Professional Documents
Culture Documents
Precision and Accuracy of The Leukocyte Differential
Uploaded by
blanket_thOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Precision and Accuracy of The Leukocyte Differential
Uploaded by
blanket_thCopyright:
Available Formats
Sysmex Journal International Vol.11 No.
1 (2001)
Precision and Accuracy of the Leukocyte Differential on the Sysmex XE-2100
R. HERKLOTZ and A. R. HUBER
Zentrum fr Labormedizin, Kantonsspital Aarau, 5001 Aarau, Switzerland.
The automated leukocyte(WBC) 5-part differential count is expected to produce accurate and precise results. Furthermore pathological blood samples need to be detected at a high sensitivity. In this study we evaluated the WBC differential count as well as the new parameters for immature myeloid granulocyte counts of the new automated haematology analyser, the Sysmex XE-2100. We tested the performance in terms of accuracy and precision using normal, pathological and leukopenic samples. Precision profiles showed excellent performance even for leukopenic samples. Investigations of the count parameters for immature cell populations obtained from the IMI-channel (immature cell information) and the IG (immature granulocyte count) obtained from the DIFF-channel also showed a good performance, although the imprecision was found to be higher. We compared the WBC differential to the manual 500 cell diff. The general performance for the differential count was excellent with a correlation coefficient (r) of 0.83 for monocytes (MONO), 0.97 for eosinophils (EO), and 0.99 for lymphocytes (LYMPH) and neutrophils (NEUT). For obvious reasons the basophil (BASO) correlation was found at expected level of 0.51, which is caused by the very low total count and the high imprecision of the manual differential for this particular parameter." (Sysmex J Int 11 : 8-21, 2001) Key Words
Automated Hematology Analyzer, XE-2100, WBC Differential, Precision, Accuracy
INTRODUCTION
The reliable detection of pathological blood samples and the screening of normal blood samples, respectively, are of major importance for the haematology laboratory. Use of modern haematology analysers aims to reduce the need for visual differential leukocyte(WBC) counts whilst retaining optimal diagnostic security and in that respect system precision and accuracy are very important. The modern differential WBC count, as a minimum, is expected to produce an accurate quantitation of the 5 major physiologic WBC subpopulations: neutrophil (NEUT), eosinophil (EO), basophil (BASO) granulocytes (GRAN), monocytes (MONO) and lymphocytes (LYMPH). Of additional interest is quantitation of immature myeloid and lymphoid cells on one hand and the detection, and, if possible, quantitation of reactive NEUT (band cells) and atypical LYMPH on the other. The parallel application of different measurement principles, based on flow cytometry, allows comparatively inexpensive and rapid analysis of a remarkable number of blood cells thus delivering the statistical prerequisites for acceptable precision at all count levels. The purpose of the present study was to evaluate the precision and accuracy of the differential WBC count generated by one of the latest and recently launched haematology systems, the Sysmex, XE-21001). According to the
8
manufacturers claims, the system can be utilised for the regular 5-part differential WBC count, enumeration of nucleated red blood cells (NRBC), reticulocytes (RET) and their precursors, and for quantitation of immature granulocytes (IG) (metamyelocytes, myelocytes and promyelocytes). Additionally flagging algorithms suggest the presence of further pathological cells and elements such as blasts, IG, etc.
MATERIAL AND METHODS
WBC Differentiation on the XE-2100
The Sysmex, XE-2100 analyser differentiates WBC into the following 5 sub-populations (Table 1). In the presence of certain abnormalities the XE-2100 can often count specific cell types in a different channel2) and correct the original sub-population by an equivalent amount (the corrected parameter will be flagged with & - see table 2). In case of other abnormalities the abnormal cells are allocated to a sub-population without correction. IG and NRBC are detected separately and are subtracted from NEUT and LYMPH respectively. Additional morphological abnormalities are reported as suspect messages (flags). These are listed in Table 3 together with the cell type included in each message.
Sysmex Journal International Vol.11 No.1 (2001)
Table 1 The regular WBC parameters of XE-2100 Abbreviation WBC NEUT LYMPH MONO EO BASO Parameter Leukocytes Neutrophils Lymphocytes Monocytes Eosinophils Basophils Parameter contents, respective blood cells NEUT, LYMPH, MONO, EO, BASO Band cells and mature neutrophils Lymphocytes, plasma cells Monocytes Eosinophils Basophils
Table 2 XE-2100 parameter when morphologically abnormal cells are present Parameter contents, allocation of normal and abnormal cells WBC&, NRBC NEUT, LYMPH&, MONO, EO, BASO NEUT&, IG Band and segmented neutrophils Promyelocytes, myelocytes, metamyelocytes Myeloblasts, promyelocytes, myelocytes, metamyelocytes LYMPH&, nucleated red blood cells (NRBC) LYMPH, plasma cells, myeloblasts Monocytes Eosinophils Basophils NRBC
Abbreviation WBC WBC& NEUT NEUT& IG IMI LYMPH LYMPH& MONO EO BASO NRBC
Parameter Leukocytes Leukocytes corrected Neutrophils Neutrophils corrected Immature granulocytes Immature myeloid information Lymphocytes Lymphocytes corrected Monocytes Eosinophils Basophils NRBC
Table 3 Suspect messages (flags) for morphological abnormalities of the WBC Abbreviation Blasts? Imm Gran? Left Shift? Atypical Lymph? Abn Lymph/L-Blasts? Expected cell type Myeloblasts Promyelocytes, myelocytes, metamyelocytes Band cells (stab) Atypical lymphocytes, plasma cells Abnormal lymphocytes, lymphoid blasts
Principles and technology used for the WBC differential count
Using flow cytometry technology, the Sysmex, XE-2100 produces a differential WBC count in two distinct channels (WBC/BASO- and DIFF-channel) 1,3). When passing through the flow cell, cells are interrogated by the light beam from a semi-conductor laser with a wavelength of 633 nm and are differentiated by two out of three captured signals (forward scatter, side scatter and side fluorescence). Forward scattered light is detected by a photodiode while side scattered light and side fluorescence intensity at an angle of 90 are detected by a photo multiplier after filtering at specific wavelengths (>640nm and >660nm, respectively). The intensity of forward scattered light is equivalent to the cell volume while side scattered light yields information about the cellular content (nuclear size and granularity). The side fluorescence intensity is equivalent to the amount of RNA and DNA present in the cell. The XE-2100 is equipped with an additional channel (IMI channel) to generate the flags for the WBC differential. In the IMI channel radio frequency and direct current measurement principles (RF/DC detection method) are used. The direct current (DC) pulse height is equivalent to cell volume. The radio frequency measurement provides information on the internal composition of the cell (nucleus, granules).
