Professional Documents
Culture Documents
Hypertension
Uploaded by
Princess MurilloOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypertension
Uploaded by
Princess MurilloCopyright:
Available Formats
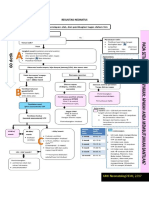
HYPERTENSION The heart pumps blood into the arteries with enough force to push blood to the far
reaches of each organ from the top of the head to the bottom of the feet. Blood pressure can be defined as the pressure of blood on the walls of the arteries as it circulates through the body. Blood pressure is highest as its leaves the heart through the aorta and gradually decreases as it enters smaller and smaller blood vessels (arteries, arterioles, and capillaries). Blood returns in the veins leading to the heart, aided by gravity and muscle contraction.
Hypertension is the medical term for high blood pressure. It is known as the "silent killer" since it has no initial symptoms but can lead to long-term disease and complications.
How is blood pressure measured? Blood pressure is measured with a blood pressure cuff and recorded as two numbers, for example, 120/80 mm Hg (millimeters of mercury). Blood pressure measurements are usually taken at the upper arm over the brachial artery. The top, larger number is called the systolic pressure. This measures the pressure generated when the heart contracts (pumps). It reflects the pressure of the blood against arterial walls. The bottom, smaller number is called the diastolic pressure. This reflects the pressure in the arteries while the heart is filling and resting between heartbeats.
ANATOMY & PHYSIOLOGY
Central Nervous System Medulla Oblongata; relays motor and sensory impulses between other parts of the brain and the spinal cord. Reticular formation (also in pons, midbrain, and diencephalon) functions in consciousness and arousal. Vital centers regulate heartbeat, breathing (together with pons) and blood vessel diameter. Hypothalamus; controls and intergrates activities of the autonomic nervous system and pituitary gland. Regulates emotional and behavioral patterns and circadian rhythms. Controls body temperature and regulates eating and drinking behavior. Helps maintain the waking state and establishes patterns of sleep. Produces the hormones oxytocin and antidiuretic hormone.
Cardiovascular System Baroreceptor, pressure-sensitive sensory receptors, are located in the aorta, internal carotid arteries, and other large arteries in the neck and chest. They send impulses to thecardiovascular center in the medulla oblongata to help regulate
blood pressure. The two most important baroreceptor reflexes are the carotid sinus reflex and the aortic reflex. Chemoreceptors, sensory receptors that monitor the xhemical composition of blood, are located close to the baroreceptors of the carotid sinus and the arch of the aorta in small structures called carotid bodies and aortic bodies, respectively. These chemoreceptors detect changes in blood level of O2, CO2, and H+.
Renal System Renin-Angiotensin-Aldosterone system. When blood volume falls or blood flow to the kidneys decreases, juxtaglomerular cells in the kidneys secrete renin into the bloodstream. In sequence, renin and angiotensin converting enzyme (ACE) act on their substrates to produce the active hormone angiotensin II, which raises blood pressure in two ways. First, angiotensin II is a potent vasoconstrictor; it raises blood pressure by increasing systemic vascular resistance. Second, it stimulates secretion of aldosterone, which increases reabsorption of sodium ions and water by the kidneys. The water reabsorption increases total blood volume, which increases blood pressure. Antidiuretic hormone. ADH is produced by the hypothalamus and released from the posterior pituitary in response to dehydration or decreased blood volume. Among other actions, ADH causes vasoconstriction, which increases blood pressure. Atrial Natriuretic Peptide. Released by cells in the atria of the heart, ANP lowers blood pressure by causing vasodilation and by promoting the loss of salt and water in the urine, which reduces blood volume. Causes In 90% of people with hypertension, the cause of high blood pressure is not known and is referred to as primary or essential hypertension. While the specific cause is unknown, there are risk factors that can contribute to developing high blood pressure.
