Professional Documents
Culture Documents
Lactancia Materna - Guía para Profesionales
Uploaded by
Carolina Andrea Vasquez HenriquezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lactancia Materna - Guía para Profesionales
Uploaded by
Carolina Andrea Vasquez HenriquezCopyright:
Available Formats
546890
research-article2014
NCPXXX10.1177/0884533614546890Nutrition in Clinical PracticeSchwartz et al
Special Report
Nutrition in Clinical Practice
Volume 29 Number 6
Gastrostomy Tube Placement in Patients With December 2014 829–840
© 2014 American Society
Advanced Dementia or Near End of Life for Parenteral and Enteral Nutrition
DOI: 10.1177/0884533614546890
ncp.sagepub.com
hosted at
online.sagepub.com
Denise Baird Schwartz, MS, RD, CNSC, FADA, FAND, FASPEN1;
Albert Barrocas, MD, FACS, FASPEN2; John R. Wesley, MD, FACS, FAAP, FASPEN3;
Gustavo Kliger, MD4; Alessandro Pontes-Arruda, MD, MSc, PhD, FCCM5,6;
Humberto Arenas Márquez, MD7; Rosemarie Lembo James, RD, CNSC, LD/N8;
Cheryl Monturo, PhD, MBE, ACNP-BC9; Lucinda K. Lysen, RD, LD, RN, BSN10;
and Angela DiTucci, RD, LDN11
Abstract
Based on current scientific literature, gastrostomy tube (G-tube) placement or other long-term enteral access devices should be withheld in
patients with advanced dementia or other near end-of-life conditions. In many instances healthcare providers are not optimally equipped
to implement this recommendation at the bedside. Autonomy of the patient or surrogate decision maker should be respected, as should the
patient’s cultural, religious, social, and emotional value system. Clinical practice needs to address risks, burdens, benefits, and expected
short-term and long-term outcomes in order to clarify practice changes. This paper recommends a change in clinical practice and care
strategy based on the results of a thorough literature review and provides tools for healthcare clinicians, particularly in the hospital setting,
including an algorithm for decision making and a checklist to use prior to the placement of G-tubes or other long-term enteral access
devices. Integrating concepts of patient-centered care, shared decision making, health literacy, and the teach-back method of education
enhances the desired outcome of ethical dilemma prevention. The goal is advance care planning and a timely consensus among health
team members, family members, and significant others regarding end-of-life care for patients who do not have an advance directive and
lack the capacity to advocate for themselves. Achieving this goal requires interdisciplinary collaboration and proactive planning within a
supportive healthcare institution environment. (Nutr Clin Pract. 2014;29:829-840)
Keywords
nutritional support; aged; dementia; ethics; terminal care; enteral nutrition
Studies worldwide consistently demonstrate a very high mortal- Executive Summary
ity rate in older adults with advanced dementia who have feed-
ing tubes.1-4 The potential for inadequate communication The following approach is recommended for patients with
advanced dementia or other near end-of-life conditions who
between practitioners and patients, family members, significant
others, caregivers, and surrogate decision makers, as well as a
difference in ethical values may lead to beginning therapies that From 1Providence Saint Joseph Medical Center, Burbank, California; 2Atlanta
Medical Center, Atlanta, Georgia; 3Division of Pediatric Surgery, Ann &
do not benefit the patient. The application of unnecessary thera- Robert H. Lurie Children’s Hospital, Chicago, Illinois; 4Clinical Nutrition
pies may dramatically increase the cost of healthcare. Service and Nutrition Support Unit, Austral University Hospital, Buenos
In developing this special report, the International Clinical Aires, Argentina; 5Christus University School of Medicine, Fortaleza, Ceara,
Ethics Section (ICES) of the American Society for Parenteral Brazil; 6Baxter Healthcare, Singapore, Singapore; 7Intestinal Failure Unit,
Sanvite, Zapopan, Mexico; 8Martin Health System, Stuart, Florida; 9West
and Enteral Nutrition (A.S.P.E.N.) advocates for weighing the
Chester University of Pennsylvania, West Chester, Pennsylvania; 10Nutrition
potential benefits derived from a particular mode of nutrition Support Consultant, Chicago, Illinois; and 11Veterans Affairs Boston
support therapy against inherent risks and burdens within a Healthcare System–West Roxbury Campus, Boston, Massachusetts.
patient-centered framework of culture, religion, ethical princi- Financial disclosure: None declared.
ples, and personal values. The professional judgment of the
Appendices A-C are available as an online data supplement for this paper
attending healthcare professional, with input from the interdis- at www.ncp.sagepub.com.
ciplinary team and considerate of the patient’s wishes, is the
This article originally appeared online on October 7, 2014.
primary component of quality healthcare.
Laws of the jurisdiction in which the patient is located may Corresponding Author:
Denise Baird Schwartz, MS, RD, CNSC, FADA, FAND, FASPEN,
also impact the range of options available to healthcare profes- Providence Saint Joseph Medical Center, 501 South Buena Vista Street,
sionals. Legal aspects of this issue are not covered in this Burbank, CA 91505, USA.
report. Email: denisebairdschwartz@gmail.com
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
830 Nutrition in Clinical Practice 29(6)
are being considered for gastrostomy tube (G-tube) placement. Huntington’s disease, lead to a progressive loss of mental func-
Throughout this paper, the term G-tube refers to any long-term tions. Other types of dementia can be halted or reversed with
enteral access device: appropriate treatment. People with moderate or advanced demen-
tia typically need constant care and supervision to prevent them
1. The decision to withhold or withdraw tube feeding in from harming themselves or others. They also may need assis-
end-stage illness is supported by current scientific tance with daily activities such as eating, bathing, and dressing.6
evidence. Numerous articles have been published about advanced
2. Advanced dementia should be seen by the healthcare dementia and use of feeding tubes, yet there remains a high con-
team as a terminal illness, and healthcare team mem- sistency in finding a lack of efficacy in tube feeding in this
bers should clearly communicate this perspective to population. Current scientific evidence suggests that the poten-
the patient’s family, significant others, caregivers, and/ tial benefits of tube feeding do not outweigh the associated bur-
or surrogate decision makers. dens of treatment in persons with advanced dementia. Studies
3. A thorough discussion should take place with the consistently demonstrate a very high mortality rate in older
patient, family, significant others, caregivers, and/or adults with advanced dementia who have feeding tubes.1-4
surrogate decision makers. The conversation should Dementia is a leading cause of death in the United States
cover the most updated evidence-based findings but is under-recognized as a terminal illness.7 The clinical
regarding short-term and long-term risks, burdens, and course of long-term care facility residents with advanced
benefits. dementia has not been well described. In one study, researchers
4. Alternatives such as assisted oral feeding and other described 323 long-term care facility residents with advanced
innovative oral interventions should be thoroughly dementia and their healthcare proxies for 18 months in 22
explored and discussed with the patient, family, sig- long-term care facilities.7 Data were collected to characterize
nificant others, caregivers, and/or surrogate decision the residents’ survival, clinical complications, symptoms, and
makers. treatments, and to determine the proxies’ understanding of the
5. The autonomy of the patient or surrogate decision residents’ prognoses and the clinical complications expected in
maker should be respected. Emphasis should be placed patients with advanced dementia. Pneumonia, febrile episodes,
on functional status and quality of life. An essential and eating problems were found to be frequent complications
aspect of the process involves cultural, religious, in patients with advanced dementia, and these complications
social, and emotional sensitivity to the patient’s value were associated with a high 6-month mortality rate.7
system. A time-limited trial of nasogastric feedings Other near end-of-life conditions include chronic disease
may be considered if a decision to proceed in the future processes that progress to an end stage, leaving the patient with
with a G-tube is made. only months, weeks, or even days to live. Acute illnesses can
6. The final informed decision should be reached via a also progress rapidly in the intensive care unit, potentially
patient-centered approach, including family, significant causing irreversible organ damage; with these constraints there
others, caregivers, and/or surrogate decision makers. are significant risks and burdens associated with G-tube place-
7. Clinicians in healthcare institutions, both hospitals and ment that are greater than the benefits to the end-of-life patient.
