Professional Documents
Culture Documents
MS Case
Uploaded by
Juwaka OsakaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MS Case
Uploaded by
Juwaka OsakaCopyright:
Available Formats
A. Nursing Health History Patient x is 59 years old, male, married, Roman Catholic. He was born February 4, 1950.
He is happily married to his wife and has 2 children. He lives together with his wife and children at Tondo Manila. I gathered this information last June 15, 2009 with the help of my clients wife, my client itself and his chart to be able to obtain facts and datas that are appropriate to my client.
B. Chief complaint Nanghina at nawalan ng lakas ng kaliwang kamay ko as verbalized by the client.
C. History of the Present illness Few hours admission upon waking up, patient experienced numbness of the left arm, but able to move with associated headache and slurring of speech patient immediately rushed to nearly hospital (Jose Reyes Memorial Medical Center). BP taken 130/90, advised admission but transfer due to unavailability of room have brought of Capitol Medical Center and was admitted
D. Past Medical History According to the client, It is the third time to be confined in a hospital. He claims to be hypertensive, not asthmatic and has no any other diseases. He has no allergies to food, medications/ drugs, and/or in environment. He claims to be hypertensive since he was on college years. He had never undergo any operation/surgery. He could not recall any more what kind of immunization he had when he was young. He claims to be smoker consuming 2-3 packs a day and drink alcohol beverage occasionally
GF
GM
GF
GM
C1
C2
Legend: Patient No hereditary disease Deceased Hypertensive DM type II
The Client claims that he has family history of hyper tension. His grandparents on her mother side because of diabetes and hypertension. As well as with his grandfather side. His mother died because of diabetes type II and his father is because of hypertension. E. Social History The client lives with his own family at Tondo Manila. He has good relationship with his neighbors. He has no work and his financial is support with his brother and sister abroad. He claims to hypertensive since he was in college.
Review of System 1. Self-Perception-Self-concept Pattern According to the patient. He has no normal life in the past few years. He is a happy person and contented on what they have right now. According to him he is getting older as the time goes by and he always pray to God to not experienced any illness that lead him to suffer. 2. Role Relationship Pattern The client support system is his wife and children, his family. He believes that if Gods will nothing can change that. He also claims that this time he has a support from his brother and sister abroad because he has no work. Him and also his wife is deciding for the family. Their income is insufficient mostly when having emergency bills like hospital bills. 3. Sexuality and Reproductive Pattern According to my patient he is already circumcised when he is 10 yrs.old. He claimed that they not use any contraceptive during their early years. 4. Cognitive Perceptual Pattern The patient did not experience any hearing difficulty but in visual he cannot recognized object clearly and dont use any eyeglasses.
5. Copying Stress Tolerance Pattern My Patient is already matured and through the years of his life he can able to compensate to the environment. His family is always there to support him everywhere he have a problem.
6. Value Belief Pattern The Client claimed that health and nutrition are important to their family but the client seems to be reckless and for not taking care of her own health. He go to his physician for consultation and check-up very seldom most especially when he feels that the situations is getting worst. 7. Elimination The client claimed that he already voided 320 cc of urine before the interview. He already claimed that he dont feel any pain or discomfort while urinating. He also told that he has normal bowel. He defecates once or twice a day and dont feel any pain and discomfort while defecating.
8. Rest and Activity Pattern Household chores for him serve as an exercise. He chat with their neighborhood as his spare time. The client normally sleeps from 8pm to 5am before the hospitalization but now he has cutting hour of sleep because he keep on thinking about his hospital bill. 9. Oxygenation The client claimed that he dont experienced any difficulty of breathing even when doing something inside the war
10.
Nutrition
Patient doesnt have any food or fluid preferences. The doctor ordered a low sodium low fat diet. 24 hr. dietary recall Breakfast Oatmeal Saging Water (4 glass) Dinner Nissin Cup Noodles Water (2 glass)
A. General Appearance Our client has a small frame body built, upright posture and smooth rhythmic gait. He is appropriately dressed with no body and breath odor. His vital signs are Temp. 36.4 C, BP 140/80 RR: 19/min PR: 61 min. He looks so restless.
B. Mental Status My client is conscious and cooperative and uses simple words in communication
C. Skin Our client has a normal skin color, the temperature is warm, moisture is dry and flaky because sebaceous and sweat glands are less active during his age. His turgor is wrinkly less of elasticity mostly to his face and neck. It appears thin and translucent because of loss of dermis at sebaceous fat. His skin hair is evenly distributed. D. Nails His nail plate shape cover 160, nail addition is smooth, nail bed color is pink and capillary refill within 3 seconds
E. Head and Face My client face head is proportional to his body size with smooth contour and non-tender upon palpation. His hair is fine and evenly distributed with no lessons and his scalp is white. He has symmetrical eyeball in size and Pupil are briskly reacted in light and accommodation His visual acuity decreases it is 20/40 and lachrymal apparatus are moist. He has symmetrical facial movement and with no difficulty in talking, he was able to smile. His head is round in shape consistency is hard.
