Professional Documents
Culture Documents
Pityriasis Rosea
Uploaded by
gagauzne1969Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pityriasis Rosea
Uploaded by
gagauzne1969Copyright:
Available Formats
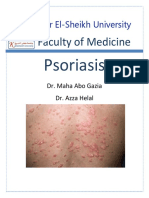
Pityriasis rosea
ICD-10: L42 Pityriasis rosea (also known as "Pityriasis rosea Gibert") is a skin rash. It is non-dangerous but may inflict substantial discomfort on some people. Classically, it begins with a single "herald patch" lesion, followed in 1 or 2 weeks by a generalized body rash lasting about 6 weeks. Pityriasis rosea is a common, self-limited rash that typically occurs in healthy adolescents and young adults. The appearance of the rash is striking and often causes concern to the bearer and family, but it truly does resolve on its own. Pityriasis Rosea Facts The cause of pityriasis rosea is unknown. Studies looking for a viral or bacterial origin are not conclusive to date. Although its cause is unknown, the rash itself is associated with the following characteristics: The majority occur between ages 10 and 35 years Two percent of patients have a recurrence It may be preceded by a recent acute infection with fever, fatigue, headache, and sore throat It occurs more often in the colder months It occurs in all races equally. Pityriasis Rosea Rash Appearance Often the rash starts with a "herald patch" -- a single, 2- to 10-cm round/oval lesion which can occur anywhere but often shows up on the trunk. The herald patch often looks likeringworm. Within a few days to several weeks, smaller lesions appear mainly on the trunk but can spread to the arms, legs, and face. On light skin, the lesions are salmon-colored, and on dark skin they are hyperpigmented. These eruptive lesions are typically oval and the long axis of the oval is oriented along skin lines. A fine, tissue-like scale stays attached to the border of the lesion. A typical eruption lasts six to eight weeks, but it can persist for five months or more. The lesions may be very itchy. Atypical Pityriasis Rosea Rash Appearance While the above description is typical, pityriasis rosea does have several atypical forms. In younger children, pregnant women, and people with dark skin the rash can be morepapular (bumpy). Vesicles and wheals can also occur in infants. A number of oral lesions can occur during a breakout. Also, at times the rash can occur on the whole body.
Signs and symptoms
Pityriasis rosea on human torso
The symptoms of this condition include:
An upper respiratory tract infection may precede all other symptoms in as many as 69% of patients A single, 2- to 10-cm oval red "herald" patch appears, classically on the abdomen. Occasionally, the "herald" patch may occur in a 'hidden' position (in the armpit, for example) and not be noticed immediately. The "herald" patch may also appear as a cluster of smaller oval spots, and be mistaken foracne. Rarely, it does not become present at all.
7-14 days after the herald patch, large patches of pink or red, flaky, oval-shaped rash appear on the torso. In 6% of cases an inverse distribution may occur, with rash mostly on the extremities. The more numerous oval patches generally spread widely across the chest first, following the rib-line in a
characteristic "christmas-tree" distribution (Langers lines). Small, circular patches may appear on the back and neck several days later. It is unusual for lesions to form on the face, but they may appear on the cheeks or at the hairline.
About one-in-four people with PR suffer from mild to severe symptomatic itching. (Moderate itching due to skin over-dryness is much more common, especially if soap is used to cleanse the affected areas.) The itching is often non-specific, and worsens if scratched. This tends to fade as the rash develops and does not usually last through the entire course of the disease.
The rash may be accompanied by low-grade fever, headache, nausea and fatigue. Over-the-counter medications can help manage these.
Causes
The cause of pityriasis rosea is not certain, but its clinical presentation and immunologic reactions suggest a viral infection as a cause. Also, HHV-7 is frequently found in healthy individuals, so its etiologic role is controversial.