long-term care facilities, should develop a process that Table 1 lists several types of discomfort commonly experi-
is interdisciplinary, collaborative, proactive, integrated, enced by end-of-life patients with advanced dementia with or
and systematic in order to facilitate decision making without artificial nutrition and hydration (ANH).
that engages the patient, family, significant others, care-
givers, and/or surrogate decision makers. The process
should promote advance directives that provide health-
Literature Review on Decisions to
care based on the patient’s wishes and best interest. Withhold or Withdraw Tube Feeding
Reviews of evidence regarding the clinical risks, burdens, and
Overview of Advanced Dementia and benefits of ANH for patients with advanced dementia and termi-
nal illness have been published by A.S.P.E.N.13 At the cornerstone
Other Near End-of-Life Conditions of decision making is the concept of the “troubling trichotomy”:
People with advanced dementia generally experience eating dif- (1) “can” of nutrition support technology, (2) “should” of bioeth-
ficulties in conjunction with profound loss of memory, verbal, ics, and (3) “must” of the law.13
and functional abilities due to the underlying neurodegenerative Many peer-reviewed articles are available in the scientific
process. Patients with advanced dementia are dependent on oth- literature on the topic of G-tube placement in patients with dif-
ers for all aspects of their care, and must rely on others to make ferent levels of dementia or in the terminal phases of their
decisions about the types of care they receive.5 Many disorders lives.1,6,8,14-18 Numerous authors have addressed the issue of
can cause dementia. Some, such as Alzheimer’s disease or forgoing G-tubes in patients with advanced dementia and at the
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
Schwartz et al 831
Table 1. Advanced Dementia and End-of-Life Suffering/Discomfort With or Without ANH.
Author Findings/Conclusions
Barrocas, Geppert, Artificial hydration of terminally ill patient can lead to discomfort due to:
Durfee, et al8 •• Fluid overload
•• Pulmonary and generalized edema
•• Shortness of breath
•• Use of catheters
•• Additional laboratory tests and blood draws
•• Administration of medications and electrolytes
•• ANH complications
•• Use of physical restraints
ANH may be discontinued on clinical and ethical grounds provided such determination is not in conflict with:
•• Existing laws
•• Institutional policies
•• Consent/consensus of decision makers
Scientific evidence in the physiology of patients with brain death, coma, or PVS indicates that these patients
do not experience thirst or hunger, and therefore not likely to suffer.
Ciocon, Silverstone, ANH in dying patients:
Graver, Foley9 •• Increased diarrhea, nausea, and vomiting
•• Caused repeated aspiration pneumonia
Ellenshaw, Sutcliffe, Fluids cause or exacerbate:
Saunders10 •• Dyspnea
•• Bronchial secretions
•• Urinary frequency
•• Bladder distension
•• Pulmonary edema/effusions
•• Ascites
Friederich11 Adverse occurrences with ANH:
•• Infections at surgical site
•• Perforations
•• Leakage
•• Does not prevent skin breakdown or pressure ulcers despite greater protein intake
McCann, Hall, Ketosis and dehydration, in absence of ANH, provide:
Groth-Juncker12 •• Anesthetic/sedative effects to the terminally ill or advanced demented patients
•• Benefit, as these patients may retain the ability to experience discomfort or suffering
ANH, artificial nutrition and hydration; PVS, persistent vegetative state.
end of life (Table 2), yet a gap exists between evidence-based patient’s general condition. For patients with terminal
facts and practice based on the risks, burdens, and benefits of dementia (eg, irreversible, immobile, unable to communi-
expected short-term and long-term outcomes. cate, completely dependent, lack of physical resources) tube
There are a number of resources8,30,31 for the development feeding is not recommended. The decision for or against tube
of guidelines to address this sensitive issue in combination feeding must always be a personal decision for each patient,
with updated data specific to G-tube placement in patients with made together with caregivers, legal custodians, family,
advanced dementia or near the end of life. ESPEN Guidelines healthcare providers, and therapists. When in doubt and
on Enteral Nutrition32 address some of the ethical and legal when legal advice may be necessary for definitive decision
issues that have become an increasing part of the clinical deci- making, the decision in each case must be made on a case-
sion-making process in providing nutrition support therapy. by-case basis.
These guidelines include ethical and legal aspects of enteral National healthcare organizations that are not specifically
nutrition in relation to dementia and the dying patient. See nutrition focused also have developed position statements
Appendix A online. related to G-tube placement in patients with dementia or near
According to the ESPEN Guidelines on Enteral Nutrition: end of life (Table 3). These documents provide support for not
Geriatrics,33 the outcome and success of nutrition therapy in recommending G-tube placement for this patient population
demented patients are strongly influenced by the severity of and guidelines to help clinicians with the decision-making
the disease, the kind and extent of comorbidities, and by the process.
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
832 Nutrition in Clinical Practice 29(6)
Table 2. Support for Forgoing G-Tubes in Advanced Dementia and Near End-of-Life Conditions.
Authors Findings/Conclusions
19
Haddad, Thomas Cumulative study analyses
•• High mortality and morbidity rates
•• Questionable effectiveness except in critical illness and amyotrophic lateral sclerosis
Oyoga, Schein, Gardezi, Wise20 Mortality rate—100 consecutive patients undergoing G-tube placement in community teaching
hospital
•• 41% 30-day mortality
•• 4% related to procedure
Abuskis, Mor, Segal, et al21 Nursing home patients referred for G-tube placement
•• 87% had dementia
•• 39.5% mortality rate (when intention-to-treat analyses were applied to data)
Grant, Rudberg, Brody22 Mortality rates—81,105 patients following G-tube placement
•• 23% - 30 day
•• 63% - 1 year
•• 81.3% - 3 years
Finucane, Christmas, Travis23 Meta-analysis−5266 nursing home residents
•• No improvement in rates of aspiration pneumonia, pressure sores, survival
•• Decline in activities of daily living
•• Tube feedings in patients with advanced dementia should be discouraged based on clinical grounds
Murphy, Lipman24 Feeding tubes do not prolong survival in patients with dementia
Cervo, Bryan, Farber25 No reduction in oral or gastric aspiration, or pneumonia
Gillick26 Feeding tubes in advanced dementia:
•• Increase mortality, morbidity
•• Often require physical and chemical restraints
•• Increase discomfort
•• Compromise human dignity
Kaw, Sekas27 Feeding tubes in advanced dementia have no long-term proven benefit
Meier, Ahronheim, Morris, Feeding tubes in advanced dementia reduced short-term survival after in hospital placement
Baskin-Lyons, Morrison28 in chronically demented patients with superimposed delirium
Sampson, Candy, Jones29 Cochrane database systematic review revealed:
•• Insufficient evidence to suggest EN benefits in patients with advanced dementia
•• Lacking data on adverse events associated with EN
EN, enteral nutrition. G-tube refers to any long-term enteral access device.
