Professional Documents
Culture Documents
Trauma
Uploaded by
URo KkuOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Trauma
Uploaded by
URo KkuCopyright:
Available Formats
Trauma short note by S.
Wichien (SNG KKU)
Primary survey 1.Airway -first priority in 1survey -require cervical spine immobilize -abnormal voice require aw evaluate -most com I/C = alter mental status Prophylactic ETT -penetrating inj to neck -chemical/thermal inj -extensive subcu air in neck -complex maxillofacial inj -airway bleeding Definite AW Nasotracheal tube -in brething spontaneous pt -contraindicate in apnic pt Orotracheal tube -direct visualize of cord -apnic pt Cricothyroidotomy -emergency -max tube in adult = no.6 mm -C/I in pt < 8 yr = subglottic stenosis -vertical incision (avoid ant jugu v.) Emergency tracheostomy -Fx.laryngeal--clothesline inj if cricothyroidotomy--further damage 2.Breathing Tension pneumothorax -contralateral lung is compressed -heart is rotated about SVC&IVC -dec cardiac output -immediate tube thoracostomy -4 or 5th ICS ant axillary line Open pneumothorax -sucking chest wound -Temporary Rx = occlusive dressing -definite Tx = ICD Flail chest/pulmo contusion ->=3 ribs are fx -at least 2 locations -paradoxical movement -often have pulmo contusion :progress during 12 hr 3.Circulation -tachycardia : earliest sign -pt on b-block may not inc PR -carotid pulse = 60 femoral pulse =70 radial pulse = 80 -iv resus = 2 peri.line, >=no.16 <6yr = fail iv*2 -interosseous cannulation -proximal tibia, if Fx--distal femur -femoral v. = relative C/I -venous thrombosis 4 life threatening 1.massive hemothorax (>1500 ml) -blunt=ICS a inj -penetrate=systemic/pulmo.hilar vv 2.cardiac tamponade -100 ml in acute can tamponade -Tx=pericardiocentesis 3.massive hemoperitoneum 4.unstable Fx pelvis Emer.department thoracotomy (EDT) I/C 1.post arrest -penetrate trauma <15m -blunt trauma <5m 2.persist hypoT due to -cardiac tamponade -hmg -air embolism C/I -penetrate trauma >15m -blunt trauma >5m +no sign of life Procedure -lt anterolateral thoracotomy 5th ICS -tamponade=longitu peicardiotomy :ant to phrenic n :release tamponade,cardiac repair -air emboi=hilar x clamp -extrathorasic hmg=aortic x clamp -if SBP>70mmhg=go to OR Survival -highest=isolated cardiac inj shock=35% no v/s=20% -penetrating inj=15% -blunt inj=1-2% 4.Disability&exposure GCS -13-15 = mild head inj -9-12 = moderate inj -<9 = severe inj
*GCS<14 should CT scan
Trauma short note by S.Wichien (SNG KKU)
Secondary survey AMPLE hx A-allergy M-medications P-past illness /preg L-last meal E-event relate inj PE -head to toe -back,axilla,perineum -PR--sphincter,high riding prostate Adjunct -foley cath to decompress,Uo -NG tube to decrease risk of aspirate -FAST -CXR,lat cervical spine,pelvis (big three in blunt) Mechanism of inj 1.blunt inj a.hi energy -MCA,car >40 km/hr -fall from height >20 feet b.low energy -bicycle 2.penetrating inj a.GSW -hi velocity >2000 ft/s b.SGW -close range wound <7m (hi velocity) -long range wound General principle -NOM of solid inj replaced EL who require sx -less radical resection :splenorrhaphy,partial nephrectomy :1repair colon -limited initial sx -definite repair delay after resus unstable Fx pelvis -preperitoneal pelvic packing -as well as EF Transfusion Guideline -Hb >10gldL -INR <1.5 -PTT <45 sec -plt >50,000 (normal plt fxn) (MBT=plt dysfxn kerp >100,000) -fibrinogenn <100 mg/dL--cryo Massive blood Txn -1o unit in 6 hr -Type O in emer transfusion Situation 1.MCA c hypotension -Tear aorta vs Splenic inj -should emergency laparotomy first -if hypotension from aorta=not survive 2.hit a tree -epidural hematoma vs intraab fluid -can done silmutaneous 3.serious fx vs major thoracoabdo sx -can't silmutaneous -poor metabolic condition -defer until ok despite inc risk OM
Trauma short note by S.Wichien (SNG KKU)