Sysmex Journal International Vol.11 No.1 (2001)
WBC/BASO-channel: counting WBC and BASO
In this channel the XE-2100 uses forward and side scattered light signals to quantify total WBC and BASO. An acidic surfactant lyses and shrinks red blood cells(RBC), platelets (PLT) and WBC with the exception of BASO. This results in RBC ghosts and PLT, WBC nuclei, and a further population of BASO whose cellular integrity remains intact. The BASO therefore appear on the diagram of forward scatter (y-axis) and side scatter (x-axis) as a distinct population of cells.
IMI-channel: Presence of myeloid precursors
The IMI-channel (Immature Myeloid Information) selectively detects immature myeloid cells normally not occurring in peripheral blood of healthy individuals. The reaction principle in the IMI-channel is based on differences in membrane composition between mature and IG: mature cells contain in their membranes a relatively high concentration of cholesterol and lower concentration of proteins. Addition of the channel-specific reagents (non-ionic surfactant of the polyoxyethylene class, sulphur containing amino acids, cationic surfactant) causes membrane damage (mainly due to the cationic surfactant) in mature cells followed by elution of intracellular components. The membranes of IG are also partly damaged, however, the non-ionic surfactant and the sulphur containing amino acids enter the cell and fix both the membrane and the intracellular components. Since various types of IG react differently to the reagent, they occupy distinct areas in the IMI scattergram. Thus it is possible to distinguish blast cells from less immature WBC and in turn, IG such as myelocytes, metamyelocytes from left shifted NEUT. The IMI-channel determines the total number of myeloid precursor cells and the information about their positioning is used to generate different suspect messages.
DIFF-channel counting NEUT, LYMPH, MONO, EO and IG
In the DIFF-channel, the XE-2100 differentiates the WBC into four sub-populations by means of side fluorescence (x-axis) and side scattered light (y-axis): LYMPH, MONO, EO and NEUT. BASO lie within the NEUT cluster and any NRBC are included in the LYMPH cluster. NEUT = WBC LYMPH MONO EO BASO (1) The surfactant applied in this channel induces complete lysis and shrinkage of the red cell and PLT membrane while the effect on WBC is only a slight increase in permeability thus permitting a polymethine dye with high affinity for RNA and DNA to enter the cells. When excited by a 633 nm laser beam the stained cells emit a fluorescence proportional to their content of nucleic acid. Blasts, atypical LYMPH, plasma cells and IG show an intense fluorescence. Thus IG are quantified by separating them from the mature NEUT. NEUT& = NEUT IG (2) Another reagent (an organic acid) binding specifically to the granules of EO allows their discrimination from the NEUT based on a greater side scatter signal intensity.
Q-flag system: Quantitative interpretative (IP) messages for WBC from DIFF- and IMI-channels
The XE-2100 replaces the traditional Yes/No flags by a series of column-diagrams4). The numerical value for the intensity of a flag reflects the probability of this specific flag. The trigger limit can be adjusted and is pre-set to an arbitrary value of 100. If the value is below 100 the information is considered as being negative. If it is between 100 and 300 (max. level) the respective warning is displayed as a flag. The value of the Q flag is that it provides information on the degree of positivity or negativity of a flag. The XE-2100 offers the following Q-flags indicating the suspicion for a qualitative (morphological) abnormality of WBC: Blasts?, Imm Gran?, Left Shift?, Abn Lymph/L-Blasts? and Atypical Lymph?. The Blasts? flag indicating the suspicion for myeloblasts is displayed when both, the DIFF-channel (in the Blasts/Atypical Lymph area) and the IMI-channel (in the Blast area) identify cells of the respective cell type, . e.g., the message for IG (theoretically promyelocytes, myelocytes and metamyelocytes = Imm Gran?) appears as soon as in the respective area of either the DIFF scattergram or the IMI scattergram cells are spotted. The intention of this system is the diagnostic interpretability of characteristic patterns of Q-flags leading to selective action messages as well as the adaptation of sensitivity and specificity of the flagging performance to individual laboratory needs4).
Corrected WBC and LYMPH count when NRBC are present
The Sysmex XE-2100 features a separate channel to quantify NRBC (NRBC-channel). Even though the present study did not focus specifically on NRBC, the data from this channel is important since it allows correction of total WBC and LYMPH counts. WBC& = WBC NRBC (3) LYMPH& = LYMPH NRBC (4) In the following, LYMPH and WBC # are always meant to be the corrected values thus transforming equation (1) into equation (5). NEUT = WBC& LYMPH& MONO EO BASO (5)
Blood samples and reference values
For the present study whole blood samples from the routine workload of the Kantonsspital, Aaarau, Switzerland collected in 4.5mL K3EDTA-Vacutainers (Hemogard,
10
Sysmex Journal International Vol.11 No.1 (2001)
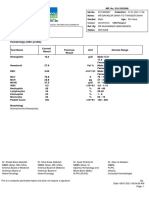
Table 4 Reference ranges. Absolute and percentage reference ranges for leukocyte differentiation Abbreviation XE-2100 Leukocytes Neutrophils Neutrophils corrected Segment Gran. Band cells (stab) Immature granulocytes Metamyelocytes Myelocytes Promyelocytes Myeloblasts Eosinophils Basophils Monocytes Lymphocytes Plasma cells Immature Myeloid Information WBC NEUT NEUT& SEG STA IG MET MYZ PMZ MYB EOS BAS MON LYZ PLA Reference range (109/L) (%) 4.0 10.0 1.6 8.5 1.6 8.5 1.6 7.5 < 1.0 < 0.05 < 0.05 < 0.02 < 0.6 < 0.2 0.1 1.0 0.8 4.0 < 0.1 < 0.07
Manual Diff.
40 85 40 85 40 75 < 10 < 0.5 < 0.5 < 0.2 <5 <2 2 10 20 40 <1 < 0.7
EO BASO MONO LYMPH IMI
Becton Dickinson), were used after having been processed on one of the routine systems of the haematology laboratory (Sysmex, SE-9500). Both, pathological and normal samples (the latter representing the control/reference groups) were collected and stored at room temperature (1822C). Pathological samples for the study were selected when showing a positive flag for WBC on the SE-9500 (Blasts?, Imm Gran?, Left Shift?, Aty/Abn Lymph?, Abn Lymph/Aged?). If no flags were present and percentage and absolute values for all parameters were normal, then the sample was included in the control/reference group. The reference ranges in this study have been adapted to those established in our laboratory except for Blasts, IG and the IMI count which had to be fixed anew due to the much higher analytical sensitivity of the analyser compared to visual microscopy. Reference ranges as listed in Table 4 have been used to analyse both the results of the XE-2100 and the microscopic differentiation. Newly introduced reference ranges are displayed in italics. The reference range for myeloblasts, promyelocytes, myelocytes and metamyelocytes is 0 (routine). The reference range for IMI-count is composed of the sum of the reference ranges for IG and myeloblasts.
average of the values above the fixed limits represents the total precision for each sub-population of the WBC count (total SD, total CV). Secondly, from the first two measurements of the same samples the total precision has been calculated by analysis of variance (ANOVA). The results then were compared to those of the precision profiles.
