Professional Documents
Culture Documents
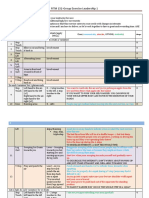
Anesthesia and Neurodevelopment in Children Time.2
Uploaded by
Gustavo OrsoliniOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anesthesia and Neurodevelopment in Children Time.2
Uploaded by
Gustavo OrsoliniCopyright:
Available Formats
䉬 EDITORIAL VIEWS
Anesthesiology 2008; 109:757– 61 Copyright © 2008, the American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc.
Anesthesia and Neurodevelopment in Children
Time for an Answer?
Editor’s Note: This is the first in a three-part series of Editorial Views regarding design of clinical trials to address the effect
of anesthesia on the developing brain. Animal studies have suggested that anesthetic exposure could affect neurocognitive
development, and there is an urgent need for clinical trials to determine whether this effect occurs in humans. This series
presents the opinions of three world thought leaders in the possible designs of such clinical trials.
James C. Eisenach, M.D., Editor-in-Chief
RECENT animal studies have suggested that anesthetics changes in anesthetic practice were recommended, the
may be toxic to the immature developing brain.1–3 In panel did recommend that studies to determine whether
rodents, ␥-aminobutyric acid receptor agonists and N- anesthetics are developmental neurotoxins in children
methyl-D-aspartic acid receptor antagonists, including should be urgently performed. The concerns raised by
ketamine, isoflurane, midazolam, and nitrous oxide, in- both the animal studies and the Food and Drug Adminis-
duce dose- and age-dependent neuronal apoptosis and tration’s response have generated media interest resulting
neuronal cell death in vitro,1,2 with the most prominent in sensational headlines and reports on the potential “brain
effects being observed at postnatal day 7, which inter- damage” children might sustain from exposure to anesthesia.
estingly is also the peak period for synaptogenesis. Ket- Because there has been no clinical study specifically
amine produces similar age- and dose-dependent neurotox- designed to examine the effect of anesthesia on neuro-
icity in nonhuman primates.3 Alarmingly, these in vitro cognitive function in children, it is therefore reasonable
findings were shown to have long-term functional con- to look to other studies that may inform the debate.
sequences resulting in deficits in memory, learning, at- Studies that can tangentially address this issue include
tention, and motor function in adult rats after neonatal neurodevelopmental outcome after surgery in groups
exposure to anesthetics.2 Comparable data are not yet such as premature infants and infants with congenital
available in nonhuman primates. Although the dose and cardiac defects.8 –21 In premature infants, neurodevelop-
duration of anesthetic exposure used in most laboratory mental outcome was worse in those who had surgery for
studies are substantially higher than those used in chil- ligation of patent ductus arteriosus compared with those
dren, these findings are nevertheless of serious con- who were treated medically.17 Similarly, very low-birth-
cern.4,5 Moreover, recent work indicates that neurotox- weight infants and premature infants who had surgery
icity could indeed occur with doses within the human for necrotizing enterocolitis fared worse neurodevelop-
range.6 mentally than those who did not have surgery.18 The
According to the 2004 National Hospital Discharge Boston Circulatory Arrest Trial examined neurodevelop-
Survey, close to three million children in the United ment in infants who had repair of congenital cardiac
States receive anesthesia for surgical procedures, and defects and found that these children had normal or only
many more require anesthesia and sedation for dental very modest decreases in full scale intelligence quotient
procedures and imaging studies. Given this large expo- (IQ) but had specific deficits in memory, language skills,
sure vulnerability for so many infants and children to attention, and visuospatial skills.8 –16,22,23 These studies,
agents that seem to be neurotoxic to animals, it is critical however, contain many confounding variables that make
to understand whether such toxicity also occurs in chil- it impossible to separate the effects of anesthesia from
dren exposed to anesthesia. This concern prompted the surgery and comorbid conditions. The comparison of
US Food and Drug Administration to hold an Advisory outcomes in a group of relatively healthy children who
Committee meeting in March 2007 to review the data on had tympanostomy either before age 3 yr or up to 9
neurotoxicity and determine whether changes in anes- months later is therefore of particular interest. At follow-
thesia practice should be recommended.7 Although no up, the two groups did not differ in their neurodevelop-
mental or neurocognitive function at age 6 yr.24,25 There-
Accepted for publication July 31, 2008. This Editorial View solely represents
fore, although these studies provide some reassurance
the views of the authors and the investigators of the PANDA Research Network that anesthesia exposure before age 3 yr does not ad-
and does not necessarily reflect the views of all of the participants of the First
Columbia University-Morgan Stanley Children’s Hospital of New York Sympo-
versely affect neurodevelopment, they do not directly
sium on “Neurodevelopment and Anesthesia in Children.” address the issue of anesthetic neurotoxicity because
Anesthesiology, V 109, No 5, Nov 2008 757
758 EDITORIAL VIEWS
they were not designed to examine the effect of anes- In addition, we might also apply the lessons learned
thesia per se, but were a comparison between children from a variety of clinical neurodevelopmental studies in
who received anesthesia at two different ages. Indeed, considering which endpoint measures might be relevant
none of the aforementioned studies could specifically in studying the neurotoxic effects of anesthetic agents in
address the potential effects of anesthesia on neurode- children. Studies of developmental outcomes related to
