Professional Documents
Culture Documents
Stroke Patients Guide in Best Practices
Uploaded by
Csn StafferOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Stroke Patients Guide in Best Practices
Uploaded by
Csn StafferCopyright:
Available Formats
canadian stroke network
A Patients Guide to Canadian Best Practice Recommendations for Stroke Care
Canadian Best Practice Recommendations for Stroke Care have been developed by stroke experts across the country. These recommendations focus on optimal treatment for stroke patients. This guide provides patients and their families with practical information drawn from the recommendations. Learn more about the Canadian Stroke Strategy at www.canadianstrokestrategy.ca
A Patients Guide to Stroke Care
Stroke Prevention, Treatment and Recovery: Basic Information for Patients and Their Families
Strokes can be prevented and treated. Canadian Best Practice Recommendations for Stroke Care describe how to prevent stroke and how to care for patients with stroke. These recommendations are based on current research. When the Best Practices are followed, the impact of stroke is reduced.
Be informed | Be involved | Take action
KNOW ABOUT STROKE
Stroke is a medical emergency. The faster a possible stroke patient gets to hospital, the better their chances of receiving treatments that could help reverse the effects of the stroke. Be familiar with the warning signs of stroke and take immediate action by calling 9-1-1 or your local emergency number.
Know the Signs and Symptoms of Stroke:
WeaknessSudden loss of strength or sudden numbness in the face, arm or leg, even if temporary. Trouble speakingSudden difficulty speaking or understanding or sudden confusion, even if temporary. Vision problemsSudden trouble with vision, even if temporary. HeadacheSudden severe and unusual headache. DizzinessSudden loss of balance, especially with any of the above signs.
EMERGENCY RESPONSE
Never drive yourself or the person having a stroke to the hospital. Call an ambulance. Ask to be taken to the closest hospital that provides expert stroke care. You should be seen by doctors and nurses quickly after you arrive at hospital. You should receive a brain scan to find out if your stroke was caused by a blood clot or bleeding into your brain. If there is a blood clot in your brain, you should be assessed to see if you might benefit from a clot-busting drug (called tPA) that can help re-open blocked arteries. This drug can reduce the severity of the stroke and reverse some of the effects of the stroke. However, it must be given as soon as possible. Find out if tPA can help you. If you have had a mini-stroke, called a transient ischemic attack or TIA, you need immediate treatment to prevent a major stroke, even if you are not admitted to hospital. Ask about treatment and follow-up appointments.
To obtain additional copies of this publication at no charge, contact us at info@canadianstrokenetwork.ca
The contents of this publication may be reprinted without permission. However, a credit is requested. In print, please send a copy to the Canadian Stroke Strategy.
A Patients Guide to Stroke Care
STROKE CARE IN HOSPITAL
A Patients Guide to Stroke Care
You should be seen by a team of health-care professionals who are experts in stroke, preferably in a special unit dedicated to the care of stroke patients. The stroke team will plan your treatment and rehabilitation needs, and discuss these with you. Get involved in the plan. You should be assessed to see if you have trouble swallowing. Swallowing difficulties are common after stroke and can lead to choking and pneumonia. Your diet should be assessed as well. If your stroke was caused by a blood clot, you should be given a blood thinner, like ASA (commonly referred to as Aspirin) to help prevent more blood clots. Ask if a blood thinner can help you. You should have a special scan to see if the blood vessels in your neck are blocked and are a cause of your stroke. If your neck arteries are blocked, you should be assessed to see if you need surgery. You should have your blood pressure checked to make sure it is not too high. High blood pressure is the leading cause of stroke. Know your blood pressure. You should have your blood sugar checked to find out if you have diabetes. Diabetes is an important risk factor for stroke.
REHABILITATION
Your rehabilitation plan should be updated as your recovery progresses. Your mood, memory, ability to handle personal affairs and your ability to think should be assessed. Depression is very common after stroke for both patients and their caregivers. Share your concerns. Your ability to communicate, use your limbs, walk by yourself, carry out personal care and other daily tasks necessary to safely return home should be assessed. You should work with your health-care team to get ready for your return home. Know what changes need to be made in your home to make it safe and accessible. When you leave hospital, rehabilitation should continue and may occur either in a day hospital, in a clinic, other community services, or at home. Know what your continued rehabilitation needs are. When returning home, you may require additional help from family or other caregivers. Know what help you may need from others. Rehabilitation, recovery and reintegration into the community can continue for days, months, or years after stroke.
A Patients Guide to Stroke Care
Your rehabilitation team should involve you in deciding what kind of rehabilitation you need and develop a plan just for you. Get involved in making the plan.
PREVENTION
A Patients Guide to Stroke Care
Once you have had a stroke or mini-stroke, the chance of having another one is higher. Know the signs and symptoms and be prepared to respond. You need to work with health-care providers to develop a plan to deal with the things that put you at risk of stroke. Know your risk factors for stroke and find out how to reduce them. Take action. These include: high blood pressure unhealthy diet lack of exercise smoking high cholesterol (lipids) You may be prescribed ASA (commonly referred to as Aspirin) or another blood thinner to take every day. A combination of lifestyle changes and medications may be necessary to control your blood pressure, diabetes, and cholesterol. Take control.