Accuracy of WBC differentiation
The accuracy of WBC differentiation and of detection of immature myeloid precursors on the XE-2100 has been analysed by measuring 153 pathological samples within 2 hours of sample collection and comparing the results with those of the visual differential. Passing / Bablock, linear regression and correlation coefficient have been calculated.
Microscopic differential WBC count
For the determination of accuracy, from each sample two spun smears (Horizonter, Hettich) were prepared within two hours of sample collection. The smears were stained by the May-Grnwald-Giemsa (Pappenheim) method. The smears were distributed to several technical assistants of the haematology laboratory who performed 500 cell-differentials on each under routine conditions.
Precision
The precision of the XE-2100 in counting WBC and differentiating the sub-populations has been determined for pathological and for normal samples in two different ways. All measurements were performed within 2 hours of sample collection. First, the standard deviation (SD) and coefficient of variation (CV) profiles have been determined by 10 measurements each from samples representative of the range encountered in clinical practice. The variations of those different samples were checked for equivalence. The results obtained caused us to fix limits that made CV and SD not equivalent when those limits were undercut. The
RESULTS
Precision
First, the precision profiles, i.e., CV and SD profiles for the absolute WBC counts were determined. For that purpose normal, leukopenic and pathological samples were utilised. Fig. 1 displays the CV of the absolute results. As expected the CV increased for leukopenic samples. However, even in extremely low WBC # a CV of only
11
Sysmex Journal International Vol.11 No.1 (2001)
8% was found representing a highly acceptable precision. 2.5 109/L has been fixed as the upper limit for a sample to be classified as leukopenic and thus not included in the total CV determination. It should be noted that all leukopenic samples have also been excluded from the calculation of the total precision of the individual WBC sub-populations. Fig. 2 shows the SD as function of the absolute values for pathological, normal and leukopenic samples. For the calculation of total SD of WBC the leukopenic samples have been excluded (lower limit for normal: 2.5 109/L). A similar study was performed using the absolute NEUT #. Figs. 3 (CV) and 4 (SD) show the precision data for NEUT. Here, as well, the total-CV when considering the sample exceeding the fixed cut-off shows a maximum of 4% and on average is as low as 1.3%. The XE-2100 thus performs absolute NEUT # with very high precision. Since the differentiation of LYMPH and MONO is technically challenging those two cell populations were considered initially as the sum of both and analysed accordingly. Fig. 5 (CV) and 6 (SD) display the imprecision above the cut-off level of 0.5 109/L. This is slightly higher at 34%, however these CV values are very acceptable from a clinical point of view. Figs. 7 and 8 show the CV- and SD-profiles respectively for LYMPH at concentrations > 0.5 109/L. A CV of ~5% has been obtained. Figs. 9 and 10 reflect the CV and the SD for MONO, respectively. Not unexpectedly the MONO differentiation shows the highest imprecision. This results from, on one hand, the low concentration in the peripheral blood, and, on the other hand, by its well recognised instability over time. Nevertheless, a surprisingly low total impreci-
sion of 8% and 12% is found. Figs. 11 (CV) and 12 (SD) show the precision profiles for EO. In addition we have studied the innovative sub-populations, IG and IMI counts. Precision studies for IG are illustrated in Figs. 13 (CV) and 14 (SD). At a concentration of 0.025 IG per 109/L a CV of around 20% was observed however this rapidly increases not surprisingly at still lower concentrations. Finally the precision of the IMI-count has been analysed and is displayed in Figs. 15 (CV) and 16 (SD). Figs. 17 (CV) and 18 (SD) display the precision profiles for proportional (percentage) measurement values for NEUT. At first glance these appear unsatisfactory in leukopenic samples, but in reality only serve to highlight the fallacy of statistical treatment on proportional (relative or percentage) numbers. As a result it was decided not to perform profiles on proportional numbers for other cell types. Unfortunately, in doctors offices, in clinics and on the wards particularly of smaller hospitals it is still common practice to report the differential WBC count in proportional values (percentages) even though such practice can be clinically misleading. Table 5 indicates the measurement range of absolute and percentage values for determination of total precision. Tables 6 and 7 comprehensively display the calculated SD and CV of our study and the variance analyses of both the absolute and the percentage measurement values. The CV for the variance analysis of the different WBC subtypes varies from 1% to 8%. Only in case of BASO and IG are higher CV values around 20% found. All our experimental results are within the specifications claimed by the manufacturer (Table 8).
10.0
0.50
9.0
8.0
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
0.40
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
7.0
5.0
4.0
SD (109/L)
0.0 5.0 10.0 15.0 20.0 25.0 30.0 35.0 40.0 45.0 50.0 55.0 60.0
6.0
0.30
CV (%)
0.20
3.0
2.0
0.10
1.0
0.0
0.00 0.0 5.0 10.0 15.0 20.0 25.0 30.0 35.0 40.0 45.0 50.0 55.0 60.0
WBC (109/L)
WBC (109/L)
Fig. 1 Precision profile of WBC-count-CV as function of absolute values
Fig. 2 Precision profile of WBC-count-SD as function of absolute values
12
Sysmex Journal International Vol.11 No.1 (2001)
40.0
0.50
35.0
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
0.40
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
30.0
25.0
20.0
SD (109/L)
0.0 2.5 5.0 7.0 10.0 12.5 15.0 17.5 9 20.0 22.5 25.0 27.5 30.0
0.30
CV (%)
0.20
15.0
10.0 0.10 5.0
0.0
0.00 0.0 2.5 5.0 7.0 10.0 12.5 15.0 17.5 20.0 22.5 25.0 27.5 30.0
NEUT (10 /L)
NEUT (109/L)
Fig. 3 Precision profile for NEUT-count-CV as function of absolute values
40.0 0.50
Fig. 4 Precision profile for NEUT-count-SD as function of absolute values
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
35.0
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
0.40
30.0
25.0
20.0
SD (109/L)
0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5 4.0 4.5 5.0
0.30
CV (%)
0.20
15.0
10.0 0.10 5.0
0.0
0.00 0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5 4.0 4.5 5.0
LYMPH and MONO (109/L)
LYMPH and MONO (109/L)
Fig. 5 Precision profile of LYMPM+MONO-count-CV as function of absolute values
40.0
Fig. 6 Precision profile of LYMPM+MONO-count-SD as function of absolute values
0.50
35.0
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