velopmental outcome. environmental neurotoxins have used a wide range of
The absence of clinical data to address this critically endpoint measures, including mental and motor devel-
important public health issue underscores the need for opment, intelligence quotients, behavioral deviations,
more rigorous and definitive studies to examine whether and quality of home environments.29 Both large-scale
anesthetic agents cause neurotoxicity in children. Such national studies of brain development in normal children
studies may have many different possible approaches: and studies of neurodevelopment outcomes after sur-
experimental, observational, prospective, or retrospec- gery have also used similar ranges of endpoint measures,
tive. Perhaps not one single study could provide the including intelligence, verbal and nonverbal abilities,
answer to the question, and data may need to be gener- memory, attention, multidomain development, and be-
ated from various sources that converge to answer the havioral pathologies.12,18,20 –22,30,31 It is important to
research question. To be more precise, the research note that these defined endpoints involve specific devel-
question should be directed to address the effects of opmental domains and are not the same as a global
anesthetic exposure on neurodevelopment in children measure of intelligence. In the Boston Circulatory Arrest
with and without surgery. The two most important de- Trial, even in situations of significant physiologic inju-
sign considerations for such a study are the identification ries, decrements in general IQ scores were extremely
of the appropriate endpoints to use to determine modest, and deficits were only detected using a targeted
whether neurotoxicity exists and the choice of the epi- examination that assessed specific areas such as execu-
demiologic design. In addition, the successful implemen- tive function, memory, and attention.9,11,16 In human
studies, although it would be informative to have an IQ
tation of such a study must consider feasibility issues and
measure, more specific information can only be obtained
the cost and duration for the study.
by evaluating defined developmental domains. Assess-
Taking all of these considerations into account, we pro-
ment could be selective for the specific domains of
pose a study with a mixed epidemiologic design using a
interest and does not necessarily require a complete
retrospective historical cohort that had anesthesia expo-
battery of neuropsychological testing. Although these
sure during early childhood before age 3 yr, but a prospec-
studies did not specifically address the question of anes-
tive follow-up for direct assessment of outcome. The neu-
thesia neurotoxicity, they do demonstrate the value of
rodevelopmental outcome measures will include global IQ
examining global as well as domain-specific outcome
and targeted areas of neurocognitive function, including measures. The need to perform long-term follow-up as-
attention, memory, behavior, and motor function. The sessment is illustrated by the results from neurobehav-
comparison group will be developmental age–matched sib- ioral outcome studies in children after surgery and anes-
lings without history of anesthesia exposure. The assess- thesia. The overwhelming majority of these clinical studies
ment will be performed within a specified age range in late have consistently identified minor behavioral regressions
childhood for both the index and the comparison group followed by recovery within a month. Therefore, they have
using validated age-specific instruments. been limited to assessment of short-term rather than long-
With respect to identifying the appropriate endpoints, term neurodevelopmental consequences.32–36
the existing findings from animal studies, mostly on rat Therefore, based on the findings in the preclinical
pups, cannot be directly extrapolated to children who anesthetic neurotoxicity studies and other developmen-
receive anesthesia because of interspecies differences in tal neurotoxicity studies in children, we propose to as-
brain development and in the brain’s age- and dose- sess the neurodevelopmental endpoints by direct assess-
dependent vulnerability to injury26,27 In addition, anes- ments of both global intelligence measures and specific
thetic neurotoxicity may be modulated by noxious stim- domain measures in executive functioning, attention,
uli such as occurs during surgery.28 Nevertheless, the memory, and motor development. Because human de-
preclinical data do provide consistent and irrefutable velopment is impacted by complex interactions, inter-
evidence that anesthetic exposure can produce negative pretation will also require the appraisal of social, behav-
neurodevelopmental consequences. The specific areas ioral, and family function. The rationale for using direct
in which deficits were identified in rodents could be assessment for these outcome measures is that the data
translated to corresponding neuropsychological func- will be specific, consistent, and complete with respect
tional domains in humans and could be readily measured to the research question. Unlike using a clinical diagno-
in children by trained professionals using a wide range of sis, which not only may lack standardization and uniform
available and well-established developmental neuropsy- criteria but may only point to significant and serious
chological tests. conditions, direct assessment allows for detection of
Anesthesiology, V 109, No 5, Nov 2008
EDITORIAL VIEWS 759
more subtle, though important, functional deficits. For number of potential subjects. Second, if only subjects who
example, a diagnostic endpoint of attention deficit hy- have sufficient quality of documentation are enrolled, the
peractivity disorder would exclude more subtle atten- actual dose and duration of anesthetic exposure could be
tion dysfunctions that are, nevertheless, suboptimal for examined. Third, one could use age-specific, validated as-
age and impact on learning, such as poor selective and sessment tools for the direct assessment of outcomes.
