Professional Documents
Culture Documents
Departments of Neurology, James J. Peters Veterans Affairs Medical Center, Bronx, NY, and Mount Sinai School of Medicine, New York, NY
Uploaded by
yuli0 ratings0% found this document useful (0 votes)
88 views1 pagePdf
Original Title
algoritma khorea
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPdf
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
88 views1 pageDepartments of Neurology, James J. Peters Veterans Affairs Medical Center, Bronx, NY, and Mount Sinai School of Medicine, New York, NY
Uploaded by
yuliPdf
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
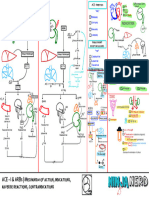
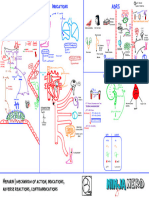
A flow chart for the evaluation of chorea
Ruth H. Walker, MB., Ch.B., Ph.D.
Departments of Neurology, James J. Peters Veterans Affairs Medical Center, Bronx, NY, and Mount Sinai School of Medicine, New York, NY
ruth.walker@mssm.edu
Patient with
chorea Infant/child Streptococcal?
+ve
Age of sore throat, rheumatic
Autosomal recessive/sporadic heart disease Sydenham's chorea
Onset?
ASO, anti-DNAse
B titers
Lesch-Nyhan syndrome
Confirm with gene test Tardive dyskinesia
Autosomal Adult
X-linked Inheritance? Normal
recessive
Delayed
Autosomal Medication- Yes
Check Childhood onset, Direct
Yes dominant Time course?
gouty arthritis, MRI; normal induced? Immediate or side effect
uric acid self-mutilation?
Fe in basal dose related
Calcium Acute infarct in
ganglia ? deposition posterior limb of
in basal internal capsule. Infantile bilateral
Phospholipase-associated
ganglia. Diffusion- No
Normal No Pantothenate CT scan weighted MRI
striatal necrosis;
neurodegeneration ?PDE10A mutations
kinase-associated Yes No (see review by
neurodegeneration Yes Structural lesion; Tonduti et al. 2016)
•Mix blood 1:1 with 0.9% NaCl containing 10IU/ml heparin
•Incubate at room temperature for 30-120 min on a shaker •Childhood onset PKAN: T2 weighted MRI Stroke, tumor
•Take 5+ microphotographs from each wet preparation •Occasional later onset Yes Leigh’s syndrome,
(phase-contrast microscope) •Pigmentary retinopathy
MRI arteriovenous malformation, Lactate/
•Count cells with spicules: normal value < 6.3 % •Dystonia
•10% have acanthocytosis
PANK2 Normal PLA2G6 calcification (SLC20A2, pyruvate other mitochrondrial?
Lubag No Ceruloplasmin?
No No Yes mutation? mutation? PDGFRB, PDGFB, XPR1?), etc Confirm with gene test
Acanthocytosis? Filipino? Confirm with
gene test
GPR88 Basal ganglia
No mutations? No
Typical phenotype = dystonia- necrosis?
parkinsonism, but should be Other neurodegeneration No
Yes considered in any Filipino with an
with brain iron
unexplained movement disorder, Caudate Yes
including women Yes Accumulation disorder… White matter GNA01 Recent Post-infectious
nucleus
FAHN, MPAN, BPAN… lesions mutations? Yes infection? striatal necrosis
•Full panel of 23 Kell abs usually available atrophy?
Courtesy of Dr Hans H. Jung, Zürich at regional blood centers; •Childhood onset
•Ask to “exclude McLeod phenotype” Pseudo- Aceruloplasminemia •Seizures (variable)
•Delayed myelination
dominant or normal MRI Yes Features
•Iron overload
inheritance? •Diabetes mellitus in 20’s (from pancreatic iron)
suggestive of Yes Work-up for inherited
Gordon Holmes syndrome/ metabolic
Liver enzymes or Kx and Kell •Middle-age onset
RNF216 mutations? metabolic diseases;
creatine kinase ags
McLeod syndrome •Retinal degeneration (from iron deposition) disease?