Patient or Caregiver Decision Maker of food through relationships, dietary restriction, sharing and car-
Concerns ing, and the importance of food is formed by the patient’s socio-
economic background and relationships. Speech-language
Addressing the need for shared caregiver-patient experiences pathologists and occupational therapists provide assistance in an
analogous to the strong bonds of food may be key in avoiding effort to enhance oral feedings through patient-centered
unnecessary G-tube placement. Nurturing a patient at the end approaches with careful hand feedings.
of life may include providing both physical comfort measures These findings are consistent with Meares’43 work on the
and other activities to allow for mental engagement, such as relationship between dying cancer patients and caregivers and
listening to music, reading, and looking at photographs. the loss of “dinnertime.” He noted that meanings associated with
Physical comfort measures such as frequent mouth care, skin food were temporal, and provided relational, cultural, ritual, and
care, lubricant eye drops, and pain and antiemetic medications personal significance to subjects.43 Meanings, beliefs, and val-
are easy to deliver and could involve family members or sig- ues related to food should be acknowledged and incorporated
nificant others as caregivers.41 into the decision-making processes for ANH through a G-tube.
The emotional and symbolic meaning of food is rarely exam- When dealing with end-of-life issues, healthcare profession-
ined in the healthcare literature. In one qualitative study, older als do not appear to be prepared for a common statement from
adults considered appropriate for palliative care or who were suf- families: “My family member is going to starve if they do not
fering from advanced progressive or terminal illnesses identified have a feeding tube.” In a 2007 Japanese survey, 70% (n = 354)
the meaning of food as highly symbolic and temporal in nature, of family members expressed a high degree of emotional distress,
reflecting two distinct schemas of “eating to live” and “living to including feelings of helplessness and guilt, when a terminally ill
eat.”42 These schemas reflected the socially constructed memories cancer patient became unable to take nourishment orally.44 Many
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
Schwartz et al 833
Table 3. Healthcare Organizations Supporting Similar Views on Decision Making or G-Tube Placement in Patients With Advanced
Dementia or Near End of Life.
Organizations Standards, Statements, Positions, and/or Guidelines
Academy of Nutrition and In cases where the evidence strongly suggests that feeding or hydration does not provide
Dietetics30,31 benefit, it is the responsibility of the multidisciplinary healthcare team to explain this to
the individual or authorized surrogate, but it is the individual or authorized surrogate who
decides.
Advanced Dementia−Numerous studies found no evidence that enteral tube feeding
provides any benefit in terms of survival time, mortality risk, quality of life, nutrition
parameters, physical function, or improvement or reduced incidence of pressure ulcers.
Other studies indicate that feeding tube insertion in nursing facility residents was
associated with poor survival and a significant increase in the use of healthcare services
after insertion. Rather than enteral tube feeding, the preferred intervention for providing
nutrition is usually total assistance with oral feedings.
American Academy of Hospice and Do not recommend percutaneous feeding tubes in patients with advanced dementia; instead,
Palliative Medicine34 offer oral assisted feeding.
American College of Physicians35 Artificial administration of nutrition and fluids is a medical intervention subject to the same
principles of decision making as other treatments. Imminently dying patients may develop
fluid overload as their kidneys stop functioning, with peripheral and pulmonary edema;
continued administration of intravenous fluids exacerbates these symptoms and may
cause substantial distress.
American Geriatric Society5 Percutaneous feeding tubes are not recommended for older adults with advanced dementia.
American Medical Association36,37 Life-sustaining treatments should provide medical benefits and should respect a patient’s
preferences, as communicated by the patient or a legally recognized surrogate. Treatments
such as mechanical ventilation and artificial nutrition and hydration should be provided
only with appropriate authorization from a patient, a surrogate, or court.
American Nurses Association ANA believes that adults with capacity or, in the event of incapacity, their surrogates are in
(ANA)38 the best position to weigh the harms and benefits of nutrition and hydration as evaluated
and discussed with them by the healthcare team. The acceptance or refusal of food and
fluids, whether delivered by normal or artificial means must be respected. This belief is
consistent with the ANA’s expressed values and goals relative to respect for autonomy,
relief of suffering, and expert care at the end of life.
American Society for Parenteral Artificial nutrition and hydration may not provide any benefit and may have associated
and Enteral Nutrition8 risks in patients with severe dementia or in a persistent vegetative state.
European Society of Parenteral and Guidelines on Enteral Nutrition: Ethical and Legal Aspects of Enteral Nutrition Dealing
Enteral Nutrition32 with Dementia and the Dying Patient (see Appendix A online)
In the late stages of disease (Alzheimer’s or cerebrovascular dementia), the balance of
evidence is that artificial tube feeding has more risks than benefits and should not be
undertaken. In recent studies of terminal dementia, it was shown that tube feeding does
not prolong life and causes more complications than benefits.
National Association of Social Social workers shall incorporate assessments in developing and implementing intervention
Workers39 plans that enhance the clients’ abilities and decisions in palliative and end-of-life care.
Hospice and Palliative Nurses HPNA is committed to compassionate care of persons at the end-of-life. HPNA believes
Association (HPNA)40 that the decision to initiate, withhold, or withdraw artificial nutrition and hydration
should be made by the patient and family with accurate and nonjudgmental input from the
healthcare team.
G-tube refers to any long-term enteral access device.
perceived a necessity for improvement in professional practice. A healthcare professionals confront.45 A recent review studied
recommended care strategy developed from the study and patients admitted from 2000 to 2007 and represented 2797 acute
addressed 4 major domains: (1) relieving the family members’ care hospitals with 280,869 admissions among 163,022 long-term
sense of helplessness and guilt; (2) providing up-to-date informa- care facility residents with advanced cognitive impairment.45
tion about hydration and nutrition at the end of life; (3) under- Certain factors were associated with increased rates of feeding
standing family members’ concerns and providing emotional tube insertion, even after adjusting for patient-level characteris-
support; and (4) relieving the patient’s symptoms.44 tics. These factors included for-profit ownership, larger hospital
The decision to place a feeding tube in a patient with advanced size, and greater intensive care use. Inserting a feeding tube in a
dementia is one of the sentinel decisions that family members and patient with advanced cognitive impairment demonstrated a gap
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
834 Nutrition in Clinical Practice 29(6)
Table 4. Risks, Burdens, and Benefits Comparison for G-Tube Placement in Patients With Advanced Dementia or Near End of Life. 8,14,16-18,31,46
Risks and Burdens Benefits
Aspiration Artificial nutrition and hydration may help to prevent more serious
Cellulitus, stomal inflammation, excoriation at tube site debilitating conditions, when used at the early signs of malnutrition
Deprived pleasure of eating Decreased distress in patients who experience coughing and choking
Diarrhea with oral intake
Fluid overload Preservation of ability to perform simple instrumental daily life
Gastrointestinal and venous distention activities
Increased use of pharmacological sedation Relief of dehydration
Increased use of restraints Weight maintenance
Nausea and vomiting
Negative impact on quality of life through decreased social
interaction at mealtime or decreased delivery of attention
required during assisted oral feeding
Not associated with improved survival based on feeding tube
insertion timing, relative to onset of eating problems
Peritonitis
Tube occlusion
G-tube refers to any long-term enteral access device.
between the existing practice and lack of patient benefit in the Decision-Making Processes for Artificial
studied population.45 This study called for multifactorial interven- Nutrition
tions to ensure that the insertion of feeding tubes during acute hos-
pitalization was consistent with patient preferences after thorough Respect for autonomy is essential, defined as the individual’s
discussion of the risks, burdens, and benefits. Most importantly, right to self-determination as expressed in healthcare decision
nutrition support experts must clarify with the decision makers making; this may not be possible when the patient has a
what the underlying illness and prognosis is to help with their decreased mental capacity. Unfortunately, if the individual has
decision process. By indicating if the treatment being provided is not expressed their wishes prior to their decline in mental
curative, rehabilitative, or palliative, those involved in the deci- capacity either verbally to a surrogate decision maker or in an
sion-making process can determine if the treatment is right for advance directive, someone else will be required to make the
them. Only then can a decision about long-term enteral access healthcare decisions for them.