sustained attention abilities, self-regulation, and monitor- Fourth, the comparison is within a well-defined develop-
ing. We further propose that the assessment be per- mental period and not across ages of different developmen-
formed in a single session later in childhood, at least 3 yr tal periods. It is difficult to make comparison across ages
after exposure, to determine the long-term outcome. To representing different periods of physiologic and psycho-
perform the assessment in a single session would mean logical development, because the predictive value from
that the comparison of these outcome measures be- one age group to another is relatively weak with the cur-
tween the exposed and unexposed groups could be rently available age-specific neuropsychological assessment
performed using the same age-specific instruments dur- tools.37 Finally, this approach offers economy in the time
ing a defined developmental period. This would elimi- required to obtain initial results, and in the potential cost of
nate the methodologic challenge of interpreting data the study because there will be no need to budget for
obtained using different age-specific instruments across extensive follow-up.
sequential developmental periods in childhood. Poor All of the preclinical data have consistently demonstrated
predictability over time of widely used and respected that neuronal apoptosis and degeneration in response to
instruments for infants and young children, e.g., the anesthetic exposure were developmental age dependent,
Bayley Scales of Infant Development,37 is well docu- with the greatest vulnerability occurring during the period
mented and would constitute a significant limitation. of synaptogenesis. We therefore propose to assemble a
The second important consideration in study design is retrospective cohort that had anesthetic exposure before
the choice of the epidemiologic approach. Direct and age 3 yr, a period for synaptogenesis in humans.
prospective neuropsychological evaluation would pro- The choice of comparison group is perhaps the most
vide the most valid information. However, useful data important consideration in this study design. In our pro-
derived from direct but nonprospective neuropsycho- posed design, the comparison group consists of siblings
logical evaluation may be available in certain life-course who had no anesthesia exposure. Parental education and
birth cohorts constructed over the past 50 yr in the socioeconomic status are two of the most important
United States and elsewhere.38 – 43 Because almost all confounding factors to control for in any study involving
birth cohort studies have some information on child evaluation of neurocognitive function. For this reason,
health and development and are likely to have surgical the adoption of siblings as the comparison group has
histories, this has the appeal of providing answers rela- been widely used in psychiatric research.45,46 In using the
tively quickly. Several of the more recent birth cohort sibling as the comparison group, one important consider-
studies, including the MoBa-Norway cohort constructed ation is the intersibling differences in IQ that may exist.
in 1999 and the National Child Study initiated in 2006,43 Though a recent study has documented a difference in IQ
are particularly attractive because they would not in- based on the birth order of siblings when they were tested
volve any significant changes in anesthesia practice in as adults,45 other sibling studies have shown little intersib-
children and therefore exposure history to obsolete ling differences in intelligence when testings were per-
agents, as would be the case with some of the older birth formed at ages 4, 7, and 11 yr.46,47 Although intersibling
cohorts. However, these birth cohorts have not com- differences in more subtle aspects of brain functioning
pleted their enrollment, and any data from these studies related to learning and behavior are less known, these data
may not be available for some time to come. do strongly suggest that the choice of age for testing is
Direct and prospective neuropsychological evaluation important in the study design when sibling comparison
could be performed as a randomized controlled trial or as groups are used for studies examining neurocognitive func-
an observational study. Because surgery without anesthesia tion as an outcome.
is not an ethical or acceptable option, a placebo-controlled It is clear that a study to determine whether anesthet-
randomized clinical trial is precluded. Observational stud- ics are neurotoxic in children is urgently needed. The
ies could be performed with either a prospective cohort or proposed epidemiologic design would be efficient and
a retrospectively assembled exposed and unexposed co- feasible and would yield reliable and valid outcome data.
