Professional Documents
Culture Documents
Anemia
Uploaded by
Mila Canoza HerreraOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anemia
Uploaded by
Mila Canoza HerreraCopyright:
Available Formats
INTRODUCTION
Anemia is a clinical condition that results from an insufficient supply of healthy red blood cells (RBCs), erythrocytes, to oxygenate the bodys tissue adequately; hypoxia results. The anemias are classified by either the etiology or the morphology of the specific anemia. It is caused in one of the three ways: 1) decrease production of healthy RBCs, 2) increase RBC destruction (hemolysis), or 3) loss of blood. The production of RBCs, erythropoiesis, takesplace in the bone marrow. The requirements for healthy RBCs include precursor cells, reticulocytes, and adequate supplies of iron, vitamin B12, folic acid, protein, pyridoxine, and traces of copper. If any of these factors is missing, the RBCs will be fragile, misshapen, of abnormal size, lacking hemoglobin, or too few. Increase destruction of RBCs can be due to extrinsic causes such as physical trauma while intrinsic causes may include defective hemoglobin. Anemia may also be due to acute blood loss, most commonly seen in trauma or vessel rupture. Morphologic classification is based on erythrocyte size, shape, and color. Morphologic categories include 1. normocytic/normochromic (normal size and color), 2. macrocytic/normochomic (large size, normal color), and 3. microcytic/hypochomic (small size, pale color). TYPES A. ANEMIA CAUSED BY DECREASED ERYTHROCYTE PRODUCTION Decrease production may be due to (1) decrease synthesis of normal hemoglobin, as seen in iron deficiency anemia and thalassemia; (2) defective DNA synthesis, as seen in megaloblastic anemia resulting from cobalamin (vitamin B12) and folate deficiency; or (3) reduced availability of erythrocyte precursors as seen in aplastic anemia.
1. Iron Deficiency Anemia (IDA) is a chronic, hypochromic, microcytic
anemiaresulting from an insufficient supply of iron in the body. Without iron, hemoglobin concentration in the RBCs is reduced and the cells are unable to oxygenate the bodys tissues adequately, resulting in anemia. Major risk factors for IDA include (1) insufficient dietary intake of iron, (2) blood loss, (3) impaired absorption of iron, and (4) excessive demands for RBC production as a result of hemolyis.
2. Thalassemia is a group of genetic disorders that result in inadequate
normal Hb production. Whereas IDA affects heme synthesis, thalassemia disrupts the synthesis of globin. These disorders include alphathalassemia, a relatively benign and asymptomatic condition; beta-
thalassemia minor, a mild to moderate form of microcytic anemia; and beta-thalassemia major, a severe, microcytic, hypochromic anemia that may be fatal. These disorders also cause hemolysis. All are chronic conditions.
3. MegaloblasticAnemiasare a group of disorders caused by impaired DNA
synthesis resulting in defective RBCs. These anemia share the morphology of megaloblasts (large, abnormal, and premature RBCs) in the blood and bone marrow. They are caused by deficiencies of cobalamin (vitamin B12) and folic acid.
a. Cobalamin (vitamin B12) Deficiency/ Pernicous Anemiais an
autoimmune disorder characterized by the absence of intrinsic factor (IF) in gastric secretions, leading to malabsorption of cobalamin (vitamin B12).
b. Folic Acid Deficiency Anemia. Inadequate amounts of folate in the
diet is the usual cause of folate deficiency, with the disorder developing most often in the poor, pregnant women, and in chronic alcoholics. Because folatehelps in the synthesis of DNA, a folate deficiency results in fewer cell divisions and, therefore, decrease red blood cell production. A deficiency in folate during pregnancy is also associated with birth disorders call neural tube defects, such as spina bifida.
4. Aplastic Anemia is caused by failure of the bone marrow, leading to
insufficient production of peripheral blood elements. The marrow failure is due to primary defects in, or damage to, the stem cell or marrow microenvironment. Aplastic anemia may be either hereditary or acquired.
B. ANEMIA CAUSED BY INCREASE ERYTHROCYTE DESTRUCTION
1. Hemolytic Anemia is an end result of many conditions that lead to
hemolysis. Hemolysis, the premature destruction of erythrocytes, can result from physical damage, intrinsic membrane defects, abnormal Hb, erythrocytic enzymatic defects, immune destruction of RBCs by macrophages, or hypersplenism. Anemia occurs when the bone marrow fails to replace RBCs at the rate they are destroyed.