Shock class1 bl loss 750 %bl loss 15% PR <100 BP normal PP nor/inc RR 14-20 urine >30 CNS anxious class3 bl loss 1500-2000 %bl loss 30-40% PR >120 BP dec PP dec RR 30-40 urine 5-15 CNS confuse class2 750-1500 15-30% >100 normal dec 20-30 20-30 anxious class4 >2000 >40% >140 dec dec >35 lethargy DDx of cardiogenic shock 1.tension pneumothorax 2.cardiac tamponade 3.myocardial contussion 4.air embolism -inj bronchus-->air to-->inj pulmo v. -bronchovenous fistula-->air in LV -in systolic-->air to coronary a Typical -penetrating chest inj + cvs stable -but sudden arrest after ETT/+ve P. Rx -Trendelenburg position -emer thoracotomy -cross clamping pulmo hilum -aspirate air from LV+aortic root c 18 gauge needle+50 ml syringe -vigorous massage--force air in coro :fail=tuberculin syring use in coro a -control pulmo.venous 5 source of bl loss -scalp-chest-abdo-pelvis-extremity Fx related blood loss Rib Fx 100-200 ml Tibia Fx 300-500 ml Femur Fx 800-1000 ml Pelvis Fx >1000 ml
Initial fluid resus -2L iv bolus , 20 ml/kg -NSS,RLS Urine output -indicator of organ perfusion 0.5 ml/kg in adult 1 ml/kg in child (2 ml/kg in <1yr) Respond to fluid resus 1.responder 2.transient responder 3.non responder (persistent hypoT)
Trauma short note by S.Wichien (SNG KKU)
Damage control sx -limit sx, break vicious cycle -temporary technic,delay definite sx Goal -control sx bleeding -lint GI spillage I/C -BT<35 -PH<7.2 -base def <15 (<6 in over 55yr) -INR/PTT >50% normal Abdo.inj -aorta inj must be repair--PTFE -celiac a may be ligate -SMA must flow :intravascu.tempo shunt -illiac ,infrainguinal vv :intravascu.tempo shunt -vein can ligate, except :suprarenal IVC,popliteal v -spleen/1KN--excision > repair -liver inj :packing :translobar GSW =ballon cathter :deep LW tract=foley cath Thorasic inj -bleed peipheal pulmo inj :wedge resection by GIA -penetrating inj :pulmo tractotomy :ligate bronchi 3-0 PDS suture -cardiac inj :running 3-0 prolene :pledgeted repair Blunt cerebrovascular inj (BCV inj) Denver grading 1=wall irregular,<25%stenosis 2=>25%stenosis 3=pseudoaneurysm 4=vv transection Risk hi energy mech with -displace mid face Fx (Le Fort 2/3) -basilar skull Fx c carotid canal involve -DAI & GCS<6 -c-spine Fx -hanging c anoxic brain inj -clothesline inj S+S -bright red blod from nose/mouth -cervical bruit in<50yr -expanding cervical hematoma -focal nuro def--TIA,horner,paresis -stroke Tx 1.S+S-->CT -ve--but hi suspect=angio +ve--can sx=sx 2.can't sx -antithrombotic (not have C/I) -repeat study in 7-10d heal--discon not heal--continu 6 m1+re-immaging
Trauma short note by S.Wichien (SNG KKU)
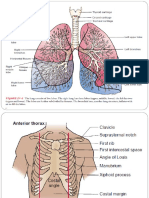
Head -orbital Fx--ocular entrapment -otorrhea/rhinorrhea/battle sign -ant facial Fx--step off -abnormal dental closure -nasal Fx -EDH--middle meningeal a/skull Fx -SDH--venous disruption DAI -hi speed decerelation inj -direct axonal inj -CT--blurring of grey white matter -multiple small puncture hmg Neck 1.cervical spine -r/o in all blunt inj until not -sx--nuro def,angulate>11, >3.5 cm 2.Fx larynx -direct blow -result in aw compromise -horseness -subcu.emphysema -palpable Fx 3.Trachea inj -end to end single layer -interrupt nonabsorb suture 4.SC inj Central cord synd -hyperextend inj -dec motor,pain,temp in upper ext -preserve lower ext Ant cord synd -loss motor,pain,temp below level inj -intact position,vibrate -poor pronosis Brown sequard synd -transect half of SC -ipsil--loss motor,propio,vibrate -contralat--loss pain,temp Methyl pred (non penetrating inj) -30 mg/kg iv bolus then 5.4 mg/kg (inj in 3hr=24hr , 3-8 hr=48hr) 5.Penetrating neck inj zone1--clavicle-cricoid zone2--cricoid-angle of mandible zone3--above angle of mandible Tx 1.hemodynamic unstable -operative exploration 2.hemodynamic stable+symp (expand hematoma,aw compromise dysphagia,subcu.emphy,hoarseness) zone1=CT neck/chest,eso/broncho zone2=sx zone3=angio+emboize 3.asymptomatic zone1=CT neck/chest,eso/broncho zone2=observe (trancervical GSW=as zone 1) zone3=observe Cervical exposure Midline structure -trachea,thyroid,carotid sheath -collar incision -2 FB above sternum notch Unilat.neck exploration -mastoid to clavicle,ant border SCM -carotid sheath=carotid a+v, vagus -facial v=carotid bifurcation -usually ligate facial v expose ICA Expose distal carotid a (zone 3) -divide ansa cervicalis--mobilize CN12 -transect post part of digastric m -mobilize CN9,10 -may remove styloid process -may ant displace of mandible Maxillofacial inj 3 region 1.upper face--frontal sinus,brain 2.mid face--orbit,nose, zygomaticomaxillary complex 3.lower face--mandible Bleeding from facial Fx -nasal packing -foley tamponade post nasal -angiembolization Aware -Fx tooth bearing bone=ATB -orbital Fx=diplopia -nose Fx=lacrimal inj,rhinorrhea