F. Eye The clients eye condition is straight normal. His eyebrows are equally distributed which are thick. His eyelid and lashes has effective
closure and frequent bilateral response. He also has symmetrical eyeball with clear bulbar and conjunctiva and sclera. His pupil are equal in size reaction to light and accommodation. Sunken eyeballs is present
G. Ears His auricle is in normal racial tone, symmetrical and elastic and his pinna recoils when folded. External canal is normal presence of some cerumen.
H. Nose Client external nose was in normal racial tone. His septum is on the midline. He has a pink mucosa which has good patency for both air lobes. He has moist nasal cavity with sinuses which are non-tender.
I. Mouth Our client lips are pink and symmetrical. Mucosa is pink and his tongue is on the midline with smooth pink texture. He has incomplete of teeth (23) with pink gums.
J. Pharynx Client uvula is on the midline with dry and pink mucosa. He also had tonsils which are not inflamed and also posterior pharynx. His gag reflex is slightly sluggish
K. Neck Our Client has voluntary movements in appearance, equal in size neck muscles with muscle strength of 5/5 that can resist. His trachea is n the midline. Thyroid gland is not palpable. His lymph woles are palpable.
L. Breast My client breast size is symmetrical, contour is flat, color is light brown, skin surface is smooth. The nipples color is dark brown which are everted and there is no discharge upon palpation. There is no presence of lumps pain and discomfort upon palpation.
M.
Chest and Lungs
Our client chest color is light brown some with skin tone. Shape is AT lateral ration 1:2, intercostals retraction is present and with 45 degrees coastal angle.
N.
Abdomen
The patients abdomen is normal racial tone, flat symmetrical on movement. Bowel sounds are normal. Bladder is not distended and liver is not palpable. There is no presence of rectal bleeding or black tarry stools. During the assessment there is no abnormal pain, liver or gallbladder trouble.
O. Upper Extremes The patient motor strength is 2/5. There are decrease in speed, strength resistance due to weakness. There is no presence of lesions nor any physical deformities. He has poor muscle tone.
P. Lower Extremties The patient motor strength is 5/5 that can resist force. There is no presence of lesions nor any physical deformities.
Q. Genitals Not assess the patient refused
Diagnostic Procedure Chest x-ray
This is the most frequent requested radiograph. Used to diagnosed cancer. Tuberculosis and other pulmonary diseases, disorder of the mediastinum and bony thorax. This provide a record of the sequential progress of development of the disease.
Ref Values Normal Normal appearing and normally positioned chest, bony thorax (all bones present, aligned symmetrical and normally shaped) soft tissues, mediastinum, lungs, pleura, heart and aortic arch
Interfering Factors An Important consideration in interpreting chest radio graph is to ask whether the film was taken in full aspiration. Certain disease states do not allow the patient to inhale fully. The ff. condition may alter the patients ability to breathe properly and should be considered when evaluating radiographs. 1. 2. 3. 4. Obesity Severe pain Congestive heart failure Scanning of lung tissues
Nursing Responsibility
Pre. Test 1. No special preparation is required. However, the patient should be given a brief explanation of the purpose. 2. Remove all the jewelry and other ornamentation in the chest and to follow all breathing instructions during the procedure.
Post test 1. Interpret test outcomes and monitor for pulmonary disease and chest orders. Explains changes in therapy based on results Ceg. Diuretics for pulmonary edema, endo tracheal tube repositioning, starting or stopping mechanical ventilation, further testing to determine new chest infiltrates.
Results: Previously noted pleural thickening and fibrotic densities in the night upper unchanged No new infiltrates are seen Both lungs remain hyper aerated The heart remains normal in size The rest of the findings are stationary
Impression: Stable chest findings
Hematology Performs different test on blood. These are the basic screening test that addresses disorder of hemoglobin (HGH) or cell production.
Specific Indication -To determine certain blood disorders, inflammation, infecting and inherited disorders of KBS, WBC, and platelet.
Nursing Responsibilities
Pre-test Explain procedure, tell that slight discomfort may be felt when skin is punctured. Avoid stress as possible because altered physiologic stats of influences and changes normal hemogram values Select hemogram components may altered values
Post test care Apply manual pressure and dressing to the puncture site Monitor the puncture site for oozing. Resume activity and diet back to normal habits.