0.40
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
30.0
25.0
20.0
SD (109/L)
0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5 4.0 4.5 5.0
0.30
CV (%)
0.20
15.0
10.0 0.10 5.0
0.0
0.00 0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5 4.0 4.5 5.0
LYMPH (109/L)
LYMPH (109/L)
Fig. 7 Precision profile of LYMPH-count-CV as function of absolute values
Fig. 8 Precision profile of LYMPH-count-SD as function of absolute values
13
Sysmex Journal International Vol.11 No.1 (2001)
40.0
0.50
35.0
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
0.40
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
30.0
25.0
20.0
SD (109/L)
0.30
CV (%)
0.20
15.0
10.0 0.10 5.0
0.0 0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5 4.0 4.5 5.0
0.00 0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5 4.0 4.5 5.0
MONO (109/L)
MONO (109/L)
Fig. 9 Precision profile of MONO-count-CV as function of absolute values
80.0 0.10
Fig. 10 Precision profile of MONO-count-SD as function of absolute values
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
70.0
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
0.08
60.0
50.0
40.0
SD (109/L)
0.0 0.1 0.2 0.3 0.4 0.5
9
0.06
CV (%)
0.04
30.0
20.0 0.02 10.0
0.0 0.6 0.7 0.8 0.9 1.0
0.00 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0
EO (10 /L)
EO (109/L)
Fig. 11 Precision profile of EO-count-CV as function of absolute values
160.0 0.10
Fig. 12 Precision profile of EO-count-SD as function of absolute values
pathologic samples normal samples lower limit for determination of precision profiles
140.0
pathologic samples normal samples lower limit for determination of precision profiles
0.08
120.0
100.0
80.0
SD (109/L)
0.05 0.10 0.15 0.20 0.25 0.30 0.35 0.40 0.45 0.50
0.06
CV (%)
0.04
60.0
40.0 0.02 20.0
0,0 0.00
0,00 0.00
0.05
0.10
0.15
0.20
0.25
0.30
0.35
0.40
0.45
0.50
IG (109/L)
IG (109/L)
Fig. 13 Precision profile of IG-count-CV as function of absolute values
Fig. 14 Precision profile of IG-count-SD as function of absolute values
14
Sysmex Journal International Vol.11 No.1 (2001)
160.0
0.10
140.0
pathologic samples normal samples lower limit for determination of precision profiles
0.08
pathologic samples normal samples lower limit for determination of precision profiles
120.0
100.0
80.0
SD (109/L)
0.05 0.10 0.15 0.20 0.25 0.30 0.35 0.40 0.45 0.50
0.06
CV (%)
60.0
0.04
40.0 0.02 20.0
0.0 0.00
0.00 0.00
0.05
0.10
0.15
0.20
0.25
0.30
0.35
0.40
0.45
0.50
IMI (109/L)
IMI (109/L)
Fig. 15 Precision profile of IMI-count-CV as function of absolute values
Fig. 16 Precision profile of IMI-count-SD as function of absolute values
40.0
35.0
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
5.0
4.0
pathologic samples normal samples leukopenic samples lower limit for determination of precision profiles
30.0
25.0 3.0
CV (%)
20.0
SD (%)
2.0 1.0 0.0 10.0 20.0 30.0 40.0 50.0 60.0 70.0 80.0 90.0 100.0 0.0 0.0 10.0 20.0 30.0 40.0 50.0 60.0 70.0 80.0 90.0 100.0
15.0
10.0
5.0
0.0
NEUT (%)
NEUT (%)
Fig. 17 Precision profile of NEUT-count-CV as function of percentage values
Fig. 18 Precision profile of NEUT-count-SD as function of percentage values
Table 5 Measurement range of absolute and percentage values for determination of total precision Absolute measurement values Parameter Limit (109/L) WBC# NEUT# NEUT&# LY+MO# LYMPH# MONO# EO# BASO# IG# IMI# >2.50 >1.00 >1.00 >0.50 >0.50 >0.25 >0.10 >0.025 >0.025 >0.025 Range Mean Max Min Parameter Limit (%) Percentage measurement values Range Mean Max Min
9.69 7.11 7.08 2.30 1.62 0.79 0.32 0.072 0.083 0.103
28.60 26.79 26.77 4.57 3.33 1.77 0.69 0.358 0.205 0.392
4.24 2.03 1.93 0.65 0.61 0.27 0.11 0.028 0.032 0.030
NEUT% NEUT&% LY+MO% LYMPH% MONO% EO% BASO% IG% IMI%
> 10.0 > 10.0 > 5.0 > 5.0 > 2.5 > 1.0 > 0.25 > 0.25 > 0.25
68.92 68.57 28.99 21.70 9.22 3.28 0.86 0.80 1.26
93.67 93.58 70.77 42.28 32.46 11.25 2.52 1.66 3.04
33.75 32.08 6.26 5.58 3.45 1.07 1.25 0.26 0.25
15
Sysmex Journal International Vol.11 No.1 (2001)
Table 6 Total-SD and -CV from precision profiles and from variance analysis of absolute measurement values Included in the values from the profiles are the highest and the lowest measurement values for SD and CV. SD from Precision profiles SD (109/L) 0.114 0.096 0.097 0.062 0.064 0.063 0.018 0.013 0.012 0.015 Max Min Variance analysis SD CV (%) 1.29 1.61 1.63 2.94 4.48 8.25 6.91 20.34 15.18 20.20 CV from Precision profiles Max Min Variance analysis CV
Parameter WBC# NEUT# NEUT&# LY+MO# LYMPH# MONO# EO# BASO# IG# IMI#
n 46 46 46 46 43 46 23 35 16 22
0.230 0.241 0.244 0.122 0.128 0.159 0.034 0.033 0.028 0.032
0.039 0.031 0.031 0.016 0.017 0.018 0.008 0.004 0.004 0.005
0.105 0.090 0.091 0.056 0.074 0.070 0.018 0.011 0.017 0.020
2.60 3.35 3.49 8.26 14.01 13.37 14.08 41.26 23.77 49.35
0.33 0.54 0.55 0.76 0.84 2.85 2.50 8.43 8.15 6.65
1.09 1.27 1.29 2.44 4.59 8.89 5.78 14.89 20.10 17.97
Table 7 Total-SD and CV from precision profiles and variance analysis of the relative measurement values The values of the profiles also include the highest and lowest SD- and CV-values measured. SD from Precision profiles SD (%) 0.64 0.65 0.66 0.80 0.71 0.22 0.17 0.12 0.21 Max Min Variance analysis SD CV (%) 1.03 1.05 2.40 4.27 8.00 8.94 22.44 17.20 20.26 CV from Precision profiles Max Min Variance analysis CV
Parameter NEUT% NEUT&% LY+MO% LYMPH% MONO% EO% BASO% IG% IMI%
n 46 46 46 43 46 23 35 16 22
1.46 1.46 2.73 2.36 1.71 0.53 0.64 0.24 0.58
0.14 0.10 0.14 0.15 0.17 0.06 0.06 0.04 0.05
0.66 0.69 0.66 0.95 0.81 0.21 0.16 0.16 0.35
3.36 3.75 5.55 17.81 13.06 24.94 59.57 49.48 48.99
0.18 0.13 0.52 1.03 2.23 1.56 8.13 5.33 6.15
0.96 1.00 2.26 4.38 8.77 6.47 19.25 19.76 25.57
Table 8 Manufacturers precision specifications Precision of blood cell differentiation with normal fresh samples is measured 10 times or more. Listed are the maximum acceptable CV% and the validity range of the measurements. If no range is indicated then, in case the CV% is exceeded between two measurement values the maximum deviation as indicated is supposed to occur. The relative measurements are only valid if the WBC count is > 4.00 109/L. Absolute measurement values Parameter WBC# NEUT# LYMPH# MONO# EO# BASO# CV (%) < 3.0 < 8.0 < 8.0 <20.0 <25.0 <40.0 Limit (109/L) >4.00 >1.20 >0.60 >0.20 0.12 0.06 Tolerable deviation Parameter Relative measurement values CV (%) Limit (%) Tolerable deviation
NEUT% LYMPH% MONO% EO% BASO%
< 8.0 < 8.0 <20.0 <25.0 <40.0
> 30.0 > 15.0 > 5.0 1.5 1.0
16
Sysmex Journal International Vol.11 No.1 (2001)
Accuracy of WBC differential