device placement be made. A systematic review was conducted to examine how treat-
ment decisions for ANH were made when patients exhibited
decreased mental capacity.47 From 1990 to 2011, 66 studies
Risks, Burdens, and Benefits of G-Tube
were identified, comprising data from 40 countries and 34,649
Placement patients, caregivers, and clinicians.47 Of the papers analyzed, 49
In order to prevent inappropriate placement of long-term involved individuals with dementia, 30 involved people with
enteral access devices, the risks, burdens, and benefits acquired brain injuries, and only 4 examined individuals with
should be addressed prior to their placement in patients with intellectual disabilities. Six themes emerged: (1) clinical indica-
advanced dementia or at the end of their life. Patients with a tions were similar across countries but were insufficient alone
terminal disease, such as cancer or respiratory failure, or for determining outcomes; (2) quality of life was the main fac-
those unwilling to continue medical treatment for similar tor in deciding treatment, but its meaning varied; (3) prolonging
conditions due to quality of life factors would be considered life was the second most-cited factor; (4) patient’s wishes were
near end of life. The particular aspects of these risks, bur- influential but not determinative; (5) families had some influ-
dens, and benefits of feeding for G-tube placement in this ence but were infrequently involved in final recommendations;
patient group are identified in Table 4. It is also important to and (6) clinicians often felt conflicted about their roles. Based
acknowledge the focus of patient-centered care; as each per- on the results of the literature review,47 implications for clinical
son is a unique individual, they may perceive the risks, bur- practice were identified and are listed in Appendix B of the
dens, and benefits differently. When G-tube placement is online data supplement that accompanies this paper.
being considered, it is important to consider the variance in Decision making regarding ANH can also involve a time-
perception in the obligatory discussion with the healthcare limited trial. For example, a hospitalized patient with advanced
team, family, or significant others. dementia is admitted with aspiration pneumonia and is on
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
Schwartz et al 835
mechanical ventilation. The patient’s family or significant hospital for a variety of reasons. These reasons may be related to
other is asked to make a decision about placement of a G-tube. financial issues, limited staffing to feed patients requiring additional
Some families may need time to mentally process the medical time and care for hand feeding, reimbursement factors, and other
information about the risk, burdens, and benefits of artificial concerns.49,50 Long-term care facility requirements driving feeding
nutrition. The clinician could then suggest a time-limited trial tube placement in patients with advanced dementia in acute care
of 1 week or other realistic jointly agreed-upon time period for hospitals needs to be better addressed to reduce inappropriate
the placement of a nasogastric tube feeding to determine if the G-tube placement. Education of family members, significant oth-
patient is able to be extubated and resume an oral diet with ers, and healthcare professionals alike is the fundamental first step
modified food and fluid consistency as needed. toward the sensible use of these feeding tubes.49
Acute Care Hospital and Long-Term Care Development of a Systematic Process to
Facility Roles in Feeding Tube Placements Prevent Ethical Dilemmas With G-Tube
in Patients With Dementia Placement in Patients With Dementia
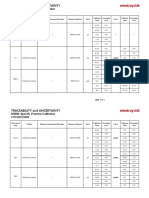
The 2000 Minimum Data Set (MDS), which contains data on A collaborative algorithm for decision making, such as the one
long-term care facility residents living in all Medicare-certified illustrated in Figure 1, along with a checklist (Figure 2) for use
or Medicaid-certified facilities in the United States, was exam- prior to ordering G-tube or other long-term enteral access
ined for this study.48 The study population was further parti- device placement in patients with dementia or near end of life
tioned into a subset having a feeding tube inserted within a is useful for clinicians. This special report does not intend to
year of their first MDS assessment (N = 5209). Two-thirds of focus on the long-term enteral access device selection related
all feeding tubes (68.1%) were inserted during an acute care to optimum location (gastric vs small bowel) or the type of
hospitalization. The most common primary diagnoses associ- insertion options (endoscopic, laparoscopic, fluoroscopic, and
ated with feeding tube insertion during a hospitalization open techniques/surgical),51 but rather intends to demonstrate
included aspiration pneumonia, dehydration, dysphagia, uri- that these feeding tubes are not recommended in patients with
nary tract infection, malnutrition, and pneumonia,48 although advanced dementia or near end of life.
no evidence exists that feeding tubes reduce the risk of any of Clinicians frequently care for patients for whom long-term
these problems. Outcomes in the year following the procedure enteral tube feeding is considered. The substantial increase in the
were poor: 64.1% died in the year following the procedure, and use of endoscopically placed tubes for long-term feeding reflects
1 in 5 tube-fed residents experienced a tube-related complica- the aging population, advances in medicine and technology, and
tion necessitating a hospital transfer. According to this study,48 inadequate advance care planning. Confusion regarding medical
long-term care facility residents who had a feeding tube and ethical guidelines for long-term tube feeding often exists
inserted were less likely to have an advance directive limiting among clinicians, patients, and surrogate decision makers.52
aggressive care than those who did not get tube-fed. In addi- There is a need for improved education for physicians, patients,
tion, tube-fed long-term care facility residents had a lower like- family members, significant others, caregivers, and surrogate
lihood of having a designated healthcare proxy through a decision makers about the use of long-term enteral access devices
durable power of healthcare attorney. and the ethical implications in specific patient populations.
An important finding of this study48 was that the focal point Integrating concepts of patient-centered care, shared deci-
of decision making for feeding tubes among long-term care sion making, health literacy, and the teach-back method of edu-
facility residents with advanced dementia occurred in an acute cation enhances ethical dilemma prevention53 (Table 5). The
care hospitalization. If the decision to insert a feeding tube was concepts to be stressed during this discussion should include
primarily occurring at the hospital rather than in the long-term respect for autonomy (an individual’s right to self-determina-
care facility, the researchers raised questions about the extent to tion as expressed in healthcare decision making, either verbally
which advance directives were being followed, and whether or in an advance directive), surrogate decision making, cultural
alternatives such as hand-feeding could be sustained during an and religious diversity, enteral nutrition through a tube as a
acute care hospitalization.48 Knowing the final location of deci- medical therapy, and the importance of advance care planning.
sion making for tube insertions is crucial in order to adequately The process should incorporate current literature; engage
target and shape interventions to decrease the presumed overuse the patient, family, significant others, caregivers, and/or sur-
of feeding tubes. These results support further observations that rogate decision makers; and utilize advance directives to pro-
the providers in the hospital setting need to be targeted for inter- vide healthcare by clinicians, based on the patient’s wishes.
ventions aimed at improving this decision-making process. Physician Orders for Life-Sustaining Treatment (POLST) are
Long-term care facilities may require G-tube placement in spe- forms that may be used in hospitals and long-term care facili-
cific patients prior to transferring the patient from the acute care ties that also address a patient’s wishes.
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
836 Nutrition in Clinical Practice 29(6)
Patient Admitted With Dementia,
Declining PO Intake and Possible Aspiration
Physician or Designee
Coordinates Collegial Patient-Centered Care, Shared Decision-Making Process
Reviews Advance Directive, Identifies Surrogate Decision Maker
Communicates and Collaborates with Healthcare Team and Surrogate Decision Maker
Documents in Electronic Health Record along with Healthcare Team Members
Registered Nurse Registered Registered Speech-Language
(RN) Dietitian (RD) Pharmacist (RPh) Pathologist (SLP)
Coordinates MD orders Initiates Nutrition Care Coordinates medication Bedside swallow
with bedside care Process (NCP) needs with MD. evaluation.