EDUCATION
If you had a stroke or mini-stroke, or if you are at risk for stroke, you should be given key information from health-care professionals at every stage of your care. Find out: What has the stroke done to me? What will my recovery be like? What are my needs after I leave the hospital? What are my emotional needs and those of my family? What can I do to prevent another stroke? How can I access services and support in my community? Before you leave hospital, you should receive educational materials, such as the Heart and Stroke Foundations Lets Talk About Stroke.
Design EarthLore Communications
Ask questions, get answers.
There is hope after stroke. To learn more, visit:
www.canadianstrokestrategy.ca www.heartandstroke.ca www.canadianstrokenetwork.ca www.sodium101.ca www.strokengine.ca
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Drug-Food Interactions in Anti-Cancer TherapyDocument16 pagesDrug-Food Interactions in Anti-Cancer Therapyさゆう FayaNo ratings yet
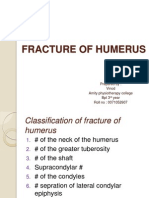
- Fracture of HumerusDocument56 pagesFracture of HumerusDr. Vinod Gupta100% (2)
- Smoking Is Injurious To HealthDocument11 pagesSmoking Is Injurious To HealthÏmŗäņPŗïņċë100% (1)
- L1.clinical ChemistryDocument37 pagesL1.clinical Chemistrysini gangNo ratings yet
- Removing Contaminated Gown and Gloves ChecklistDocument3 pagesRemoving Contaminated Gown and Gloves ChecklistFar Ri NaNo ratings yet
- Final - Health 8.5 - Prenatal and Postnatal Health Care, 1 LessonDocument26 pagesFinal - Health 8.5 - Prenatal and Postnatal Health Care, 1 LessonReggie SanguyoNo ratings yet
- Strangles and GlandersDocument26 pagesStrangles and Glandersanil regmiNo ratings yet
- CDC Lead Poisoning Prevention Signatures PDFDocument1,125 pagesCDC Lead Poisoning Prevention Signatures PDFJenika Liddell JacksonNo ratings yet
- Chapter 8. Clinical Case Studies of AuriculotherapyDocument25 pagesChapter 8. Clinical Case Studies of AuriculotherapyIkshitNo ratings yet
- Nursing Health Assessment Guide: San Pedro CollegeDocument3 pagesNursing Health Assessment Guide: San Pedro CollegeRue Cheng MaNo ratings yet
- FIN255 Answer Key 4Document4 pagesFIN255 Answer Key 4Wendz RepaldaNo ratings yet
- RESEARCH (Edited)Document6 pagesRESEARCH (Edited)Navarrete, AliceNo ratings yet
- Scott Foresman Science Grade 4Document8 pagesScott Foresman Science Grade 4rofi modiNo ratings yet
- Treatment of Acute AppendicitisDocument17 pagesTreatment of Acute Appendicitiszamir90No ratings yet
- Comprehensive Periodontics Dental Hygienist 4th Weinberg Test Bank PDFDocument8 pagesComprehensive Periodontics Dental Hygienist 4th Weinberg Test Bank PDFEmeka NnajiNo ratings yet
- D021201078 - Muhammad Fadhil Raihan - English Exercise Week 3Document3 pagesD021201078 - Muhammad Fadhil Raihan - English Exercise Week 3Faren KiriNo ratings yet
- Autonomic NeuropathyDocument20 pagesAutonomic NeuropathyRegina CaeciliaNo ratings yet
- NCP - Ineffective Airway ClearanceDocument4 pagesNCP - Ineffective Airway ClearanceKen RegalaNo ratings yet
- JPediatrCritCare2167-4903094 133710Document18 pagesJPediatrCritCare2167-4903094 133710brajendra singhNo ratings yet
- Crossectional Anatomy: Ahmed MohammedDocument26 pagesCrossectional Anatomy: Ahmed Mohammedhawi adugnaNo ratings yet
- Med SurgDocument35 pagesMed SurgChinkee Mangente82% (11)
- Physiology Biochemistry Gen Surgery AnswersDocument7 pagesPhysiology Biochemistry Gen Surgery AnswersSanNo ratings yet
- Case Taking Proforma - Respiratory SystemDocument7 pagesCase Taking Proforma - Respiratory SystemK Haynes Raja100% (11)
- EAES 2015 Scientific Program BucharestDocument14 pagesEAES 2015 Scientific Program BucharestIulia NiculaeNo ratings yet
- Unit 3 - Transudates and Exudates IIIDocument17 pagesUnit 3 - Transudates and Exudates IIIRubina KhatunNo ratings yet
- Freud and AnesthesiaDocument5 pagesFreud and AnesthesiaRaluca LNo ratings yet
- Endocrine SystemDocument4 pagesEndocrine SystemCELLINA CLARISSE DE LEONNo ratings yet
- Pschology 2Document35 pagesPschology 2Sarah Mae SaringanNo ratings yet
- NCMC103 Prelims ReviewerDocument13 pagesNCMC103 Prelims ReviewerVeronica ShaneNo ratings yet
- Tugas Bahasa Inggris Mandiri Speech Class Program Gouty ArthritisDocument3 pagesTugas Bahasa Inggris Mandiri Speech Class Program Gouty ArthritisWisnu 12No ratings yet