Professional Documents
Culture Documents
Aspergillosis of The Orbit
Uploaded by
Deba P SarmaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aspergillosis of The Orbit
Uploaded by
Deba P SarmaCopyright:
Available Formats
Aspergillosis of the orbit
DEBA SARMA, MD WILLIAM ROHR, MD CHRISTIAN HAINDEL, MD New Orleans
Lspergillosis of the orbit is a rare entity, only 35 cases have been reported in the literature since 1913.l ~ ' Interestingly, three of the 35 cases have been from the New Orleans area.1- 8 We are reporting an additional case of orbital aspergillosis to illustrate the difficulties that may be encountered in making such a diagnosis.
Case Report
A 57-year-old man presented in November 1980 to the Veterans Administration Hospital of New Orleans with a two-year history of proptosis of the right eye. The patient s past medical history included pulmonary tuberculosis diagnosed in 1945 by examination of gastric specimens and radiologic findings. Treatment consisted of bed rest for one year. A 1962 follow-up chest film revealed significant changes and he received treatment with INH and pyridoxine for one year. There was no further evidence of tuberculosis. Additional medical history included a hemorrhoidectomy in 1971 and resection for benign prostatic hyperplasia in 1979. The patient was a non-smoker and a school bus driver for most of his life. There was no history of agricultural work. Initial physical examination including x-rays and CT scan revealed a soft tissue mass of the right frontal, ethmoid and maxillary sinuses and the inferior orbit. A Caldwell-Luc exploration was performed. It was clinically felt to be a mucocele involving the maxillary sinus; however, a biopsy revealed chronic inflammation and foreign body giant cell reaction of nasal mucosa. The patient did well until September 1981 when his proptosis began to increase. A repeat Caldwell-Luc procedure was performed. Biopsy tissue revealed marked chronic inflammation, fibrosis and diffuse granulomatous inflammation with focal caseous-like necrosis. There was no vasculitis. Special stains for organisms were negative. Cultures of this tissue failed to grow fungi or tuberculous organisms. Histology was, however, compatible with tuberculosis despite the absence of organisms and the
From the Departments of Pathology and Otolaryngology, LSI 1 Medical Center and Veterans Administration Medical Center, New Orleans, La.
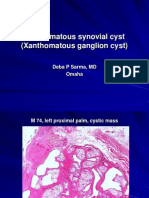
Fig. 1. Biopsy tissue showing necrotic and granulomatous process containing septate hyphae with dichotomous branching of Aspergillus species (PAS x 200).
patient was again placed on anti-tuberculosis medications. Worsening proptosis necessitated readmittance in April 1982 for reevaluation. A repeat CT scan showed a mass invading the right orbit and cribriform plate. Clinically it was then felt that because of previous histology7, failure to respond to antituberculous therapy and location of the process the patient had lethal midline granuloma. He was then placed on prednisone. One month later in May 1982 worsening proptosis necessitated a third Caldwell-Luc exploration. Biopsy tissue showed chronic inflammation, fibrosis. and granulomatous inflammation. Special stains revealed septate fungal hyphae with uniform diameter and dichotomous branching consistent with Aspergillus species (Fig 1). Culture of the tissue specimen grew Aspergillus fumigatus sensitive to Amphotericin B. The patient was put on intravenous Amphotericin B therapy. In November 1982 a CT scan revealed invasion of the roof of the right orbit, which on biopsy showed granulomatous inflammation with focal necrosis containing Aspergillus hyphae. After excluding an involvement of the central nervous system by clinical examination,