The accuracy of WBC sub-population enumeration and that of their myeloid precursors has been studied by comparison with a reference method based on visual microscopy. For that purpose samples with normal, reduced and increased WBC counts and pathological samples with marked left shift have been analysed. Comparison of the different cell types was done by calculation of Passing / Bablock and CV. Fig. 19 displays the correlation for the absolute NEUT #. As NEUT the system classifies segmented NEUT, band cells (stab), and IG. With a slope of 0.999 and an intercept of only 0.105 the correlation of the results of both methods is outstanding. Equally impressive is the correlation coefficient of 0.9986. This can be explained by the very low total imprecision of the NEUT # of the analyser (CV% = 1.27%) and, in case of high cell concentrations, the acceptable precision also for the visual differential. Fig. 20 illustrates the comparison of the percentage NEUT # with visual microscopy. As expected linear regression and intercept are less good than for absolute counts. This is due to the high percentage of NEUT in the samples. The results obtained for the corrected neutrophil counts (NEUT&) are almost identical to the results of the neutrophil count itself (NEUT). This is due to the relatively low percentage of IG as compared to the high percentage of segmented NEUT and band cells. This comparison is not illustrated however linear regression and correlation coefficient are listed in Table 9. Figs. 21 and 22 display the method comparison for LYMPH. For LYMPH, despite the technically challenging differentiation from MONO, an excellent linear regression between the two methods has been obtained. Also, the increase in imprecision of the visual method in case of low cell concentrations had only little impact on the correlation: the correlation coefficients for the absolute counts and relative counts were 0.9865 and 0.9866, respectively. Figs. 23 and 24 illustrate the correlations for absolute and percentage MONO counts. Not unexpectedly the MONO differentiation shows a worse correlation than the
LYMPH. This is due to the higher imprecision of the measurement for both the visual and the instrument rated count. Nevertheless, surprisingly good correlation coefficients have been obtained: 0.8360 for the absolute counts and 0.8629 for the percentage counts. The linear regression reveals a systematic difference between the two MONO detection methods since it is positioned significantly above the ideal function of y = x. This is for both, the absolute and the proportional count. At a concentration of 1.0 109/L or 10% MONO, respectively, the analyser detects 1013% more MONO as does the microscopy differential count. Figs. 25 and 26 illustrate the absolute and percentage comparisons for EO. Considering the very low EO concentration of the blood samples the measurement values of the two methods show an excellent correlation. Figs. 27 and 28 show the respective comparisons for BASO. The XE-2100 showed a higher sensitivity compared to the visual differential. As anticipated the correlation coefficients are poor due to the high imprecision of both methods (particularly the visual differential). Subsequently we focussed on the myeloid precursors. The system is capable of detecting myeloid precursors by the simultaneous and parallel application of different measurement principles (see methods): in the DIFF-channel the IG are quantified while the IMI-channel generates the supportive qualitative parameter of the IMI-count.
Immature Granulocytes (IG)
Since the detection of IG is of great clinical importance and has to be carried out quite frequently but hitherto only possible by visual microscopy, the ability of the XE2100 in that respect has been analysed with great interest. The accuracy of the newly launched IG count was examined. Initially while the correlation between the XE-2100 and the visual differential was good, the slope of the linear regression was < 0.5 according to Passing/Bablock. A possible cause for this low slope may have been misadjustment of standard sensitivity which would impact on
Table 9 Summary of comparability studies For the IG# also the results excluding the promyelocytes are listed (IG#*). IG data before re-adjustment of sensitivity. For the IMI# also the results excluding the outliers are shown (IMI# *). Absolute measurement values Parameter NEUT# NEUT&# LYMPH# MONO# EO# BASO# IG# IG# * IMI# IMI# * Slope 0.999 0.997 0.975 1.121 0.963 1.625 0.438 0.467 1.626 1.393 y-axis intercept -0.105 -0.043 0.034 0.009 0.000 0.010 0.013 0.017 0.011 0.015 Corr.coeff. (r) 0.9986 0.9985 0.9865 0.8360 0.9658 0.5098 0.8509 0.8473 0.7279 0.9428 Parameter NEUT% NEUT&% LYMPH% MONO% EO% BASO% Proportional measurement values Slope 1.049 1.017 1.010 1.044 0.987 1.633 y-axis intercept -5.001 -1.915 0.045 0.610 0.000 0.058 Corr.coeff. (r) 0.9874 0.9875 0.9866 0.8629 0.9542 0.5798
17
Sysmex Journal International Vol.11 No.1 (2001)
the detection of IG. Following readjustment, a much improved correlation and slope were found when comparing the two methods (Fig. 29). These results are also in agreement with results as found in another study6).
IMI Count
Even though the XE-2100 only utilizes the IMI-information qualitatively and the results are not regularly displayed, it is nevertheless an important measure for total myeloid precursors (myeloblasts, promyelocytes, myelocytes, metamyelocytes) (see methods below). Figs. 30, 31 and 32 illustrate a number of experimental comparisons. In Fig. 30 straight comparison of the IMI-count with the visual differential is illustrated. Here the steep slope (1.626) indicates the detection of additional sub-populations in the IMI-channel which are omitted from the IMI definition. This assumption is confirmed in Fig. 30 in which two sub-populations of paired values are present: one is located around the Passing / Bablock linear regression while the second is aligned to the y-axis and consists of badly correlating values (outliers in circles). Those
paired values are from samples with left shift exclusively limited to the stage of band cells (stab). In Fig. 31 the comparison has been repeated but this time excluding those blood samples which showed an absolute band cell count > 0.3 on microscopy but only a few more immature forms. The slope of the linear regression decreases from 1.626 to 1.393 and the correlation coefficient improves to a very good value of 0.9428. Fig. 32 finally illustrates the comparison between IGcount from the DIFF-channel and the IMI-count from the IMI-channel. As already observed in Fig. 30 and now also in Fig. 32, the paired values aligned with the y-axis are observed. Yet again they derive almost exclusively from blood samples with a marked left shift but without other immature cells. In Table 9 the results of our comparability analyses are displayed comprehensively in total. Table 10 shows the results of an UK study5) for comparison. It can be seen that the results for IG from the UK study correspond well with our results obtained after re-adjustment of the standard sensitivity. All results satisfy the manufacturer performance claims which are displayed in Table 11.