Test
Result
Unit
Reference
Interpretation
Hemoglobin
131
O/L
M: 135 160 F: 120- 150
LOW
Hematocrit
0.38
F 0.37 + 0.45 M: 0.40 - 0.48
LOW
Total WBC Neutrophils Hymphocytes Monocyte Eosinophils Basophil Stabs Red Cell Morphology Red Cell Morphology Platelet
8.2 0.66 0.26 0.07 0.01 0.00 0.00 Normocytic
10 3/L
5.0 10.0 0.55 0.65 0.25 0.40 0.02 0.6 0.01 0.050 0 0.0005 0.01 0.05
N N N N N N N
Nomochromic
Normal
Estimate Urinalysis
Urinalysis is an essential procedure for patients undergoing hospital admission or physical examination. It is useful indicator of a healthy or diseased state, has remained an integrated part of the patient examination. Indication It determines the ff. determines the properties of urine color, turbidity, specific gravity, PH, glucose, ketones, blood, protein, bilirubin, and other abnormal constituents by microscopic examination of the urine specimen.
Nursing responsibility
Instruct the client to obtain clean catch mid stream urine Label the container to avoid any error. Perform the procedure promptly to avoid alternations Observe sterile technique Date Test Appearances: Sp. Gravity: PH: Sugar: Protein: RBC: WBC: Result Yellow/ St. Cloudy 1.025 6.5 (-) (-) 0-1 / hpf 0-1 / hpf
06-13-09
Cast: Crystal: Bacteria: No
None None
Total Protein Creatinine: Creatinine clearance Calcium Phosphorus Sodium Uric acid
(up to 0.150 9 / days) (7,000 16,000 mmol / day) (70 140 MI /min) (1.0 10 mmol / day) (110 323 mmol / day) (40 240 mmol / day) (1.5 4.4 x 103 umd/ day)
Blood Chemistry: : Lupid File
Indication Lipoprotein measurements hyperlipidomia and hylpolipidemia. are diagnostic indicators for
Nursing Responsibility
Date values
Explain the purpose of the procedure Note and document drugs the patient is taking Encourage the patient to relax Interpret the results and its indication. Tests Cholesterol Triglyceride Result 5.4 N Inter Unit mmol/L mmol/L mmol/L mmol/L Normal 0.00 0.20 0.34 2.25 0.90 1.55 0.60 4.10
06/13/09
2.60 HI
AHDL cholesterol 0.85 LO LOL 3.4 N
Tests PD2 Non fasting
Result
Inter
Unit
Normal Values
Blood Urea Nitrogen Creatinine Uric Acid Hemoglucotest Sodium Potassium Chloride 4.3 121 429
4.0 HI HI 6.9 145
umol/L umol/L umol/L mmol/L mmol/L mmol/L
2.50 6.40 53.00 - 115.00 155.00 428.00
137.00 145.00 3.60 - 5.00 98 107.00
106
CT scan of the Head and neck, brain, eyes
CT scan of the head is a relatively simple x-ray examination done by means of a special scanning machine to evaluate for suspected Intracranial lessons. The results from a cross-sectional picture of the anatomic structure, brain tissue, and surrounding cerebrospinal fluid. This axial image of the head is similar to a view looking down through the top of the head.
Procedure 1. During the test, have the patient he perfectly still on a motorized table with his or her head comfortably immobilized. The table is moved into a doughnut-shaped frame called a gantry. X-ray tubes situated within this gantry move around the patient in a circular fashion. 2. Inject an iodinated radio ague contrast substance if tissue density enhancement is desired because a questionable area needs further classification. Some patient experience nausea and vomiting after receive this contrast agent. 3. Take additional images during contrast injection.
A. Be aware that during and after the intravenous injection. The patient may experience warmth, flushing face, salty taste or nausea. Encourage the patient to breathe deeply. An emesis basin should readily available. 5. Watch for other untoward signs such as respiratory difficulty, diaphoresis, numbness or palpitations. Interfering factors
1. A false negative CT-scan can occur in the presence of hemorrhage. As hematomas age, their appearance on Ct-scans changes from high-intensity to low-intensity levels, partly because older hematomas become more transparent to x-rays. 2. Patient movements negatively affect image quality and accuracy.