Interacts with Interacts with Interacts with Interacts with
healthcare team and healthcare team and healthcare team and healthcare team and
surrogate decision surrogate decision surrogate decision surrogate decision
maker maker maker maker
Social Worker Optimizes PO intake Recommends food/ Video swallow
Assists with obtaining fluid consistency study
with small frequent
advance directive, social meals, nutrient dense,
needs, emotional Pass–continue Fail–address
comfort foods, and current diet feeding decision
support with emphasis
on culture, values, and feeding assistance options
faith diversity Determines best route of
medication administration
Palliative Care Consult for RN, RD, RPh, SLP completes Case
Quality of life goal discussion checklist Prior to G-tube placement
with surrogate decision maker
Manager
MD discusses with surrogate decision maker Assists with
feeding options and explains goals patient
Spiritual Care Supports Family Care Conference placement
surrogate decision maker and options
religious aspects of care
RN coordinates RD continues NCP, RPh continues to SLP provides feeding
MD orders with recommends feeding address medication options to surrogate
bedside care components (if G-tube administration routes decision maker if
Interacts with all placed) or oral feedings based on patient decision made not to
healthcare providers based on patient wishes for G-tube or place G-tube,based on
and surrogate wishes and/or best oral feedings patient wishes and/or
decision maker interest of patient best interest of patient
Figure 1. Collaborative algorithm process prior to gastrostomy tube placement in patients with dementia. G-tube, gastrostomy tube;
PO, per os. G-tube refers to any long-term enteral access device.
Limiting Factors for Practice Change lack of awareness, knowledge deficit, ineffective communica-
tion, misconceptions, and conflicting role of healthcare profes-
Appendix C (online) lists some of the limiting factors for practice sionals. They also include the lack of advance directives that
change that lead to inappropriate G-tube placement in patients define the plan of treatment for terminal illness, as well as the
with dementia or near end of life. Although not all of these factors concern by healthcare providers over malpractice issues. It also
may be present at each healthcare facility, the list provides an touches on the lack of awareness by the patient’s family or sig-
opportunity to establish an interdisciplinary and systematic pro- nificant other, and/or surrogate decision maker over the potential
cess to facilitate decision making that incorporates the patient, use of restraints if the patient is pulling at their feeding tube.
family, significant others, caregivers, and/or surrogate decision Education is a key element required to address the factors
makers’ engagement. It also promotes the use of advance direc- identified for all stakeholders—from the patient, family, sig-
tives to provide healthcare based on the patient’s wishes and best nificant others, caregivers, and/or surrogate decision makers to
interest. The items listed in Appendix C predominately deal with the healthcare providers and facility administrators. Care can
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
Schwartz et al 837
Clinical Presumed oral intake will provide insufficient nutrition and/or is unsafe due to
indication possible aspiration for period greater than 4 weeks on nasogastric tube feeding?
Yes No
Determined the correct location of the long-term enteral access device based on the
gastrointestinal tract function? Yes No
Swallow Was a video swallow study completed? Yes No
evaluation If yes, when? Was this abnormal? Specify.
Consistent with Is use of tube consistent with patient’s preferences as supported by patient’s quality of
patient’s wishes life goals? Yes No
Preferences How have patient’s preferences, goals, and values been obtained?
obtained for tube (Check all that apply.)
placement Discussed directly with patient
Discussed with patient’s surrogate (for patient lacking decision-making
capacity)
Documented in patient’s advance directive and/or POLST form
Other (specify):
Surrogate Committee formed to make decision on patient’s behalf? Yes No
Preferences Are patient’s preferences, goals, and values formally documented in medical record or
documented Surrogate Committee? Yes No If yes, date:
Medical Is patient’s medical condition expected to remain stable to discharge?
condition stable Yes No
Expected Is patient expected to survive for at least 30 days post tube placement?
survival time Yes No
Primary driving Patient preference Family preference Physician
force for tube Skilled nursing facility requirement; facility name
Other
Are any following conditions present? (This list is not comprehensive. Check if
Potential condition is present or write in any condition that would qualify as “other”.)
contraindications Serious coagulation disorder
Status post cardiac arrest with poor neurological function after 48-72 hours
Extensive tumor infiltration of stomach
End stage dementia (bed-bound, incontinent, nonverbal, dysphagia with
history of aspiration)
Multiorgan failure greater than 3 organs nonreversible
Stage 4 cancer with life expectancy of less than 6 months
Significant intracranial bleed with expected permanent ventilator dependence
Complete obstruction of bowel
Marked peritoneal carcinomatosis
Severe ascites
Peritonitis
Severe psychosis
Other ____________________________________________________________
Clearly limited life expectancy, specify:
Recommendation Based on above answers, is patient appropriate for tube? Yes No If No,
recommend consults for discussion/decision making with patient, family, caregiver,
surrogate decision maker for feeding option needs by: Dietitian
Speech-Language Pathologist Pharmacist Palliative Care Ethics
POLST, physician’s orders for life-sustaining treatment. *Includes gastrostomy, gastrojejunal, jejunal tube
with placement options: endoscopic, laparoscopic, or fluoroscopic;percutaneous endoscopic gastrostomy
tubemost commonlong-term enteral accessdevice.
Figure 2. Checklist prior to gastrostomy tube or other long-term enteral access device placement.
be improved by requiring the knowledge of advance directives Preparing for the Conversation With
in the same way allergy listings are required once a patient is Patient, Family, Significant Other,
admitted for care. Such requirements create systems within
Caregiver, and/or Surrogate Decision
healthcare that better reframe patient-provider relationships
around the question, “What matters most to you?”59 For Maker
patients who are not able to provide this information, surrogate The decision process dealing with the placement of G-tubes in
decision makers will need to indicate, “What would matter patients with dementia or near end of life can benefit from con-
most to the patient if they could speak for themselves?”59 This cepts being developed by the Institute for Healthcare
patient-centered approach will prevent unnecessary medical Improvement (IHI).59 The IHI, an independent not-for-profit
therapies, including tube feedings that do not meet the patient’s organization, is a leading innovator in health and healthcare
quality of life goals. improvement worldwide. According to the IHI, many healthcare
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
838 Nutrition in Clinical Practice 29(6)
Table 5. Patient-Centered Care Concepts.
Concept Definition
54
Health literacy •• Degree to which individuals obtain, process, and understand basic health information to make
informed health decisions.
•• Major problem as to patient’s understanding of what healthcare provider says to them.
Patient-centered care31,55,56 •• Defined by Institute of Medicine Care that is respectful of and responsive to individual patient
preferences, needs, and values and ensures that patient values guide all clinical decisions.
•• Clinicians and healthcare system to shift focus away from diseases and back to patient and family.
•• Active engagement of patients when fateful healthcare decisions must be made.
•• Focuses on improving health literacy.
Preventive ethics57 •• Activities performed by an individual or group on behalf of a healthcare organization to identify,
prioritize, and address systemic ethics issues.
•• Proposes that ethical conflict is largely preventable and can be avoided with proactive interventions
aimed at the organization, unit, and individual levels.
•• Goal to use a proactive approach, to identify common triggers of ethical conflict, and to address these
triggers before they contribute to conflict.
•• Represents a dramatic shift from the traditional ethics approach, which uses a case-by-case approach.
Shared decision making56 •• Patients should be educated about the essential role they play in decision making and be given
effective tools to help them understand their options and the consequences of their decisions.
•• Patients should receive the emotional support they need to express their values and preferences and be
able to ask questions without censure from their clinicians.
•• Clinicians need to relinquish their authoritative role and train to become more effective coaches or partners.
•• Shared decision making is the pinnacle of patient-centered care.
Teach-back method58 •• Ensures that individuals understand what they have been taught.
