Professional Documents
Culture Documents
Immune Evasion by Fungi
Uploaded by
m5bbs09Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Immune Evasion by Fungi
Uploaded by
m5bbs09Copyright:
Available Formats
Lecture overview
Fungal pathogens introduction Immune defences against fungi
Immune evasion by fungi
Immune evasion by fungi
Dr Ruth Ashbee Principal Clinical Scientist Mycology Reference Centre Leeds General Infirmary
1 2
Fungal pathogens
Fungi are eukaryotes Most fungi can only cause systemic disease in people who are immunocompromised (opportunistic); a few fungi can cause systemic disease in healthy people (true pathogens) Antifungal drugs are often toxic due to nonspecificity of their targets (i.e. humans often have the same/similar targets) Yeasts: Candida, Cryptococcus Moulds: Aspergillus, Fusarium Dimorphic: Histoplasma, Coccidioides, Blastomyces,
Fungal pathogens
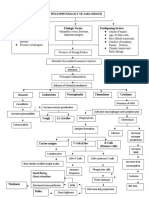
PATHOGENIC FUNGI
Pneumocystis jiroveci
Moulds Dimorphic
Yeasts
Paracoccidioides
Fungal pathogens
Innate host defences
Skin and mucosal surfaces
skin integrity, antimicrobial peptides, secretions mucociliary escalator urinary tract
Commensal population
established populations in niches
pH
skin pH (sweat & sebaceous secretions); vaginal pH, gastric pH
Complement cascade
classical pathway (immune complexes) lectin pathway (terminal mannose residues) alterative pathway (LPS, yeast cell wall)
Phagocytes
neutrophils macrophages dendritic cells
Innate immune responses
Fungus invading tissue
Pathogen associated molecular patterns (PAMP), e.g. -glucans, galactomannan, mannan Pattern recognition receptors (PRR), e.g. Toll-like receptors, dectins, pentraxin 3 T-cell receptor Antibody
Innate immune responses
Fungus invading tissue
Pathogen associated molecular patterns (PAMP), e.g. -glucans, galactomannan, mannan Pattern recognition receptors (PRR), e.g. Toll-like receptors, dectins, pentraxin 3 T-cell receptor Antibody
Neutro
Macro
Immature dendritic cell
Neutro
Macro
Superoxide
TNF-, IFN-, IL-1, IL-6, IL-12
Draining lymph node
TH1
IFN- Respiratory burst Granule release
including defensins, elastase, myeloperoxidase and reactive oxygen species
INFLAMMATORY RESPONSE
IL-10, IL-4, IL-5
Superoxide
produced by NADPH oxidase complex
H 2O 2
HOCl
Treg
Dendritic cell
Plasma cell
B-cell
TH2
Adaptive host defences
T lymphocytes (CD4, CD8)
cytokine production some killing regulation of immune response
Role of the phagocyte in fungal infection
Neutropenia is the main predisposing factor for invasive fungal infections Functional problems with neutrophils (e.g. Chronic granulomatous disease) predisposes to fungal infections Neutropenic patients who are treated with antifungals often dont respond until their neutrophil count recovers
B lymphocytes
antibody production
10
Pattern recognition receptors (PRR)
PRRs (TOLL-like receptors, Ctype lectins e.g. Dectin 1) on host cells interact with polysaccharides (e.g. chitin, glucans) and mannosylated proteins of the fungal cell wall. Dectin 1 recognises -1-3glucan, which triggers multiple signalling pathways via Syk kinase and NF-B. Results in
initiation of respiratory burst and enhanced phagocytosis production of IL-12 and TNF induction of humoral immunity stimulation of cytotoxic T cells
11
Modulation of inflammatory signals
TLR 2 activation leads to Th2 response, production of IL4, IL5 and IL10, a humoral immune response and lack of effective antifungal response. TLR4 activation leads to a Th1 response, production of proinflammatory cytokines and a good antifungal response
12
Modulation of inflammatory signals
C. albicans and A. fumigatus activate the TLR2 and hence bias the response to Th2 Polysaccharide capsule of Cryptococcus induces IL10 and biases towards Th2 response Blastomyces dermatitidis has a surface adhesin which limits release of TNF- by macrophages
Masking of PAMPS (-glucans)
Organism
Masking strategy Mannoprotein* Hydrophobin layer on conidia Polysaccharide capsule Switch to -linked glucans in yeast phase
C. albicans Aspergillus fumigatus Cryptococcus neoformans Histoplasma capsulatum Paracoccidioides brasiliensis Blastomyces dermatitidis
* Antifungal treatment may reverse this by unmasking -1-3-glucan
13 14
Phagocytosis
Phagocytosis of fungal spores
15
16
Antiphagocytic mechanisms