•Parkinsonism/dystonia, orofacial involvement is typical organic/amino acids, lysosomal
•Behavioural changes/ •hypogonadism
•Dementia usually later
psychopathology •dementia
•Seizures Fasano et al. 2008 •MRI may not show Fe accumulation (Skidmore et al. 2007)
•ataxia
Enzymes, skin biopsy etc
•Peripheral neuropathy Gradient echo T2* No
Normal •Hyporeflexia
Normal •Cardiomyopathy
No Normal Negative
•Hepatosplenomegaly
?
Normal Kayser- Normal
McNeill et al 2008
Fast spin echo Fleischer Ceruloplasmin? Creatine kinase Liver enzymes
rings? Diagnosis Diagnosis
Yes Ferritin 24hr Cu
Lactate/ Normal Chorein chorein
mutations? excretion?
pyruvate Normal assay Normal
Dobson-Stone et al. 2004
Normal
Contact – danek@lmu.de
Recent
Neuroferritinopathy liver No +ve +ve
+ve
disease?
No
•Middle-age onset
•Parkinsonism/dystonia
Wilson’s disease Metabolic
•Occasional ataxia, spasticity
Ataxia? work-up (2) Metabolic
•Dementia rare •Dystonia/parkinsonism/dystonia more common Normal Anti-phospholipid ab Normal work-up (1)
•Adolescent onset Electrolytes
•Risus sardonicus
SLE, other autoimmune
Mitochondrial Chorea-acanthocytosis •Psychiatric disease Yes Polycythemia vera Glucose
Yes huntingtin Celiac disease Pregnancy test
disorder? Confirm with gene test HIV, B12, RPR TSH
Confirm with gene test mutation? Normal Acquired hepatocerebral Pb
•Behavioural changes/psychiatric disease But can be normal degeneration Frataxin
Friedreich’s ataxia
•Self-mutilation of lips, tongue, other body parts in pre-menopausal
•Seizures women with
mutation?
•Hyporeflexia
•Hepatomegaly
Huntington’s No
Ferritin level? neuroferritinopathy
•Onset in childhood
•Ataxia may be absent
disease Chorea is a common movement disorder, the etiology of which is •Reflexes increased or decreased
•Cardiomyopathy •Onset in childhood
rarely identifiable from its appearance. The identification of genetic •Susceptible to radiation
•Risk of malignancy, infection
causes for some of the inherited choreas has facilitated their •Elevated α-feto-protein
Courtesy Dr Jane Zheng, UNC-CH C9ORF2 C9ORF72
mutation? diagnosis, in addition to increasing the spectrum of phenotypes for
disease Ataxia-telangiectasia
other disorders in which chorea may occur less often. A number of Telangiectasia?
•Variable phenotype Confirm with ATM mutation
•Often upper motor neuron clues in the family and medical history, clinical examination, and
signs
No •Reduced penetrance laboratory findings may inform the diagnosis. Whilst we typically
•Variable age of onset
consider these simultaneously when evaluating the patient with
African chorea, there is a need for an algorithm to generate consideration of Yes Ataxia with oculomotor
Yes Junctophilin-3 α-feto- Senataxin
Yes ancestry? No some of the rarer etiologies.
Huntington’s disease-like 2 protein mutation? apraxia type 2
mutation? (may be
•Onset in childhood
•Behavioural changes/psychiatric disease occult) •Peripheral neuropathy
•May have more dystonia/parkinsonism?
•10% have acanthocytosis
This flow chart aims to present the various factors which facilitate •Elevated creatine kinase
No Iron in basal making the correct diagnosis, and the appropriate testing to consider Consider AD
ganglia? Consider AD
depending upon previous test results. The list of differential diagnoses Aprataxin spinocerebellar
ataxias
and X-linked
mutation? pathways
Spinocerebellar ataxia 1,2,3,8,12,17, Yes SCA/DRPLA Non-diagnostic
of chorea is ever-evolving with advances in the molecular biology of e.g. homozygosity?
mutations? MRI movement disorders. This algorithm which is open to further
DRPLA? White matter
Yes
lesions? development in the light of new knowledge, and may indeed become
•Ataxia, eye movement abormalities, peripheral
Cryopyrin-associated Ataxia with oculomotor Autoimmune
neuropathy etc are typical, but may be pure HD phenocopy somewhat obsolete as whole exome/genome sequencing becomes
•DRPLA – myoclonus, dementia, dystonia typical
No periodic syndrome? apraxia type 1 non-paraneoplastic
Yes more available.
Huntington’s •Deafness
•Onset in childhood
syndrome
disease-like 1?