Interventions
Pre-test Patient care 1. Explain test purpose and procedure. Provide written instructions. Reinforce knowledge regarding possible adverse effects such as radiation exposure or allergy to iodine contrast media. The amount of x-ray exposure for this examination is about the same as that received during a routine skull x-ray. 2. Assess pregnancy status of female patients. If positive, advise radiology department 3. Refer to iodine contrast test precaution. A creative level may be required before the study. 4. Generally, the patient should fast 2 to 3 hours before the test if a contrast study is planned. In most cases, prescribed medication can be taken before CT studies. 5. Re-assure the patient that scanning procedures no greater radiation than conventional x-ray studies. 6. Check the patient allergies. Nausea and vomiting, warmth and flushing of the face may signal a possible iodine allergy. 7. Administer analgesics and sedatives, especially to minimize pain and unnecessary movement. Post test Patient care 1. Determine whether an iodine contrast substance was used. If used. Observe and record information about reactions if they occur. Reactions may include hives, skin rashes, nausea, swelling of parotid glands (Iodism), or, most serious of all anaphylaxis.
2. Notify the physician immediately if allergic reactions occur. 3. Documentation should include assessment of information needs, instructions given, time examination was completed, patient response to the procedure and any allergic reactions.
CT Scan result Impression Bilateral pen ventricular and sub cortical white matter ischemic changes, probably due to small-vessel arteriosclerosis The nervous system is involved in some way in nearly every body function. Some major functions of the nervous system are: 1. Sensory Input. Sensory receptors monitor numerous external stimuli that may interpreted as touch, temperature, taste, smell, sound, blood pressure, and body position. Action potentials from the sensory receptors travel along nerves to the spinal cord and brain, where they are interpreted.
2. Integration. The brain and spinal cord are the major organs for processing sensory input and initiating responses. The input may produce an immediate response, may be stored as memory, or may be ignored.
3. Homeostasis. The nervous system plays an important role in the maintenance of homeostasis. This function depends on the ability of the nervous system to detect, interpret, and respond to changes in internal and external conditions. In response, the nervous system can stimulate or inhibit the activities of other systems to help maintain a constant internal environment.
4. Mental Activity. The brain is the center of mental activity including consciousness, memory and thinking.
5. Control of muscle and glands. Skeletal muscle normally contract only when stimulated by the nervous system. Thus through the control of skeletal muscle, the nervous system controls the major movements of the body. The nervous system also participate in controlling cardiac muscle, smooth muscle, and many glands
Pathophysiology
Ischemnia
Energy Failure
Acidosis
Ion Imbalance Glutamate Depolarization
Intracellular calcium Increased
Cell membranes and proteins break down Formation of free radicals Protein production decreased
Cell Injury and death
Treatment: IVF (PNSS IL X 80CC/hr) The Intravenous therapy is the administration of liquid substance directly into the vein. The intravenous route is the fastest way in which we deliver fluid and medications into the body. The client received IVF also for fluid and electrolyte replacement. Nursing Consideration - Monitor and regulate IVF at prescribed rate - Assess for the site of IV for any inflammation and infiltration - Incorporate prescribed amt. of medication in the IVF. - Make sure not to let the tubing run dry to prevent air embolism to the client. Date Administered 06-12-09 80cc/hr 06-13-09 06-13-09 06-14-09 I II III IV PNSSII PNSSIL PNSSIL PNSSIL 80cc/hr 8 10 80cc/hr 06-15-09 PNSS V
Diet: Low Sodium Low fat diet To control/decrease levels of cholesterol in your blood. To control/decrease blood pressure and/or fluid retention.
Exercise The client was advised to have gradual exercise as tolerated. This is to improve body circulation and to increase muscle strength and muscle tone. Active ROM also advised.
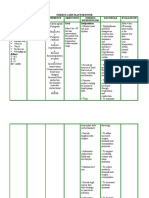
Day
Diagnostic Procedure
Diet
Activity
Medications
Treatment
Surgery
Admission June 12, 2009
Chest X-ray Urinalysis CT-Scan
LSLF
ROM
Citichlone 1gm, Plavix 75mg, ASA 80mg, Atorvastation 40mg, Lactulose 30cc, Ranitidine 150mg, Amcase 50mg, Aprovel 150mg. Plavix x 75mg, ASA 80mg, Atorvastatin 40mg, Lactulose 30cc, Ranitidine 150mg/tab, Amvase 50mg, Aprovel 150mg
PNSSIL x 80cc/hr
None
June 13, 2009
Hematology Blood Chemistry
LSLF
ROM
PNSSIL x 8
None
June 14, 2009
None
LSLF
ROM
Plavix 75mg/tab, ASA 80mg, Atorvastation 40mg, Lactulose 30cc, Ratidine 150mg/tab, Amcase 50mg, Aprovel 150mg Plavix 75mg/tab, ASA 80mg, Atorvastatin 40mg, Lactulose 30cc Amvasc 50mg, Aprovel 150mg Ranitidine 150mg, Plavix 75mg, ASA 80mg, Lupitor 40mg, Lactulose 30ml
PNSSIL x 10
None
June 15, 2009
None
LSLF
ROM, Walking
PNSSIL x 80cc
None
Discharge June 16, 2009
None
LSLF
ROM, walking
None
None
Evaluation
After 5 days of hospitalization the client was able to recover and regain strength with the proper and medical intervention given to treat neuro patient. After hospitalization the patient was advised to have an enough rest and continue the medication as prescribed by the physician. After a week the patient is advised to return for the follow-up check up for the reassessment of the health status. First thing to do is to assess the patient condition. Tell the patient that he need to take his medication as prescribed by the physician. These medications are Amvase 50mg, Aprovel 150mg, Ranitidine 150 mg, Plavix 75mg, ASA 80mg, Lipitor 40mg, Lactulose 30ml.