Trauma short note by S.Wichien (SNG KKU)
Chest injury Large air leak s/p thoracostomy -fiberoptic bronchoscopy -search bronchial tear or FB Persist hemothorax s/p 2 ICD -caked hemothorax -Tx=thoracotomy Thorasic vascular inj -lt side hematoma=des.aortic inj rt side hematoma=innominate inj ->95% inj distal to lt subclavian a :tether by lig arteriosum Suggest des.thoracic aortic inj 1.widening mediastinum 2.abnormal aortic contour 3.trachea shift 4.NG shift 5.rt/lt paraspinal thickening 6.depress lt main bronchus 7.lt apical cap 8.obliterate aorticopulmo window 9.lt pulmo hilar hematoma I/C fo sx -ICD>1L (penetrate) >1.5L(blunt) -ICD>200ml/hr *3hr -caked hemothorax -select des.aorta inj,great vv -cardiac tamponade -massive air leak s/p ICD + inadequate ventilation -trachea/main bronchus inj -open pneumothorax -eso.perforation Thorasic incision Anterolateral thoracotomy -5th ICS, inframammary line Clamshell thoracotomy -expose bilat pleural cavity Trap door thoracotomy -expose lt subclavian -4th ICS, sup sternal extension -lt supraclavicular incision Sternotomy+supraclavi incision -expose prox. lt subclavian, innominate v, prox.carotid -sternotomy--control vascular -supraclavi--definite sx Median sternotomy -limit in cardiac trauma -use for ant heart stab wound Posterolateral thoracotomy -post of trachea,main bronchus -des.aorta,intrathorasic eso
Trauma short note by S.Wichien (SNG KKU)
Vascular inj Hard sign -pulsatile bleeding -thrill/ bruit -no pulse -expanding hematoma Ix 1.uncomplicated penetrate injPE 2.complicated penetrate injangiogram -false aneurysm/traumatic AVF -missile pararell A -multiple site inj -chronic vv inj 3.blunt vv injangiogram Operating room angiogram -inject 50 ml contrast via CFA -x ray 2 film 1.45 mllook inj site 2.50 ml+wait 5 slook distal run off Tx Step for sx 1.suitable preparation -unijured site for graft 2.proper sx incision 3.prox/distal control 4.local heparinization 5.debride vv 6.repair vv 7.tissur repair+coverage (full thickness) Repair technique -non absorb suture -atraumatic needle -end-end anastomosis -if cantgraft -unstableligate except SVC, suprarenal IVC, bilat IJV -repair in extend position -if cross jointring graft Post op sx -no routine heparin -not drain -elevate leg -splinting Sx adjunct 1.complete angiogramstd Tx 2.intraluminal shunt -bridging Tx -can 52 hr 3.fasciotomy -ischemic > 5hr -shock -crush inj -combine skeletal+vv inj -ligate major vv -intra compart P >25 mmhg Combined vv inj 1.Temp intraluminal shunt 2.skeletal stabilization 3.tissue DB 4.definite vv repair 5.tissue coverage 6.phophylactic fasciotomy Venous inj -no Ix -often asso A inj -if no C/Iattempt repair :lateral/end to end repair -no complex repair :thrombosis -dextran improve patency -no role of anti ply/coag -ligate should fasciotomy -no role of Ix for F/U
Trauma short note by S.Wichien (SNG KKU)
Great vessel inj 90%=penetrating inj Simple lacerate of asc/transv Aorta -lateral aortorrhaphy Post inj,need interposition graft -require cardiopulmo.bypass Innominate a inj -use bypass exclusion technic :avoid need cardiopulmo.bypass -PTFE graft :end to side from prox aorta :end to end innominate a -oversewn at inj part Des.thoracic aorta inj -esmolol ,SBP<100mmhg, HR<100 Open sx -lt posterolat thoracotomy,4th ICS -partial lt heart bypass :perfuse SC when clamp aorta :sup pulmo v-->lt common FA :maintain distal perfuse P>65 mmhg Endovascu stent -in can't 1 lung ventilate ->65yr,risk cardiac decompensate -uncontrol IC HT Heart inj most result of penetrating inj Control hmg -atria=clamped c Satinsky -ventricle=digital control -larger lesion=foley cath occlusion Definite repair -running 3/o prolene or interrupt pledgeted 2/o prolene Coronary a inj -horizontal mattress -if running=stenosis Repair valve -rare necessary Blunt cardiac inj Clinical -arrhytmia -tamponade--rupture atirum/RV commotio cordis -blow to precordium--sudden arrest Tracheobronchial inj (blunt=within 2.5 cm of carina) Massive air leak -initial Tx = ETT one lung to contralat -end to end with 3/0 PDS Non sx -no persist major air leak -inj <1/3 circum Peripheral bronchial inj -bronchoscope+fibrin glue Pulmo.parenchyma inj Peripheral inj -stapled wedge resection Central inj -lobectomy/pneumonectomy -Pulmonary tractomy Pneumatocele -posttrauma pulmo pseudocyst Empyema -most com c/p after sx Esophageal inj Can mobilize -1 single lay,end to end GE jxn perforate -segmental resect+gastric pull up Large destruct inj -eso.exclusion -loop esophagos + gastros Diaphragm inj Blunt -75%=left -tear in central tendon Sx -ICD -no.1 prolene,running -using simple running technique -large avulsion=polypropylene mesh
Trauma short note by S.Wichien (SNG KKU)
Abdominal inj DPL +ve Ant abdo stap wound RBC >100,000 WBC >500 amylase >19 ALP >2 bili >0.01 Bleed midline in retroperitonium -direct manaul pressure by pad -clamp aorta at diphragmatic hiatus Bleed from pelvis -clamp infrarenal aorta Illiac vv inj -multiple vascular inj=common -pelvis vascular isolation Missed inj in penetrating inj -wound tract not follow entire distan -retroperitonium :asc-desc colon :2nd-3rd duodenum :ureter Abdo.compartment syndrome 1-intra Abdo.inj 2-after massive resuscitation Physiology -comp KN--dec RBF,Uo -dec VR--dec CO--ext/splanchnic ische -inc intrathorasic P--hypoxia Dx 1.bladder pressure -50 ml nss in bladder -can't in BD rupture,pelvic packing, neurogenic BD gr 1 2 3 4 bladder P 10-15 mmhg 16-25 mmhg 26-35 mmhg >35 mmhg--sx
Thoracoabdo stab wound >10,000 >500 >19 >2 >0.01
u/s -sense to detect fluid >250cc :morison pouch,LUQ,pelvis CT when -alter mental status -confounding injury -gross hematuria -signi pelvis fx -persistent LUQ tender -unexplain hct<35 % (ped<33%) Penetrating inj 1.hemodynamic unstable=sx 2.hemodynamic stable GSW -ant abdo=sx -RUQ=CT -tangential, back/frank=CT SGW -back/flank=CT -ant abdo stab+local w explor :DPL vs CT Blunt abdo 1.hemodynamic stable -peritonitis--sx -no peritonitis--FAST -ve--criteria for CT +ve--NOM--no=sx/yes=CT 2.hemodynamic unstable -FAST+ve--sx -FAST not sure--DPL Emergency abdo exploration -long midline incision -<6yr=transverse incision -if active bleed when opening :Liver,aorta,inf venacava,illiac vv Bleed from liver inj -clamp at pedicle (pringle maneuver) -laparotomy pad packing
Trauma short note by S.Wichien (SNG KKU)
Abdominal exploration midline incision <6yr=transverse incision Blunt -spleen,liver should be palpate -packing if Fx -inspect infracolic mesentery r/o inj If SBP<70 mmhg -clamp aorta at diaphragmatic hiatus -localized source hmg -liver=pringle maneuver -spleen=clamp splenic hilum Expose vascular -lt medial visceral rotation -incise white line of Toldt -distal desc.colon--post spleen--eso -lt colon,spleen,stomach to medial -prefer leave KN in situ Expose IVC -rt medial visceral rotation -prox.control=direct P SMA inj Fullen zone1 -post to pancreas--lt medial rotation Fullen zone2 -pancreatic edge to middle colic -approach via lesser sac -along inf edge of pancreas -may divide pancreatic body Fullen zone3/4 -direct in mesentery Illiac vv -infrarenal aortic clamping Pelvic vascular isolation -initial,clamp aorta,IVC,bilat EI vv -move clamp progressively close to inj -limit unwanted ischemia Expose bifurcate of IVC,rt CIV -can divide rt CIA -repair rt CIA after repair v Enteric contaminate -after control hmg -serial running look all smb/colon -look ant/post stomach :need open lesser sac -look duodenum=kocher maneuver -visual & palpate pancreas :just palpate is not sufficient :because fascia may mask inj :mobilize post pancreas is critical Morel Lavallee lesion -complex soft tissue wound of abdo -such as degloving inj after blunt inj Principle of Sx 1.control bleeding -blunt=4 Q packing -penetrate=along tract -supraceliac control -aortic clamping 2.identify inj site -supramesocolicduo,GB,stomach -inframesocoliclig Treitz to rectum -retroperitoneum Z1=explore all Z2=penetrateexplore all Bluntexplore expand hematoma Z3=explore penetrate inj 3.Exposure 1.aorta=lt sidel visceral rotation -mattox maneuver -white line of Toldt 2.IVC=rt side visceral rotation -kocher maneuver -cattell Braasch maneuvercaecum to L of treitz 4.control contamination 5.Decision -definite repair vs Damage sx control
