Professional Documents
Culture Documents
AUHS Chapter 19
Uploaded by
Ilyas Bin Mohd YusofOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AUHS Chapter 19
Uploaded by
Ilyas Bin Mohd YusofCopyright:
Available Formats
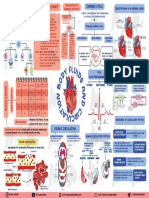
Chapter 21: Cardiovascular Physiology
Blood Flow Purpose of cardiovascular regulation is maintenance of adequate blood flow through capillaries in peripheral tissues and organs Actual volume of blood flowing through a vessel, an organ, or the entire circulation in a given period: Is measured in per min Is equivalent to (CO), considering the entire vascular system Is relatively constant when at rest Varies widely through individual organs, according to immediate needs Is determined by the interplay between (P) and (R) Blood Flow, Blood Pressure, and Resistance Blood flow (F) is proportional to the difference in blood pressure (P) between two points in circulation If P increases, blood flow . If P decreases, blood flow . Blood flow is proportional to resistance (R) If R increases, blood flow . If R decreases, blood flow . is more important than in influencing local blood pressure In summary, Flow (F) = . Resistance Resistance force that opposes blood flow Measure of amount of blood encounters as it passes through vessels Referred to as resistance (PR) The three important sources of resistance are: Blood - thickness of blood Normally stable but disorders that affect change viscosity and thus PR Increase viscosity resistance Total blood vessel . Normally constant but may increase with . Increase vessel length resistance Blood vessel . Most important factor affecting resistance Decrease diameter resistance More blood in contact with walls of vessel Vessel Diameter and Resistance Vessel diameter determines how much blood flows through a tissue or organ decreases resistance, increases blood flow increases resistance, decreases blood flow Relationship between resistance and vessel diameter is expressed as: R= . Fatty plaques from atherosclerosis Cause blood flow Dramatically resistance due to turbulence Velocity of Blood Flow Blood velocity: Changes as it travels through the systemic circulation Is proportional to the cross-sectional area
Slow capillary flow allows adequate time for
between blood and tissues
Flow at Different Points From aorta to capillaries, flow for 3 reasons greater distance, more to flow smaller of arterioles and capillaries farther from heart, total cross sectional area From capillaries to vena cava, flow again Closer to heart, cross sectional area never regains velocity of large arteries Capillary Exchange Only occurs across capillary walls between blood and surrounding tissues 3 routes across endothelial cells clefts through . Mechanisms involved diffusion, transcytosis, filtration and reabsorption Diffusion Most important mechanism -soluble substances steroid hormones, O2 and CO2 diffuse easily Lipid-insoluble substances and must pass through channels, fenestrations or intercellular clefts Large particles , held back Transcytosis transport vesicles across cell . Important for fatty acids, albumin and some hormones (insulin) Filtration and reabsorption Opposing forces : movement of fluid and solutes out of blood blood ( ) pressure drives fluid out of capillary physical force exerted against walls by blood high on end of capillary, low on end : movement of fluid and solutes into blood pressure (COP) draws fluid into capillary results from plasma (albumin) increasing osmolarity of blood net COP = blood COP (BCOP) - intersitial COP (ICOP)
Edema Edema due to build-up of tissue fluid Capillary filtration ( capillary or ) poor return congestive heart failure edema insufficient activity failure (water retention, hypertension) makes capillaries more permeable Capillary reabsorption ( BCOP) - cirrhosis, famine, burns, kidney disease Obstructed drainage Normally drains fluid not reabsorbed by capillaries Consequences of Edema Tissue . oxygen delivery and waste removal impaired Pulmonary edema . edema headaches, nausea, seizures and coma shock excess fluid in tissue spaces causes low blood volume and low BP Tissue Perfusion Refers to blood flow through tissues Factors that affect tissue perfusion include: Regulatory mechanisms used to control perfusion mechanisms mechanisms Autoregulation of Blood Flow Maintains fairly constant blood flow despite BP variation Involves 2 different mechanisms 1. control mechanisms: vascular smooth muscle contracts when stretched & relaxes when not stretched E.g. decreased arterial pressure causes cerebral vessels to dilate & vice versa 2. control mechanism matches blood flow to local tissue needs Low (acidity due to lactic acid) or high CO2 (hypercapnia), or K+ from high , low metabolism cause vasodilation which increases blood flow ( ) Regulation of Blood Flow Endothelium produces several regulators that promote relaxation: (NO) NO is involved in setting resting tone of vessels Levels are by parasympathetic activity Vasodilator drugs such as nitroglycerin or Viagra act thru NO Sympathetic activation causes increased & increased in periphery & viscera Blood flow to muscles is increased arterioles dilate in response to epinephrine Thus blood is shunted viscera & skin to muscles
Hormonal Regulation of Tissue Perfusion hormone released in response to blood volume Increases water retention by kidneys released in response to a in blood pressure Causes . released if BP falls or O2 levels are abnormally low Stimulates production of . peptides released in response to excessive right stretch Causes . Circulatory Pressure Circulatory pressure is divided into three components pressure (BP) pressure, reported in mm Hg Range from about 100 at entrance to aorta to about 35 at start of capillary network pressure (CHP) Pressure within capillary beds (35 mm Hg at start18 at end) pressure Pressure within the venous system ; pressure gradient from venules to right atrium is about .18 mm Hg P across the entire systemic circuit is called the . Averages about 100 mm Hg For circulation to occur, this pressure must be sufficient to overcome resistance of entire cardiovascular system
Blood Pressure Force that blood exerts against a vessel wall Measured at brachial artery of arm pressure: BP during ventricular systole pressure: BP during ventricular diastole Normal value, young adult: < mm Hg Pulse pressure: systolic - diastolic important measure of stress exerted on small arteries Mean arterial pressure (MAP): diastolic pressure + (1/3 of pulse pressure) Perfusion pressure of organs > mmHg adequate to sustain organs Importance of arterial elasticity expansion and recoil maintains steady flow of blood throughout cardiac cycle, smoothes out pressure fluctuations and stress on small arteries BP with age: arteries less distensible BP determined by , blood and . Abnormalities of Blood Pressure . chronic resting BP > 140/90 Consequences: can weaken small arteries and cause . low resting BP < 90/60 caused by , Consequences: Inadequate tissue
, anemia, excessive vasodilation .