-Emphasize simple walking for the client for equal distribution of muscle. -Advise/Instruct to perform range of motion exercise to the affected extremity to gain muscle and motor strength.
Instruct to monitor blood pressure -Turning every 2 hours to enhance circulation. - Instruct patient to take medicine on proper time and in proper dosage.
-Emphasize importance of keeping follow-up check-up after 1 week of being discharged to hospital -Patient is on low sodium low fat diet to control and decrease cholesterol and prevent fluid relention.
Prioritization
Nursing Diagnosis Rank Rationale
1. Disturbed sleep pattern to maladaptive conditioned weakness as evidence by outing hour of sleep every two hours
This is first to be prioritized because according to Henderson sleeping is one of his 14 fundamentals need and because of this it needs an immediate intervention to gain independence in meeting his 14 fundamental needs. This is 2ns to be prioritized because this is stimulation needs that is needed by my patient in order to do normal activities of daily living. This is third to be prioritized because patient is at risk if there is no intervention done it may lead to be an actual problem of my patient. This enhancement does not need an immediate
2. Activity intolerance to weakness localized weakness (left arm) as evidence by motor strength of 2/5 3. Risk for peripheral Neurovascular dysfunction related to immobilization 4. Readiness to enhance for effective therapeutic
regimen management.
intervention and this is not occurring on the actual problem and also this can be done by follow-up intervention. 5 This is the fifth to be prioritized nursing diagnosis which under Atkinsons 13 human basis needs which is no. 10. This is also can be done by follow-up intervention.
5. Readiness to enhance for therapeutic regimen management
Nursing Care Plan
Assessment Nursing Diagnosis
S: Putolputol ang tulog ko dahil di ako mapakali kakaisip as verbalized by the patient. Disturbed sleep pattern related to maladaptiv e conditioned weakness. As evidence by cutting hour of sleep every 2 hours Discharge outcome After 2 days of nursing intervention the client will be able to gain normal sleeping pattern. Advise the patient significant other about the importance of a normal sleeping pattern of the patient. Teach the client on roper positioning of the patient on comfortable position. Explore other sleep aids (e.g. warm bath) Determine Clients /SOs expectation of adequate sleep Collaborative Administer For the patient to know and acknowledge the importance of sleeping of nursing by kazier. To promote comfort to the patient. Ref: Fundamentals of Nursing by kazier. To assist client to establish optimal sleep pattern. Provide opportunity Discharge outcome: After 2 days of nursing intervention the goal achieved because the client will be able to gain normal sleeping pattern.
Planning
Implementation
Rationale
Evaluation
Short term Outcome Objective - Cutting hour of sleep every 2 -sunken After 8 of nursing intervention the client will be able to identify 3 out of 5 ways on how to gain
Short term Outcome
After 8 of nursing
eyeballs restlessness
normal sleeping pattern.
medication as prescribed by the physicians. (Sleeping pills)
to address misconceptio ns / unrealistic expectations Ref: Fundamentals of nursing by kazier To promote healing Ref: Medical and Surgical Nursing by Brunner
intervention the client was able to identify 3 out of 5 ways on how to gain normal sleeping pattern.
Nursing Care Plan
Assessment Nursing Diagnosis Planning Implementation Rationale Evaluation
S: Nanghihin a at nawawalan ng lakas ang kaliwang kamay ko as verbalized by the patient.
Activity intolerance related to localized weakness (left arm) as evidence by motor strength of 2/5
Discharge outcome:
O: BP: - Motor strength 2/5 - Left arm weakness - Poor muscle tone
Note client reports of weakness, After 2 fatigue, difficulty days of accomplishing nursing takes. interventio Assess emotional n be able / psychological to increase factors affecting in activity the current tolerance. situation. Monitor vital signs, watching Short for changes in Term: blood pressure, After 8 of heart and nursing respiratory rate, interventio note skin pallor n the client and/or cyanosis will be able and presence of to identify confusion. 3 out of 5 Plan care with ways on rest periods how to between activities increase Provide positive activity atmosphere, while tolerance. acknowledging the client.