Trauma short note by S.Wichien (SNG KKU)
Stomach inj -oversewn running single layer -most com miss=post wall :theough & through penetrating inj -question inj=methylene blue via NG Destructive inj -partial gastrectomy -Billoth 1,2 Damage both Latarjet n -drainage procedure Small bowel inj <1/3 circum -transverse running 3/o PDS Destructive inj/multi penetrate inj -segmental resection -end to end anastomosis -prolene 3/o Colon injury 3 concepts method 1.primary repair -lateral suture or resection c ileocolos or colocolstomy -running single layer -safe&effective in all penetrating inj 2.end colostomy -damage control sx 3.primary repair+diverting ileostomy -hi risk pt Rectum inj Intestinal diversion 1.sigmoid loop colostomy 2.loop ileostomy Sigmoid colostomy 1.adequate mobilization 2.maintain common wall of prox & distal limb above skin with one half inch nylon rod 3.longitudinal incision in tenia coli 4.immediate maturation in OR If inj accessible (in post intraperitoneum part) -repair should also be attempt If inj is extensive -presarcral drain w penrose drain -along Waldeyer fascia -via perianal incision
Duodenum inj 1.duodenal hematoma -direct blow to abdomen -occur children > adult -vomiting following blunt abdomen -barium=coiled spring sign or obstr -most tx by nonoperative :NG tube and parenteral nutrition -surgical intervention :evacuation of hematoma :by pass procedure :laparoscopic evacuation 2.duodenal perforation -blunt,penetrating inj -difficult to dx due to neutral pH,few bacteria,retroperitonium -most can be treat by primary repair :running,single layer of 3-0 monofila 1st part (prox to duct of santorini) -debridement and anastomosis -due to mobility and rich bl.supply 2nd part -tethered to head pancreas -no more than 1 cm can mobilized -end to end=narrow lumen Tx 1.patched w vascularized jejunal graft 2.Roux en Y duodenojejunostomy (best Tx in distal to papilla of vater) 3rd,4th part (behind mesenteric vv) -resect & duodenojejunostomy on lt side of sup mesenteric vv
Trauma short note by S.Wichien (SNG KKU)
Liver inj NOM -stable pt -no overt peritonitis Radio intervention -stable pt -PRC 4u/6hr or 6u/24hr Initial control hmg Perihepatic packing -lt lobe=not effective (mobilize+comp btw surgeon hand) Pringle manuver -can't HV, retrohepatic vena cava can ligate celiac to com HA (but HA proper should repair) rt or lt HA/PV may be ligate ligate rt HA=cholecystectomy hmg despite packing-->direct repair SX Hepatic vascular isolation 1.clamp -diaphragmatic aorta -suprarenal vena cava -suprahepatic vena cava 2.atriocaval shunt 3.Moore Pilcher balloon shunt Topical hemostatic -argon beam coagulator -microcrystalline collagen -topical thrombin -fibrin glu Suture -cause hepatic necrosis -no.0 chromic,running suture -large curve blunt needle -shallow=simple running -deeper=interupt horizontal mattress Translobar penetrating inj Foley/balloon occlusion Hepatotomy c selective ligation -finger fracture technique -with ligate bleeder Angioemboization Complication Hemorrhage Biloma Biliary ascites -disrupt major bile duct -often require sx Sx--resection debridement Pseudoaneurysm -rupture to bile=hemobilia :RUQ pain+UGI+jx -rupture to PV=portal HT Tx-angioemboization Fistula Biliovenous fistula -rapid jx -Tx-ERCP+EST Bronchobiliary/peurobiliary fistula -asso diaphragm inj GB&EHBD 1.GB inj -cholecystectomy 2.extrahepatic duct inj Small laceration -T tube or lat suture -4/0,5/0 monofil, absorb suture Signi tissue loss/transect -Roux-en-y choledochojejunostomy
Trauma short note by S.Wichien (SNG KKU)