hort, which is then followed and assessed, in a prospective The neurodevelopmental endpoint measures for the pro-
fashion. The approach of prospective assessment of a ret- posed study, including tests of memory, attention, motor
rospective cohort has been successfully used in studies of function, and behavior, are chosen based on extrapolat-
childhood cancer survivors44 and on the effect of tympa- ing the deficits identified in the available though limited
nostomy on childhood development.24,25 Creating a cohort animal data, while incorporating the experiences from
with anesthesia exposure having occurred in the past has a other developmental neurotoxicity studies. The assess-
number of distinct advantages. First, there would be a large ment will be performed within a specified age range in
Anesthesiology, V 109, No 5, Nov 2008
760 EDITORIAL VIEWS
late childhood for both the index and the comparison icine, Harvard Medical School, Boston, Massachusetts); Randall Flick, M.D.,
M.P.H. (Assistant Professor, Department of Anesthesiology, Mayo Clinic, Roch-
group using validated age-specific instruments. Finally, ester, Minnesota); Michael M. Todd, M.D. (Professor and Head, Department of
the study is designed to detect modest effects of anes- Anesthesia, University of Iowa Carver College of Medicine, Iowa City, Iowa);
David Bellinger, Ph.D. (Professor, Department of Neurology, Harvard Medical
thetic agents on the neurodevelopmental outcome in the School, Boston Children’s Hospital, Boston, Massachusetts); Alan J. Moskowitz,
context of surgery. Therefore, a relatively large sample M.D. (Professor, Department of Medicine and Department of Health Policy and
Management, and Co-Director, InCHOIR, Columbia University, New York, New
size for such a study would be anticipated, which could York); and Ezra Susser, M.D., Dr.P.H. (Anna Cheskis Gelman and Murray Charles
be more effectively achieved with a multisite design. Gelman Professor and Chair, Department of Epidemiology, Mailman School of
Public Health, Professor, Department of Psychiatry, Columbia University).
Irrespective of the epidemiologic design, distinguishing The authors also acknowledge other significant contributors to the design and
the effects of anesthesia from the effects of surgery repre- development of the PANDA Study Research Network: Charles Dean Kurth, M.D.
(Professor, Departments of Anesthesia and Pediatrics, University of Cincinnati
sents a daunting challenge to clinical researchers. Our pro- College of Medicine, and Anesthesiologist-in-Chief and Director, Department of
posed study design may be the most appropriate and im- Anesthesia, Cincinnati Children’s Hospital, Cincinnati, Ohio); Annetine Gelijns,
Ph.D. (Professor, Department of Health Policy and Management and Surgical
mediate approach to perform an observational study to Science, and Co-Director, InCHOIR, Columbia University); William J. Greeley,
address the research question of anesthetics as potential M.D., M.B.A. (Professor, Departments of Anesthesia and Pediatrics, University of
Pennsylvania School of Medicine, and Anesthesiologist-in-Chief and Chair, De-
developmental neurotoxins. With the proposed study de- partment of Anesthesiology and Critical Care Medicine, Children’s Hospital of
sign, if there is no difference in any neurodevelopmental Philadelphia, Philadelphia, Pennsylvania); Charles Schleien, M.D. (Professor, De-
partments of Pediatrics and Anesthesiology, Columbia University, and Director,
outcome between groups, then that is strong evidence that Pediatric Intensive Care Unit, Morgan Stanley Children’s Hospital of New York–
anesthesia does not produce neurotoxicity, but if the re- Presbyterian, New York, New York); Charles J. Stolar, M.D. (Rudolph N. Schul-
linger Professor, Departments of Surgery and Pediatrics, Columbia University,
sults show any evidence for any difference between ex- and Surgeon-in-Chief, Morgan Stanley Children’s Hospital of NewYork–Presbyte-
posed and unexposed groups in any neurodevelopmental rian); Joseph R. Tobin, M.D. (Professor and Chair, Department of Anesthesiology,
Wake Forest University Baptist Medical Center, Winston-Salem, North Carolina);
outcome, then no definite conclusion can be made that this and Margaret Wood, M.D. (E.M. Papper Professor and Chairman, Department of
effect is due to the surgery or the anesthesia. Anesthesiology, Columbia University).
In the context of history of anesthesiology as a specialty, The authors thank Barbara Lang, B.S. (Administrative Assistant, Department of
Anesthesiology, College of Physicians and Surgeons, Columbia University, New
once before, the anesthesia scientific community had an- York, New York), for her excellent editorial assistance.