2. Sickle Cell Anemia. Sickle cell disease (SCD) is a group of inherited
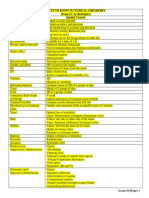
disordes of mutant hemoglobin (HbS) that causes the characteristic sickling of RBCs. Sickling occurs only under conditions of low oxygenation. The abnormally shaped RBCs become trapped in capillaries, causing organ damage from infarcts and tissue hypoxia, or are damage in transit, leading to severe anemia. TYPE OF ANEMIA A. ANEMIA CAUSED BY DECREASED ERYTHROCYTE PRODUCTION Iron Deficiency Anemia CAUSATIVE FACTORS (1) Insufficient dietary intake of iron - Malnutrition, Economic constraints, poor dentition, poor appetite Excellent Source of Iron: Almonds, asparagus, beans, carrots, cauliflower, celery, liver, egg yolk, soybeans (2) Blood loss - GI tract (most common site) bleeding, most common in men; Accidents 3) Impaired absorption of iron - Diarrhea, celiac disease, gastrectomy, tannates (in tea and coffee), carbonates, antacid magnesium trisilicate, eating clay and starch. (4) Excessive demands for RBC production as a result of hemolyis (1) Genetically - Mediterranean, African, Southeast Asia origin Those who inherit alpha-genes have alpha thalassemia. Those who inherit one betagene have thalassemia minor; two beta-genes have thalassemia major. (1) Insufficient dietary intake: Rare with cobalamin but common with folate. (2) Drugs that impede absorption in the stomach - Purine analogs (azathioprine), pyrimidine analogs (5-FU), ribonnucleotidereductase inhibitors (hydroxyurea), anticonvulsants (phenytoin), and oral contraceptives. (3) Drugs that impair SIGNS AND SYMPTOMS - Fatigue, weakness - Shortness of breath - Pallor (earlobes, face, palms and mouth, nail bed, conjunctiva) - Brittle spoon-like nails - Cheilosis (sore at the corners of the mouth) - Cheilitis (inflammation of the lips) - Smooth and sore tongue, Glossitis (inflammation of the tongue) - Dizziness - Pica (clay or starch) Angular stomatitis (inflammation of the mucosa of the mouth)
Thalassemia
Pain Failure to thrive Frequent infections Diarrhea Splenomegaly Hepatomegaly Jaundice Bone marrow hyperplasia
Megaloblastic Anemia
a. Cobalamin (vitamin B12)
Deficiency/ Pernicous Anemia Pallor, slight jaundice with a complaint of weakness Smooth, sore, beefy red tongue (glossitis) Diarrhea Paresthesia (altered sensation such as numbness or tingling in the extremeties)
a. Cobalamin
(vitamin B12) Deficiency/ Pernicous Anemia b. Folic Acid Deficiency Anemia
uptake in the ileum Nitrous oxide, cholestyramine, para-aminosalicylic acid, neomycin, metformin, phenformin, and colchicine (4) Genetic Disorders Imerslund-Grasbeck syndrome (defects in the ileal receptors of IF), hereditary trascobalamin II (TCII) deficiency (5) Impaired absorption resulting from medications, neoplasms, GI diseases, or surgical resection of the terminal ileum. (6) GI disorders Gastric atrophy, geastrectomy, gastric stapling, bypass for pancreatic insufficiency of protease, which release Cbl from r binders so Cbl can bing with IF (7) Zollinger-Ellison Syndrome
Aplastic Anemia -
(1) Hereditary Fanconi syndrome, dyskeratosis congenital, Shwachman-Diammond syndrome, Pearson syndrome, Diamond-blackfan syndrome, Amegakaryocytic thrombocytopenia (absent radius [TAR] syndrome) (2) Acquired High-dose radiation and chemotherapy drugs (e.g., antimetabolites, alkylating agents) Toxic chemicals: hair and aniline dyes, herbicides and insecticides, benzene and its derivatives (gasoline, mothballs, paint and varnish removers, dye-cleaning solutions and household cleaners) Certain drugs: chloramphenicol,
Impaired proprioception (difficulty identifying ones position in space, which may progress to difficulty with balance) - Fair-haired or prematurely gray - GI : weight loss, appetite loss, nausea, vomiting, abdominal distension, diarrhea - Neurologic disorder: Paresthesia (altered sensation such as numbness or tingling in the extremeties), poor gate, memory loss, cognitive problems, depression b. Folic Acid Deficiency Anemia - Pallor, progressive weakness, fatigue - Shortness of breath, cardiac palpitations - Glossitis, Cheilosis - GI: same as in Pernicous Anemia - Neurological symptoms in Vitamin B12 deficiency are not seen in folic acid deficiency - Fatigue, weakness, headache - Dyspnea, rapid heart rate - Pallor - Frequent infections - Unexplained bruising, easy bruising - Nosebleeds, bleeding gums - Heavy menses - Blood in the stool - Prolonged bleeding from cuts - Skin rash - Bone pain - Foot swelling - Fever