Diagnosis
A herald patch of pityriasis rosea which started before the rest of the lesion as failed treatment with antifungals
Pityriasis rosea is diagnosed clinically, based on the typical appearance of the rash. If the rash is not typical, pityriasis rosea can be confused with ringworm, psoriasis, nummular eczema, and syphillis. Often a KOH test will be done to rule out ringworm and a blood test identifies syphillis. In rare cases, a lesion may need to be biopsied. Experienced practitioners may make the diagnosis clinically. If the diagnosis is in doubt, tests may be performed to rule out similar conditions such asringworm, guttate psoriasis, nummular or discoid eczema, drug eruptions, other viral exanthems, and especially secondary syphilis. A biopsy of the lesions will show extravasated erythrocytes within dermal papillae and dyskeratotic cells within the dermis.
Treatment
No treatment is usually required. It is unclear whether pityriasis rosea is contagious, but isolation is not recommended. Few good studies have been conducted to assess treatment options. One study showed that high dose erythromycin for two weeks
may shorten the course. Lesions exposed to direct sunlight resolve faster than those in unexposed areas. Ultraviolet light B (UVB) therapy may reduce itching and speed resolution lesions but therapy is most beneficial during the first week of the eruption. Oral antihistamines and topical steroids may help with itching. Oral antihistamines or topical steroids may be used to decrease itching. Steroids do provide relief from itching, and improve the appearance of the rash, but they also cause the new skin that forms (after the rash subsides) to take longer to match the surrounding skin color. While no scarring has been found to be associated with the rash, itching and scratching should be avoided. Irritants such as soap should be avoided, too; a soap containing moisturizers (such as goat's milk) may be used, however, any generic moisturizer can help to manage over-dryness. Direct sunlight makes the lesions resolve more quickly. According to this principle, medical treatment with ultraviolet light has been used to hasten resolution, though studies disagree whether it decreases itching or not. UV therapy is most beneficial in the first week of the eruption.
Prognosis
In most patients, the condition lasts only a matter of weeks; in some cases it can last longer (up to six months). The disease resolves completely without long-term effects. Two percent of patients have recurrence.
Epidemiology
The overall prevalence of PR in the United States has been estimated to be 0.13% in men and 0.14% in women. It most commonly occurs between the ages of 10 and 35. It is more common in spring. PR is not viewed as contagious, though there have been reports of small epidemics in fraternity houses and military bases, schools and gyms.
You might also like
- Ptyriasis Rosea: Clinical FeaturesDocument3 pagesPtyriasis Rosea: Clinical FeaturesRizky FajriNo ratings yet
- Pityriasis RoseaDocument14 pagesPityriasis Rosearamanda putra hasibuanNo ratings yet
- Kuliah 4 A - EritropapuloskuamousDocument46 pagesKuliah 4 A - EritropapuloskuamousTimothy TobiasNo ratings yet