swered a pressing question of anesthetic toxicity and
safety. Forty years ago, the National Halothane Study was
the largest epidemiologic study ever performed up to that References
time. It was a multisite study that used a retrospective 1. Fredriksson A, Ponten E, Gordh T, Eriksson P: Neonatal exposure to a
cohort design, similar to the study proposed here. The combination of N-methyl-D-aspartate and ␥-aminobutyric acid type A receptor
anesthetic agents potentiates apoptotic neurodegeneration and persistent behav-
results of The National Halothane Study significantly influ- ioral deficits. ANESTHESIOLOGY 2007; 107:427–36
enced anesthetic practice and assured the public of the 2. Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K,
Zorumski CF, Olney JW, Wozniak DF: Early exposure to common anesthetic
safety of the anesthetic agent halothane.48 We believe, 40 agents causes widespread neurodegeneration in the developing rat brain and
yr later, it is once more time for a major anesthesia-related persistent learning deficits. J Neurosci 2003; 23:876–82
3. Slikker W Jr, Zou X, Hotchkiss CE, Divine RL, Sadovova N, Twaddle NC,
epidemiologic study. It is both a responsibility and an Doerge DR, Scallet AC, Patterson TA, Hanig JP, Paule MG, Wang C: Ketamine-
opportunity for the specialty of anesthesiology. It is our induced neuronal cell death in the perinatal rhesus monkey. Toxicol Sci 2007;
98:145–58
responsibility to address this critical public health issue 4. Anand KJ: Anesthetic neurotoxicity in newborns: Should we change clinical
related to pediatric anesthesia. It is also an opportunity for practice? ANESTHESIOLOGY 2007; 107:2–4
5. Loepke AW, McGowan FX Jr, Soriano SG: Con: The toxic effects of anes-
us to lead the way in translational research from develop- thetics in the developing brain: The clinical perspective. Anesth Analg 2008;
mental neuroscience to population child health. 106:1664–9
6. Johnson SA, Young C, Olney JW: Isoflurane-induced neuroapoptosis in the
Lena S. Sun, M.D.,* Guohua Li, M.D., Dr.P.H.,† Charles DiMaggio, developing brain of nonhypoglycemic mice. J Neurosurg Anesthesiol 2008;
Ph.D., M.P.H.,† Mary Byrne, Ph.D., M.P.H.,‡ Virginia 20:21–8
Rauh, Sc.D., M.S.W.,§ Jeanne Brooks-Gunn, Ph.D., Ed.M.,㥋 7. Mellon RD, Simone AF, Rappaport BA: Use of anesthetic agents in neonates
and young children. Anesth Analg 2007; 104:509–20
Athina Kakavouli, M.D.,# Alastair Wood, M.D.,** Coinvesti-
8. Forbess JM, Visconti KJ, Bellinger DC, Howe RJ, Jonas RA: Neurodevelop-
gators of the Pediatric Anesthesia Neurodevelopment Assessment mental outcomes after biventricular repair of congenital heart defects. J Thorac
(PANDA) Research Network†† *Departments of Anesthesiology and Pedi- Cardiovasc Surg 2002; 123:631–9
atrics, Columbia University, New York, New York. lss4@columbia.edu. †De- 9. McGrath E, Wypij D, Rappaport LA, Newburger JW, Bellinger DC: Predic-
partments of Anesthesiology and Epidemiology, ‡School of Nursing, §Depart- tion of IQ and achievement at age 8 years from neurodevelopmental status at age
ment of Population and Family Health, School of Public Health, 㛳Teachers’ 1 year in children with D-transposition of the great arteries. Pediatrics 2004;
College and Department of Pediatrics, #Department of Anesthesiology, Co- 114:e572–6
lumbia University. **Departments of Internal Medicine and Pharmacology, 10. Wernovsky G, Stiles KM, Gauvreau K, Gentles TL, duPlessis AJ, Bellinger
DC, Walsh AZ, Burnett J, Jonas RA, Mayer JE Jr, Newburger JW: Cognitive
Vanderbilt University, Nashville, Tennessee; Department of Internal Medicine
development after the Fontan operation. Circulation 2000; 102:883–9
and Department of Pharmacology, Weil Cornell Medical College, New York, 11. Bellinger DC, Wypij D, Kuban KC, Rappaport LA, Hickey PR, Wernovsky
New York. ††See appendix. G, Jonas RA, Newburger JW: Developmental and neurological status of children
at 4 years of age after heart surgery with hypothermic circulatory arrest or
low-flow cardiopulmonary bypass. Circulation 1999; 100:526–32
The authors acknowledge the contribution of all of the guest participants of 12. Bellinger DC, Wypij D, duDuplessis AJ, Rappaport LA, Jonas RA,
the First Columbia University–Morgan Stanley Children’s Hospital of New York Wernovsky G, Newburger JW: Neurodevelopmental status at eight years in
Symposium on “Neurodevelopment and Anesthesia in Children,” held on May 3, children with dextro-transposition of the great arteries: The Boston Circulatory
2008: Cynthia Salorio, Ph.D. (Assistant Professor, Department of Physical Medi- Arrest Trial. J Thorac Cardiovasc Surg 2003; 126:1385–96
cine and Rehabilitation, Johns Hopkins School of Medicine, and Pediatric Neu- 13. Bellinger DC, Bernstein JH, Kirkwood MW, Rappaport LA, Newburger JW:
ropsychologist, Department of Rehabilitation and Department of Neuropsychol- Visual-spatial skills in children after open-heart surgery. J Dev Behav Pediatr 2003;
ogy, Kennedy Krieger Institute, Baltimore, Maryland); Gregory Crosby, M.D. 24:169–79
(Associate Professor, Department of Anesthesiology, Perioperative and Pain Med- 14. Bellinger DC, Rappaport LA, Wypij D, Wernovsky G, Newburger JW:
Anesthesiology, V 109, No 5, Nov 2008
EDITORIAL VIEWS 761
Patterns of developmental dysfunction after surgery during infancy to correct outcomes in children: Effects of sedative premedication. ANESTHESIOLOGY 1999;
transposition of the great arteries. J Dev Behav Pediatr 1997; 18:75–83 90:758–65
15. Bellinger DC, Jonas RA, Rappaport LA, Wypij D, Wernovsky G, Kuban KC, 36. Kain ZN, Wang SM, Mayes LC, Caramico LA, Hofstadter MB: Distress
Barnes PD, Holmes GL, Hickey PR, Strand RD: Developmental and neurologic during the induction of anesthesia and postoperative behavioral outcomes.