•• Asking patient to explain or demonstrate what they have been taught.
•• If patient does not explain correctly, individual retaught using a different method and then asked again
to explain or demonstrate what they have been taught.
organizations have no processes in place to prompt discussions 4. Exemplify this work in our own lives so that we under-
with patients, families, caregivers, and/or surrogate decision stand the benefits and challenges.
makers about healthcare directives or end of life wishes.59 If this 5. Connect in a manner that is culturally and individually
has not already been done, the optimal time to record, access, respectful of each patient.
and follow these instructions is at the time the patient is admit-
ted, rather than later during the hospitalization. Ideally, patients A cohesive team approach can be achieved by incorporating
and their families discuss and refine advance directives gradu- these concepts: the physician should be in charge of overall
ally over time, before an illness or hospitalization, working with management of the patient; the bedside registered nurse should
a familiar healthcare provider whom the patient knows and interact continuously with the patient and the patient’s family
trusts and who understands the patient’s unique values, instead or significant other; the registered dietitian should apply the
of working with unfamiliar providers in a crisis situation. nutrition care process; the pharmacist should consult on medi-
IHI and a group of end-of-life experts and concerned health- cation administration alternatives for patients on tube feedings
care organizations have launched the “Conversation Ready” or with altered swallowing ability; and the speech pathologist
initiative.60 This group is committed to developing and enact- and occupational therapists should present oral feeding alter-
ing processes to create systems that reframe patient-provider natives. All of these clinicians in addition to the bedside nurse
relationships around the question, “What matters most to would interact with the patient, patient’s family, or significant
you?” IHI is organizing a broader “Conversation Ready Health other to provide information and education. A stronger, more
Care Community” for organizations committed to working to interactive, and more collaborative position between all of
develop reliable care processes based on the following core these clinicians cannot be overemphasized. To enhance facili-
principles: tation of what is most appropriate for the patient, there must be
cohesion between these roles. With the constant interaction
1. Engage with our patients and families to understand between these disciplines, from working together at the bed-
what matters most to them at the end of life. side, to meeting with the physician and others, collaboration
2. Steward this information as reliably as we do allergy regarding patient needs, desires, and the appropriateness of
information. feeding can be collectively determined. Early involvement
3. Respect patient’s wishes for care at the end of life by with a palliative care team would also be beneficial in recog-
partnering to develop shared goals of care. nizing the patient’s expected decline and need for long-term
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
Schwartz et al 839
support given their impediment in decision making concerning Nutrition (A.S.P.E.N.). The authors wish to acknowledge the
their medical therapy.61 A.S.P.E.N. Board of Directors for providing final approval (Daniel
The decision-making tools for patients with dementia Teitelbaum, MD; Ainsley Malone, MS, RD, CNSC; Gordon Sacks,
included in this special report will provide direction and may PharmD, BCNSP, FCCP; Charlene W. Compher, PhD, RD, CNSC,
be placed in every patient’s chart as the guideline for continued LDN, FADA, FASPEN; Lawrence A. Robinson, BS, MS, PharmD;
Phil Ayers, PharmD, BCNSP, FASHP; Albert Barrocas, MD,
evaluation of patients with declining oral intake. This informa-
FACS, FASPEN; Bryan Collier, DO, CNSC, FACS; M. Molly
tion may be made readily available for patients, family, signifi- McMahon, MD; Christina J. Valentine, MD, MS, RD; Jennifer A.
cant others, caregivers, and/or surrogate decision makers who Wooley, MS, RD, CNSC; and Charles W. Van Way III, MD,
are dealing with decisions about G-tube placements for indi- FASPEN) as well as A.S.P.E.N. Staff: Jennifer Kuhn, MPS; Donna
viduals near end of life. Interdisciplinary education, collabora- Klinger; and Kimberly Rosenfield. The authors acknowledge the
tion, and integration with family, significant others, caregivers, following individuals for their efforts in the development of this
and/or surrogate decision makers are vital to the proper man- special report: Colleen Christmas, MD, FACP; Trisha Fuhrman,
agement of these patients and cannot be overemphasized. MS, RDN, LD, FAND; and Laura Matarese, PhD, RD, LDN,
CNSC, FADA, FASPEN.
Conclusion
References
The decision not to perform G-tube placement in a patient with
1. Sampson EL, Candy B, Jones L. Enteral tube feeding for older people with
advanced dementia or near end of life is acceptable and sup-
advanced dementia. Cochrane Database Syst Rev. 2009;(2):CD007209.
ported by current scientific evidence. Advanced dementia should 2. Hanson LC. Tube feeding versus assisted oral feeding for persons with
be seen by the healthcare team as a terminal illness and profes- dementia: using evidence to support decision-making. Annals of Long
sionals can communicate this information to the patient’s family Term Care: Clinical Care and Aging. 2013;21(1):36-39.
or significant others. A thorough discussion should take place 3. Teno JM, Gozalo PL, Mitchell SL, et al. Does feeding tube insertion and
its timing improve survival? J Am Geriatr Soc. 2012;60(10):1918-1921.
with the patient, family, significant others, caregivers, and/or
4. Givens JL, Selby K, Goldfield KS, Mitchell SL. Hospital transfers
surrogate decision makers, touching on the risks, burdens, and of nursing home residents with advanced dementia. J Am Geriatr Soc.
benefits, as well as the most updated evidence-based findings. 2012;60(5):905-909.
The final informed decision should be reached by all members 5. American Geriatric Society. Feeding tubes in advanced dementia: position
of the healthcare team using a patient-centered approach. statement, May 2013. Available at: http://www.americangeriatrics.org/
files/documents/feeding.tubes.advanced.dementia.pdf. Accessed January
The autonomy of the patient or surrogate decision maker
27, 2014.
should be respected and considered above all other ethical 6. National Institute of Neurological Disorders and Stroke. Reducing the
principles. Emphasis should be placed on functional status and burden of neurological disease: dementia information page. Available at:
quality of life. Cultural, religious, social, and emotional sensi- http://www.ninds.nih.gov/disorders/dementias/dementia.htm. Assessed
tivity is essential in the process. July 12, 2014.
7. Mitchel SL, Teno JM, Kiely DK, et al. The clinical course of advanced
Healthcare institutions, both hospitals and long-term care
dementia. N Engl J Med. 2009;361(16):1529-1538.
facilities, should develop a systematic process to facilitate deci- 8. Barrocas A, Geppert G, Durfee SM, et al; A.S.P.E.N. Board of Directors.
sion making that promotes advance directives to provide health- A.S.P.E.N. ethics position paper. Nutr Clin Pract. 2010;25(6):672-679.
care based on the patient’s wishes and best interest. The role of 9. Ciocon JO, Silverstone FA, Graver LM, Foley CJ. Tube feedings in
education for all stakeholders in the process of patient-centered elderly patients: indications, benefits and complications. Arch Intern Med.
1988;48(2):429-433.
care is essential. Awareness and application of knowledge will
10. Ellenshaw JE, Sutcliffe JM, Saunders CM. Dehydration and the dying
be required to resolve the practice gap between evidence-based patient. J Pain Symptom Manage. 1995;10(3):192-197.
medicine and G-tube use in patients with advanced dementia or 11. Friederich L. End-of-life nutrition: is tube feeding the solution? Annals of
near end of life, including risks, burdens, benefits, and expected Long Term Care: Clinical Care and Aging. 2013;(10):30-33.
short-term and long-term outcomes. 12. McCann RM, Hall WJ, Groth-Juncker A. Comfort care for the termi-
nally ill patients: the appropriate use of nutrition and hydration. JAMA.