- Dermatology Common Skin RashesDocument8 pagesDermatology Common Skin RashesMeredith BarbNo ratings yet
- Psoriasis A Case StudyDocument14 pagesPsoriasis A Case StudyYayin PestañoNo ratings yet
- Pityriasis Rosea Update March 2019 - Lay Review February 2019Document3 pagesPityriasis Rosea Update March 2019 - Lay Review February 2019chloee smythNo ratings yet
- Psoriasis: Risk FactorsDocument9 pagesPsoriasis: Risk FactorsJohn Michael TaylanNo ratings yet
- Pityriasis Lichenoides Update September 2016 - Lay Reviewed July 2016Document3 pagesPityriasis Lichenoides Update September 2016 - Lay Reviewed July 2016Diah KurniawatiNo ratings yet
- Pustular Psoriasis Sep 20Document8 pagesPustular Psoriasis Sep 20RemNo ratings yet
- Psoriasis: Posted: 02 Aug 2010 11:18 PM PDTDocument5 pagesPsoriasis: Posted: 02 Aug 2010 11:18 PM PDTScamb TrekNo ratings yet
- PsoriasisDocument40 pagesPsoriasisAmrit Preet KaurNo ratings yet
- Kuliah 4 B - PSORIASISDocument30 pagesKuliah 4 B - PSORIASISTimothy TobiasNo ratings yet
- Scabies Bites FactsDocument5 pagesScabies Bites FactsnisircNo ratings yet
- The Complete Guide to Psoriasis & Eczema: Symptoms, Risks, Prevention, Treatments & SupportFrom EverandThe Complete Guide to Psoriasis & Eczema: Symptoms, Risks, Prevention, Treatments & SupportRating: 4 out of 5 stars4/5 (1)
- All About PsoriasisDocument37 pagesAll About PsoriasisNiño Joshua Ong BalbinNo ratings yet
- SGD LBM 4 DilaDocument5 pagesSGD LBM 4 DilaAnnisa Safira NurdilaNo ratings yet
- PsioriasisDocument8 pagesPsioriasisRofi IrmanNo ratings yet
- PSORIASISDocument27 pagesPSORIASISnurulzakinahnunu100% (1)
- Speaker NotesDocument21 pagesSpeaker Noteschinnupepsi4allNo ratings yet
- Psoriasis: Why It HappensDocument3 pagesPsoriasis: Why It HappensPutra PrayogaNo ratings yet
- PsoriasisDocument27 pagesPsoriasisMala PotterNo ratings yet
- Pityriasis Rosea - StatPearls - NCBI Bookshelf PDFDocument4 pagesPityriasis Rosea - StatPearls - NCBI Bookshelf PDFEndah SNo ratings yet
- Scabies Guideline 2015Document13 pagesScabies Guideline 2015Brenda KristiNo ratings yet
- What Is Psoriasis?: Autoimmune ConditionDocument4 pagesWhat Is Psoriasis?: Autoimmune ConditionpallaviNo ratings yet
- Physical Trauma (Koebner's Phenomenon) Is A Major Factor in Eliciting LesionsDocument12 pagesPhysical Trauma (Koebner's Phenomenon) Is A Major Factor in Eliciting LesionsNaomi AnastacioNo ratings yet
- Scabies NotesDocument9 pagesScabies NotesAvi eNo ratings yet
- Pityriasis RoseaDocument20 pagesPityriasis RoseaMendy Herianto100% (1)
- What Is PsoriasisDocument13 pagesWhat Is Psoriasiscmahossain4880No ratings yet
- Okir A DatuDocument6 pagesOkir A DatuRonel FillomenaNo ratings yet
- Fox Scabies EncyclopediaDocument10 pagesFox Scabies EncyclopediaNimfa Christina R WibowoNo ratings yet
- Dermatitis Herpetiformis: A Concise Guide to Causes, Tests and Treatment OptionsFrom EverandDermatitis Herpetiformis: A Concise Guide to Causes, Tests and Treatment OptionsNo ratings yet
- CA PsoriasisDocument3 pagesCA PsoriasisSugar Capule - ManuelNo ratings yet
- Scabies: Signs and SymptomsDocument8 pagesScabies: Signs and Symptomspragna novaNo ratings yet
- Faculty of Medicine: Kafr El-Sheikh UniversityDocument11 pagesFaculty of Medicine: Kafr El-Sheikh UniversityjayNo ratings yet