Factors that can not be changed: Age: The older a person is, the greater the likelihood that he or she will develop high blood pressure, especially elevated systolic readings. This is largely due toarteriosclerosis, or "hardening of the arteries." Race: African Americans develop high blood pressure more often than Caucasians. They develop high blood pressure at a younger age and develop more severe complications sooner in life. Socioeconomic status: High blood pressure is found more commonly among the less educated and lower socioeconomic groups. Residents of the southeastern United States, both Caucasian and African American, are more likely to have high blood pressure than residents of other regions. Family history (heredity): The tendency to have high blood pressure appears to run in families. Gender: Generally men have a greater likelihood of developing high blood pressure than women. This likelihood varies according to age and among various ethnic groups.
Factors that can be changed: Obesity: As body weight increases, the blood pressure rises. Obesity is defined as having a body mass index (BMI) greater than 30 kg/m. A BMI of 25-30 kg/m is considered overweight (BMI=weight in pounds x 703/ height in inches ) Being overweight increases the risk of high blood pressure. Health care practitioners recommend that all obese people with high blood pressure lose weight until they are within 15% of their healthy body weight. Obese people are two to six times more likely to develop high blood pressure than people whose weight is within a healthy range. Not only the degree of obesity is important, but also the manner in which the body accumulates extra fat. Some people gain weight around their belly (central obesity
or "apple-shaped" people), while others store fat around their hips and thighs ("pear-shaped" people). "Apple-shaped" people tend to have greater health risks for high blood pressure than "pear-shaped" people. Sodium (salt) sensitivity: Some people have high sensitivity to sodium (salt), and their blood pressure increases if they use salt. Reducing sodium intake tends to lower their blood pressure. Americans consume 10-15 times more sodium than they need. Fast foods and processed foods contain particularly high amounts of sodium. Many over-the-counter medicines also contain large amounts of sodium. Read food labels and learn about salt content in foods and other products as a healthy first step to reducing salt intake. Fast food restaurants also make the salt and calorie content of their food available to consumers at their restaurants, Alcohol use: Drinking more than one to two drinks of alcohol per day tends to raise blood pressure in those who are sensitive to alcohol. Birth control pills (oral contraceptive use): Some women who take birth control pills develop high blood pressure. Lack of exercise (physical inactivity): A sedentary lifestyle contributes to the development of obesity and high blood pressure. Medications: Certain drugs, such as amphetamines (stimulants), diet pills, and some medications used for cold and allergy symptoms such aspseudoephedrine, tend to raise blood pressure.
Symptoms High blood pressure usually causes no symptoms and high blood pressure often is labeled "the silent killer." People who have high blood pressure typically don't know it until their blood pressure is measured. Sometimes people with markedly elevated blood pressure may develop: headache, dizziness,
blurred vision, nausea and vomiting, and chest pain and shortness of breath.
People often do not seek medical care until they have symptoms arising from the organ damage caused by chronic (ongoing, long-term) high blood pressure. The following types of organ damage are commonly seen in chronic high blood pressure: Heart attack Heart failure Stroke or transient ischemic attack (TIA) Kidney failure Eye damage with progressive vision loss Peripheral arterial disease causing leg pain with walking (claudication) Outpouchings of the aorta, called aneurysms About 1% of people with high blood pressure do not seek medical care until the high blood pressure is very severe, a condition known as malignant hypertension. In malignant hypertension, the diastolic blood pressure (the lower number) often exceeds 140 mm Hg. Malignant hypertension may be associated with headache, lightheadedness, nausea, vomiting, and stroke like symptoms Malignant hypertension requires emergency intervention and lowering of blood pressure to prevent brain hemorrhage or stroke. It is of utmost importance to realize that high blood pressure can be unrecognized for years, causing no symptoms but causing progressive damage to the heart, other organs, and blood vessels. Diagnosis Blood pressure is measured with a blood pressure cuff (sphygmomanometer). This may be done using a stethoscope and a cuff and gauge or by an automatic machine. It is a routine part of the physical examination and one of the vital signs often recorded for a patient visit. Other vital signs include pulse rate, respiratory rate (breathing rate), temperature, and weight.