Pancreatic inj 1.Pancreatic contusion -leave the ductal system -non operative Tx -close suction drainage 2.Asso pancreatic duct disruption (need intervention to prevent fistula) Identify pancreatic duct inj 1.direct exploration -of parenchymal laceration -confirm dx of ductal inject 2.operative pancreatography -through duodenotomy -canulate duct under fluorosope 3.ERCP A.Body & tail inj & transect duct 1.Roux en y pancreaticojejunostomy 2.pancreaticogastrostomy 3.distal pancreatectomy+splenectomy -not stable pt -ligate prox duct B.Pancreatic head inj Identify intraparenchymal CBD 1.squeez GB+look for bile leakage 2.cholangiogram via cystic duct Involve main PD, not CBD -central pancreatic resection w Roux en y pancreatojejunostomy Pancreaticoduodenal inj -whipple sx If no clear duct inj -placed drain Hi risk/complex Pyroic exclusion -divert GI stream -high risk/complex duodenal repair -create end duodenal fistula Procedure -gastrostomy on greater curve -grasp pylorus via gastrostomy -oversewn w 0 prolene -gastrojejunostomy -not vagotomy--low risk margins ulcer Pancreatic fistula -after d5 -amylase >3x -drain >30cc/d Splenic inj Splenectomy -hilar inj -pulverized splenic parenchyma autuTxn to greater omentum Partial splenectomy -only sup/inf pole inj -horizontal mattress Splenorrhaphy -topical methods :electrocautery,glue -absorbable mesh -pledgeted suture repair Post sx -inc plt/wbc=normal -abnormal if (>5d) Wbc >15000 Plt/wbc <20 C/p 1.subphrenic abscess 2.unrecognized iatro pancreatic inj -pancreatic ascites/fistula 3.overwhelming postsplenec sepsis -encapsulated bact -s.pneumo,h.influ,n.meningitis Tx--vaccine at 14 d
Trauma short note by S.Wichien (SNG KKU)
SMA inj Penetrating inj -GSW -black bowel+supramesocolic hemato (pathognomonic) Blunt inj -seat belt -epigastric pain+hypoT Sx -damage CS -Pruitt Inahara shunt :prevent bowel necrosis :control contaminate before graft Definite repair 1.no pancreatic inj -end to end interposition RSVG 2.asso pancreatic inj -graft should be tunneled -from aorta beneath duo to distal SMA SMV inj -digital compression -attempt venorrhaphy -ligation in life threatening situation (bowel edema) -should temp abdo closure Illiac a inj -transpelvic GSW -blunt asso pelvic Fx Sx -Pruitt Inahara shunt for DCS -interposition grafting Kidney inj Renorrhaphy -vascular occlusion control bleeding -preserve renal capsule -close collecting system separately -closed capsule over collecting system Renal vascular inj -in penetrating inj -graft interposition for preserve renal -can't repair=nephrectomy -must palpate contralat KN :unilat renal agenesis=0.1% Blunt inj -90%=NOM -sx=renovascular inj Ureter inj -pelvic Fx, penetrating inj -may not identify,until c/p (urinoma) -if suspect btw EL :iv methylene blue/indigo carmine Sx -5/o absorb monofilament -distal ureter=reimplant (Boari flap) Bladder inj 1.intraperitoneum -sx=run single layer 3/o mono,absorb 2.extraperitoneum -non sx=BD decomp 2 wk
Trauma short note by S.Wichien (SNG KKU)
Pelvic Fx Hemodynamic unstable FAST +ve -ve | | sx 2 u PRC/ED | | P.packing unstable=sx P.fixation stable=SICU | | Stable--yes----> SICU+/-CT | | no ongoing bleed | | Angiogram Pelvic packing -6 pads in paravesical space -small suprapubic incision Ant external fixation -dec pelvic volume -tamponade effect Option for tx 1.Observe -small pseudoaneurysm -intimal dissection small intimal flap -small AVF in ext 2.Lateral suture -small a inj c little or no loss tissue 3.End to end anastomosis -transect or nearly, defect 1-2 cm -mobilize end of vv by ligate small br -aorta,subcla,BA--difficult to mobilize -beveling--inc diameter/avoid stenosis 4.Interopsition graft -autogenous v/a,PTFE,dacron VV<6mm -int carotid,brachial,sup femoral,PA -should use SV from contralat groin -PTFE--thrombosis Larger a -subclavian,innominate,aorta,CIA -PTFE graft Enteric contaminate -aorta,illiac vv inj -can use graft -irritation before place graft 5.Transposition -use when has bifurcation Prox.inj of int carotid -mobilize ext carotid,divide distal -end to end anastomosis CIA/EIA -rt CIA transpose to lt CIA -lt IIA transpose to distal rt CIA -rt IIA transpose to rt EIA 6.Extra anatomic bypass 7.Interventional radiology -for tx a,v inj that can't surgery -stent in int carotid a,in base of skull -control hmg in hepatic inj or pelvic fx vein -more difficult to repair--thrombosis -SVC,suprarenal VC,PV--can't ligate -other v may be ligate chronic hypertensive avoid by 1.EB toe to hip at end of procedure 2.continu elevate lower ext 30-45 ( 1wk)