19
June 1984 - Vol. 136, No. 6
J. LOUISIANA STATE M. Soc.
radiologic evidence, and examination of spinal fluid, he underwent a right orbital exenteration. Post-operatively the patient was placed on Rifampin and Amphotericin B and was discharged in satisfactory condition one month later. Discussion Aspergillus is a saphrophytic fungus grouped with the ascomycetes. It is virtually ubiquitous and is tound as an infectious agent in agricultural workers and those exposed to pigeons. It is a normal flora of the mucous membranes. In man, Aspergillus infections are usually those involving the lower respiratory tract and show a predilection for the immunosuppressed host. It frequently is implicated in "swimmer's ear" caused by Aspergillus nisfr}. Infections of the paranasal sinuses and orbit are considered rare. The diagnostic work-up of Aspergillus intection includes the clinical and radiologic examination, culture and the microscopic examination of exudates or tissue with the use of special stains, serologic methods, and less commonly skin testing and injection of infected material into pigeons. Infection of the orbit is usually the result ot direct extension from paranasal sinuses. The eveball can become infected as well bv this process. There are no pre-
disposing factors and most of the cases have been tound in warm, humid climate such as that of the southeastern United States. The disease is ot slow, insidious onset. The patient usually presents with proptosis and impaired ocular movement. There may be destruction of bony orbital walls on x-ray and CT scan. Physical examination usually reveals a sinusitis. Histologic studies of biopsied material show granulomatous inflammation and fibrosis with uniform, septate hyphae with dichotomous branching that stain better on periodic acid-Schiff i PAS) stain than hematoxylin and eosin (H&E) stain. Most cases ot orbital Aspergillosis are caused by Aspergillus fumigatus or Aspergillus niger. A. orijzae and A. flavus have also been implicated. l Treatment is primarily surgical including exenteration of the orbit. Systemic antitungal drugs, such as Amphotericin B. 5-Flurocytosin and Rifampin have been used as well as local washings by pimaricin. Antifungal susceptibility testing is of utmost importance. Outcome is often fatal. This case demonstrates problems in the diagnosis ot orbital aspergillosis. First, growth of the organism may be difficult. Repeated attempts at growth were unsuccessful. The reason tor this is probably inadequate sampling. Secondly, serologic testing was non-reactive on both serum and cerebrospinal fluid for Aspergillus antibodies. Thirdly, the spectrum of granulomatous disease is quite broad, especially in the paranasal area, therefore an aggressive attempt at diagnosis should be made. A differential should include fungal disease as well as tuberculosis, sarcoidosis. secondary lues and gummas. earlv leprosy, lethal midline granuloma. polymorphic "reticulosis." Wegener s granulomatosis and relapsing polvchondritis. In addition to Aspergillosis. histoplasmosis. leishmaniasis. actinomycosis and coccidioidomvcosis should be included in the differential diagnosis. References
1. Green \VR. Font RL. Zimmerman LE. Aspergillosis of the orbit. Report or' ten cases and review of the literature. Arch Ophthalmol 1969:82:302-313 2. Zinneman HH: Sinus-orbital aspergillosis. Minn Med 1972-55:661664 5. Lacaz CD. De Azevedo ML. Varuas AA. et al: Orbital aspereillosis caused bv Aspergillus tlavus. Rfc Paul Med 1978.91:64-67 4. Dhir SP. Banerjee AK. Chopra [S. et al: Orbitocramal aspergillo sis. Indian ] Ophthalmol 1978:26:34-38 5. Harmsch IP. Oberwinder D. Staib F. et al: Orbital asperaiilosis. Win Monatsbl Ausenheilkd 1979:175:65-71 6. SekulaJ. Popeilski L. Betkowski A: A case 01 aspergillosis involving the frontal sinus and orbit. Otolanmsol Pol 19SI.J.V365-369 7. Yu V'L. \VagnerGE. Shadomv S: Sino-orbital asperaiilosis treated with combination of antifunaal therapy. JAMA 180:244:814-815 S. Seaburv JH. Samuels M: The pathoeenetic <pectrum of asperaillosis. Am J Ctin Pathol 1963.40:21-33