B. ANEMIA CAUSED BY INCREASE ERYTHROCYTE DESTRUCTION Hemolytic Anemia
sulfonamides, quinacrine, phenylbutazone, anticonvulsants (Phenytoin and Mephenytoin), gold compounds, streptomycin, tripenelamine, meprobamate, carbon tetrachloride, arsenic. - Autoimmune disorders such as systemic lupus eryhtematosus - Infectious agents: hepatitis, Epstein-Barr virus, human immunodeficiency virus, parvovirus, military tuberculosis, and mycobacterial infections - Diseases of the bone marrow: leukemia, graft-versus-host disease. Eosinophilic fasciitis, and fulminant hepatitis - Preganacy (rare like autoimmune) - Idiopathic (an environmental etiology is rarely identified) Hemolysis can result from: (1) Hereditary disorders - Intracorpuscular defects (G-6PD) (2) Acquired Hemolytic condition - Immune reactions - Toxic chemicals: arsenic, lead copper, and certain snake venoms - Drugs: penicillin, ampicillin, cephalothin, methicillin, phenylbutazone, phenacetin, quinine, quinidine, and L-dopa - Parasitic disease that disruots RBC membrane (malaria, Clostridium welchii) - Physical damage to the RBC membrane: hemodialysis, heart-lung machines and prosthetic cardiac valves
The client with hemolytic anemia may suffer all the general manifestations of anemia. Pallor, severe fatigue, malaise, weakness, lightheadedness Fever Exertional dyspnea Headache Vertigo Sensitivity to cold Weight loss Glossitis Cheilosis Cheilitis Paresthesias Confusion Loss of balance Mental depression Dry skin, brittle nails, spoon-shaped concave nails Pallor Jaundice Fatigue Irritability Large joints and surrounding tissue may become swollen during crisis
Sickle Cell Anemia
(1) Genetically Areas of the world where malaria is endemic: Africa, Mediterranean, Middle East, India
Priapism (abdominal, painful continuous erection of the penis) may occur if the penile vein are obstructed Pain
POSSIBLE COMPLICATIONS
Anemia diminishes the capability of individuals who are affected to perform physical labor. This is a result of one's muscles being forced to depend on anaerobic metabolism. The lack of iron associated with anemia can cause many complications, including hypoxemia, brittle or rigid fingernails, cold intolerance, impaired immune functioning, and possible behavioral disturbances in children. Hypoxemia resulting from anemia can worsen the cardio-pulmonary status of patients with pre-existing chronic pulmonary disease. Brittle or rigid fingernails may be a result of abnormal thinness of nails due to insufficient iron supply. Cold intolerance occurs in one in five patients with iron deficiency anemia, and becomes visible through numbness and tingling. Impaired immune functioning leading to increased likelihood of sickness is another possible complication. Finally, chronic anemia may result in behavioral disturbances in children as a direct result of impaired neurological development in infants, and reduced scholastic performance in children of school age. Behavioral disturbances may even surface as an attention deficit disorder.
DIAGNOSIS Procedures: 1. Complete Blood Count (CBC)is a series of tests used to evaluate the composition and concentration of the cellular components of blood. It measures the following: The number of red blood cells (RBCs) The number of white blood cells (WBCs) The total amount of hemoglobin in the blood The fraction of the blood composed of red blood cells (hematocrit) The mean corpuscular volume (MCV) the size of the red blood cells CBC also includes information about the red blood cells that is calculated from the other measurements: MCH (mean corpuscular hemoglobin) - the average mass of hemoglobin per red blood cell in a sample of blood. MCHC (mean corpuscular hemoglobin concentration) - the average mass of hemoglobin per red blood cell in a sample of blood. The platelet count is also usually included in the CBC.