status of children after heart surgery with hypothermic circulatory arrest or Anesth Analg 1999; 88:1042–7
low-flow cardiopulmonary bypass. N Engl J Med 1995; 332:549–55 37. Hack M, Taylor HG, Drotar D, Schluchter M, Cartar L, Wilson-Costello D,
16. Bellinger DC, Wernovsky G, Rappaport LA, Mayer JE Jr, Castaneda AR, Klein N, Friedman H, Mercuri-Minich N, Morrow M: Poor predictive validity of
Farrell DM, Wessel DL, Lang P, Hickey PR, Jonas RA: Cognitive development of the Bayley Scales of Infant Development for cognitive function of extremely low
children following early repair of transposition of the great arteries using deep birth weight children at school age. Pediatrics 2005; 116:333–41
hypothermic circulatory arrest. Pediatrics 1991; 87:701–7 38. Susser E, Hoek HW, Brown A: Neurodevelopmental disorders after prena-
17. Chorne N, Leonard C, Piecuch R, Clyman RI: Patent ductus arteriosus and tal famine: The story of the Dutch Famine Study. Am J Epidemiol 1998; 147:
its treatment as risk factors for neonatal and neurodevelopmental morbidity. 213–6
Pediatrics 2007; 119:1165–74 39. Susser E, Terry MB, Matte T: The birth cohorts grow up: New opportuni-
18. Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF, Poole ties for epidemiology. Paediatr Perinat Epidemiol 2000; 14:98–100
WK, Blakely ML, Wright L, Higgins R, Network NNR: Neurodevelopmental and 40. Susser M: Commentary: The longitudinal perspective and cohort analysis.
growth outcomes of extremely low birth weight infants after necrotizing entero- Int J Epidemiol 2001; 30:684–7
colitis. Pediatrics 2005; 115:696–703 41. Terry MB, Susser E: Commentary: The impact of fetal and infant exposures
19. Loepke AW, Soriano SG: An assessment of the effects of general anesthet- along the life course. Int J Epidemiol 2001; 30:95–6
ics on developing brain structure and neurocognitive function. Anesth Analg 42. Susser E, Bresnahan M: Epidemiologic approaches to neurodevelopmental
2008; 106:1681–707 disorders. Mol Psychiatry 2002; (suppl 2):S2–3
20. Rees CM, Pierro A, Eaton S: Neurodevelopmental outcomes of neonates 43. Landrigan PJ, Trasande L, Thorpe LE, Gwynn C, Lioy PJ, D’Alton ME,
with medically and surgically treated necrotizing enterocolitis. Arch Dis Child Lipkind HS, Swanson J, Wadhwa PD, Clark EB, Rauh VA, Perera FP, Susser E: The
Fetal Neonatal Ed 2007; 92:F193–8 National Children’s Study: A 21-year prospective study of 100,000 American
21. Schulzke SM, Deshpande GC, Patole SK: Neurodevelopmental outcomes children. Pediatrics 2006; 118:2173–86
of very low-birth-weight infants with necrotizing enterocolitis: A systematic 44. Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows
review of observational studies. Arch Pediatr Adolesc Med 2007; 161:583–90 AT, Friedman DL, Marina N, Hobbie W, Kadan-Lottick NS, Schwartz CL, Leisen-
22. Forbess JM, Visconti KJ, Hancock-Friesen C, Howe RC, Bellinger DC, Jonas ring W, Robison LL, Childhood Cancer Survivor Study: Chronic health conditions
RA: Neurodevelopmental outcome after congenital heart surgery: Results from an in adult survivors of childhood cancer. N Engl J Med 2006; 355:1572–82
institutional registry. Circulation 2002; 106:I-95–102 45. Kristensen P, Bjerkedal T: Explaining the relation between birth order and
23. Wypij D, Newburger JW, Rappaport LA, duPlessis AJ, Jonas RA, Wer- intelligence. Science 2007; 316:1717
novsky G, Lin M, Bellinger DC: The effect of duration of deep hypothermic 46. Lawlor DA, Bor W, O’Callaghan MJ, Williams GM, Najman JM: Intrauterine
circulatory arrest in infant heart surgery on late neurodevelopment: The Boston growth and intelligence within sibling pairs: Findings from the Mater-University
Circulatory Arrest Trial. J Thorac Cardiovasc Surg 2003; 126:1397–403 study of pregnancy and its outcomes. J Epidemiol Community Health 2005;