June L9S4 - Vol. 136. No. 6
Sarma DP, Rohr W, Haindel C(1984): Aspergillosis of the orbit. J La State Med Soc 136:19-20. PMID: 6376706 [PubMed - indexed for MEDLINE]
You might also like
- Pilar Cyst With Crystals. Deba P Sarma, MDDocument2 pagesPilar Cyst With Crystals. Deba P Sarma, MDDeba P SarmaNo ratings yet
- Acantholytic Acanthoma (Epidermolytic Acanthoma), M 65, NeckDocument5 pagesAcantholytic Acanthoma (Epidermolytic Acanthoma), M 65, NeckDeba P SarmaNo ratings yet
- Acantholytic Acanthoma. M 60, ScrotumDocument8 pagesAcantholytic Acanthoma. M 60, ScrotumDeba P SarmaNo ratings yet
- Acantholytic Acanthoma (Epidermolytic Acanthoma), M 65, NeckDocument5 pagesAcantholytic Acanthoma (Epidermolytic Acanthoma), M 65, NeckDeba P SarmaNo ratings yet
- Publications of Deba P Sarma With The Pathology Residents and Medical Students, CUMC 2006-12Document14 pagesPublications of Deba P Sarma With The Pathology Residents and Medical Students, CUMC 2006-12Deba P SarmaNo ratings yet
- Acantholytic Bullous DiseaseDocument4 pagesAcantholytic Bullous DiseaseDeba P SarmaNo ratings yet
- Accessory TragusDocument3 pagesAccessory TragusDeba P SarmaNo ratings yet
- Pilar Cyst With CrystalsDocument2 pagesPilar Cyst With CrystalsDeba P SarmaNo ratings yet
- Deba P Sarma, MD Publications 1974 To 2010 DSDocument12 pagesDeba P Sarma, MD Publications 1974 To 2010 DSDeba P SarmaNo ratings yet
- Acantholytic Bullous Disease (Darier's Disease, Keratosis Follicularis)Document3 pagesAcantholytic Bullous Disease (Darier's Disease, Keratosis Follicularis)Deba P SarmaNo ratings yet
- Acantholytic Solar Keratosis, M 67, Forehead PDFDocument6 pagesAcantholytic Solar Keratosis, M 67, Forehead PDFDeba P SarmaNo ratings yet
- Deba P Sarma's Publication With Bryan Teruya, Creighton University Medical School, 2006-2012Document1 pageDeba P Sarma's Publication With Bryan Teruya, Creighton University Medical School, 2006-2012Deba P SarmaNo ratings yet
- Accessory Tragus, M, 1 MonthDocument3 pagesAccessory Tragus, M, 1 MonthDeba P SarmaNo ratings yet
- Acantholytic Dermatosis With DyskeratosisDocument11 pagesAcantholytic Dermatosis With DyskeratosisDeba P SarmaNo ratings yet
- Acantholytic Actinic KeratosisDocument4 pagesAcantholytic Actinic KeratosisDeba P SarmaNo ratings yet
- Acantholytic Actinic Keratosis, M 67, ForeheadDocument6 pagesAcantholytic Actinic Keratosis, M 67, ForeheadDeba P SarmaNo ratings yet
- Balanitis Circumscripta Plasmacellularis (Zoon's Balanitis, Plasma Cell Balanitis)Document6 pagesBalanitis Circumscripta Plasmacellularis (Zoon's Balanitis, Plasma Cell Balanitis)Deba P SarmaNo ratings yet
- Acantholytic Acanthoma. M 60, ScrotumDocument8 pagesAcantholytic Acanthoma. M 60, ScrotumDeba P SarmaNo ratings yet
- Xanthogranuloma: Deba P Sarma, MD OmahaDocument9 pagesXanthogranuloma: Deba P Sarma, MD OmahaDeba P SarmaNo ratings yet
- Xanthomatous Synovial Cyst (Xanthomatous Ganglion Cyst), M 74, Left PalmDocument7 pagesXanthomatous Synovial Cyst (Xanthomatous Ganglion Cyst), M 74, Left PalmDeba P SarmaNo ratings yet
- Deba P Sarma's Dermatology Publications1975-2012Document8 pagesDeba P Sarma's Dermatology Publications1975-2012Deba P SarmaNo ratings yet
- DR Sarma's Melanoma Template 2013Document1 pageDR Sarma's Melanoma Template 2013Deba P SarmaNo ratings yet
- Results of Search in Google Scholar On 'Deba P Sarma'Document28 pagesResults of Search in Google Scholar On 'Deba P Sarma'Deba P SarmaNo ratings yet
- Xanthogranuloma: Deba P Sarma, MD OmahaDocument6 pagesXanthogranuloma: Deba P Sarma, MD OmahaDeba P SarmaNo ratings yet
- Xanthogranuloma: Deba P Sarma, MD OmahaDocument7 pagesXanthogranuloma: Deba P Sarma, MD OmahaDeba P SarmaNo ratings yet
