Professional Documents
Culture Documents
Von Stein 2019
Uploaded by
Meylindha Ekawati Biono PutriCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Von Stein 2019
Uploaded by
Meylindha Ekawati Biono PutriCopyright:
Available Formats
I nnovative Approaches
E FFECT OF A SCHEDULED
NURSE INTERVENTION ON
THIRST AND DRY MOUTH IN
INTENSIVE CARE PATIENTS
By Michelle VonStein, BSN, RN, CCRN, Barbara L. Buchko, DNP, RN, Cristina
Millen, BSN, RN, PCCN, Deborah Lampo, DNP, RN, NE-BC, Theodore Bell, MS,
and Anne B. Woods, PhD, MPH, RN
Background Thirst is a common, intense symptom
reported by hospitalized patients. No studies indicate
frequency of use of ice water and lip moisturizer with
menthol to ameliorate thirst and dry mouth. In an audit
of 30 intensive care unit patients at a 580-bed commu-
nity teaching hospital, 66% reported dry mouth with
higher thirst distress and intensity scores than in pub-
lished studies.
Objectives To evaluate the effectiveness of scheduled
use of ice water oral swabs and lip moisturizer with
menthol compared with unscheduled use in relieving
thirst and dry mouth for intensive care unit patients.
Methods In a quasi-experimental design, adult patients
admitted to 2 intensive care units at a community hos-
pital were provided with ice water oral swabs and lip
moisturizer with menthol upon request. The intervention
was unscheduled in 1 unit and scheduled in the other
unit. The scheduled intervention was provided hourly
during a 7-hour period (n = 62 participants). The unsched-
uled intervention consisted of usual care (n = 41 partici-
pants). A numeric rating scale (0-10) was used to measure
thirst intensity, thirst distress, and dry mouth before and
after 7 hours in both groups.
Results The scheduled-use group had significant lessen-
ing of thirst intensity (P = .02) and dry mouth (P = .008).
Thirst distress in the scheduled-use group did not differ
This article is followed by an AJCC Patient Care Page from that in the unscheduled-use group (P = .07).
on page 47. Conclusion Scheduled use of ice water oral swabs and
lip moisturizer with menthol may lessen thirst intensity
and dry mouth in critical care patients. (American Journal
©2019 American Association of Critical-Care Nurses
of Critical Care. 2019;28:41-46)
doi:https://doi.org/10.4037/ajcc2019400
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, January 2019, Volume 28, No. 1 41
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 8, 2019
T
hirst can be defined as “a perception that provokes the urge to drink fluids”1 and “is
a prevalent, intense, distressing, and underappreciated symptom in intensive care
patients.”2 Dry mouth, or xerostomia, can be associated with thirst.1 Thirst and dry
mouth are common symptoms and may affect patients’ experience in intensive care
unit (ICUs).3 In a study of 171 ICU patients by Puntillo et al,4 thirst was one of the
most common and intense symptoms reported.
A more recent retrospective, descriptive study5 was tested in a randomized control study in 252 ICU
of patients who had cardiac surgery and received patients.1 Overall, use of the bundle resulted in a
mechanical ventilation confirmed that dry mouth statistically significant decrease in thirst intensity,
and thirst cause discomfort. The researchers5 sug- thirst distress, and dry mouth. These findings are
gested that these symptoms could be addressed by strengthened by the randomized control design of
nursing staff, but studies were needed to identify the study and assessment of potential confounders.
interventions. In a phenomenological study, Kjeld- In a quality improvement audit, we assessed for
sen et al6 found that patients treated with mechani- thirst distress, thirst intensity, and dry mouth in 30
cal ventilation experienced powerlessness and patients who were not receiving mechanical ventila-
frustration because of the inability to satisfy thirst. tion and whose status was nothing by mouth. