruzNo ratings yet
- Nursing Care PlanDocument5 pagesNursing Care PlanJohn Paul Delos Santos100% (1)
- Nursing Care Plans for Pain Management and Self-CareDocument15 pagesNursing Care Plans for Pain Management and Self-CareKarl Vincent Soso100% (1)
- Acute Confusion Nursing DiagnosisDocument4 pagesAcute Confusion Nursing Diagnosisasmika danaNo ratings yet
- Gender Dysphoria NCPDocument1 pageGender Dysphoria NCPSeann LorescoNo ratings yet
- Risk For Infection NCP Ortho JadDocument1 pageRisk For Infection NCP Ortho JadjadpauloNo ratings yet
- Teaching Plan Gerontologic NursingDocument3 pagesTeaching Plan Gerontologic NursingJoan AbardoNo ratings yet
- NCPDocument2 pagesNCPShubhangi SarwanNo ratings yet
- NCP Impaired Skin IntegrityDocument4 pagesNCP Impaired Skin IntegrityElgie SantosNo ratings yet
- HoplessnessDocument16 pagesHoplessnessHamza IshtiaqNo ratings yet
- Activity IntoleranceDocument2 pagesActivity IntoleranceDiane AbanillaNo ratings yet
- GENERAL SANTOS DOCTORS’ MEDICAL SCHOOL FOUNDATION NURSING CARE PLANDocument4 pagesGENERAL SANTOS DOCTORS’ MEDICAL SCHOOL FOUNDATION NURSING CARE PLANFran LanNo ratings yet
- Cues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalDocument4 pagesCues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalKei Cruz100% (1)
- Nursing Diagnosis Care Plan HyponitremiaDocument2 pagesNursing Diagnosis Care Plan HyponitremiaAbdallah AlasalNo ratings yet
- Risk For Fall and Risk For Imbalanced Nutrition Less Than Body Requirements Pantoprazole, Ketorolac, Cefoxitin Drug StudyDocument4 pagesRisk For Fall and Risk For Imbalanced Nutrition Less Than Body Requirements Pantoprazole, Ketorolac, Cefoxitin Drug StudyKevin John ReaLubit SaLisiNo ratings yet
- Central Nervous System Nursing Care PlanDocument11 pagesCentral Nervous System Nursing Care PlanUday Kumar100% (1)
- Nursing Assessment Objectives and Intervention for ConjunctivitisDocument2 pagesNursing Assessment Objectives and Intervention for ConjunctivitisIna Marie Calungcaguin Castro100% (1)
- Risk For InfectionDocument5 pagesRisk For InfectionRochelle Corneta JoreNo ratings yet
- FractureDocument1 pageFractureReechie TeasoonNo ratings yet
- NCP Impaired Physical MobilityDocument1 pageNCP Impaired Physical MobilityCharmaine SolimanNo ratings yet
- Acute Pain Assessment and Nursing InterventionsDocument1 pageAcute Pain Assessment and Nursing InterventionsAi RouNo ratings yet
- Doxofylline: D 400 MG TabletsDocument33 pagesDoxofylline: D 400 MG TabletsBibek Singh Mahat100% (2)
- High Percentage of Sleep Disturbances Can Affect The Recovery of The PatientDocument1 pageHigh Percentage of Sleep Disturbances Can Affect The Recovery of The PatientMatt SinnungNo ratings yet
- Nursing Care Plan Format Name: - Medical Diagnosis: - DateDocument2 pagesNursing Care Plan Format Name: - Medical Diagnosis: - DateSheryl Ann Barit PedinesNo ratings yet
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- Compartment Syndrome NCP (PAIN)Document2 pagesCompartment Syndrome NCP (PAIN)eunica16No ratings yet
- NCP Ineffective Airway Clearance Related To The Accumulation of Exudates in The Alveoli TBDocument3 pagesNCP Ineffective Airway Clearance Related To The Accumulation of Exudates in The Alveoli TBMa. Elaine Carla Tating0% (1)
- NCP Assessment Diagnosis Planning Short-Term GoalDocument4 pagesNCP Assessment Diagnosis Planning Short-Term GoalJessieRamosAnicetoNo ratings yet
- Disturbed Sensory PerceptionDocument3 pagesDisturbed Sensory PerceptionJoenna GaloloNo ratings yet
- Nursing Care Plan for Improving HygieneDocument2 pagesNursing Care Plan for Improving HygieneMartin Lєtmaku EspinaNo ratings yet
- NCP Self CaRE DeficitDocument1 pageNCP Self CaRE Deficitnicole pageNo ratings yet
- Psych NCPDocument1 pagePsych NCPEliza Joy Franco RNNo ratings yet
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 pagesCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- Idoc - Pub Nursing Care Plan For Seizure NCPDocument2 pagesIdoc - Pub Nursing Care Plan For Seizure NCPACERET, IVAN LAURENTINE G.No ratings yet
- AudiDocument3 pagesAudiFlorygene Kris Disagon0% (1)
- Health Education Plan - Case StudyDocument7 pagesHealth Education Plan - Case StudyRenzy Mayven Pedriña LobatonNo ratings yet
- Risk For Impaired SwallowingDocument3 pagesRisk For Impaired SwallowingCalimlim Kim100% (1)
- NCP Sensory PerceptionDocument2 pagesNCP Sensory PerceptionGina TangneneiNo ratings yet
- Impaired Physical Mobility...Document3 pagesImpaired Physical Mobility...Christy BerryNo ratings yet
- NCP ImpairedSocial AutismDocument2 pagesNCP ImpairedSocial AutismPaul AnteNo ratings yet
- Nursing Diagnosis: Urinary Retention: NOC Outcomes (Nursing Outcomes Classification)Document4 pagesNursing Diagnosis: Urinary Retention: NOC Outcomes (Nursing Outcomes Classification)rem_No ratings yet
- 3 NCP AsthmaDocument6 pages3 NCP AsthmajaninenicoleNo ratings yet
- Nursing Care PlansDocument7 pagesNursing Care PlansJayson Sumampong100% (1)
- bsn-3 l2Document30 pagesbsn-3 l2Valerie LuoNo ratings yet
- Coonk CapstoneseminarDocument23 pagesCoonk Capstoneseminarapi-251977061No ratings yet
- Disturbed Thought ProcessesDocument5 pagesDisturbed Thought ProcessesZarah Jane Cadavez EspañoNo ratings yet
- Irr of Ra 9266Document27 pagesIrr of Ra 9266Gracelle Anne Pajarillaga Padolina100% (1)
- BP 344Document58 pagesBP 344Ultrabuilders Const100% (14)
- DocumentDocument2 pagesDocumentShivajiNo ratings yet
- CCPM 1 Day Training Extract PDF v10 20151018 PDFDocument71 pagesCCPM 1 Day Training Extract PDF v10 20151018 PDFExia QuinagonNo ratings yet
- Bio Philia 1Document32 pagesBio Philia 1Exia QuinagonNo ratings yet
- Bio Philia 1Document32 pagesBio Philia 1Exia QuinagonNo ratings yet
- Exia Nareye Quinagon Bs Arch VB Section I - Basis of Project DecisionDocument2 pagesExia Nareye Quinagon Bs Arch VB Section I - Basis of Project DecisionExia QuinagonNo ratings yet
- Kevin Rig Don Elements and Principals of DesignDocument45 pagesKevin Rig Don Elements and Principals of DesignNoeliaNo ratings yet
- Theory of Architecture LectureDocument15 pagesTheory of Architecture Lecturejella218100% (1)
- Comprehensive Famous ArchitectsDocument25 pagesComprehensive Famous ArchitectsExia QuinagonNo ratings yet
- Change Management On Construction Projec PDFDocument16 pagesChange Management On Construction Projec PDFExia QuinagonNo ratings yet
- Network Scheduling, Planning & Controlling: TechniquesDocument38 pagesNetwork Scheduling, Planning & Controlling: TechniquesExia QuinagonNo ratings yet
- 6020635Document48 pages6020635Exia QuinagonNo ratings yet
- Camella BantayDocument13 pagesCamella BantayExia QuinagonNo ratings yet
- Plumbing - LecturesDocument235 pagesPlumbing - LecturesCirky NadleiNo ratings yet
- PlanningDocument1 pagePlanningExia QuinagonNo ratings yet
- Guidelines For NursesDocument18 pagesGuidelines For NursesExia QuinagonNo ratings yet
- Urban Growth Through Industrial LocationDocument3 pagesUrban Growth Through Industrial LocationExia QuinagonNo ratings yet
- Shaping BuildingsDocument28 pagesShaping BuildingsPrakhar JainNo ratings yet
- Fundamentals of Urban Planning and Devel PDFDocument28 pagesFundamentals of Urban Planning and Devel PDFExia QuinagonNo ratings yet
- Introduction to the dimensions of heritageDocument76 pagesIntroduction to the dimensions of heritageExia QuinagonNo ratings yet
- Theresa Marie B. Presto Bs Arch 4BDocument5 pagesTheresa Marie B. Presto Bs Arch 4BExia QuinagonNo ratings yet
- Fundamentals of Urban Planning and CommunityDocument6 pagesFundamentals of Urban Planning and CommunityExia QuinagonNo ratings yet
- Conservation Principles for Protecting Cultural HeritageDocument57 pagesConservation Principles for Protecting Cultural HeritageExia Quinagon100% (1)
- Case Study PlanningDocument26 pagesCase Study PlanningExia QuinagonNo ratings yet
- EDRA39-Scherrmer 1Document6 pagesEDRA39-Scherrmer 1Exia QuinagonNo ratings yet
- Rizal's Early Life and EducationDocument41 pagesRizal's Early Life and EducationExia QuinagonNo ratings yet
- Business Letter PartsDocument6 pagesBusiness Letter PartsExia QuinagonNo ratings yet
- Whatsdifferentbetweenurbanplan UrbandesiDocument13 pagesWhatsdifferentbetweenurbanplan UrbandesiExia QuinagonNo ratings yet
- The coming Evil? paper explores apocalyptic end timesDocument22 pagesThe coming Evil? paper explores apocalyptic end timesclaudiomainoNo ratings yet
- Ackermann Et Al 2022 - Assessing Performing Artists in Medical and Health Practice - The Dancers, Instrumentalists, Vocalists, and Actors Screening ProtocolDocument3 pagesAckermann Et Al 2022 - Assessing Performing Artists in Medical and Health Practice - The Dancers, Instrumentalists, Vocalists, and Actors Screening ProtocolCarlos TinocoNo ratings yet
- Peer Pressure and FOMO: Causes, Effects and How to OvercomeDocument5 pagesPeer Pressure and FOMO: Causes, Effects and How to OvercomeAaryan ChhabraNo ratings yet
- A3 ASD Mind MapDocument1 pageA3 ASD Mind Mapehopkins5_209No ratings yet
- HSC PDHPE Study NotesDocument29 pagesHSC PDHPE Study NotesJovian Hon100% (1)
- 8 - Sullivan - Interpersonal TheoryDocument11 pages8 - Sullivan - Interpersonal TheoryAuie Trajano100% (1)
- Legal Medicine Solis Notes Ethics And Legal IssuesDocument101 pagesLegal Medicine Solis Notes Ethics And Legal IssuesLeoj AnuleNo ratings yet
- Chapter 9, 10, & 11 Intrapersonal, Academic, & Social Life SkillsDocument14 pagesChapter 9, 10, & 11 Intrapersonal, Academic, & Social Life SkillseyobgashawNo ratings yet
- The Impact of Disaster On Mental Health: Prospective and Retrospective AnalysesDocument20 pagesThe Impact of Disaster On Mental Health: Prospective and Retrospective AnalysesIrma ZarinaNo ratings yet
- Project Management-Kaitlyn Baldwin Nurs 495Document12 pagesProject Management-Kaitlyn Baldwin Nurs 495api-239640492No ratings yet
- Declamation PiecesDocument4 pagesDeclamation PiecesAxeliaNo ratings yet
- Is The Lefkoe Belief Process A FraudDocument5 pagesIs The Lefkoe Belief Process A FraudzvasanthNo ratings yet
- Jeff Pages - Homeopathic SymptomsDocument8 pagesJeff Pages - Homeopathic SymptomsSatish MishraNo ratings yet
- The Effects of Childhood Sexual Abuse On Children's Psychology andDocument6 pagesThe Effects of Childhood Sexual Abuse On Children's Psychology andLeonan PalmaNo ratings yet
- NCP Inffective Individual CopingDocument1 pageNCP Inffective Individual CopingNatalie DulawanNo ratings yet
- A Safe Container For FearDocument3 pagesA Safe Container For FearMārs LaranNo ratings yet
- Untitled PDFDocument74 pagesUntitled PDFatjoerossNo ratings yet
- The Foundation of Natural GameDocument6 pagesThe Foundation of Natural GamewhitepaladinNo ratings yet
- Understanding Emotions Through NeuroscienceDocument7 pagesUnderstanding Emotions Through NeuroscienceEffie VlachouNo ratings yet
- Crisis Theory: Definition, Description, DynamicsDocument8 pagesCrisis Theory: Definition, Description, Dynamicsjhaxeq_0205No ratings yet
- Preoperative and Post Liver Transplant Nursing Care PlanDocument5 pagesPreoperative and Post Liver Transplant Nursing Care PlanOctoober67% (6)
- NSTP CWTS 1 Module 3 Drug and Substance Abuse Prevention and Control Part 2Document40 pagesNSTP CWTS 1 Module 3 Drug and Substance Abuse Prevention and Control Part 2Kate MabbunNo ratings yet
- Role of Parents and Exam Anxiety IssuesDocument13 pagesRole of Parents and Exam Anxiety IssuesZeeshan TaslimNo ratings yet
- Nursing Care Plan For "Disaster Considerations"Document15 pagesNursing Care Plan For "Disaster Considerations"jhonroks100% (14)
- Marisol Cortes Rincon DissertationDocument8 pagesMarisol Cortes Rincon DissertationWebsitesToTypePapersUK100% (1)
- Introduction:-: Study The Strategies of Overcoming Stage FrightDocument7 pagesIntroduction:-: Study The Strategies of Overcoming Stage FrightAmbika Hiraji GaikwadNo ratings yet
- Inositol - Benefits, Side Effects and DosageDocument14 pagesInositol - Benefits, Side Effects and DosageAri Sa FaNo ratings yet
- The Brief Symptom Inventory An Introductory ReportDocument5 pagesThe Brief Symptom Inventory An Introductory ReportSubhan AnsariNo ratings yet
- Parenting Style in Pediatric Dentistry PDFDocument7 pagesParenting Style in Pediatric Dentistry PDFJude Aldo PaulNo ratings yet
- S3 Perinatal DeppressionDocument15 pagesS3 Perinatal DeppressionAmir Iqbal Mallick100% (1)