Professional Documents
Culture Documents
Water and Ion Concentration
Uploaded by
Ali TagerCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Water and Ion Concentration
Uploaded by
Ali TagerCopyright:
Available Formats
05/01/2011
Water and Solute Movement
1. Ion and Water Transport in the nephron.
Proximal Convoluted Tubule:
1) Returns water and dissolved chemicals to the bloodstream,
permeable to water and moderately permeable to most dissolved substances
including urea.
2) Na+ and glucose are co-transported across the cells of the proximal
tubule into the blood, thus returning large amounts of glucose to the
bloodstream.
Proximal
The descending part of the Loop of Henle is very permeable to water
and thus water diffuses into the interstitial fluid, concentrating the still dilute
filtrate, as the filtrate passes down the tubule.
Most of the water moves into the interstitial fluid at the start because
the filtrate is most dilute there and diffusion depends upon the difference in
water concentration between the filtrate (high water conc.) and the
interstitial fluid (lower water concentration).
-As urine moves deeper in the descending tubule, water movement
from the tubule is less, but not zero. The filtrate becomes more
concentrated, but the interstitial fluid is also more concentrated than at the
top of the tubule. Water still diffuses from the filtrate to the interstitial fluid.
The ascending portion of the Loop of Henle is quite impermeable to
water, becoming particularly so in the upper portion with a thickened wall.
-Sodium and chloride passively move out of the filtrate in the thin
portion of the ascending tubule and actively in the thick portion and the
distal tubule and into the interstitial fluid surrounding the nephron. The
water is left behind, making the filtrate more dilute again, even more dilute
than when it entered the descending tubule but with MUCH LESS VOLUME.
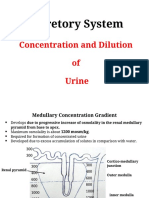
The gradient of osmolarity in the interstitial fluid is produced
by the "vasa recta" capillary network. (Blood flow enters the glomerulus
from the afferent arteriole and leaves via the efferent arteriole, and finally
goes into the "vasa recta" network of capillaries which twist and branch
around the ascending and descending tubules. The blood enters the
network at the ascending tubule and leaves from the descending
tubule, thus the blood moves in the OPPOSITE DIRECTION TO THE
URINE.)
Sodium ions pumped out of the ascending tubule enter the blood
stream, thus increasing the concentration of sodium in the blood. When the
blood reaches the inner medulla, sodium concentration in the blood is high,
causing sodium to flow out of the blood and into the interstitial fluid. Since
the inner medullary portion of the Loop of Henle is impermeable to sodium,
sodium stays in the interstitial fluid and creates the gradient of high
osmolarity in the medullary portion of the interstitial fluid and lower
osmolarity in the outer medullary and cortex regions of interstitial fluid.
Now we have set up a gradient of interstitial fluid osmolarity as a
result of the asymmetry in water permeability and sodium chloride
movement between descending and ascending tubules.
Now, the collecting duct goes "down" again, water progressively
diffuses out of the collecting duct into the more "concentrated" interstitial
fluid and the result is concentrated urine with low volume. (Eckert, Fig. 14-
34)
3. Renin-Angiotensin-Aldosterone System.
This system is helps maintain arterial blood pressure when blood
volume decreases, for example if there is blood loss.
The afferent arteriole acts as a pressure receptor, causing secretion of
renin when blood flow is low.
Low salt concentrations detected by the macula densa also cause renin
secretion. This leads to a complicated chain of events, including Angiotensin
II causing arteriolar vasoconstriction and increased blood pressure. The
adrenal gland releases Aldosterone, causing reduction in excretion of sodium
chloride and thus a decrease in water excretion. (You should know what the
following do: Macula densa, Renin, Angiotensin I and II, ACE, Aldosterone,
ADH.)
3. Diuretics cause increased output of urine, sometimes by preventing
sodium transport from the tubules.