-to Identify causative/ precipitating factors. Ref: Fundamental s of Nursing by: Kazier -Stress and/or depression might be the result of being forced into inactivity. -To assist client to deal with contributing factors. Ref: Medical Surgical Nursing By: Brunner -To reduce fatigue.
Discharge outcome:
Goal achieved after 2 days of nursing intervention the client was able to increase. Short term Outcome:
Goal achieved after 8 of nursing intervention the client was be able to identify 3 out of 5 ways on how to increase activity.
Encourage client to maintain positive attitude; suggest use as visualization guided imagery as appropriate. Collaborate :
Ref: fundamental s of Nursing By: Kozier -Helps minimize frustration
Administer medication by the physician.
rechannel energy. ref: Fundamental of Nursing by Kozier. -To promote healing Ref: Medical Surgical Nursing By Brunner
You might also like
- Keith RN Asthma Case StudyDocument16 pagesKeith RN Asthma Case StudyCHARLES MAINANo ratings yet
- Comprehensive H&P Note Template For Phase 1 Spring Assessment 2016Document5 pagesComprehensive H&P Note Template For Phase 1 Spring Assessment 2016Derek JonesNo ratings yet
- Emergency and Disaster NursingDocument17 pagesEmergency and Disaster NursingKoleen Kirsten67% (3)
- Heart Healthy Lifestyle Lesson Plan For 2817Document5 pagesHeart Healthy Lifestyle Lesson Plan For 2817api-354388331No ratings yet
- Study Cases Assignment Nursing Student PathologyDocument4 pagesStudy Cases Assignment Nursing Student PathologyRoody AdthinyNo ratings yet
- Discussion QuestionsDocument2 pagesDiscussion QuestionsMary RiasNo ratings yet
- HIV Practice TestDocument2 pagesHIV Practice TestJoslyn GrossNo ratings yet
- Congestive Heart Failure OutlineDocument4 pagesCongestive Heart Failure OutlineDominique PorterNo ratings yet
- Synthesis Paper On The Framework For Pathophysiology: EtiologyDocument4 pagesSynthesis Paper On The Framework For Pathophysiology: EtiologyTiger KneeNo ratings yet
- Lifestyle DiseasesDocument44 pagesLifestyle Diseaseskyro draxNo ratings yet
- TEMPLATE Clinical Reasoning Case Study2Document10 pagesTEMPLATE Clinical Reasoning Case Study2Ianne MerhNo ratings yet
- Transitional Care Case Study-Pulling It All TogetherDocument13 pagesTransitional Care Case Study-Pulling It All TogethermatthewNo ratings yet
- Chapter 30 StudyGuide WorkbookDocument5 pagesChapter 30 StudyGuide WorkbookJacqueline GreerNo ratings yet
- Fluids Electrolytes Acid Base DisordersDocument6 pagesFluids Electrolytes Acid Base DisordersJerikaDolorPadilloPatricioNo ratings yet
- Lewis COPD Case StudyDocument2 pagesLewis COPD Case Studyatarisgurl08No ratings yet
- Pharm Practice QuestionsDocument42 pagesPharm Practice QuestionsShannon Garcia100% (1)
- Midwifery CurriculumDocument112 pagesMidwifery Curriculumsolomon johnNo ratings yet
- IM Clinics History 2Document4 pagesIM Clinics History 2LucyellowOttemoesoeNo ratings yet
- Altered Tissue PerfusionDocument10 pagesAltered Tissue PerfusionLaurence ZernaNo ratings yet
- Cancer Practice QuestionsDocument3 pagesCancer Practice QuestionsJoslyn Gross100% (1)
- Decision Making, Problem Solving, and Critical Thinking: Requisites For Successful Leadership and ManagementDocument28 pagesDecision Making, Problem Solving, and Critical Thinking: Requisites For Successful Leadership and Managementkit_dalkis5No ratings yet
- Genitourinary Problem: Nephrotic Syndrome Wilm's Tumor ManagementDocument19 pagesGenitourinary Problem: Nephrotic Syndrome Wilm's Tumor ManagementJayson CruzNo ratings yet
- Lecture 10 - Micro Level Factors - Health and Social Care 2017 Student (Autosaved)Document22 pagesLecture 10 - Micro Level Factors - Health and Social Care 2017 Student (Autosaved)ChéSterrNo ratings yet