Cell size: too big to be taken up Hyphal forms of Candida albicans and Aspergillus fumigatus arent internalised efficiently Polysaccharide capsule of Cryptococcus Titan or Giant cells of Cryptococcus (10x size of normal yeasts) Metabolites produced by C. albicans inhibit uptake by macrophages by interfering with cytoskeleton
17
Capsule of Cryptococcus
Blocks opsonic effect of complement and antibodies Negative charge of capsule repels negatively charged host cells
18
Titan/Giant cells of Cryptococcus
Intraphagocytic survival
Histoplasma capsulatum can survive within phagocytes and replicate in macrophages modulates pH to minimise activity of enzymes
19
20
Outgrowth from phagocytes
C. glabrata recently been shown to survive macrophage phagocytosis and replicate intracellularly
Doesnt cause apoptosis Inhibits proinflammatory cytokine production Suppresses ROS production Alters phagosome maturation Replicates in non-acidic phagosome Escapes from macrophages by uncertain mechanisms
C. albicans can transform to hyphal phase, under the influence of carbon dioxide, pierce and kill the macrophage
21
22
Expulsion from phagocytes
Cryptococcus can permeabilise the phagosomal membrane Ejected from the macrophage causing no damage to fungus or host during vomocytosis
Modulation of phagocytic killing mechanisms Phagocytes undergo respiratory burst and produce toxic metabolites:
Nitric oxide Hydrogen peroxide Superoxide anion Hypochlorous acid
Various fungi have ways to modulate the ability of these toxic metabolites to kill
23
24
Inhibition of nitric oxide production
Occurs by several fungi mechanisms unclear for some C. albicans produces detoxification enzymes (e.g. catalases, superoxide dismutase (SOD)) C. posadasii* secretes an uncharacterised factor which may mediate by down-regulation of inducible NO synthase mRNA in macrophages C. neoformans produces many enzymes (4 catalases, 2 SODs and many others) and can also enlarge capsule
25
Melanin
High MW, hydrophobic pigments Produced by organisms in all biological kingdoms Extremely resistant need boiling in acid to dissolve! Provide pigment in many organisms humans, insects, fungi In fungi, produced via phenoloxidases Associated with virulence in fungi
26
Melanin in Cryptococcus
Melanin: protection against host defences
Effect
Phagocytosis
Organism
C. neoformans P. brasiliensis S. schenckii F. pedrosoi
Magnitude (%)*
7 (in vivo) 27 (in vitro) 9 50 36 31 18 >30 27 22 22 75 20 22
Killing by host cell
C. neoformans A. fumigatus P. brasiliensis S. schenckii F. pedrosoi
Oxidants
C. neoformans Aspergillus spp S. schenckii
Microbial peptides
C. neoformans
* Maximum protection for organisms with melanin cf those without
27
28
Complement cascade
Classical Pathway: Ag-Ab complexes C1q, C1r, C1s C4 and C2 Lectin Pathway: Carbohydrates MBL, MASPs, C4 and C2 C3 convertase C3a C3 C3b Amplification step C5 convertase C5a C5 C5b C5b-9 Membrane attack complex Lysis of some pathogens and cells Potent anaphylatoxin Chemotaxis Phagocyte activation Generation of oxygen radicals T-cell activation and survival Alternative Pathway e.g LPS C3, FB FD
Inhibition of the complement cascade
Binding of complement components
Mast cell activation Chemotaxis Phagocyte activation Generation of oxygen radicals T-cell activation and survival Opsonin
Secretion of antiphagocytic protein 1 (App1) protein by Cryptococcus which binds to complement receptors 2 and 3, so inhibiting complement-mediated uptake of Cryptococcus C. albicans binds several complement regulatory factors, including Factor H and C4b-binding protein (C4BP) thus inhibiting complement activity. C. albicans produces Pra1 (pH-regulated antigen) which binds plasminogen, Factor H and Factor H-like protein. This mediates complement evasion and extracellular degradation
29
30
Inhibition of the complement cascade
Binding of complement components Other fungi also bind complement regulators: Aspergillus fumigatus conidia Paracoccidioides brasiliensis Cryptococcus Pneumocystis jiroveci
Inhibition of the complement cascade
Degradation of complement components C. albicans produces Secreted Aspartyl Proteases (SAPs) which can degrade complement proteins (C3b, C4b and C5) and extracellular matrix proteins. Asp fumigatus also produces a secreted serine protease (Alp1) which degrades C3b, C4b and C5
31
32
Summary
Mechanisms used by fungi to evade host defences:
Shielding of PAMPs Ability to live and multiply in phagocytes Outgrowth from phagocytes Modulation of phagocytic killing mechanisms Role of melanin in immune protection Inhibition of complement cascade Degradation of complement proteins