•Elevated anti-cardiolipin IgG
•Peripheral neuropathy
Neoplasm
•Mutation of NLPR3 Negative workup
This flow chart does not necessarily indicate the temporal course of •Elevated cholesterol evaluation;
Hypotonia, •hypoalbuminemia Anti-Hu, Yo, +ve Paraneoplastic
ADCY-5 dyskinesia
Hyperreflexia,
Yes the diagnostic work-up of chorea, especially if the family history is not CRMP-5, GAD65
Facial movements, Non-progressive, No NMDA, VGCC syndrome
Adenylate cyclase-5 Paroxysmal/fluctuating no dementia?
known, but should be used a guideline to generate the consideration Caspr2, LGI-1,
mutation movements? of various clinical entities in light of the available information. striational Creutzfeldt-Jakob
Prion Single Yes ……..
No PLED’s? disease
Thyroid, mutation? case?
MRI findings?
+ve
No -ve (chorea more common
pulmonary,
Consider atypical forms of CSF 14-3-3 in new variant)
involvement? No
Benign hereditary chorea No AD, X-linked or AR disorders, Confirmed by pathology
NKX2.1 (TITF-1) mutation Other FTD syndrome? No depending upon inheritance -ve
CACNA1A mutation?
VCP, FUS, UBQLN2
You might also like
- The GcMAF BookDocument79 pagesThe GcMAF BookVíctor Valdez100% (1)
- Group Imago and The Stages of Group DevelopmentDocument16 pagesGroup Imago and The Stages of Group DevelopmentNarcis Nagy100% (3)
- One Second and A Million Miles - The Bridges of Madison - County - JRBDocument4 pagesOne Second and A Million Miles - The Bridges of Madison - County - JRBKFarnum Jr.0% (6)
- Orthodox America 1794-1976 - Constance J. Tarasar, John H. Erickson, Alexander Doumouras, - 1975 - Orthodox Church America - Anna's ArchiveDocument364 pagesOrthodox America 1794-1976 - Constance J. Tarasar, John H. Erickson, Alexander Doumouras, - 1975 - Orthodox Church America - Anna's ArchivemarcelNo ratings yet
- Anaerobic Digester Design and CalculationDocument41 pagesAnaerobic Digester Design and CalculationJohn TauloNo ratings yet
- Master Kinesiotaping HandoutDocument11 pagesMaster Kinesiotaping HandoutcosasdeangelNo ratings yet
- PEMF ClinicalStudies 1Document38 pagesPEMF ClinicalStudies 1OaNa Miron100% (3)
- Mindful Medical Practice - Clinical Narratives and Therapeutic InsightsDocument169 pagesMindful Medical Practice - Clinical Narratives and Therapeutic InsightsSkg KonNo ratings yet
- Date Performed: August 18, 2015 Group No. and Section: Group 5 WCDE-A Date Submitted: September 1, 2015 Group MembersDocument28 pagesDate Performed: August 18, 2015 Group No. and Section: Group 5 WCDE-A Date Submitted: September 1, 2015 Group MembersCm MacaliaNo ratings yet
- Antibiotic Chart-Infectious Disease Bug Drug Table-2019Document2 pagesAntibiotic Chart-Infectious Disease Bug Drug Table-2019Duy LuuNo ratings yet
- Nhs Bronchiolitis Pathway Acute Setting South East Coast SCNDocument2 pagesNhs Bronchiolitis Pathway Acute Setting South East Coast SCNdrgrizahNo ratings yet
- Cardiovascular Disease Worldwide: Top Causes of Death From CVDDocument1 pageCardiovascular Disease Worldwide: Top Causes of Death From CVDcoloradoresourcesNo ratings yet
- Honest Food GuideDocument1 pageHonest Food Guidepeanutmilk100% (3)
- Cardiovascular Pharmacology) 08 ACE-I - ARBs - KeyDocument1 pageCardiovascular Pharmacology) 08 ACE-I - ARBs - Keyhasanatiya41No ratings yet
- Oral Sur 2 MidtermDocument22 pagesOral Sur 2 Midtermnapat kidsanakaraketNo ratings yet