- Cushing Triad: Bradycardia, Wide Pulse Irregular RespirationsDocument3 pagesCushing Triad: Bradycardia, Wide Pulse Irregular RespirationsZachary T HallNo ratings yet
- Encinada, Regine Mae M. BSN 4 Fundamentals of Nursing NCLEX Practice Questions Quiz #4Document12 pagesEncinada, Regine Mae M. BSN 4 Fundamentals of Nursing NCLEX Practice Questions Quiz #4Regine Mae Encinada100% (1)
- Pneumonia Causative Agent: 1. Infectious - Bacteria (Streptococcus Pneumonia) Virus FungiDocument2 pagesPneumonia Causative Agent: 1. Infectious - Bacteria (Streptococcus Pneumonia) Virus FungiFreeNursingNotes100% (1)
- Patho Test 3Document7 pagesPatho Test 3Stephanie 'Sveen' HansenNo ratings yet
- Physical AssessmentDocument22 pagesPhysical AssessmentKate CorderoNo ratings yet
- The Autonomic Nervous SystemDocument15 pagesThe Autonomic Nervous SystemAnonymous kQuaT9arl5No ratings yet
- PathophysiologyDocument52 pagesPathophysiologyVisalini Chandran67% (3)
- Respiratory System MedicationsDocument2 pagesRespiratory System Medicationsmlbrown8No ratings yet
- CTSP Case 2 - Hypoglycemia and HyperglycemiaDocument2 pagesCTSP Case 2 - Hypoglycemia and HyperglycemiaVanessa HermioneNo ratings yet
- Acute Respiratory Failure 1Document7 pagesAcute Respiratory Failure 1Trish 0019No ratings yet
- Pain LectureDocument13 pagesPain LectureDale BuckmanNo ratings yet
- Concept MapDocument1 pageConcept Mapapi-246466200No ratings yet
- A. Cardiac Failure: Biologic CrisisDocument11 pagesA. Cardiac Failure: Biologic CrisisJillian CaumbanNo ratings yet
- Addison and Cushing DMDocument22 pagesAddison and Cushing DManon_391984943No ratings yet
- Heart Failure CaseDocument2 pagesHeart Failure CasePaulo Arwin BaduriaNo ratings yet
- Urinary System DisordersDocument14 pagesUrinary System DisordersGideon P. CasasNo ratings yet
- Pathophysiology and Management of Psoriasis Diseas1Document28 pagesPathophysiology and Management of Psoriasis Diseas1Priyanka YadavNo ratings yet
- Chapter 64 - Administration of Injectable MedicationsDocument11 pagesChapter 64 - Administration of Injectable Medicationskristie donaldNo ratings yet
- Respiratory Care ModalitiesDocument63 pagesRespiratory Care ModalitiesErica Clerigo LandichoNo ratings yet
- Pall CareDocument81 pagesPall Careडा. सत्यदेव त्यागी आर्यNo ratings yet
- Med-Surg Final Jeopardy Review.Document3 pagesMed-Surg Final Jeopardy Review.jenn1722No ratings yet
- Chronic Kidney Disease: Prepared by Zakia RogerDocument27 pagesChronic Kidney Disease: Prepared by Zakia Rogerbene dugaNo ratings yet
- PnuemoniaDocument102 pagesPnuemoniaRegineCuasSulibNo ratings yet
- Ibd AnushaDocument32 pagesIbd AnushaRupesh R100% (1)
- October 1997 Paper 1 Clinical Nursing Essay - Type Test ItemsDocument2 pagesOctober 1997 Paper 1 Clinical Nursing Essay - Type Test ItemsTkNo ratings yet
- Nursing Case Study - With Final Slides.Document77 pagesNursing Case Study - With Final Slides.veejai_kumar100% (2)
- Saunders NCLEX Questions NPHDocument62 pagesSaunders NCLEX Questions NPHHasan A AsFour100% (1)
- Gastritis Is An Inflammation of The Gastric MucosaDocument6 pagesGastritis Is An Inflammation of The Gastric MucosaJanineLingayoCasilenNo ratings yet
- Chapter 29 Practice TestDocument8 pagesChapter 29 Practice Testnursingstudentd100% (1)
- Soap Notes HypertensionDocument6 pagesSoap Notes HypertensionCHRISTINE KARENDINo ratings yet
- Infectious Disease MedicationsDocument8 pagesInfectious Disease MedicationsSheril MarekNo ratings yet
- Pharmacology For Nurses: The Islamic UniversityDocument118 pagesPharmacology For Nurses: The Islamic UniversityRojina AdhikariNo ratings yet
- Strep Throat FactsDocument2 pagesStrep Throat FactsFactPaloozaNo ratings yet