References
GD Brown (2011) Innate antifungal immunity: the key role of phagocytes. Ann Rev Immunol 29:1-21 LA Chai et al (2009) Fungal strategies for overcoming host innate immune response. Med Mycol 47:227-236 JR Collette & MC Lorenz (2011) Mechanisms of immune evasion in fungal pathogens Curr Opin Micro (in press) L Romani (2004) Immunity to fungal infections Nature Rev Immunol 4:113 K Seider et al (2010) Interaction of pathogenic yeasts with phagocytes: survival, persistence and escape. Curr Opin Microbiol (2010) 13: 392400 K Seider et al (2011) The facultative intracellular pathogen Candida glabrata subverts macrophage cytokine production and phagolysosome maturation. J Immunol (in press) PF Zipfel et al (2011) Immune escape of the human facultatitve pathogenic yeast Candida albicans: The many faces of the Candida Pra1 protein. Int J Med Microbiol 301:423-430
34
33
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Introduction To ImmunologyDocument14 pagesIntroduction To Immunologykaiyeol exoNo ratings yet
- Case Study Neonatal SepsisDocument21 pagesCase Study Neonatal SepsisLenjun0% (1)
- Turgeon Review QuestionsDocument88 pagesTurgeon Review QuestionsMedTech FilesNo ratings yet
- Fundamentals of Nursing - by Darius CandelarioDocument332 pagesFundamentals of Nursing - by Darius CandelarioEmman RamosNo ratings yet
- PsiconeuroinmunologíaDocument10 pagesPsiconeuroinmunologíaLuis Alfredo Rosales GuerreroNo ratings yet
- Immunity All NotesDocument112 pagesImmunity All NotesJonathan Carlisle CheungNo ratings yet
- 13 OCTOBER, 2021 Wednesday Biology Transport SystemDocument12 pages13 OCTOBER, 2021 Wednesday Biology Transport SystemOyasor Ikhapo AnthonyNo ratings yet
- Fistulas Enterocutaneas MaingotDocument20 pagesFistulas Enterocutaneas MaingotroyvillafrancaNo ratings yet
- Medical - 1 PPT UOGDocument1,003 pagesMedical - 1 PPT UOGCHALIE MEQUNo ratings yet
- Chapter 9 The Immune System NotesDocument8 pagesChapter 9 The Immune System NotesFelix LeNo ratings yet
- Resistance of The Body To Infection: Maria Verena R. Remudaro, MDDocument69 pagesResistance of The Body To Infection: Maria Verena R. Remudaro, MDRen AlvNo ratings yet
- Chapter 15 Innate ImmunityDocument38 pagesChapter 15 Innate Immunityapi-270625839No ratings yet
- HSC Biology Module 7Document11 pagesHSC Biology Module 7arabellatav23No ratings yet
- Blood Vessel Anatomy and Physiology QuizDocument86 pagesBlood Vessel Anatomy and Physiology QuizAaronMaroonFive100% (1)
- Olympic 2014Document10 pagesOlympic 2014Ngọc LêNo ratings yet
- Glucocorticoid Effects On The Immune System - UpToDateDocument23 pagesGlucocorticoid Effects On The Immune System - UpToDatedita novia maharani100% (1)
- Heat and Cold Application 1Document42 pagesHeat and Cold Application 1Bea Trisha ArietaNo ratings yet
- InflammationDocument17 pagesInflammationNajwa AbdualgaderNo ratings yet
- IMS - Immunomodulation & ImmunodeficienciesDocument3 pagesIMS - Immunomodulation & ImmunodeficienciesJeanne RodiñoNo ratings yet
- Animal Physiology Scaffold SheetDocument5 pagesAnimal Physiology Scaffold SheetSuki ChanNo ratings yet
- Cleo - Agustin - Pathophysiology of SarcoidosisDocument1 pageCleo - Agustin - Pathophysiology of SarcoidosisCleobebs AgustinNo ratings yet
- Mod 3 Structures and Compositions of MicroorganismsDocument8 pagesMod 3 Structures and Compositions of MicroorganismsCelne CentinoNo ratings yet
- 1.3 - Defense MechanismsDocument7 pages1.3 - Defense MechanismsJEMIMA RUTH MARANo ratings yet
- Chapter 1: Introduction and Natural ImmunityDocument12 pagesChapter 1: Introduction and Natural ImmunityjoydalanonNo ratings yet
- Investigating time of death biologyDocument31 pagesInvestigating time of death biologyVanlee Mika TrindadeNo ratings yet
- Specific Host Defenses: The Immune ResponseDocument52 pagesSpecific Host Defenses: The Immune ResponseRicardo M GomezNo ratings yet
- Chapter 1 Basic Immunology Ppts DZ 2010Document50 pagesChapter 1 Basic Immunology Ppts DZ 2010Eng-Hussein MohamedNo ratings yet
- Introduction To Immunity and The Immune System: HistoryDocument149 pagesIntroduction To Immunity and The Immune System: HistoryMarissa CordovaNo ratings yet
- Final Micro ModuleDocument231 pagesFinal Micro ModuleSamuel SisayNo ratings yet
- Immunity Definition and Innate Immunity2Document30 pagesImmunity Definition and Innate Immunity2005 Abseena A ANo ratings yet