- ArthropodsDocument42 pagesArthropodsKateNo ratings yet
- Dermatology Common Skin RashesDocument5 pagesDermatology Common Skin RashesMeredith BarbNo ratings yet
- Dermatology Most Common Skin RashesDocument5 pagesDermatology Most Common Skin RashesMeredith BarbNo ratings yet
- Scabies: Diagnostic and Therapeutic Update: Robert N. RichardsDocument7 pagesScabies: Diagnostic and Therapeutic Update: Robert N. RichardsanantaNo ratings yet
- What Are The Symptoms of Scabies?: Rash 130 MillionDocument2 pagesWhat Are The Symptoms of Scabies?: Rash 130 Millionrachel mariamNo ratings yet
- Pityriasis RoseaDocument29 pagesPityriasis RoseaAsressieNo ratings yet
- Psoriasis: PathophysiologyDocument23 pagesPsoriasis: PathophysiologyImran KhanNo ratings yet
- Pit VeriscolorDocument5 pagesPit VeriscolorNida Fithria FadhilaNo ratings yet
- Dermatology DDXDocument29 pagesDermatology DDXM.Dalani100% (2)
- CarbuncleDocument28 pagesCarbunclemimie23No ratings yet
- How Do I Get Psoriasis?Document10 pagesHow Do I Get Psoriasis?bilguun12No ratings yet
- PsoriasisDocument23 pagesPsoriasisvasavavipul38022No ratings yet
- Psoriasis - StatPearls - NCBI BookshelfDocument8 pagesPsoriasis - StatPearls - NCBI BookshelfMehmet TaşçıNo ratings yet
- SkinlesionsDocument4 pagesSkinlesionsjanina mykaNo ratings yet
- What Is Pityriasis Rosea?Document1 pageWhat Is Pityriasis Rosea?andinaNo ratings yet
- Paediatric DermatologyDocument12 pagesPaediatric DermatologyDuranka PereraNo ratings yet
- ROSACEADocument4 pagesROSACEAAlfeus GradyNo ratings yet
- Pityriasis VersicolorDocument3 pagesPityriasis VersicolorJamalul AdilNo ratings yet
- 17.pityriasis RoseaDocument5 pages17.pityriasis RoseahaidarTRVNo ratings yet
- Ntagious-Skin-Diseases/scabies ScabiesDocument10 pagesNtagious-Skin-Diseases/scabies ScabiespmNo ratings yet
- What Is PsoriasisDocument6 pagesWhat Is PsoriasisAlbean DelojeroNo ratings yet
- Shingles Update May 2020 - Lay Reviewed March 2020Document5 pagesShingles Update May 2020 - Lay Reviewed March 2020vieru nicoletaNo ratings yet
- Dermatology Essentials for Medical AssistantsFrom EverandDermatology Essentials for Medical AssistantsRating: 4 out of 5 stars4/5 (1)
- 2010 Rheumatoid Arthritis Classification - EXCERPT 2010Document1 page2010 Rheumatoid Arthritis Classification - EXCERPT 2010Jocho NeavesNo ratings yet
- Comparison of Different Types of ArthritisDocument1 pageComparison of Different Types of Arthritisgagauzne1969No ratings yet
- Interpretation of Serologic Test Results For HBV InfectionDocument1 pageInterpretation of Serologic Test Results For HBV Infectiongagauzne1969No ratings yet
- Corticosteroid Comparison Chart: Short ActingDocument1 pageCorticosteroid Comparison Chart: Short Actinggagauzne1969No ratings yet
- Ctcae 4 With Lay TermsDocument15 pagesCtcae 4 With Lay Termsrobertjohn23No ratings yet
- Child Pugh ScoreDocument1 pageChild Pugh Scoregagauzne1969No ratings yet
- Varicella and Herpes ZosterDocument19 pagesVaricella and Herpes Zostergagauzne1969No ratings yet
- Christian Medical College VelloreDocument167 pagesChristian Medical College VelloreElisa 1209No ratings yet
- Abnormalities of PuerperiumDocument16 pagesAbnormalities of PuerperiumUjjawalShriwastavNo ratings yet