Nursing Responsibilities: (1) Apply pressure on the venipuncture site after obtaining a sample (done by RMT). (2) Observe for bleeding. (3) Explain the purpose of the procedure. (4) Secure laboratory request prior to examination. 2. Bone Marrow Aspiration is the withdrawal of specimen of bone marrow. The sites are posterior superior iliac crest fro adults and proximal tibia for children. Nursing Responsibilities: (1) Secure consent. (2) Inform the client that the procedure may cause discomfort and pain. (3) Position the client in a prone or lateral position. (4) Monitor and maintain pressure dressing over punctured site for 10 minutes. (5) Assess for discomfort. (6) Administer prescribed pain meds.
3. Peripheral Blood Smear is a blood test that gives information about the
number and shape of blood cells.
4. Schillings Test is a urine test done to evaluate whether vitamin B12 is being absorbed by the body.
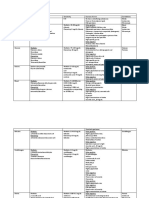
Nursing Responsibilities: (1) Instruct the patient to fast, may drink water, before starting the test, then eat normally for the next 24 hours. (2) You may ask the client to stop taking any medications for it may affect the test. (3) Instruct the client to have not undergone any parenteral (intramuscular injection) of vitamin B12 3 days prior to the test. (4) Instruct the client to wash their genital/perineal thoroughly with clean water and wipe with clean towel before obtaining urine sample. 5. Amniocentesis is the aspiration of amniotic fluid from the uterus. It is done at 14 to 16 weeks of pregnancy. Expected Outcomes: Iron deficien cy RBC count Hb/HcT RBC morpholo gy Reticuloc yte Platelets MCV MCH MCHC Serum Iron Mic/H N or N or + Thalasse mia N to - (beta trait +) Mic/H Cobalami n B12 Mac/N + - to N + - With malFolic acid Deficien cy Mac/N + - to N + Aplasti c Anemi a N/N N N N Hemoly tic Anemia N/N + Sickle Cell Anemia Sickle cells + +
+ +
N or +
absoption TIBC Serum Ferritin Bilirubin Marrow Aspirate + N or Absence of hemosiderin + + Megaloblasts Megaloblasts Aplastic : remaining cells normal -WBC N to + - Indirec t bilirubin N or +
Others
-Transferrin saturatio n
Hb electrophoresis, Amniocentesis
-Serum vit. B12 + Schilling
-Serum Folate
-Folate
+Hb S, Hb electrophoresis, -Haptoglobin, + Fibrinogen , + Urobilinogen, + Stercobilinogen, Amniocentesis
+ Increase or positive; - decrease or negative; Hb hemoglobin; HcT hematocrit; Hb S sickle hemoglobin; Mac/N macrocytic/normochromic; MCV mean corpuscular volume; MCH mean corpuscular hemoglobin; MCHC mean corpuscular hemoglobin concentration; Mic/H microcytic/hypochromic; N normal; N/N normocytic/normochromic; RBC red blood cell; TIBC total iron-binding capacity; WBC white blood cell
MEDICATION and THERAPY 1. Oxygen Therapy Oxygen therapy may be prescribed for clients with severe anemia because their blood has a reduced capacity for oxygen. Oxygen helps to prevent tissue hypoxia and lessen the workload of the heart as it struggles to compensate for the lower Hb levels. 2. Eryhtropoietin Subcutaneous injections of erythropoietin can be given to treat anemias of chronic disease because this drug increases the production of RBCs. For this drug to be effective, the client must have bone marrow capable of producing RBCs and sufficient nutrients for the production of RBCs. 3. Iron Replacement
Iron can be given to augment oral intake in cases where the need for iron is immediate or the demands are beyond dietary measures. The oral form of iron should used because it is inexpensive and convenient. It is usually given for mild forms of anemia. 4. Blood Transfusion Blood transfusions are valuable in treating anemia resulting from acute blood loss. It may also befit clients with severe chronic anemia (Hb<6 g/dL) who have responded poorly to other forms of therapy. Packed RBCs may be given to clients who have lost blood in surgery or due to trauma.