Vascular inj Hard sign--open sx -pulsatile hmg -absent pulse -acute ischemia Soft sign--further evaluation -signi hematoma -asso n inj -AA index <0.9 (SBP inj/SBP un-inj) -thrill/bruit Repair -prox+distal control -heparin (50 u:1ml) prevent clot Artery should repair -carotid,innominate,brachial, sup.mesenteric,proper hepatic, renal,illiac,femoral,popliteal Vein should repair -SVC, IVC prox.to renal V,PV
Trauma short note by S.Wichien (SNG KKU)
Ext inj Common combine inj 1.Fx clavicle/1st rib 2.dislocate shoulder/ prox.humerous Fx 3.dislocate elbow/ Supracondyle Fx 4.Fx femur 5.dislocate knee Compartment synd -early sign=numbness 1st/2nd toe -coma pt=difficult dx compartment P -handheld Stryker device -gradient=DBP-comp P -<35mmhg=fasciotomy Fasciotomy -4 compartment fasciotomy :2 incision :lateral incision=ant&lat comp :medial incisin=flex comp (must detach soleus from tibia) (decomp deep flex comp) Arterial spasm guidelines step1-intra a. Alteplase bolus step2-intra a. NTG bolus step3-intra a. Verapamil bolus step4-intra a. Papaverine drip
subclavian a axillary a brachial a femoral a popliteal a
Fx fixation vs repair a -controversy which be done 1st -prefer temp intravascular shunt Sx -artery access for on table angiogram in OR in pt evidence of limb threat :percu femoral vv or direct cannulate :SFA just above medial knee subclav/axillary a -exam brachial plexus before sx -RSVG/6mm PTFE Brachial a -medial upper ext longitu incision -RSVG SFA -RSVG Popliteal a -medial one incision approach -detach semiten,semimem,graccilis if have v inj -repair v 1st c PTFE graft -a is shunted Isolate a inj -RSVG
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Urologic Imaging For Externist PDFDocument55 pagesUrologic Imaging For Externist PDFURo KkuNo ratings yet
- Abdominal PainDocument76 pagesAbdominal PainURo KkuNo ratings yet
- Malignant Renal TumorDocument17 pagesMalignant Renal TumorURo KkuNo ratings yet
- Hepatoblastoma ReseachDocument32 pagesHepatoblastoma ReseachURo KkuNo ratings yet
- Mesenteric AdenitisDocument28 pagesMesenteric AdenitisURo KkuNo ratings yet
- GEP NETsDocument3 pagesGEP NETsURo KkuNo ratings yet
- Perirenal HematomaDocument23 pagesPerirenal HematomaURo KkuNo ratings yet
- แบบฝึกหัด Essay 4.1Document1 pageแบบฝึกหัด Essay 4.1URo KkuNo ratings yet
- Case Discussion: Stab Injury L Frank CHFDocument27 pagesCase Discussion: Stab Injury L Frank CHFURo KkuNo ratings yet
- Ruptured DiverticulitisDocument18 pagesRuptured DiverticulitisURo KkuNo ratings yet
- LRP PresentationDocument21 pagesLRP PresentationURo KkuNo ratings yet
- Renal Trauma BluntDocument40 pagesRenal Trauma BluntURo KkuNo ratings yet
- แบบฝึกหัด Essay 3Document1 pageแบบฝึกหัด Essay 3URo KkuNo ratings yet
- Histology: GIST Short Note by by S.Wichien (SNG KKU)Document3 pagesHistology: GIST Short Note by by S.Wichien (SNG KKU)URo KkuNo ratings yet
- Reflec in SXDocument2 pagesReflec in SXURo KkuNo ratings yet
- Reflec in SXDocument2 pagesReflec in SXURo KkuNo ratings yet
- Possible Sign of Superfi V.abnor: 2 Primary FXNDocument7 pagesPossible Sign of Superfi V.abnor: 2 Primary FXNURo KkuNo ratings yet
- แบบฝึกหัด Essay 3Document1 pageแบบฝึกหัด Essay 3URo KkuNo ratings yet
- UrologyDocument10 pagesUrologyURo KkuNo ratings yet
- Prophylactic ETT 6yr Fail IV 2: Primary Survey 1.airway 3.circulationDocument17 pagesProphylactic ETT 6yr Fail IV 2: Primary Survey 1.airway 3.circulationURo KkuNo ratings yet
- Endopeptidase: Carbo ProteinDocument12 pagesEndopeptidase: Carbo ProteinURo KkuNo ratings yet
- Parietal Cell: Angle of His Angularis IncisuraDocument13 pagesParietal Cell: Angle of His Angularis IncisuraURo Kku100% (1)