- Conns Current Therapy 2021 Rick D Kellerman Full ChapterDocument67 pagesConns Current Therapy 2021 Rick D Kellerman Full Chapterkelly.caughlin506100% (2)
- Patient Admission Hospital Admission ChecklistDocument6 pagesPatient Admission Hospital Admission ChecklistSweetly MamukoNo ratings yet
- Fiebre de Origen Desconocido NEJMDocument15 pagesFiebre de Origen Desconocido NEJMJacinto RamonNo ratings yet
- 11-Iv Admixture 0Document20 pages11-Iv Admixture 0udinNo ratings yet
- Band Keratopathy ArticleDocument9 pagesBand Keratopathy ArticleDecha Pradea MaulinaNo ratings yet
- Alternative Certificate - Foundation Competences ProtectedDocument12 pagesAlternative Certificate - Foundation Competences ProtectedFlavian Costin NacladNo ratings yet
- Anatomy Review: Blood Vessel Structure & Function: Page 1. Introduction Page 2. GoalsDocument6 pagesAnatomy Review: Blood Vessel Structure & Function: Page 1. Introduction Page 2. GoalsUta Provinsiana SukmaraNo ratings yet
- Educ763 Chart AlignmentDocument6 pagesEduc763 Chart Alignmentapi-297105278No ratings yet
- Data Pending Rs Citra Arafiq 25112018Document20 pagesData Pending Rs Citra Arafiq 25112018Zahirman HamzahNo ratings yet
- Acute Heart FailureDocument18 pagesAcute Heart FailureGeorge GeorgeNo ratings yet
- DUE of PIPERACILLIN and TazobactumDocument73 pagesDUE of PIPERACILLIN and Tazobactumanup jagarlamudiNo ratings yet
- Patient CounsellingDocument46 pagesPatient CounsellingKeith OmwoyoNo ratings yet
- Science10 Q3 SLM1 1Document15 pagesScience10 Q3 SLM1 1Bien Divinaflor100% (1)
- Evaluation of Dysuria in AdultsDocument8 pagesEvaluation of Dysuria in AdultspapermintNo ratings yet
- Tricuspid AtresiaDocument5 pagesTricuspid AtresiaCassyDelaRosaNo ratings yet
- Managment of Sepsis and Septic ShockDocument2 pagesManagment of Sepsis and Septic ShockDavid Simon CruzNo ratings yet
- Article With BhajanDocument4 pagesArticle With BhajanBibek SutradharNo ratings yet
- EpidemiologyDocument86 pagesEpidemiologySainab Moohamoud83% (6)
- PRO Post Natal AssessmentDocument9 pagesPRO Post Natal AssessmentMali KanuNo ratings yet
- Diabetic Foot InfectionDocument26 pagesDiabetic Foot InfectionAmanda Abdat100% (1)
- Approach To GI DisordersDocument28 pagesApproach To GI DisordersdrvivekshimlaNo ratings yet
- Abuajela Sreh - St5 Gastroenterology - Sheffield Teaching Hospitals 1 4 / 0 1 / 2 0 2 2Document48 pagesAbuajela Sreh - St5 Gastroenterology - Sheffield Teaching Hospitals 1 4 / 0 1 / 2 0 2 2sryh2012No ratings yet
- Cure Gum Disease Naturally: Heal and Prevent Periodontal Disease and Gingivitis With Whole Foods - Ramiel NagelDocument5 pagesCure Gum Disease Naturally: Heal and Prevent Periodontal Disease and Gingivitis With Whole Foods - Ramiel Nageljopupima50% (4)
- Hyperbilirubinemia: West Visayas State University College of Medicine Neonatal Intensive Care UnitDocument49 pagesHyperbilirubinemia: West Visayas State University College of Medicine Neonatal Intensive Care UnitDonna LabaniegoNo ratings yet
- Head and Neck SurgeryDocument92 pagesHead and Neck SurgeryAlbert GheorgheNo ratings yet
- Oral Meds ChecklistDocument2 pagesOral Meds ChecklistMonika Sarmiento100% (1)
- 2464 8451 1 PBDocument6 pages2464 8451 1 PBSuwenda MadeNo ratings yet
- Acute Flaccid ParalysisDocument4 pagesAcute Flaccid ParalysisZharah RuzNo ratings yet