You might also like
- CBCDocument12 pagesCBCDaNa Al-jomah100% (1)
- Immunology and Serology ReviewDocument30 pagesImmunology and Serology ReviewEuliz G.100% (1)
- Bacte Day 2Document24 pagesBacte Day 2Jadey InfanteNo ratings yet
- Compatibility Testing - BloodDocument5 pagesCompatibility Testing - BloodMunish DograNo ratings yet
- Serologic Tests Part 1Document4 pagesSerologic Tests Part 1Joshua TrinidadNo ratings yet
- Aub F Urine Screening For Metabolic DisordersDocument4 pagesAub F Urine Screening For Metabolic DisordersRomie SolacitoNo ratings yet
- MedtechDocument7 pagesMedtechLyudmyla GillegoNo ratings yet
- Analysis of Physical Properties of UrineDocument2 pagesAnalysis of Physical Properties of UrineameerabestNo ratings yet
- Chapter Blood: RBC Platelet HemostasisDocument89 pagesChapter Blood: RBC Platelet Hemostasisapi-19916399100% (1)
- MUST To KNOW in Clinical ChemistryDocument53 pagesMUST To KNOW in Clinical ChemistryTristan Jay CalabiaNo ratings yet
- Red Blood Cell Anomalies: Elliptocytes & Oval MacrocyteDocument12 pagesRed Blood Cell Anomalies: Elliptocytes & Oval MacrocyteSHUPATUSSAI100% (1)
- Abnormal Urine Color and ClarityDocument4 pagesAbnormal Urine Color and ClarityJulie Anne Soro ValdezNo ratings yet
- Summary of Reagent Strip TestsDocument8 pagesSummary of Reagent Strip TestsDarla YsavelNo ratings yet
- COMPLETE BLOOD COUNT Lecture GuideDocument9 pagesCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaNo ratings yet
- SubcutaneousDocument2 pagesSubcutaneousMary ChristelleNo ratings yet
- HEMOSTASIS Coagulation PathwayDocument3 pagesHEMOSTASIS Coagulation PathwayGianna SablanNo ratings yet
- Clin Chem CompiledDocument9 pagesClin Chem CompiledReg LagartejaNo ratings yet
- Microscopic Examination of UrineDocument4 pagesMicroscopic Examination of UrineGlaiza Erika Baes GudaNo ratings yet
- Chapter 1: Introduction To Urinalysis: Urine CompositionDocument74 pagesChapter 1: Introduction To Urinalysis: Urine CompositionMegumi TadokoroNo ratings yet
- MedTech Licensure Exam ChecklistDocument3 pagesMedTech Licensure Exam ChecklistVianney Angeli LorenzanaNo ratings yet
- Bacte TestDocument10 pagesBacte TestRiondalionNo ratings yet
- Hematology: Dr. I. Quirt Adriana Cipolletti, Jeremy Gilbert and Susy Hota, Chapter Editors Leora Horn, Associate EditorDocument42 pagesHematology: Dr. I. Quirt Adriana Cipolletti, Jeremy Gilbert and Susy Hota, Chapter Editors Leora Horn, Associate EditorRubyrose Tagum100% (1)
- Recall 1Document4 pagesRecall 1pikachuNo ratings yet
- Top 20 Blood Banking ConceptsDocument16 pagesTop 20 Blood Banking ConceptsM CNo ratings yet
- MICROBIOLOGY MEDIADocument3 pagesMICROBIOLOGY MEDIAAisle Malibiran PalerNo ratings yet
- Evacuated Tube SystemDocument2 pagesEvacuated Tube SystemAaron James RuedasNo ratings yet
- Clinical MicrosDocument28 pagesClinical MicrosKristine Jamella Maris NaragNo ratings yet
- Clinical Chemistry IDocument8 pagesClinical Chemistry IMariel AbatayoNo ratings yet
- Immuno SeroDocument80 pagesImmuno SeroDocAxi Maximo Jr AxibalNo ratings yet
- 2.13.08 Cold Agglutinin RogersDocument27 pages2.13.08 Cold Agglutinin RogersJessica StewartNo ratings yet
- Clinical Chemistry 2 Lecture Notes in Trace ElementsDocument6 pagesClinical Chemistry 2 Lecture Notes in Trace ElementsMoira Pauline LibroraniaNo ratings yet
- Wintrobe Test PDFDocument9 pagesWintrobe Test PDFMaria Chacón CarbajalNo ratings yet
- Test Bank Exam 3Document81 pagesTest Bank Exam 3Sajjad AhmadNo ratings yet