24. Paradise JL, Campbell TF, Dollaghan CA, Feldman HM, Bernard BS, Col- 59:279–82
born DK, Rockette HE, Janosky JE, Pitcairn DL, Kurs-Lasky M, Sabo DL, Smith CG: 47. Lawlor DA, Clark H, Smith GD, Leon DA: Intrauterine growth and intelli-
Developmental outcomes after early or delayed insertion of tympanostomy tubes. gence within sibling pairs: Findings from the Aberdeen children of the 1950s
N Engl J Med 2005; 353:576–86 cohort. Pediatrics 2006; 117:e894–902
25. Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Rockette HE, 48. Summary of the national Halothane Study: Possible association between
Pitcairn DL, Smith CG, Colborn DK, Bernard BS, Kurs-Lasky M, Janosky JE, Sabo halothane anesthesia and postoperative hepatic necrosis JAMA 1996; 197:775–88
DL, O’Connor RE, Pelham WE Jr: Tympanostomy tubes and developmental
outcomes at 9 to 11 years of age. N Engl J Med 2007; 356:248–61
26. Berde C, Cairns B: Developmental pharmacology across species: Promise Appendix: Coinvestigators of the PANDA
and problems. Anesth Analg 2000; 91:1–5
27. Soriano SG, Anand KJ, Rovnaghi CR, Hickey PR: Of mice and men: Should Research Network
we extrapolate rodent experimental data to the care of human neonates? ANES-
THESIOLOGY 2005; 102:866–8; author reply 868–9
Robert I. Block, Ph.D. (Associate Professor, Department of Anesthe-
28. Anand KJ, Soriano SG: Anesthetic agents and the immature brain: Are siology, University of Iowa Roy J. and Lucille A. Carver College of
these toxic or therapeutic? ANESTHESIOLOGY 2004; 101:527–30 Medicine, Iowa City, Iowa); Jayant K. Deshpande, M.D., M.P.H. (Pro-
29. Rauh VA, Garfinkel R, Perera FP, Andrews HF, Hoepner L, Barr DB, fessor, Departments of Anesthesiology and Pediatrics, Vanderbilt Uni-
Whitehead R, Tang D, Whyatt RW: Impact of prenatal chlorpyrifos exposure on
neurodevelopment in the first 3 years of life among inner-city children. Pediatrics versity Medical Center, Nashville, Tennessee); Steven C. Hall, M.D.
2006; 118:e1845–59 (Arthur C. King Professor of Pediatric Anesthesia, Department of An-
30. Forbess JM, Visconti KJ, Bellinger DC, Jonas RA: Neurodevelopmental esthesiology, Northwestern University, Feinberg School of Medicine,
outcomes in children after the Fontan operation. Circulation 2001; 104:I127–32 Chicago, Illinois); Andreas Loepke, M.D., Ph.D., F.A.A.P. (Associate
31. Waber DP, De Moor C, Forbes PW, Almli CR, Botteron KN, Leonard G,
Milovan D, Paus T, Rumsey J: The NIH MRI study of normal brain development: Professor, Departments of Anesthesia and Pediatrics, University of
Performance of a population based sample of healthy children aged 6 to 18 years Cincinnati College of Medicine, Cincinnati, Ohio); Lynne Maxwell,
on a neuropsychological battery. J Int Neuropsychol Soc 2007; 13:729–46 M.D. (Associate Professor, Department of Anesthesiology and Critical
32. Kain ZN: Postoperative maladaptive behavioral changes in children: Inci- Care, University of Pennsylvania, Philadelphia, Pennsylvania); Francis
dence, risks factors and interventions. Acta Anaesthesiol Belg 2000; 51:217–26
33. Kain ZN, Caldwell-Andrews AA, Maranets I, McClain B, Gaal D, Mayes LC,
X. McGowan, Jr., M.D. (Professor, Department of Anesthesia, Chil-
Feng R, Zhang H: Preoperative anxiety and emergence delirium and postopera- dren’s Hospital Boston, Boston, Massachusetts); Tonya Miller, M.D.
tive maladaptive behaviors. Anesth Analg 2004; 99:1648–54 (Instructor, Department of Anesthesia, Children’s Hospital Boston);
34. Kain ZN, Caldwell-Andrews AA, Weinberg ME, Mayes LC, Wang SM, Gaal Santhanam Suresh, M.D. (Professor, Department of Anesthesia, North-
D, Saadat H, Maranets I: Sevoflurane versus halothane: Postoperative maladaptive
behavioral changes—A randomized, controlled trial. ANESTHESIOLOGY 2005; 102:
western University, Feinberg School of Medicine); Ronald S. Litman,
720–6 D.O., F.A.A.P. (Associate Professor, Departments of Anesthesiology
35. Kain ZN, Mayes LC, Wang SM, Hofstadter MB: Postoperative behavioral and Pediatrics, University of Pennsylvania).
Anesthesiology, V 109, No 5, Nov 2008
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 1 Critical Care NursingDocument11 pages1 Critical Care NursingChannelGNo ratings yet
- A Review of The Research Literature On Evidence-Based Healthcare Design Roger S. UlrichDocument76 pagesA Review of The Research Literature On Evidence-Based Healthcare Design Roger S. UlrichIsabela PiresNo ratings yet
- Training Swimming Sir LumanglasDocument16 pagesTraining Swimming Sir LumanglasJusthine Joy Magboo VisayaNo ratings yet
- PSFO - Tip Sheet - Eye-Hand CoordinationDocument2 pagesPSFO - Tip Sheet - Eye-Hand Coordinationharem bakirNo ratings yet
- Leadership, Learning & VUCA: Facilitating mastery with changeDocument8 pagesLeadership, Learning & VUCA: Facilitating mastery with changeAndrea CarterNo ratings yet
- Time To Synergize Mental Health With Brain Health: CommentDocument3 pagesTime To Synergize Mental Health With Brain Health: Commentsoliveira_149796No ratings yet
- Dark Psychology and Manipulation by Richard CovertDocument129 pagesDark Psychology and Manipulation by Richard CovertAteng Ph100% (1)
- Molykote 55 O Ring GreaseDocument7 pagesMolykote 55 O Ring GreaseRaghavendra MurthyNo ratings yet
- Worker Safety Perceptions in Low-Risk EnvironmentsDocument7 pagesWorker Safety Perceptions in Low-Risk Environmentstugas phiNo ratings yet
- 03 Movable Swimming Pool Floor - 2022Document2 pages03 Movable Swimming Pool Floor - 2022Abdullah AbdullahNo ratings yet
- SAR of Aminoglycoside Antibiotics With ExamplesDocument3 pagesSAR of Aminoglycoside Antibiotics With ExamplesSimran SidhuNo ratings yet
- Dyslexia Assessment For Languages of India (DALI) : October 2015Document4 pagesDyslexia Assessment For Languages of India (DALI) : October 2015Shaheen AlviNo ratings yet
- MSDS CR Series Not For Recharge - 2019Document7 pagesMSDS CR Series Not For Recharge - 2019Che Wei LinNo ratings yet
- New Patient Medical Form: in One SentenceDocument1 pageNew Patient Medical Form: in One SentenceAzra BarliNo ratings yet
- VINTAGE VOGUINGDocument47 pagesVINTAGE VOGUINGArianne DiosoNo ratings yet
- Hazardous Materials and Wastes Management PlanDocument5 pagesHazardous Materials and Wastes Management Planaloysius akpanNo ratings yet
- Final Cardio Prep TemplateDocument4 pagesFinal Cardio Prep Templateapi-532960622No ratings yet
- A History of The Early Days of Personality Testing in American Industry PDFDocument21 pagesA History of The Early Days of Personality Testing in American Industry PDFFernandoLacerdaNo ratings yet
- Lesson Plan On Chronic Obstructive Pulmonary DiseaseDocument11 pagesLesson Plan On Chronic Obstructive Pulmonary DiseaseFriends Forever80% (5)
- Case Study1Document32 pagesCase Study1MonicaNo ratings yet
- IM - UTI Harrison's Personal NotesDocument5 pagesIM - UTI Harrison's Personal NotesstoragejoannamsvNo ratings yet
- Business Studies Notes: Chapter 1: Role of BusinessDocument48 pagesBusiness Studies Notes: Chapter 1: Role of BusinessLevon SanossianNo ratings yet
- RNTCP National Contact Details Directory Data-FinalDocument174 pagesRNTCP National Contact Details Directory Data-Finalwasimkokni100% (2)
- Digital Transformation in Education: Its Effect On The Well - Being of Teachers at Notre Dame of Midsayap CollegeDocument24 pagesDigital Transformation in Education: Its Effect On The Well - Being of Teachers at Notre Dame of Midsayap CollegePsychology and Education: A Multidisciplinary Journal100% (1)
- BP2016 - Vol.01Document1,334 pagesBP2016 - Vol.01thu dat80% (5)
- Lifetime Physical Fitness and Wellness A Personalized Program 14th Edition Hoeger Test BankDocument25 pagesLifetime Physical Fitness and Wellness A Personalized Program 14th Edition Hoeger Test BankStevenHughesreozb100% (54)
- DiagnosticsDocument38 pagesDiagnosticssweetyxocolatNo ratings yet
- Nursing Cover LetterDocument1 pageNursing Cover Letterapi-365022171No ratings yet
- FAMILY PLANNING Action Plan For 2011-12 (For Workshop 20th)Document46 pagesFAMILY PLANNING Action Plan For 2011-12 (For Workshop 20th)keshabnNo ratings yet
- Department of Education: Republic of The Philippines Region I La Union Schools Division Office Bacnotan, La UnionDocument1 pageDepartment of Education: Republic of The Philippines Region I La Union Schools Division Office Bacnotan, La UnionChristineNo ratings yet