- IONIX ModelDocument6 pagesIONIX ModelTrường Bửu TrầnNo ratings yet
- ExerciÌ Cio e DCV - Parte 1Document10 pagesExerciÌ Cio e DCV - Parte 1Joao GuimaraesNo ratings yet
- Fever PrimaryCommunityCare Dec 16 FINAL VSDocument2 pagesFever PrimaryCommunityCare Dec 16 FINAL VSnimraNo ratings yet
- Acting Studio Applicaton FormDocument1 pageActing Studio Applicaton ForminfosysofficialhydNo ratings yet
- Health History QuestionnaireDocument4 pagesHealth History QuestionnaireDea Sudiyantika PutriNo ratings yet
- ReferralDocument1 pageReferralmanasabhavaniNo ratings yet
- HypertensionDocument1 pageHypertensionvictor.garcia4080No ratings yet
- Honest Food GuideDocument1 pageHonest Food Guideapi-3714923No ratings yet
- Unending GraceDocument15 pagesUnending GraceMelinda T. Magbanua100% (1)
- HIRADEC Rev April'23 - (REV08)Document10 pagesHIRADEC Rev April'23 - (REV08)DEEPAK MALLIKNo ratings yet
- Telaviv MapDocument1 pageTelaviv Mapshay4323No ratings yet
- Ej 4 Infor PDFDocument1 pageEj 4 Infor PDFJavier RufeteNo ratings yet
- Anthem BassDocument2 pagesAnthem BassRomoliNo ratings yet
- (PIDST) - 391 - Pidst - 20111020114358 - Filejou 2Document20 pages(PIDST) - 391 - Pidst - 20111020114358 - Filejou 2Nareunart KongkaNo ratings yet
- 8 Hullet BrochureDocument19 pages8 Hullet BrochureRonnie TanNo ratings yet
- 8 Hullet BrochureDocument19 pages8 Hullet BrochureRonnie TanNo ratings yet
- Notes AtherosclerosisDocument1 pageNotes AtherosclerosisElizabeth de GuzmanNo ratings yet
- Ujian Patoflow Yola MTDocument1 pageUjian Patoflow Yola MTAdam SipahutarNo ratings yet
- pPYqnlFGTC2UMT6pBejw - 3004-101 Proposed PlansDocument1 pagepPYqnlFGTC2UMT6pBejw - 3004-101 Proposed PlanserniE抖音 AI Mobile Phone Based MovieNo ratings yet
- ANGELES - CANTANDO - ESTAN Final ScoreDocument6 pagesANGELES - CANTANDO - ESTAN Final ScoreSergio FernandezNo ratings yet
- Non Taccostare Allurna Giuseppe Verdi - A MinorDocument5 pagesNon Taccostare Allurna Giuseppe Verdi - A MinorMohammadNo ratings yet
- Health Assessment FormDocument12 pagesHealth Assessment Formmiha3la33No ratings yet
- Vienna Map City CenterDocument1 pageVienna Map City Centeragnes nathaniaNo ratings yet
- Son Tentacion - HeridaDocument12 pagesSon Tentacion - HeridaMauricio AguilarNo ratings yet
- 1 KyrieDocument10 pages1 KyrieRémi TroisgrosNo ratings yet
- Missa Pro Pace: SanctusDocument1 pageMissa Pro Pace: SanctusDawid JuraszekNo ratings yet
- 24x24 AvenzaBasemap TolowaDunesDocument1 page24x24 AvenzaBasemap TolowaDunesMonie DNo ratings yet
- A-01 MergedDocument17 pagesA-01 MergedDeereck Huertas HizoNo ratings yet
- Picu Ready RecknerDocument2 pagesPicu Ready RecknerPranitha Reddy0% (1)
- CH2Document6 pagesCH2fd2m2n8p55No ratings yet
- Nipt TRF MedgenomeDocument4 pagesNipt TRF MedgenomepathbiomedxNo ratings yet
- Given To HospitalityDocument456 pagesGiven To HospitalityBianca PradoNo ratings yet
- Global Report On Birth Defects The Hidden Toll ofDocument1 pageGlobal Report On Birth Defects The Hidden Toll ofvolNo ratings yet
- Rateeatatagh IveDocument424 pagesRateeatatagh IveGeorge TeodorNo ratings yet
- Besame Mucho. Score.Document6 pagesBesame Mucho. Score.AndreiFloreaNo ratings yet
- Head / Hair Face Eyes Nose Oral / Throat Ears Neck: Physical Exam (Heent)Document1 pageHead / Hair Face Eyes Nose Oral / Throat Ears Neck: Physical Exam (Heent)Johnny BeeNo ratings yet