- HerniaDocument5 pagesHerniaURo KkuNo ratings yet
- Anatomy (Length: Duodenum 2.submucosaDocument12 pagesAnatomy (Length: Duodenum 2.submucosaURo KkuNo ratings yet
- BreastDocument13 pagesBreastURo KkuNo ratings yet
- Acute PancreatitisDocument36 pagesAcute PancreatitisURo KkuNo ratings yet
- Anatomy: - 4 Glands ( 4 Gland 3%) PhysiologicDocument6 pagesAnatomy: - 4 Glands ( 4 Gland 3%) PhysiologicURo KkuNo ratings yet
- ColorectalDocument26 pagesColorectalURo KkuNo ratings yet
- LiverDocument13 pagesLiverURo KkuNo ratings yet
- SpleenDocument3 pagesSpleenURo KkuNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- CLINICAL RADIOLOGY: KEY IMAGING FINDINGS OF THE THORAXDocument48 pagesCLINICAL RADIOLOGY: KEY IMAGING FINDINGS OF THE THORAXChubii Luph DokhitNo ratings yet
- Respiratory Exam GuideDocument18 pagesRespiratory Exam GuideIbi Yulia Setyani100% (1)
- Trauma Nursing IntroductionDocument12 pagesTrauma Nursing Introductionanimesh pandaNo ratings yet
- Post Tubercular Sequelae.123175034Document29 pagesPost Tubercular Sequelae.123175034Andre Prasetyo MahesyaNo ratings yet
- Urology Case Reports: Rama Firmanto, Fina Widia, Gampo Alam Irdam TDocument3 pagesUrology Case Reports: Rama Firmanto, Fina Widia, Gampo Alam Irdam TyuliaydjwNo ratings yet
- Egan's Fundamentals of Respiratory Care Chapter 20 Test Bank Imaging ReviewDocument8 pagesEgan's Fundamentals of Respiratory Care Chapter 20 Test Bank Imaging ReviewZahra Margrette SchuckNo ratings yet
- MKQ 019Document6 pagesMKQ 019faisaldanyaniNo ratings yet
- CRT Exam Review Guide Chapter 15Document27 pagesCRT Exam Review Guide Chapter 15Dharlyn MungcalNo ratings yet
- Paediatric Respiratory Reviews: Warwick J. Teague, Jonathan KarpelowskyDocument6 pagesPaediatric Respiratory Reviews: Warwick J. Teague, Jonathan KarpelowskyClaudia Sughey Herrera PalominoNo ratings yet
- Types of PneumothoraxDocument13 pagesTypes of PneumothoraxumarNo ratings yet
- CH 46 Complications of AnaesthesiaDocument29 pagesCH 46 Complications of AnaesthesiaChristian LeepoNo ratings yet
- Chest Radiology For Dummies PDFDocument6 pagesChest Radiology For Dummies PDF0395No ratings yet
- Abcde ApproachDocument3 pagesAbcde ApproachHala BahaaNo ratings yet
- Management of Chest Trauma: Corinna Ludwig, Aris KoryllosDocument6 pagesManagement of Chest Trauma: Corinna Ludwig, Aris KoryllosAnonymous GRrs0CONo ratings yet
- Thoracic Ultrasonography: Clinical Uses and ApplicationsDocument54 pagesThoracic Ultrasonography: Clinical Uses and ApplicationsMesay AssefaNo ratings yet
- Physiology of PleuraDocument16 pagesPhysiology of PleuraMohamedSalah100% (2)
- Water Seal DrainageDocument6 pagesWater Seal DrainageAmit MartinNo ratings yet
- 7 NCPDocument7 pages7 NCPVina EmpialesNo ratings yet
- P1 Compilation PDFDocument56 pagesP1 Compilation PDFJames Eugene CaasiNo ratings yet
- Atlas of Primary Care Procedures (1st Ed.)Document362 pagesAtlas of Primary Care Procedures (1st Ed.)dianadirgau2399No ratings yet
- ST Johns Medical Responder CompleteDocument40 pagesST Johns Medical Responder CompleteSuNo ratings yet
- Common Short Exam Cases in PediatricsDocument148 pagesCommon Short Exam Cases in PediatricsKoricho Mengistu100% (2)
- 3rd Edition Self-Assessment in Respiratory MedicineDocument267 pages3rd Edition Self-Assessment in Respiratory MedicineamjadsabahNo ratings yet
- A Rare Case of Vanishing Lung SyndromeDocument3 pagesA Rare Case of Vanishing Lung SyndromeMUH. RAKIB YUNUSNo ratings yet
- American College of Surgeons - Online LearningDocument18 pagesAmerican College of Surgeons - Online Learningasi basseyNo ratings yet
- Pathophysiology Pulmonary QuizDocument9 pagesPathophysiology Pulmonary QuizTanya Viars100% (1)
- Jurnal Reading RadiologiDocument38 pagesJurnal Reading RadiologiSari RezekiNo ratings yet
- Surgical Notes (Teddy)Document88 pagesSurgical Notes (Teddy)shichianNo ratings yet
- Tension Pneumothorax - StatPearls - NCBI BookshelfDocument9 pagesTension Pneumothorax - StatPearls - NCBI Bookshelfshinta damayantiNo ratings yet
- Pneumothorax Key PointsDocument2 pagesPneumothorax Key PointsJose UringNo ratings yet