When discussing blood pressure issues, the health care practitioner may ask questions about past medical history, family history, and medication use, including prescriptions, over-the-counter medications, herbal remedies, and food additives. Other questions may include lifestyle habits, including activity levels,smoking, alcohol consumption, and illegal drug use. Physical examination may include listening to the heart and lungs, feeling for pulse in the wrist and ankles, and feeling and listening to the abdomen looking for signs of an enlarged aorta. Eye examination with an ophthalmoscope may be helpful by looking at the small blood vessels on the retina in the back of the eyeball. Normal Blood Pressure Systolic less than 120 mm Hg; diastolic less than 80 mm Hg Prehypertension Systolic 120-139 or diastolic 80-89 mm Hg High Blood Pressure Stage 1: Systolic 140-159; diastolic 90-99 mm Hg Stage 2: Systolic more than 160; diastolic more than 100 mm Hg Blood tests may be considered to assess risk factors for heart disease and stroke as well as looking for complications of hypertension. These include complete blood count (CBC), electrolytes, BUN (blood urea nitrogen), and creatinine and GFR (glomerular filtration rate) to measure kidney function. A fasting lipid profile will measure cholesterol and triglyceride levels in the blood. If appropriate, blood tests may be considered to look for an underlying cause of high blood pressure includingabnormal thyroid or adrenal gland function. Ultrasound of the kidneys, CT scan of the abdomen, or both may be done to assess damage or enlargement of the kidneys and adrenal glands. Other studies may be considered depending upon the individual patient's needs
Electrocardiogram (ECG) may help evaluate heart rate and rhythm. It is a screening test to help assess heart muscle thickness. If hypertension is longstanding, the heart muscle has to hypertrophy, or get larger, to push blood against the increased pressure within the arteries of the body. Echocardiogram is an ultrasound examination of the heart It is used to evaluate the anatomy and the function of the heart. A cardiologist is required to interpret this test and can evaluate the heart muscle and determine how thick it is, whether it moves appropriately, and how efficiently it can push blood out to the rest of the body. The echocardiogram can also assess heart valves, looking for narrowing (stenosis) and leaking (insufficiency or regurgitation). A chest X-ray may be used as a screening test to look for heart size, the shape of the aorta, and to assess the lungs. Doppler ultrasound is used to check blood flow through arteries at pulse points in your arms, legs, hands, and feet. This is an accurate way to detectperipheral vascular disease, which can be associated with high blood pressure. It also can measure blood flow in the arteries to both kidneys and sometimes depicts narrowings that can lead to high blood pressure in a minority of patients.
Treatment Blood pressure control is a lifelong challenge. Hypertension can progress through the years, and treatments that worked earlier in life may need to be adjusted over time. Blood pressure control may involve a stepwise approach beginning with diet, weight loss, and lifestyle changes and eventually adding medications as required. In some situations, medications may be recommended immediately. As with many diseases, the health care practitioner and patient work together as a team to find the treatment plan that will work for that specific individual.
Medical Treatment In about half of people with high blood pressure, limiting sodium intake by eliminating table salt, cooking salt, and salty and processed foods can reduce blood pressure by 5 mm Hg. Losing weight and participating in regular physical activity can reduce blood pressure further. If these lifestyle changes and choices don't work, medications should be added. The medications have been proven to reduce the risk of stroke, heart disease, and kidney problems. Do not stop taking your medications without talking to your health care practitioner.
Medications It may take trial and error to find the proper medication or combination of medications that will help control hypertension in each case. It is important to take the medications as prescribed and only discontinue them on the advice of your health care practitioner.
Water Pills (diuretics) Diuretics are used very widely to control mildly high blood pressure, and are often used in combination with other medications. They increase sodium excretion and urine output and decrease blood volume. The sensitivity to the effect of other hormones in your body is decreased. One example of a diuretic is hydrochlorothiazide (HydroDIURIL) The most commonly used diuretics to treat hypertension include: hydrochlorothiazide (HydroDIURIL), the loop diuretics furosemide (Lasix) and torsemide (Demadex), the combination of triamterene and hydrochlorothiazide (Dyazide), and metolazone (Zaroxolyn).