- Mother Gooses Nur 00 ElliDocument128 pagesMother Gooses Nur 00 ElliBranko NikolicNo ratings yet
- Jane Jane: Monday-Sunday/HolidayDocument2 pagesJane Jane: Monday-Sunday/HolidayChristian DominguezNo ratings yet
- Jesus, Etc.: ModeratelyDocument5 pagesJesus, Etc.: ModeratelyBen McMunn100% (1)
- The Structure of Questions in EnglishDocument1 pageThe Structure of Questions in EnglishMohamed NaserNo ratings yet
- Ek Apolas A TB S 2021-22-1Document2 pagesEk Apolas A TB S 2021-22-1Krisztián TóthNo ratings yet
- THC Special OffersDocument2 pagesTHC Special OffersTotalHealthConceptsNo ratings yet
- Cardiovascular Pharmacology) 03 Heparin - KeyDocument1 pageCardiovascular Pharmacology) 03 Heparin - Keyhasanatiya41No ratings yet
- O Praise The Name AnastasisDocument6 pagesO Praise The Name AnastasisFabiana Campanha Veronezi100% (3)
- 13PLAN planMAUGDocument1 page13PLAN planMAUGEvanrey EnriquezNo ratings yet
- Chiquito Team Band - Lejos de TiDocument8 pagesChiquito Team Band - Lejos de TiMercedes Terrón EspinosaNo ratings yet
- It's So Easy Going Green: An Interactive, Scientific Look at Protecting Our EnvironmentFrom EverandIt's So Easy Going Green: An Interactive, Scientific Look at Protecting Our EnvironmentNo ratings yet
- Instant Assessments for Data Tracking, Grade 4: MathFrom EverandInstant Assessments for Data Tracking, Grade 4: MathRating: 5 out of 5 stars5/5 (2)
- Updated Recommendations On The Use of Pneumococcal Vaccines For High-Risk IndividualsDocument5 pagesUpdated Recommendations On The Use of Pneumococcal Vaccines For High-Risk IndividualsyuliNo ratings yet
- Materi I DR HadryastutiDocument38 pagesMateri I DR HadryastutiyuliNo ratings yet
- Appendix7 ChestDrainObsChart F PDFDocument3 pagesAppendix7 ChestDrainObsChart F PDFyuliNo ratings yet
- Hemodinamik SyokDocument15 pagesHemodinamik SyokyuliNo ratings yet
- Ventilation Guidelines For PICU Oct 2010Document13 pagesVentilation Guidelines For PICU Oct 2010MariaUlfaNo ratings yet
- Bookshelf NBK248066 PDFDocument167 pagesBookshelf NBK248066 PDFyuliNo ratings yet
- Febrile NuetropeniaDocument4 pagesFebrile NuetropeniayuliNo ratings yet
- How To Read A Growth Chart - Percentiles ExplainedDocument3 pagesHow To Read A Growth Chart - Percentiles ExplainedyuliNo ratings yet
- 1 Guidelines On Paediatric Parenteral Nutrition.1Document4 pages1 Guidelines On Paediatric Parenteral Nutrition.1titissetiarNo ratings yet
- Cyclophosphamide Treatment in The Oxford Kidney Unit: Renal Unit, Churchill HospitalDocument8 pagesCyclophosphamide Treatment in The Oxford Kidney Unit: Renal Unit, Churchill HospitalyuliNo ratings yet
- A174-05PaedPNGuidel Carbohydrates PDFDocument5 pagesA174-05PaedPNGuidel Carbohydrates PDFyuliNo ratings yet
- PAPER (ENG) - The Early Feeding Skills Assessment For Preterm InfantsDocument15 pagesPAPER (ENG) - The Early Feeding Skills Assessment For Preterm InfantsAldo Hip NaranjoNo ratings yet
- TPN PDFDocument9 pagesTPN PDFyuliNo ratings yet
- Cyclophosphamide Treatment in The Oxford Kidney Unit: Renal Unit, Churchill HospitalDocument8 pagesCyclophosphamide Treatment in The Oxford Kidney Unit: Renal Unit, Churchill HospitalyuliNo ratings yet
- Dialysis Disequilibrium SyndromeDocument8 pagesDialysis Disequilibrium SyndromeyuliNo ratings yet
- Pediatric Nutrition Assessment Final FarahDocument54 pagesPediatric Nutrition Assessment Final Farahyuli0% (1)