- Xanthogranuloma: Deba P Sarma, MD OmahaDocument4 pagesXanthogranuloma: Deba P Sarma, MD OmahaDeba P SarmaNo ratings yet
- Xanthogranuloma, M 30, Right ElbowDocument4 pagesXanthogranuloma, M 30, Right ElbowDeba P SarmaNo ratings yet
- Xanthogranuloma PPT DSDocument9 pagesXanthogranuloma PPT DSDeba P SarmaNo ratings yet
- XanthogranulomaDocument9 pagesXanthogranulomaDeba P SarmaNo ratings yet
- Xanthogranuloma CasesDocument38 pagesXanthogranuloma CasesDeba P SarmaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- J-Garlic in CheeseDocument12 pagesJ-Garlic in CheeseMary GinetaNo ratings yet
- Practical Finite Element Simulations With SOLIDWORKS 2022Document465 pagesPractical Finite Element Simulations With SOLIDWORKS 2022knbgamageNo ratings yet
- 4 Exploring Your Personality Q and Scoring Key (Transaction Analysis)Document3 pages4 Exploring Your Personality Q and Scoring Key (Transaction Analysis)Tarannum Yogesh DobriyalNo ratings yet
- Air Con LouvresDocument1 pageAir Con LouvresChung May LynnNo ratings yet
- Template - Time in ManufacturingDocument2 pagesTemplate - Time in ManufacturingVero RoaNo ratings yet
- Project Report On Discontinuous Puf Panels Using Cyclopentane As A Blowing AgentDocument6 pagesProject Report On Discontinuous Puf Panels Using Cyclopentane As A Blowing AgentEIRI Board of Consultants and PublishersNo ratings yet
- Rhetorical Analysis ArticleDocument6 pagesRhetorical Analysis Articleapi-242472728No ratings yet
- IntuitionDocument10 pagesIntuitionmailsonNo ratings yet
- OsmanabadDocument5 pagesOsmanabadKirankumar MutnaliNo ratings yet
- Jeremy Hughes ReviewDocument5 pagesJeremy Hughes ReviewgracecavNo ratings yet
- Bahasa InggrisDocument8 pagesBahasa InggrisArintaChairaniBanurea33% (3)
- ManuscriptDocument2 pagesManuscriptVanya QuistoNo ratings yet
- Psalms Magick of The Old Testament PDFDocument129 pagesPsalms Magick of The Old Testament PDFirrrs100% (1)
- AD 251 - Equivalent Uniform Moment Factor, M (Italic)Document1 pageAD 251 - Equivalent Uniform Moment Factor, M (Italic)symon ellimacNo ratings yet
- Digital MarketingDocument70 pagesDigital MarketingTarun N. O'Brain Gahlot0% (2)
- Lazo v. Judge TiongDocument9 pagesLazo v. Judge TiongKing BadongNo ratings yet
- Download 12,000 Shed PlansDocument27 pagesDownload 12,000 Shed PlansRadu_IS100% (2)
- Manual de Instruções Iveco Eurocargo Euro 6Document226 pagesManual de Instruções Iveco Eurocargo Euro 6rsp filmes100% (1)
- Rethinking Classification and Localization For Object DetectionDocument13 pagesRethinking Classification and Localization For Object DetectionShah Nawaz KhanNo ratings yet
- EMarketer Time Spent With Media SnapshotDocument13 pagesEMarketer Time Spent With Media SnapshotWei ShingNo ratings yet
- Horizontal Vertical MarketDocument4 pagesHorizontal Vertical MarketVikasNo ratings yet
- Math-149 MatricesDocument26 pagesMath-149 MatricesKurl Vincent GamboaNo ratings yet
- So You Want To Be A NeurosugeonDocument10 pagesSo You Want To Be A NeurosugeonColby TimmNo ratings yet
- Transport in Plants: Test Yourself 9.1 (Page 178)Document3 pagesTransport in Plants: Test Yourself 9.1 (Page 178)lee100% (3)
- Handout CalmAlphaDocument2 pagesHandout CalmAlphaDave SnowdenNo ratings yet
- Detailed Lesson Plan in MAPEH III I. ObjectivesDocument19 pagesDetailed Lesson Plan in MAPEH III I. ObjectivesJenna FriasNo ratings yet
- The Clàsh The 0nly Band That MatteredDocument255 pagesThe Clàsh The 0nly Band That MatteredNikos VaxevanidisNo ratings yet
- Your Results For: "Multiple-Choice Questions: B": DelayDocument4 pagesYour Results For: "Multiple-Choice Questions: B": DelayawairmalikNo ratings yet
- Short Answers Class 9thDocument14 pagesShort Answers Class 9thRizwan AliNo ratings yet
- Arts9 q4 Mod1 Theatricalforms v5Document30 pagesArts9 q4 Mod1 Theatricalforms v5Harold RicafortNo ratings yet