Beta-Blockers Beta-blockers reduce heart rate and decrease the force of heart contraction by blocking the action of adrenaline receptors. Beta blockers are widely prescribed and effective but can cause increased fatigue and decreased exercise tolerance because they prevent an increased heart rate as a normal response to physical activity. They are also prescribed for people who have associated heart disease,angina, or history of a heart attack. Examples of beta blockers include, carvedilol (Coreg), metoprolol (Lopressor),atenolol (Tenormin) Calcium Channel Blockers (CCBs) Calcium channel blocking agents work by relaxing the muscle in artery walls and by therefore reducing the force of contraction of heart muscle. Example of calcium channel blockers include, nifedipine (Procardia), diltiazem(Cardizem), verapamil (Isoptin, Calan), nicardipine (Cardene), amlodipine(Norvasc), and felodipine (Plendil) Angiotensin-Converting Enzyme (ACE) Inhibitors ACE inhibitors stop the production in the body of a chemical called angiotensin II, which causes blood vessels to contract. Narrower blood vessels are associated with increased blood pressure. Relaxing artery walls leads to lower blood pressure. Examples of ACE inhibitors include Captopril (Capoten), enalapril (Vasotec),lisinopril (Zestril, Prinivil), quinapril (Accupril), and fosinopril (Monopril) Angiotensin Receptor Blockers (ARBs)
ARBs work block angiotensin II receptors and prevent vasoconstriction, or narrowing of blood vessels. Examples of ARBs include losartan (Cozaar), valsartan (Diovan), candesartan(Atacand), and irbesartan (Avapro) Blockers of Central Sympathetic (autonomic nervous) System These agents block messages from the brain's autonomic nervous system that contract blood vessels. The autonomic nervous system is the part of the unconscious nervous system of the body that controls heart rate, breathing rate, and other basic functions. These medications relax blood vessels, thus lowering blood pressure. An example is clonidine (Catapres)
Direct Vasodilators Direct vasodilators relax (dilate) the blood vessels to allow blood to flow under lower pressure. These medications are most often used in times of hypertensive crisis and are injected intravenously to quickly lower blood pressure readings. Examples include nitroprusside (Nitropress), and diazoxide (Hyperstat).
Prevention High blood pressure may be prevented by living a healthy lifestyle, including some of the following: eating a nutritious, low-fat diet; exercising regularly;
decreasing salt (sodium) intake, read food labels so you know the salt content before you buy a product in the grocery store or eating a meal at a fast food restaurant, and avoid adding salt to foods;
maintain a healthy weight and if you are overweight or obese, try to lose weight; drink alcohol in moderation; stop smoking; get routine health assessments and blood pressure screening; taking your blood pressure medications as directed, even if you're feeling fine; and reduce stress and practice relaxation techniques, physical activity will help with this.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Teknik Operasi Splenektomi 2Document31 pagesTeknik Operasi Splenektomi 2sphericalfaNo ratings yet
- Les or Not Les Indice de Prediccion 758.fullDocument54 pagesLes or Not Les Indice de Prediccion 758.fullFranco PacelloNo ratings yet
- Pulsion Work Booklet: Bucarest Hemodynamic Monitoring WorkshopDocument43 pagesPulsion Work Booklet: Bucarest Hemodynamic Monitoring WorkshopghuoiNo ratings yet