Although this special report on G-tube placement is
1994;272(16):1263-1266.
intended for use in a specific patient population, concepts pre- 13. Geppert CMA, Barrocas A, Schwartz DB. Ethics and law. In: Mueller C,
sented in the paper, along with the tables and figures, may be Kovacevich DS, McClave SA, Schwartz DB, eds. The A.S.P.E.N. Adult
applied to other patients if used in conjunction with scientific Nutrition Support Core Curriculum. 2nd ed. Silver Spring, MD: American
information about that defined patient population. Ideally, this Society for Parenteral and Enteral Nutrition; 2012:656-676.
14. Cullen S. Symposium 1: options in enteral feeding. To perform percutane-
special report will serve as an educational tool to engage clini-
ous endoscopic gastrostomy or not to perform endoscopic gastrostomy:
cians and administrators in practice changes to improve care to that is the question. Gastrostomy tube feeding in adults: the risks, benefits
patients with dementia and near end of life conditions. and alternatives. Proc Nutr Soc. 2011;70:293-298.
15. Pivi GA, Bertolucci PH, Schultz RR. Nutrition in severe dementia. Curr
Gerontol Geriatr Res. 2012;2012:983056.
Acknowledgments 16. Glick SM, Jotkowitz AB. Feeding dementia patients via percutaneous
This article was developed by the International Clinical Ethics endoscopic gastrostomy. Annals of Long Term Care: Clinical Care and
Section (ICES) of the American Society for Parenteral and Enteral Aging. 2013;21:32-34.
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
840 Nutrition in Clinical Practice 29(6)
17. Teno JM, Gozalo P, Mitchell SL, Kuo S, Fulton AT, Mor V. Feeding 39. National Association of Social Workers. NASW standards for social work prac-
tubes and the prevention or healing of pressure ulcers. Arch Intern Med. tice in palliative and end of life care, 2013. Available at: http://www.social-
2012;172(9):697-701. workers.org/practice/bereavement/standards/. Accessed January 27, 2014.
18. Pivi GA, Bertolucci PH, Schultz RR. Nutrition in severe dementia. Curr 40. Hospice and Palliative Nurses Association. HPNA position statement:
Gerontol Geriatr Res. 2012;2012:983056. artificial nutrition and hydration in advanced illness, 2011. Available at:
19. Haddad RY, Thomas DR. Enteral nutrition and enteral tube feeding: http://www.hpna.org/pdf/Artifical_Nutrition_and_Hydration_PDF.pdf.
review of the evidence. Clin Geriatr Med. 2002;18(4):867-881. Accessed January 27, 2014.
20. Oyoga S, Schein M, Gardezi S, Wise L. Surgical feeding gastrostomy: are 41. Monturo CA. Artificial nutrition, advance directives and end of life in
we overdoing it? J Gastrointest Surg. 1999;3(2):152-155. nursing homes. In: Preedy VR, ed. The Handbook of Nutrition and Diet in
21. Abuskis G, Mor M, Segal N, et al. Percutaneous endoscopic gastros- Palliative Care. Oxford: CRC Press Taylor and Francis; 2011:171-181.
tomy: high mortality in hospitalized patients. Am J Gastroenterol. 42. Monturo CA, Strumpf NE. Food, meaning and identity among aging vet-
2000;95(1):128-132. erans at end of life. J Hosp Palliat Nurs. In press.
22. Grant MD, Rudberg MA, Brody JA. Gastrostomy placement among hos- 43. Meares CJ. The “Dinner Hour” and Other Losses: Caring for a Hospice
pitalized Medicare beneficiaries. JAMA. 1998;271(24):1973-1976. Patient Who Ceased Nutrition. Thesis. Boston: Boston College; 1995.
23. Finucane TE, Christmas C, Travis K. Tube feeding in patients with 44. Yamagishi A, Morita T, Miyashita M, Sato K, Tsuneto S, Shima Y. The care
advanced dementia: a review of the evidence. JAMA. 1999;282(14): strategy for families of terminally ill cancer patients who become unable to take
1365-1370. nourishment orally: recommendations from a nationwide survey of bereaved
24. Murphy LM, Lipman TO. Percutaneous endoscopic gastrostomy family members’ experiences. J Pain Symptom Manage. 2010;40(5):671-683.
does not prolong survival in patients with dementia. Arch Intern Med. 45. Teno JM, Mitchell SL, Gozalo PL, et al. Hospital characteristics associ-
2003;163(11):1351-1353. ated with feeding tube placement in nursing home residents with advanced
25. Cervo FA, Bryan L, Farber S. To PEG or not to PEG: a review of evidence cognitive impairment. JAMA. 2010;303(6):544-550.
for placing feeding tubes in advanced dementia and the decision-making 46. Frieman M, Minsky J, Grodin MA. Initiating tube feeding in the demented
process. Geriatrics. 2006;61(6):30-35. elderly: motivation for change. J Palliative Care Med. 2012;3:153.
26. Gillick MR. Rethinking the role of tube feeding in patients with advanced 47. Clarke G, Harrison K, Holland A, Kuhn I, Barclay S. How are treatment
dementia. N Engl J Med. 2000;342(3):206-210. decisions made about artificial nutrition for individuals at risk of lacking
27. Kaw M, Sekas G. Long-term follow-up of consequences of percutaneous capacity? A systematic literature review. PLoS One. 2013;8(4):e61475.
endoscopic gastrostomy (PEG) tubes in nursing home patients. Dig Dis 48. Kuo S, Rhodes RL, Mitchell SL, Mor V, Teno JM. Natural history of
Sci. 1994;39(4):738-743. feeding-tube use in nursing home residents with advanced dementia. J Am
28. Meier DE, Ahronheim JC, Morris J, Baskin-Lyons S, Morrison RS. High Med Dir Assoc. 2009;10:264-270.
short-term mortality in hospitalized patients with advanced dementia: lack 49. Finucane TE, Christmas C, Leff BA. Tube feeding in dementia: how
of benefit of tube feeding. Arch Intern Med. 2001;161(4):594-599. incentives undermine health care quality and patient safety. J Am Med Dir
29. Sampson EL, Candy B, Jones L. Enteral tube feeding for older people with Assoc. 2007;8(4):205-208.
advanced dementia. Cochrane Database Syst Rev. 2009;(2):CD007209. 50. Geppert CM, Andrews MR, Druyan ME. Ethical issues in artificial
30. O’Sullivan Maillet J, Schwartz DB, Posthauer ME; Academy of Nutrition nutrition and hydration: a review. JPEN J Parenter Enteral Nutr. 2010;
and Dietetics. Position of the Academy of Nutrition and Dietetics: 34(1):79-88.
ethical and legal issues in feeding and hydration. J Acad Nutr Diet. 51. Bankhead R, Boullata J, Brantley S; A.S.P.E.N. Board of Directors.
2013;113(6):828-833. Enteral nutrition practice recommendations. JPEN J Parenter Enteral
31. Schwartz DB, Posthauer ME, O’Sullivan Maillet J. Practice paper of Nutr. 2009;33(2):122-167.
Academy of Nutrition and Dietetics: ethical and legal issues of feeding 52. McMahon MM, Hurley DL, Kamath PS, Mueller PS. Medical and
and hydration. J Acad Nutr Diet. 2013;113(7):981. ethical aspects of long-term enteral tube feeding. Mayo Clin Proc.
32. Korner U, Bondolfi A, Bühler E, et al. Introduction part to the ESPEN 2005;80(11):1461-1476.
guidelines on enteral nutrition: ethical and legal aspects of enteral nutri- 53. Schwartz DB. Integrating patient-centered care and clinical ethics into
tion. Clin Nutr. 2006;25(2):196-202. nutrition practice. Nutr Clin Pract. 2013;28(5):543-555.