- Pharmacology Questions (CNS Drugs) PDFDocument12 pagesPharmacology Questions (CNS Drugs) PDFRuva Oscass JimmyNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Advances in Pathobiology and Management of Paget’s Disease of BoneFrom EverandAdvances in Pathobiology and Management of Paget’s Disease of BoneSakamuri V. ReddyNo ratings yet
- Hypertension, Cardiovascular Disease, Analgesics, and Endocrine DisordersFrom EverandHypertension, Cardiovascular Disease, Analgesics, and Endocrine DisordersJack Z. YetivNo ratings yet
- Cultural Awareness in Healthcare Ce Credit CertificateDocument1 pageCultural Awareness in Healthcare Ce Credit Certificateapi-582855156No ratings yet
- TRANSCRIPTS Katherine Jackson V AEG Live August 28th 2013. DR Cherilyn Lee.Document29 pagesTRANSCRIPTS Katherine Jackson V AEG Live August 28th 2013. DR Cherilyn Lee.TeamMichaelNo ratings yet
- Jimeno ArthurDocument69 pagesJimeno ArthurOdessa DysangcoNo ratings yet
- Leadership Theory PaperDocument8 pagesLeadership Theory Paperapi-349286923No ratings yet
- C.Systematic ReviewDocument12 pagesC.Systematic ReviewIta ApriliyaniNo ratings yet
- NCP For HeadacheDocument1 pageNCP For HeadacheJohn MajanNo ratings yet
- BOOK How Can We Use Simulation To Improve Competencies in NursingDocument134 pagesBOOK How Can We Use Simulation To Improve Competencies in NursingMarta PereiraNo ratings yet
- Staff Nurse VerificationDocument258 pagesStaff Nurse VerificationNARASIMHA NAIDUNo ratings yet
- Handbook: Master of Social Work StudiesDocument26 pagesHandbook: Master of Social Work StudiesSukhman ChahalNo ratings yet
- Medical Surgical NursingDocument21 pagesMedical Surgical NursingSanthosh.S.UNo ratings yet
- Nursing ImageDocument10 pagesNursing Imageapi-392400343No ratings yet
- Registered Nurse (RN) Salary in Tallahassee, FloridaDocument1 pageRegistered Nurse (RN) Salary in Tallahassee, FloridashanteroumouNo ratings yet
- Clinical Nursing Judgment 1Document6 pagesClinical Nursing Judgment 1api-546577761No ratings yet
- Module 1 - Overview of Public Health Nursing in The PhilippinesDocument7 pagesModule 1 - Overview of Public Health Nursing in The PhilippinesKatie HolmesNo ratings yet
- 231-287 Ch09 Lowdermilk PDFDocument57 pages231-287 Ch09 Lowdermilk PDFBeam PantaloNo ratings yet
- Comprehensive NursingDocument29 pagesComprehensive NursingAmir Ahmed GezaNo ratings yet
- Ebnp SippDocument18 pagesEbnp SippthethayNo ratings yet
- Homework 1: Developing A Health Teaching Program 1. What Insights and Reflections Do You Have Based On Your Understanding of The EssentialDocument2 pagesHomework 1: Developing A Health Teaching Program 1. What Insights and Reflections Do You Have Based On Your Understanding of The EssentialRianne BaetiongNo ratings yet
- Autumn Gettings ResumeDocument2 pagesAutumn Gettings Resumeapi-663930784No ratings yet
- Nursing ProcessDocument52 pagesNursing Processanisa EndrasariNo ratings yet
- Nursing Exam Questions 2023 Part 1Document4 pagesNursing Exam Questions 2023 Part 1Lejo Sunny100% (1)
- NCM 112 - Rubric For Case Presentation Part 1 - 2021 - Laf 1Document3 pagesNCM 112 - Rubric For Case Presentation Part 1 - 2021 - Laf 1Leslie CruzNo ratings yet
- Nursing Care PlansDocument16 pagesNursing Care PlansJobelle AcenaNo ratings yet
- Introduction of Psychiatric NursingDocument26 pagesIntroduction of Psychiatric NursingadiNo ratings yet
- Roger's TheoryDocument57 pagesRoger's TheorySimon Josan100% (1)
- Research1 Sessions 1 6.docx-1Document6 pagesResearch1 Sessions 1 6.docx-1Sabrina MascardoNo ratings yet
- Study Guide Blok Palliative Care 2019 PDFDocument30 pagesStudy Guide Blok Palliative Care 2019 PDFVidya R Swandi PutriNo ratings yet