- Nursing NotesDocument6 pagesNursing NotesTiffany SimnickNo ratings yet
- Arlevert (Cinnarizinedimenhydrinate)Document2 pagesArlevert (Cinnarizinedimenhydrinate)zloncar3No ratings yet
- NRSG1025 Fundamental Healing Arts Lab Manual Learner Prep Workbook - FALL 2023 WINTER 2024Document88 pagesNRSG1025 Fundamental Healing Arts Lab Manual Learner Prep Workbook - FALL 2023 WINTER 2024pham vanNo ratings yet
- ANEXA Nr. 9 Certificat Medical Medical Fitness CertificateDocument1 pageANEXA Nr. 9 Certificat Medical Medical Fitness CertificatePrisacaru MarianNo ratings yet
- 4.1 Fixator Extern Circular IlizarovDocument10 pages4.1 Fixator Extern Circular IlizarovTudorica AdrianNo ratings yet
- Chart Medical Eligibility Contraceptives EnglishDocument1 pageChart Medical Eligibility Contraceptives EnglishTiang Soon TeckNo ratings yet
- Effect of Periodontal Therapy On C-Reactive Protein Levels in Gingival Crevicular Fluid of Patients With Gingivitis and Chronic PeriodontitisDocument5 pagesEffect of Periodontal Therapy On C-Reactive Protein Levels in Gingival Crevicular Fluid of Patients With Gingivitis and Chronic PeriodontitisKanagavalli VijayakumarNo ratings yet
- Resusitasi NeonatusDocument7 pagesResusitasi NeonatusIqbal Miftahul HudaNo ratings yet
- Philippine College of Science and Technology College of NursingDocument21 pagesPhilippine College of Science and Technology College of NursingAijem RyanNo ratings yet
- Prame HaDocument49 pagesPrame HaRajith FernandoNo ratings yet
- 14th Century - Black DeathDocument16 pages14th Century - Black DeathJean-pierre NegreNo ratings yet
- Evaluation Entomological WarfareDocument62 pagesEvaluation Entomological WarfareReid Kirby100% (1)
- TextbookOfEpilepsySurgery 1steditionDocument1,624 pagesTextbookOfEpilepsySurgery 1steditionDaniela Ene100% (1)
- Makalah Leigh Disease by Boys KDocument6 pagesMakalah Leigh Disease by Boys KAzizul HakimNo ratings yet
- Diagnostic Challenges and Uncertainties of Embolic Strokes of UndeterminedDocument4 pagesDiagnostic Challenges and Uncertainties of Embolic Strokes of UndeterminedDarliana Ospina DuarteNo ratings yet
- The New Microbiology - From Microbiomes To CRISPRDocument205 pagesThe New Microbiology - From Microbiomes To CRISPRalery ahreallyNo ratings yet
- YS Curodont Sell Sheet - 8.5x11 - FINAL 1Document1 pageYS Curodont Sell Sheet - 8.5x11 - FINAL 1lucian hahaianuNo ratings yet
- Konsep Wound ManajemenDocument24 pagesKonsep Wound ManajemenNiken DewiNo ratings yet
- Hirschsprung's Disease, PDFDocument1 pageHirschsprung's Disease, PDFMr. LNo ratings yet
- Acute Complications of Diabetes Mellitus: Hypoglycemia and Hypoglycemic ComaDocument30 pagesAcute Complications of Diabetes Mellitus: Hypoglycemia and Hypoglycemic ComaCristinaGheorgheNo ratings yet
- What Is-Thrombocythemia and ThrombocytosisDocument4 pagesWhat Is-Thrombocythemia and ThrombocytosisFred C. MirandaNo ratings yet
- Antenatal Care Services: by DR - Chinedu Ibeh Thursday, 16 APRIL 2015Document81 pagesAntenatal Care Services: by DR - Chinedu Ibeh Thursday, 16 APRIL 2015SehaRizaNo ratings yet
- Dade InnovinDocument7 pagesDade InnovinchaiNo ratings yet
- Khushboo PPT Covid 19Document17 pagesKhushboo PPT Covid 19Birlal SinghNo ratings yet
- Canine Influenza FactsDocument5 pagesCanine Influenza FactsWIS Digital News StaffNo ratings yet
- Needle CricothyroidotomyDocument9 pagesNeedle Cricothyroidotomyhatem alsrour100% (2)
- ANC ModuleDocument103 pagesANC ModulePreeti ChouhanNo ratings yet