You might also like
- Physio - Water BalanceDocument8 pagesPhysio - Water Balanceavian_rose100% (2)
- Countercurrent MultiplicationDocument4 pagesCountercurrent MultiplicationMichael Briscoe100% (1)
- L8water Balance and Concentrating and Diluting MechanismDocument15 pagesL8water Balance and Concentrating and Diluting MechanismOsama MohamedNo ratings yet
- Counter Current MechanismDocument6 pagesCounter Current MechanismDr-Atin Kumar SrivastavaNo ratings yet
- Counter Current MechanismDocument21 pagesCounter Current MechanismAdnan BasheerNo ratings yet
- Counter Current MechanismDocument33 pagesCounter Current MechanismPhysiology by Dr Raghuveer67% (3)
- 6 Urine ConcentrationDocument28 pages6 Urine ConcentrationRama BiNo ratings yet
- Kidney NotesDocument5 pagesKidney Notesnad2samNo ratings yet
- Kidney Function: What Do The Kidneys Do?Document4 pagesKidney Function: What Do The Kidneys Do?A Mazid Zabir IINo ratings yet
- Kuliah 3. Pengaturan Osmolalitas UrinDocument19 pagesKuliah 3. Pengaturan Osmolalitas UrinAnnisa DamayantiNo ratings yet
- L8-Urine Conc.Document15 pagesL8-Urine Conc.Bryn MasvaureNo ratings yet
- Urine Concentration and DilutionDocument7 pagesUrine Concentration and DilutionHussein Ali AljamaliNo ratings yet
- A2 Ultrafiltration and Selective ReabsorptionDocument22 pagesA2 Ultrafiltration and Selective ReabsorptionPouyaNonubisNo ratings yet
- AP Biology Regulation Test ReviewDocument4 pagesAP Biology Regulation Test ReviewborntobewilderNo ratings yet
- IAL Biology SB2 Answers 7CDocument7 pagesIAL Biology SB2 Answers 7CsalmaNo ratings yet
- Ultrafiltration and Selective ReabsorptionDocument22 pagesUltrafiltration and Selective ReabsorptionKemoy FrancisNo ratings yet
- 1.4 Virtual Patient - Elizabeth Harding: Describe The Structure of The NephronDocument7 pages1.4 Virtual Patient - Elizabeth Harding: Describe The Structure of The NephronAbdullah RajaNo ratings yet
- Mammals and Birds Secrete A Hypertonic UrineDocument2 pagesMammals and Birds Secrete A Hypertonic UrineTommy HardiantoNo ratings yet
- Distal Convoluted Tubules, Counter Current Mechanism, MicturitionDocument94 pagesDistal Convoluted Tubules, Counter Current Mechanism, MicturitionSarah BirechNo ratings yet
- Urine Ingredient Analysis: Name: Yunita Punarisma Class: XI IA 3/ 15Document21 pagesUrine Ingredient Analysis: Name: Yunita Punarisma Class: XI IA 3/ 15ladylomoNo ratings yet
- KidneyoutlineDocument33 pagesKidneyoutlineapi-273417637No ratings yet
- 7th Lecture - Diluted and Concentrated UrineDocument9 pages7th Lecture - Diluted and Concentrated UrinewarikogatumaNo ratings yet
- ExcretionDocument2 pagesExcretionGyunho KimNo ratings yet
- Chapter 24. The Kidney.: 1. The Structure and Function of The NephronDocument8 pagesChapter 24. The Kidney.: 1. The Structure and Function of The NephronjeskevandiemenNo ratings yet
- RenalphysiologyDocument178 pagesRenalphysiologyanisreeNo ratings yet
- Proximal Tubule Distal Tubule: Nutrients Nacl Hco H O K Nacl H O HcoDocument18 pagesProximal Tubule Distal Tubule: Nutrients Nacl Hco H O K Nacl H O HcogajenraoNo ratings yet
- NephronDocument2 pagesNephronJohn SmithNo ratings yet
- Chapter 13: OsmoregulationDocument9 pagesChapter 13: Osmoregulationabrnrd56No ratings yet
- Urinalysis and Body FluidsDocument54 pagesUrinalysis and Body FluidsabdishakurNo ratings yet
- Excretion (Continued)Document9 pagesExcretion (Continued)t0000123No ratings yet