40.0
1.6
8.5 NEUT #
100
40
85
90 35.0
80 30.0
NEUT %
85
Measurements
Measurements Upper Limits 'Normal Range
70
NEUT (XE-2100) (109/L)
Upper Limits 'Normal Range Lower Limits 'Normal Range
25.0
PB-Line
NEUT (XE-2100) (%)
Lower Limits 'Normal Range
60
PB-Line
20.0
50
40
15.0
y =0.999x - 0.105 R=0.9986
40
30 10.0
8.5
5.0
20
10
y =1.049x - 5.001 R=0.9874
0.0 0.0 5.0 10.0 15.0 20.0 25.0 30.0 35.0
1.6
40.0
0 0 10 20 30 40 50 60 70 80 90 100
Segmented Granulocytes, Bands and immature Granulocytes (Microscope) (109/L)
Segmented Granulocytes, Bands and immature Granulocytes (Microscope) (%)
Fig. 19 Absolute NEUT-count: comparison with visual microscopy
5.0
Fig. 20 Percentage NEUT-count: comparison with visual microscopy
50
0.8
4.0
20
40
4.5
LYMPH #
4.0
45
LYMPH %
40
4.0
40
LYMPH (XE-2100) (109/L)
3.5
35
Measurements
3.0
LYMPH (XE-2100) (%)
Measurements
30
Upper Limits 'Normal Range Lower Limits 'Normal Range
Upper Limits 'Normal Range Lower Limits 'Normal Range
2.5
PB-Line
25
PB-Line
2.0
20
20
1.5
15
1.0
y = 0.975x + 0.034 R= 0.9865 0.8
10
y = 1.010x - 0.045 R= 0.9866
5
0.5
0.0 0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5 4.0 4.5 5.0
0 0 5 10 15 20 25 30 35 40 45 50
Lymphocytes, Plasma Cells, atypical Lymphocytes and Myeloblasts (Microscope) (109/L)
Lymphocytes, Plasma Cells, atypical Lymphocytes and Myeloblasts (Microscope) (%)
Fig. 21 Absolute LYMPH-count: comparison with visual microscopy
Fig. 22 Percentage LYMPH-count: comparison with visual microscopy
18
Sysmex Journal International Vol.11 No.1 (2001)
3.0
0.08
1.00
30
10
2.7
MONO #
Measurements Upper Limits 'Normal Range
27
MONO %
2.4
24
MONO (XE-2100) (109/L)
2.1
PB-Line
1.8
MONO (XE-2100) (%)
Lower Limits 'Normal Range
21
18
Measurements Upper Limits 'Normal Range
1.5
15
Lower Limits 'Normal Range PB-Line
1.2
12
1.00
0.9
10
9
0.6
y = 1.121x + 0.009 R= 0.8360
0.3 3
y = 1.044x + 0.610 R= 0.8629 0.08 2
0 0 3 6 9 12 15 18 21 24 27 30
0,0 0,0 0.3 0.6 0.9 1.2 1.5 1.8
MONO (Microscope) (10 /L)
2.1 9
2.4
2.7
3.0
MONO (Microscope) (%)
Fig. 23 Absolute MONO-count: comparison with visual microscopy
2.0
Fig. 24 Percentage MONO-count: comparison with visual microscopy
12
0.6
1.8
11
1.6
EO #
10
EO %
9 1.4
EO (XE-2100) (109/L)
Measurements
1.2
EO (XE-2100) (%)
Measurements
7
Upper Limits 'Normal Range PB-Line
1.0
Upper Limits 'Normal Range PB-Line
0.8
0.6
0.6
3 0.4
y = 0.963x + 0.000 R= 0.9658
0.2
y = 0.987x + 0.000 R= 0.9542
0.0 0.0 0.2 0.4 0.6 0.8 1.0 1.2 1.4 1.6 1.8 2.0
0 0 1 2 3 4 5 6 7 8 9 10 11 12
EO (Microscope) (109/L)
EO (Microscope) (%)
Fig. 25 Absolute EO-count: comparison with visual microscopy
0.35
Fig. 26 Percentage EO-count: comparison with visual microscopy
3.5
0.20
BASO #
Measurements Upper Limits 'Normal Range PB-Line
3.0
2.0
BASO %
Measurements Upper Limits 'Normal Range PB-Line
0.30
BASO (XE-2100) (109/L)
0.25
2.5
0.20
0.20
BASO (XE-2100) (%)
2.0
2.0
0.15
1.5
0.10
1.0
0.05
y = 1.625x + 0.010 R= 0.5098
0.5
y = 1.633x + 0.058 R= 0.5798
0.00 0.00
0.0 0.05 0.10 0.15 0.20 0.25 0.30 0.35 0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5
BASO (109/L)
BASO (Microscope) (%)
Fig. 27 Absolute BASO-count: comparison with visual microscopy
Fig. 28 Percentage BASO-count: comparison with visual microscopy
19
Sysmex Journal International Vol.11 No.1 (2001)
0.80
0.05
1.50
0.075
0.70 1.25
Measurements
0.60
Upper Limits 'Normal Range
IMI (XE-2100) (109/L)
IG (XE-2100) (109/L)
Measurements PB-Line
0.50
PB-Line
1.00
0.40
0.75
0.30
0.50
0.20
y = 0.7207 + 0.0035 R= 0.7949
0.25
y = 1.626x + 0.011 R= 0.7279
0.10
0.05
0.00 0.00 0.00 0.00
0.075
0.25 0.50 0.75 1.00 1.25 1.50
0.20
0.40
0.60
0.80
1.00
1.20
Promyelocytes, Myelocytes, Metamyelocytes (Microscope) (109/L)
Myeloblasts, Promyelocytes, Myelocytes and Metamyelocytes (Microscope) (109/L)
Fig. 29 Absolute IG count: comparison with visual microscopy
Fig. 30
Absolute IMI-count: comparison with visual microscopy differential which counted band cells and other immature forms
Measurements Upper Limit (IMI)
1.50
2.00
0.075
1.75
0.050
Lower Limit (IG) PB-Line
1.25 1.50
Measurements
IMI (XE-2100) (109/L)
Upper Limits 'Normal Range
1.00
PB-Line
IMI # (XE-2100) (109/L)
1.25
0.75
1.00
0.75
0.50
y = 1.393x + 0.015 R= 0.9428
0.25
0.50
y = 3.800x 0.056 R= 0.6926
0.25
0.075
0.00 0.00 0.25 0.50 0.75 1.00 1.25 1.50 0.00 0.00 0.25 0.50 0.75 1.00 1.25 1.50 1.75
0.075
2.00
Myeloblasts, Promyelocytes, Myelocytes and Metamyelocytes (Microscope) (109/L)
IG #(XE-2100) (109/L)
Fig. 31
Absolute IMI-count: comparison with visual microscopy differential. Outliers consisting of samples with band cells > 0.3 excluded.