33. Volkert D, Berner YN, Berry E, et al. ESPEN guidelines on enteral nutri- 54. Carbone ET, Zoellner JM. Nutrition and health literacy: a system-
tion: geriatrics. Clin Nutr. 2006;25(2):330-360. atic review to inform nutrition research and practice. J Acad Nutr Diet.
34. American Academy of Hospice and Palliative Medicine. Five things phy- 2012;112(2):254-265.
sicians and patients should question. Available at: http://www.aahpm.org/ 55. Reuben DB, Tinetti ME. Goal-oriented patient care: an alternative health
uploads/aahpmchoosingwisely5thingsphysicianspatientsshouldquestion. outcomes paradigm. N Engl J Med. 2012;366(9):777-779.
pdf. Accessed January 27, 2014. 56. Barry MJ, Edgman-Levitan S. Shared decision making: the pinnacle of
35. Snyder L. American College of Physicians Ethics Manual: sixth edition. patient-centered care. N Engl J Med. 2012;366(9):780-781.
Ann Intern Med. 2012;156:73-104. 57. Epstein EG. Preventive ethics in the intensive care unit. AACN Adv Crit
36. American Medical Association. AMA policy on provision of life-sustain- Care. 2012;23(2):217-224.
ing medical treatment. Available at: http://www.ama-assn.org/ama/pub/ 58. Weiss BD. Health literacy and patient safety: help patients understand
physician-resources/medical-ethics/about-ethics-group/ethics-resource- manual for clinicians, 2nd ed. May 2007. American Medical Association
center/end-of-life-care/ama-policy-provision-life-sustaining-medical. website. Available at: http://www.ama-assn.org/ama1/pub/upload/
page. Accessed January 27, 2014. mm/367/healthlitclinicians.pdf. Accessed January 27, 2014.
37. American Medical Association. AMA statement on end-of-life care. 59. Institute for Healthcare Improvement. Conversation Ready Health
Available at: http://www.ama-assn.org/ama/pub/physician-resources/ Care Community. Available at: http://www.ihi.org/offerings/Member
medical-ethics/about-ethics-group/ethics-resource-center/end-of-life- shipsNetworks/collaboratives/ConversationReadyCommunity/Pages/
care/ama-statement-end-of-life-care.page. Accessed January 27, 2014. default.aspx. Accessed January 27, 2014.
38. American Nurses Association Board of Directors. Position state- 60. Schwartz DB, Pontes-Arruda A. Integrating the “conversation ready” ini-
ment: forgoing nutrition and hydration, 2011. Available at: http:// tiative into nutrition practice. Nutr Clin Pract. 2014;29(3):406-408.
www.nursingworld.org/MainMenuCategories/Policy-Advocacy/ 61. Schwartz DB, DiTucci A, Goldman B, Gramigna GD, Cummings B.
Positions-and-Resolutions/ANAPositionStatements/Position-Statements- Achieving patient-centered care in a case of a patient with advanced
Alphabetically/prtetnutr14451.pdf. Accessed January 27, 2014. dementia. Nutr Clin Pract. 2014;29(4):556-558.
Downloaded from ncp.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on January 6, 2015
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Textbook of Gynaecological OncologyDocument58 pagesTextbook of Gynaecological OncologyMarco Vinicio Benavides Osorto100% (2)
- Anatomy and Physiology - Dengue FeverDocument3 pagesAnatomy and Physiology - Dengue Feverhael yam62% (13)
- Pathophysiology of InflammationDocument50 pagesPathophysiology of InflammationElla Jones0% (1)
- Festival Dance Lesson - Module 2 - P.E. 3rd Quarter PPT 2 of 2Document29 pagesFestival Dance Lesson - Module 2 - P.E. 3rd Quarter PPT 2 of 2Maria Fe VibarNo ratings yet
- DKA Handout1Document59 pagesDKA Handout1aleNo ratings yet
- Campylobacter Jejuni-Mediated Guillain-Barre Syndrome, An Overview of The Molecular Mimicry and Vaccine Development ApproachesDocument9 pagesCampylobacter Jejuni-Mediated Guillain-Barre Syndrome, An Overview of The Molecular Mimicry and Vaccine Development ApproachesInternational Medical Publisher0% (1)
- CH 14 Antepartum Nursing Assessment NotesDocument8 pagesCH 14 Antepartum Nursing Assessment NotesMary LowryNo ratings yet
- Cholera (5 5)Document1 pageCholera (5 5)Celestial, Maybelle MarieNo ratings yet
- Medical Biotechnology Multiple Choice Question (GuruKpo)Document13 pagesMedical Biotechnology Multiple Choice Question (GuruKpo)GuruKPO91% (11)
- Specific Proteins Calibrator-150721009-BS600Document2 pagesSpecific Proteins Calibrator-150721009-BS600S6b2No ratings yet
- Gujarat Technological University: W.E.F. AY 2017-18Document3 pagesGujarat Technological University: W.E.F. AY 2017-18raj royelNo ratings yet
- Defense Medical Epidemiology Database Report - Jan 26, 2022Document41 pagesDefense Medical Epidemiology Database Report - Jan 26, 2022adan_infowars100% (2)
- Anesthesia-Assessing Depth PDFDocument1 pageAnesthesia-Assessing Depth PDFAvinash Technical ServiceNo ratings yet
- E341 FullDocument7 pagesE341 FullwaribisalaNo ratings yet
- Seminar: Pere Ginès, Aleksander Krag, Juan G Abraldes, Elsa Solà, Núria Fabrellas, Patrick S KamathDocument18 pagesSeminar: Pere Ginès, Aleksander Krag, Juan G Abraldes, Elsa Solà, Núria Fabrellas, Patrick S KamathcastillojessNo ratings yet
- Case Study 5 Dengue Fever CorrectedDocument13 pagesCase Study 5 Dengue Fever CorrectedyounggirldavidNo ratings yet
- Ok - Effect of Melatonin On Broiler ChicksDocument12 pagesOk - Effect of Melatonin On Broiler ChicksOliver TalipNo ratings yet
- Beth PRC FormDocument11 pagesBeth PRC FormNev Bryan DapitanNo ratings yet
- LESSON 3: Exercise Variables and PrinciplesDocument31 pagesLESSON 3: Exercise Variables and PrinciplesCapulong Kimberly100% (1)
- PediatricsDocument312 pagesPediatricsمحمد ابو مناضل الافينش100% (1)
- Basic Surgical Skills FinalDocument62 pagesBasic Surgical Skills Finalamel015No ratings yet
- Physics and Imaging in Radiation OncologyDocument6 pagesPhysics and Imaging in Radiation Oncologydarr artNo ratings yet
- Unstable Angina - Cardiovascular Disorders - MSD Manual Professional EditionDocument1 pageUnstable Angina - Cardiovascular Disorders - MSD Manual Professional EditionboynextdoorpkyNo ratings yet
- Full Download Winninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions ManualDocument28 pagesFull Download Winninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions Manualnoahmya6100% (25)
- P1 RleDocument34 pagesP1 RleMary Jean GicaNo ratings yet
- McGrath Video Laryngoscope Rev 0.1Document6 pagesMcGrath Video Laryngoscope Rev 0.1adevasenNo ratings yet
- Communicable DiseasesDocument24 pagesCommunicable DiseasesJanus de LeonNo ratings yet
- Surgical Management of Gastroesophageal Reflux in Adults - UpToDateDocument22 pagesSurgical Management of Gastroesophageal Reflux in Adults - UpToDateJuan InsignaresNo ratings yet
- Acid Fast StainDocument3 pagesAcid Fast StainMartina MicicNo ratings yet