- Kidney and OsmoregulationDocument25 pagesKidney and Osmoregulationsoyoung jinNo ratings yet
- 5) Urine ConcentrationDocument14 pages5) Urine ConcentrationRaja AmiruddinNo ratings yet
- Urine ConcentrationDocument15 pagesUrine ConcentrationRamadan PhysiologyNo ratings yet
- ORALREVALIDADocument2 pagesORALREVALIDAalthea jade villadongaNo ratings yet
- Chapter 19 Excretory Products and Their EliminationDocument27 pagesChapter 19 Excretory Products and Their Eliminationamit lakraNo ratings yet
- Ansc 22 The Excretory SystemDocument11 pagesAnsc 22 The Excretory SystemJohn BildanNo ratings yet
- Excretion in MammalsDocument17 pagesExcretion in MammalsKaynat JavedNo ratings yet
- Urine Formation - Human Excretory SystemDocument13 pagesUrine Formation - Human Excretory SystemRaj KumarNo ratings yet
- Countercurrent MultiplicationDocument2 pagesCountercurrent Multiplicationeclipsed_moon3535No ratings yet
- Form'n'Function IIDocument9 pagesForm'n'Function IIRushana SadaqatNo ratings yet
- Thirst Center: Topic OutlineDocument7 pagesThirst Center: Topic OutlinePMSabioNo ratings yet
- Concentration of Urine: Maj DR Shavana R.L RanaDocument22 pagesConcentration of Urine: Maj DR Shavana R.L RanaChandan Sah100% (1)
- THE URINARY SYSTEM Anatomy and PhysiologyDocument29 pagesTHE URINARY SYSTEM Anatomy and PhysiologyYatuwa LydiaNo ratings yet
- M - 126 Structure of Nephron and Function of The Kidney PDFDocument4 pagesM - 126 Structure of Nephron and Function of The Kidney PDFDr. Tapan Kr. Dutta100% (1)
- The Counter Current Mechanisms in The KidneyDocument2 pagesThe Counter Current Mechanisms in The Kidneygoodjenny872No ratings yet
- The Counter Current Mechanisms in The KidneyDocument1 pageThe Counter Current Mechanisms in The KidneySirisha CkvNo ratings yet
- Renal System 6 1Document30 pagesRenal System 6 1gaurav singhNo ratings yet
- 11.3 - The KidneyDocument7 pages11.3 - The KidneyraghadNo ratings yet
- Counter Current MechanismDocument39 pagesCounter Current MechanismRAGHUNANDAN R100% (2)
- Chapter 19 - The Urinary System: Fluid and Electrolyte BalanceDocument28 pagesChapter 19 - The Urinary System: Fluid and Electrolyte BalanceSara SabraNo ratings yet
- Notes For HomeostasisDocument21 pagesNotes For Homeostasisfreednemon83% (6)
- Countercurrent Multiplier and ADHDocument5 pagesCountercurrent Multiplier and ADHAurora TamNo ratings yet
- Biology - Nephron NotesDocument2 pagesBiology - Nephron NotesShannen Christen NaraceNo ratings yet
- Activity 36 - Urinary Tubular Reabsorption and SecretionDocument6 pagesActivity 36 - Urinary Tubular Reabsorption and SecretionKaren Joy MagbanuaNo ratings yet
- Blood Filtration and Nutrient and Water ReabsorptionDocument2 pagesBlood Filtration and Nutrient and Water ReabsorptionNadia SalwaniNo ratings yet
- Excretory Organs in Different Organisms: Excretory Products and Their ElimnationDocument7 pagesExcretory Organs in Different Organisms: Excretory Products and Their ElimnationSreeyansu RajNo ratings yet
- PP24 Functioning of The KidneyDocument81 pagesPP24 Functioning of The KidneyLeloNo ratings yet
- Watercycle (Streams, Rivers, Lakes and Oceans): 2nd Grade Science Workbook | Children's Earth Sciences Books EditionFrom EverandWatercycle (Streams, Rivers, Lakes and Oceans): 2nd Grade Science Workbook | Children's Earth Sciences Books EditionNo ratings yet
- Care of Clients With Problems in OxygenationDocument5 pagesCare of Clients With Problems in OxygenationSkyla FiestaNo ratings yet