Fig. 32 Comparison of absolute IG-count and absolute IMI-count
Table 10 Results of the comparability study performed in University College London Hospital, London5) Relative measurement values Parameter NEUT% LYMPH% MONO% EO% BASO% IG% Slope 0.938 0.961 0.936 0.909 0.940 0.744 y-axis intercept 0.094 0.108 0.157 0.046 0.041 0.065 Corr.coeff. (r) 0.9812 0.9887 0.6470 0.8096 0.1983 0.8173
Table 11 Accuracy of blood cell differentiation Manufacturers specifications. Displayed is the maximum tolerable mean value of the differences from the result of the standard system and the correlation coefficient with the reference method if 100 or more normal samples are analysed. Relative measurement values Parameter NEUT% LYMPH% MONO% EO% BASO% Maximum tolerable deviation (%) 3.0% 3.0% 2.0% 1.0% 1.0% Corr.coeff. (r) >0.90 >0.90 >0.75 >0.80 >0.50
20
Sysmex Journal International Vol.11 No.1 (2001)
DISCUSSION
As shown by our data the XE-2100 possesses outstanding precision. The performance of the instrument far exceeds the precision claims made by he manufacturer which. Only in cases of low absolute and proportional values not unexpectedly does the imprecision increase. For severely leukopenic patients it does not matter that much if the values show greater imprecision. In such circumstances the appearance of blast cells has clinical relevance. But in such case the purely binary statement (yes/no = pathological/non-pathological) is absolutely sufficient. Subsequently, additional diagnostic procedures such as bone marrow puncture (morphology/ flow cytometry, immunophenotyping and special stains) are required anyway. In addition, the highly precise counts of immature myeloid cells will prove extremely valuable. It might be anticipated that the rapid identification and precise enumeration of immature myeloid cells in the peripheral blood will contribute significantly to the diagnosis of infectious diseases. Should this become evident it would then be possible to come to important clinical decisions by just performing a simple automated differential. Additionally, we would expect that therapeutic monitoring would be of great clinical benefit. Such studies are currently underway in our institution. The present study also raises the question of reference ranges in health. The fact that some samples from apparently healthy individuals show a low concentration of immature cells in rare instances necessitates a re-evaluation of reference ranges in health. Such cells are not detected in the frequently performed routine clinical dif-
ferential of 2 50 or 2 100 WBC. That leads to a false reference value of 0. The experience and the insight gained with new technology analysers such as the Sysmex, XE-2100 prompts such studies. In summary, the Sysmex, XE-2100 impresses the user with its outstanding precision for the 5-part differential. In addition, the system generates precise quantitative data on immature myeloid precursors and other immature elements. With sophisticated flagging hitherto unrecognisable pathological conditions are certainly detectable. However, in the present study this has not been evaluated any further. Since this technical evaluation resulted in an outstanding performance, clinical studies are highly recommended.
References 1) Inoue H: Overview of automated hematology analyzer XE-2100. Sysmex J Int, 9: 58-64, 1999. 2) Sakata T: Reagent characteristics in the XE-2100 NRBC channel. Sysmex J Int, 10: 41-46, 2000. 3) Matsumoto H: The technology of reagents in the automated hematology analyzer Sysmex XE-2100 -red fluorescence reaction-. Sysmex J Int, 9: 179-185, 1999. 4) Goossens W, Van den Driessche M, Brusselmanns C, Vandekerckhove P: Optimisation of the flagging criteria on the Sysmex SE-9500. Sysmex J Int, 10: 18-20, 2000. 5) Briggs C, et al.: Performance evaluation of the Sysmex XE-2100, automated haematology analyser. Sysmex J Int, 9: 113-119, 1999. 6) Briggs C, et al.: New quantitative parameters on a recently introduced automated blood cell counter - the XE-2100. Clin Lab Haem, 22: 345-350, 2000.
21
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- 019 Age-Dependent Reference Ranges For AutomatedDocument7 pages019 Age-Dependent Reference Ranges For Automatedblanket_thNo ratings yet
- 015 Performance of An Automated Immature GranulocyteDocument7 pages015 Performance of An Automated Immature Granulocyteblanket_thNo ratings yet
- 027 Use of The Haemopoietic Progenitor Cell Count of The SysmexDocument7 pages027 Use of The Haemopoietic Progenitor Cell Count of The Sysmexblanket_thNo ratings yet
- 020 Evaluation of The Sysmex XT-2000iV Hematology Instrument ForDocument31 pages020 Evaluation of The Sysmex XT-2000iV Hematology Instrument Forblanket_thNo ratings yet
- 014 Immature Granulocyte Measurement Using The SysmexDocument5 pages014 Immature Granulocyte Measurement Using The Sysmexblanket_thNo ratings yet
- 022 Leucocyte Differentiation With The XT-SeriesDocument6 pages022 Leucocyte Differentiation With The XT-Seriesblanket_thNo ratings yet
- 025 Automated UrinalysisDocument6 pages025 Automated Urinalysisblanket_thNo ratings yet
- 028 Improved Performance of The AutomatedDocument6 pages028 Improved Performance of The Automatedblanket_thNo ratings yet
- 026 Evaluation of The Sysmex UF-100 Urine Cell AnalyzerDocument4 pages026 Evaluation of The Sysmex UF-100 Urine Cell Analyzerblanket_thNo ratings yet
- 018 An Evaluation of The Performance of Sysmex XE-2100 inDocument7 pages018 An Evaluation of The Performance of Sysmex XE-2100 inblanket_thNo ratings yet
- 023 Evaluation of The Sysmex UF-100 AutomatedDocument4 pages023 Evaluation of The Sysmex UF-100 Automatedblanket_thNo ratings yet
- 012 Analysis of Reticulocyte Parameters On The Sysmex XEDocument8 pages012 Analysis of Reticulocyte Parameters On The Sysmex XEblanket_thNo ratings yet