- Clinical Microscopy Safety and Urine AnalysisDocument26 pagesClinical Microscopy Safety and Urine AnalysisDarla YsavelNo ratings yet
- Bacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitDocument3 pagesBacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitJoshua TrinidadNo ratings yet
- Photo Me TryDocument3 pagesPhoto Me TrylcrujidoNo ratings yet
- Diagnostic Microbiology - : University of Santo Tomas - Medical TechnologyDocument6 pagesDiagnostic Microbiology - : University of Santo Tomas - Medical TechnologyWynlor AbarcaNo ratings yet
- Staphylococcus Spp. Gram Positive. ClusteredDocument15 pagesStaphylococcus Spp. Gram Positive. ClusteredIvy NNo ratings yet
- Coagulation NotesDocument14 pagesCoagulation NotesthrowawyNo ratings yet
- RBC and WBC Abnormalities in Blood SmearsDocument38 pagesRBC and WBC Abnormalities in Blood SmearsTorillo KimNo ratings yet
- M6 Histopath ImpregantionAndEmbeddingDocument4 pagesM6 Histopath ImpregantionAndEmbeddingninaNo ratings yet
- Basic Haematology Exercise 1 (MKEB2403)Document10 pagesBasic Haematology Exercise 1 (MKEB2403)kiedd_04100% (8)
- Synovial FluidDocument8 pagesSynovial FluidMary ChristelleNo ratings yet
- Clinial MicrosDocument53 pagesClinial MicrosDreyden HaloNo ratings yet
- A. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)Document19 pagesA. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)IceNo ratings yet
- Histopathology Staining Techniques GuideDocument2 pagesHistopathology Staining Techniques GuideRoma Ann ManahanNo ratings yet
- Introduction to Pathology and Disease MechanismsDocument17 pagesIntroduction to Pathology and Disease MechanismsAngela ReyesNo ratings yet
- Review in Microbiology Part 1Document30 pagesReview in Microbiology Part 1sini gangNo ratings yet
- Aubf Outline EditedDocument16 pagesAubf Outline EditedNoraine Princess TabangcoraNo ratings yet
- Aubf Case Study AbcdefDocument9 pagesAubf Case Study AbcdefChiara Kate CodillaNo ratings yet
- HemaDocument59 pagesHemaSteph VeeNo ratings yet
- (MT6317) Unit 6.1 Introduction To Carbohydrates and Glucose DeterminationDocument12 pages(MT6317) Unit 6.1 Introduction To Carbohydrates and Glucose DeterminationJC DomingoNo ratings yet
- Micropara Final LabNotesDocument75 pagesMicropara Final LabNotescream oNo ratings yet
- Serological TestsDocument2 pagesSerological TestsKimberly EspaldonNo ratings yet
- General Pathology Lecture Group 1 HandoutDocument6 pagesGeneral Pathology Lecture Group 1 HandoutCecille AnnNo ratings yet
- Disorders of Iron Kinetics and Heme Metabolism ConceptsDocument12 pagesDisorders of Iron Kinetics and Heme Metabolism ConceptsJoanne JardinNo ratings yet
- Studying Fungi Methods Lab DiagnosisDocument74 pagesStudying Fungi Methods Lab DiagnosisKaycee Gretz LorescaNo ratings yet
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4From EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No ratings yet
- Embryo If Embryonic Period PDFDocument12 pagesEmbryo If Embryonic Period PDFRyna Miguel MasaNo ratings yet
- Put The Items From Exercise 1 in The Correct ColumnDocument8 pagesPut The Items From Exercise 1 in The Correct ColumnDylan Alejandro Guzman Gomez100% (1)
- SEMICONDUCTORS AssignmentDocument8 pagesSEMICONDUCTORS AssignmentMaryam MuneebNo ratings yet
- IntroductionDocument34 pagesIntroductionmarranNo ratings yet
- Drafting TechnologyDocument80 pagesDrafting Technologyong0625No ratings yet