- E61 DiagramDocument79 pagesE61 Diagramthanes1027No ratings yet
- Benzil PDFDocument5 pagesBenzil PDFAijaz NawazNo ratings yet
- Education in America: The Dumbing Down of The U.S. Education SystemDocument4 pagesEducation in America: The Dumbing Down of The U.S. Education SystemmiichaanNo ratings yet
- How To Import Medical Devices Into The USDocument16 pagesHow To Import Medical Devices Into The USliviustitusNo ratings yet
- Cover Letter UchDocument1 pageCover Letter UchNakia nakia100% (1)
- ACF5950 - Assignment # 7 Semester 2 2015: The Business Has The Following Opening Balances: Additional InformationDocument2 pagesACF5950 - Assignment # 7 Semester 2 2015: The Business Has The Following Opening Balances: Additional InformationkietNo ratings yet
- Conference Version of SB 1Document486 pagesConference Version of SB 1Paul MastersNo ratings yet
- Study Notes On Isomers and Alkyl HalidesDocument3 pagesStudy Notes On Isomers and Alkyl HalidesChristian Josef AvelinoNo ratings yet
- Case Study of Milk ProductionDocument46 pagesCase Study of Milk Productionmian21100% (2)
- ALL102-Walker Shirley-Unemployed at Last-The Monkeys Mask and The Poetics of Excision-Pp72-85Document15 pagesALL102-Walker Shirley-Unemployed at Last-The Monkeys Mask and The Poetics of Excision-Pp72-85PNo ratings yet
- CONTROLTUB - Controle de Juntas - New-Flare-Piping-Joints-ControlDocument109 pagesCONTROLTUB - Controle de Juntas - New-Flare-Piping-Joints-ControlVss SantosNo ratings yet
- IPG Or-01 - PTC Train Infrastructure Electrical Safety RulesDocument50 pagesIPG Or-01 - PTC Train Infrastructure Electrical Safety Rules4493464No ratings yet
- Class Two Summer Vacation AssignmentDocument1 pageClass Two Summer Vacation AssignmentshahbazjamNo ratings yet
- Bedwetting TCMDocument5 pagesBedwetting TCMRichonyouNo ratings yet
- Bisleri Water Industry: Project ReportDocument53 pagesBisleri Water Industry: Project ReportJohn CarterNo ratings yet
- Lichens - Naturally Scottish (Gilbert 2004) PDFDocument46 pagesLichens - Naturally Scottish (Gilbert 2004) PDF18Delta100% (1)
- What Is A VolcanoDocument2 pagesWhat Is A VolcanonatachaNo ratings yet
- Soil SSCDocument11 pagesSoil SSCvkjha623477No ratings yet
- Far Eastern University - Manila Income Taxation TAX1101 Fringe Benefit TaxDocument10 pagesFar Eastern University - Manila Income Taxation TAX1101 Fringe Benefit TaxRyan Christian BalanquitNo ratings yet
- Phardose Lab Prep 19 30Document4 pagesPhardose Lab Prep 19 30POMPEYO BARROGANo ratings yet
- Report in Per Dev CorrectedDocument34 pagesReport in Per Dev CorrectedJosh lyan RiveraNo ratings yet
- As ISO 9919-2004 Pulse Oximeters For Medical Use - RequirementsDocument10 pagesAs ISO 9919-2004 Pulse Oximeters For Medical Use - RequirementsSAI Global - APACNo ratings yet
- NG Teng Fong Discharge DocumentsDocument14 pagesNG Teng Fong Discharge DocumentsAnonymous yGwMIPJRawNo ratings yet
- Procedure FireDocument28 pagesProcedure FireRichard D DuNo ratings yet
- Birding The Gulf Stream: Inside This IssueDocument5 pagesBirding The Gulf Stream: Inside This IssueChoctawhatchee Audubon SocietyNo ratings yet
- Electri RelifDocument18 pagesElectri Relifsuleman247No ratings yet
- ASOTDocument4 pagesASOTemperors_nestNo ratings yet
- Business Plan Example - Little LearnerDocument26 pagesBusiness Plan Example - Little LearnerCourtney mcintosh100% (1)
- Employee Final SettlementDocument1 pageEmployee Final SettlementZeeshan Mirza0% (1)