- 024 Evaluation of The Sysmex UF-1000i For The DiagnosisDocument6 pages024 Evaluation of The Sysmex UF-1000i For The Diagnosisblanket_thNo ratings yet
- 022 Leucocyte Differentiation With The XT-SeriesDocument6 pages022 Leucocyte Differentiation With The XT-Seriesblanket_thNo ratings yet
- 017 The New Hematology Analyzer Sysmex XE-2100Document6 pages017 The New Hematology Analyzer Sysmex XE-2100blanket_thNo ratings yet
- 016 A Method For Optimizing and Validating InstitutionDocument6 pages016 A Method For Optimizing and Validating Institutionblanket_thNo ratings yet
- 009the Automated Nucleated Red Cell Count On The Sysmex XE-2100Document5 pages009the Automated Nucleated Red Cell Count On The Sysmex XE-2100blanket_thNo ratings yet
- Precision and Accuracy of The Leukocyte DifferentialDocument14 pagesPrecision and Accuracy of The Leukocyte Differentialblanket_thNo ratings yet
- 010new Red Cell Parameters On The Sysmex XeDocument1 page010new Red Cell Parameters On The Sysmex Xeblanket_thNo ratings yet
- 008the Technology of ReagentsDocument7 pages008the Technology of Reagentsblanket_thNo ratings yet
- 013 Estimated Platelet and Differential LeucocyteDocument8 pages013 Estimated Platelet and Differential Leucocyteblanket_thNo ratings yet
- 011 Evaluation of The Automated Immature Granulocyte CountDocument1 page011 Evaluation of The Automated Immature Granulocyte Countblanket_thNo ratings yet
- Platelet Counting by The Coulter LH 750, Sysmex XE 2100Document7 pagesPlatelet Counting by The Coulter LH 750, Sysmex XE 2100blanket_thNo ratings yet
- 006the New Reticulocyte Parameter (RET-Y) of The SysmexDocument7 pages006the New Reticulocyte Parameter (RET-Y) of The Sysmexblanket_thNo ratings yet
- 005 Performance Evaluation of The Sysmex XT-2000iDocument9 pages005 Performance Evaluation of The Sysmex XT-2000iblanket_thNo ratings yet
- 004 Evaluation of Two Sysmex XE-2100 AnalyzersDocument7 pages004 Evaluation of Two Sysmex XE-2100 Analyzersblanket_thNo ratings yet
- 002performance Evaluation of The Sysmex XE-2100™Document7 pages002performance Evaluation of The Sysmex XE-2100™blanket_thNo ratings yet
- 001 Potential Utility of The New Sysmex XE 5000Document6 pages001 Potential Utility of The New Sysmex XE 5000blanket_thNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Anemia and low platelet countDocument4 pagesAnemia and low platelet countCloudCom TechnologyNo ratings yet
- Hematology (CBC Profile) : MR. No. 21011543546 Lab No. Collection: Name: Gender: Male Age: 66 YearsDocument1 pageHematology (CBC Profile) : MR. No. 21011543546 Lab No. Collection: Name: Gender: Male Age: 66 YearsAsif ShahNo ratings yet
- NCP 1Document5 pagesNCP 1Butchie's ParadiseNo ratings yet
- Labreport V SMSH 23 10141161 PDFDocument2 pagesLabreport V SMSH 23 10141161 PDFMohanNo ratings yet
- Micros 60 CS-CT User's ManualDocument124 pagesMicros 60 CS-CT User's ManualHenry VelásquezNo ratings yet
- MyChart - Test Details PDFDocument3 pagesMyChart - Test Details PDFAnonymous iy0yzUJOOrNo ratings yet
- Rent to Own Hematology Analyzer Precision CB9000Document4 pagesRent to Own Hematology Analyzer Precision CB9000Karina SantosNo ratings yet
- Soppi 2018Document5 pagesSoppi 2018dr_joe23No ratings yet
- 1 Hema LecDocument5 pages1 Hema LecAngela ReyesNo ratings yet
- 619 EDTA Antikoagulantien USDocument1 page619 EDTA Antikoagulantien USanggaririnNo ratings yet
- Blood ReportDocument39 pagesBlood Reportputri Mentari100% (1)
- Agep Poster EadvDocument1 pageAgep Poster EadvAhmet KayaaltıNo ratings yet
- ABX Pentra 60-C Plus Analyzer - Service ManualDocument314 pagesABX Pentra 60-C Plus Analyzer - Service ManualJose Rolando Orellana Rodriguez100% (2)
- Hematological ProceduresDocument14 pagesHematological ProceduresWynlor AbarcaNo ratings yet
- NCC-61 With RET ENG - User Manual V2020 - 01 - 21 - 011900 (046-090)Document45 pagesNCC-61 With RET ENG - User Manual V2020 - 01 - 21 - 011900 (046-090)Zoulikifil Abdou KarimNo ratings yet
- Nursing Care Plan for Infection and Bleeding PrecautionsDocument6 pagesNursing Care Plan for Infection and Bleeding Precautionshayascent hilarioNo ratings yet
- Hematology I Intensive Rationale - Louise MDocument20 pagesHematology I Intensive Rationale - Louise MKai YoungNo ratings yet
- CBC H Met Complete Blood CountDocument174 pagesCBC H Met Complete Blood CountAlejandro DominguezNo ratings yet
- 1-CBC InterpretationDocument10 pages1-CBC Interpretationمصطفي خندقاويNo ratings yet
- Common Laboratory ProceduresDocument165 pagesCommon Laboratory Proceduresnursereview100% (9)
- H32 Benesphera User ManualDocument43 pagesH32 Benesphera User ManualTran BaoNo ratings yet
- Complete Blood CountDocument21 pagesComplete Blood CountKrisha Vitto100% (1)
- Universal Precautions: Treat All Blood as InfectiousDocument7 pagesUniversal Precautions: Treat All Blood as InfectiousPatrick ParconNo ratings yet
- Case Study - FractureDocument35 pagesCase Study - FractureJo-anne Cordero100% (3)
- False Increase in Hematocrit Due to Insufficient CentrifugationDocument62 pagesFalse Increase in Hematocrit Due to Insufficient CentrifugationMariel AbatayoNo ratings yet
- NCM 112 Rle Case Analysis: Care of Client With Alterations in Oxygenation (ASTHMA)Document2 pagesNCM 112 Rle Case Analysis: Care of Client With Alterations in Oxygenation (ASTHMA)Joegie ArioNo ratings yet
- Mythic 18Document84 pagesMythic 18Loai AhmedNo ratings yet
- Case AnalysisDocument1 pageCase AnalysisKatrina Jude ElleNo ratings yet
- Comprehensive Lab Test Price List for Haematology, Biochemistry, Serology, Microbiology and Hormone AssaysDocument4 pagesComprehensive Lab Test Price List for Haematology, Biochemistry, Serology, Microbiology and Hormone AssaysSUMA MANOJNo ratings yet
- Med111487409 33864299 118 79600569Document7 pagesMed111487409 33864299 118 79600569Akhil MuraliNo ratings yet