- Modul-Document Control Training - Agus F - 12 Juli 2023 Rev1Document34 pagesModul-Document Control Training - Agus F - 12 Juli 2023 Rev1vanesaNo ratings yet
- Weekly Choice - Section B - February 16, 2012Document10 pagesWeekly Choice - Section B - February 16, 2012Baragrey DaveNo ratings yet
- Installation Instruction XALM IndoorDocument37 pagesInstallation Instruction XALM IndoorVanek505No ratings yet
- Programming Manual Magic 308/616-CLI Quick ReferenceDocument16 pagesProgramming Manual Magic 308/616-CLI Quick ReferencekrishnamarajublrNo ratings yet
- Cells in The Urine SedimentDocument3 pagesCells in The Urine SedimentTaufan LutfiNo ratings yet
- 2002, Vol.86, Issues 4, Hospital MedicineDocument221 pages2002, Vol.86, Issues 4, Hospital MedicineFaisal H RanaNo ratings yet
- Control SystemsDocument269 pagesControl SystemsAntonis SiderisNo ratings yet
- Assessing Gross Efficiency and Propelling Efficiency in Swimming Paola Zamparo Department of Neurological Sciences, Faculty of Exercise and Sport Sciences, University of Verona, Verona, ItalyDocument4 pagesAssessing Gross Efficiency and Propelling Efficiency in Swimming Paola Zamparo Department of Neurological Sciences, Faculty of Exercise and Sport Sciences, University of Verona, Verona, ItalyVijay KumarNo ratings yet
- 5 Important Methods Used For Studying Comparative EducationDocument35 pages5 Important Methods Used For Studying Comparative EducationPatrick Joseph63% (8)
- C Exam13Document4 pagesC Exam13gauravsoni1991No ratings yet
- Artificial IseminationDocument6 pagesArtificial IseminationHafiz Muhammad Zain-Ul AbedinNo ratings yet
- CL 5313 17021-1 Requirements Matrix-1458-5Document6 pagesCL 5313 17021-1 Requirements Matrix-1458-5Ana AnaNo ratings yet
- Creatures Since Possible Tanks Regarding Dengue Transmission A Planned Out ReviewjnspeDocument1 pageCreatures Since Possible Tanks Regarding Dengue Transmission A Planned Out Reviewjnspeclientsunday82No ratings yet
- Benjie Reyes SbarDocument6 pagesBenjie Reyes Sbarnoronisa talusobNo ratings yet
- Module - No. 3 CGP G12. - Subong - BalucaDocument21 pagesModule - No. 3 CGP G12. - Subong - BalucaVoome Lurche100% (2)
- Development of Rsto-01 For Designing The Asphalt Pavements in Usa and Compare With Aashto 1993Document14 pagesDevelopment of Rsto-01 For Designing The Asphalt Pavements in Usa and Compare With Aashto 1993pghasaeiNo ratings yet
- Course: Citizenship Education and Community Engagement: (8604) Assignment # 1Document16 pagesCourse: Citizenship Education and Community Engagement: (8604) Assignment # 1Amyna Rafy AwanNo ratings yet
- 13 Fashion Studies Textbook XIDocument158 pages13 Fashion Studies Textbook XIMeeta GawriNo ratings yet
- Lecture 1 Family PlanningDocument84 pagesLecture 1 Family PlanningAlfie Adam Ramillano100% (4)
- School Quality Improvement System PowerpointDocument95 pagesSchool Quality Improvement System PowerpointLong Beach PostNo ratings yet
- CGSC Sales Method - Official Sales ScriptDocument12 pagesCGSC Sales Method - Official Sales ScriptAlan FerreiraNo ratings yet
- (Variable Length Subnet MasksDocument49 pages(Variable Length Subnet MasksAnonymous GvIT4n41GNo ratings yet
- Operation Manual: Auto Lensmeter Plm-8000Document39 pagesOperation Manual: Auto Lensmeter Plm-8000Wilson CepedaNo ratings yet
- Trading Course DetailsDocument9 pagesTrading Course DetailsAnonymous O6q0dCOW6No ratings yet
- The Singular Mind of Terry Tao - The New York TimesDocument13 pagesThe Singular Mind of Terry Tao - The New York TimesX FlaneurNo ratings yet