- Berrington Gut Microbiota in Preterm Infants Assessment and Relevance To Health and Disease 2012Document7 pagesBerrington Gut Microbiota in Preterm Infants Assessment and Relevance To Health and Disease 2012yuliNo ratings yet
- Incessant VT VFDocument9 pagesIncessant VT VFTor JaNo ratings yet
- Venipuncture (Procedure) : Patrick Kyle C. Ignacio, RRTDocument26 pagesVenipuncture (Procedure) : Patrick Kyle C. Ignacio, RRTCielo DeguzmanNo ratings yet
- TCCC Guidelines August 2011Document12 pagesTCCC Guidelines August 2011OnTheXNo ratings yet
- Philosophy Palliative Care and End of Life Care Per 15-02-2021Document33 pagesPhilosophy Palliative Care and End of Life Care Per 15-02-2021rizki ikhsanNo ratings yet
- Planning Physical Facilities of Hospital and Educational InstitutionDocument5 pagesPlanning Physical Facilities of Hospital and Educational InstitutionSundaraBharathi100% (2)
- Group 1 BARC CaseDocument14 pagesGroup 1 BARC CaseAmbrish ChaudharyNo ratings yet
- Alcohol History Taking - Geeky MedicsDocument6 pagesAlcohol History Taking - Geeky MedicsJahangir AlamNo ratings yet
- Swyer James MacLeod SyndromeDocument12 pagesSwyer James MacLeod Syndromeflori.bNo ratings yet
- Guidebook For Preacc Entrylevelstandards SHCO PDFDocument162 pagesGuidebook For Preacc Entrylevelstandards SHCO PDFArun Kumar100% (3)
- Ambulance Nurse Checklist MMSR2017Document4 pagesAmbulance Nurse Checklist MMSR2017Ahmed OsmanNo ratings yet
- Pelvis Frozen EnglishDocument3 pagesPelvis Frozen EnglishPetar PribicNo ratings yet
- Concept of Disease 1.1 Anatomy and PhysiologyDocument15 pagesConcept of Disease 1.1 Anatomy and PhysiologyAulia SandraNo ratings yet
- Sevrage CannabisDocument29 pagesSevrage CannabismihaelaNo ratings yet
- Appi Psychotherapy 20220018Document8 pagesAppi Psychotherapy 20220018consulta.nicolaslabbeNo ratings yet
- Anesthesia in Dentistry and Extraction of Tooth by Pratyasha ParipurnaDocument42 pagesAnesthesia in Dentistry and Extraction of Tooth by Pratyasha ParipurnapariNo ratings yet
- Samantha Bradley: Work ExperienceDocument3 pagesSamantha Bradley: Work Experienceapi-399988983No ratings yet
- ADN Care Plan - DepressionDocument3 pagesADN Care Plan - DepressionDavid PerezNo ratings yet
- Letter To Stephen Muldrow USAFLM Re Dr. Asad Qamar May-12-2017Document93 pagesLetter To Stephen Muldrow USAFLM Re Dr. Asad Qamar May-12-2017Neil GillespieNo ratings yet
- Chapter 5 - Counselling Skills: The GP As An Effective CounsellorDocument19 pagesChapter 5 - Counselling Skills: The GP As An Effective Counsellorprofarmah6150100% (2)
- Rubella: Congenital Clinically Significant Congenital MalformationsDocument8 pagesRubella: Congenital Clinically Significant Congenital MalformationsAlexandraNo ratings yet
- Evaluation of Meat Quality and Carcass Characteristics of Broiler Chickens As Affected by Feed Withdrawal With Electrolytes Added To WaterDocument8 pagesEvaluation of Meat Quality and Carcass Characteristics of Broiler Chickens As Affected by Feed Withdrawal With Electrolytes Added To WaterInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- PRO Measures - Shoulder and Upper ExtremityDocument27 pagesPRO Measures - Shoulder and Upper ExtremityGonzalo QuiñonesNo ratings yet
- Rumah Sakit Bhakti MuliaDocument3 pagesRumah Sakit Bhakti MuliaSarachanda SallyNo ratings yet