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Metabolite Accumulation and Central Fatigue in Working MusclesDocument43 pagesMetabolite Accumulation and Central Fatigue in Working MusclesMuhammad Arslan Aslam100% (1)
- REGULATION OF CARDIAC ACTIVITYDocument1 pageREGULATION OF CARDIAC ACTIVITYservoculus machatteNo ratings yet
- Pathology EssayDocument19 pagesPathology EssayARUNSKNo ratings yet
- Circulatory SystemDocument2 pagesCirculatory SystemDearly Niña OsinsaoNo ratings yet
- Alice in IntensivelandDocument13 pagesAlice in IntensivelandPablo VélezNo ratings yet
- Chapter 2 Blood Circulation & TransportDocument37 pagesChapter 2 Blood Circulation & TransportYanhyNo ratings yet
- O'level Past Papers of Biology, Physics and ChemistryDocument35 pagesO'level Past Papers of Biology, Physics and ChemistryrAJBS;DF100% (1)
- Cambridge International AS & A Level: Biology 9700/12Document20 pagesCambridge International AS & A Level: Biology 9700/12GiftElishaNdawalaNo ratings yet
- AtherosclerosisDocument5 pagesAtherosclerosisJoanne LagusadNo ratings yet
- MCQ Companion To The Eye Basic Sciences in PracticeDocument139 pagesMCQ Companion To The Eye Basic Sciences in PracticeАнагаахын ОрчуулгаNo ratings yet
- Good Thesis Statement For The SwimmerDocument5 pagesGood Thesis Statement For The Swimmermichellemeienburgfortwayne100% (2)
- Basic Cardiovascular Physiology-Pasquale Pagliaro, Raffaella RastaldoDocument438 pagesBasic Cardiovascular Physiology-Pasquale Pagliaro, Raffaella RastaldoJihuhn YuNo ratings yet
- Cardiovascular DiseaseDocument22 pagesCardiovascular DiseaseSunday JamesNo ratings yet
- Circulatory - System - Exam - Ques - 1.rtf BiologyDocument5 pagesCirculatory - System - Exam - Ques - 1.rtf BiologyRekaNo ratings yet
- 36 Critical Illnesses in MalaysiaDocument1 page36 Critical Illnesses in Malaysiawan_andyNo ratings yet
- Cardiovascular System Regulation MechanismsDocument14 pagesCardiovascular System Regulation MechanismsMelisa NovitasariNo ratings yet
- A.p.sowmiya Arun PriyanDocument13 pagesA.p.sowmiya Arun PriyanShadow LeaderNo ratings yet
- Module 11Document7 pagesModule 11Jamille Nympha C. BalasiNo ratings yet
- Science 7Document14 pagesScience 7Agha Khan DurraniNo ratings yet
- Pulmonary CirculationDocument16 pagesPulmonary Circulationsajid_saiyad0% (1)
- Jurnal InternationalDocument9 pagesJurnal InternationalRulix SevenfoldNo ratings yet
- Submitted in Partial Fulfillment of My Nctvet CertificationDocument25 pagesSubmitted in Partial Fulfillment of My Nctvet CertificationJaii100% (1)
- Blood - WikipediaDocument106 pagesBlood - WikipediaZoha AliNo ratings yet
- Acs - Case StudyDocument2 pagesAcs - Case StudyAubrie StellarNo ratings yet
- What Is Light?: Figure 1: Light Always Travels in Straight LineDocument16 pagesWhat Is Light?: Figure 1: Light Always Travels in Straight LineAjitNo ratings yet
- Krvni Sudovi Arterije PDFDocument39 pagesKrvni Sudovi Arterije PDFAlexandra Anna DanilovicNo ratings yet
- Biology notes on movement, respiration and moreDocument59 pagesBiology notes on movement, respiration and moreketamineNo ratings yet
- Fundamentals of Nursing NUR 102: Maintaining Oxygenation Module JDocument24 pagesFundamentals of Nursing NUR 102: Maintaining Oxygenation Module JJenjen CorteyNo ratings yet
- Healthy Bodies Slide3Document11 pagesHealthy Bodies Slide3Larissa RevillaNo ratings yet
- Case Study For Coronary Artery DiseaseDocument8 pagesCase Study For Coronary Artery DiseaseGabbii CincoNo ratings yet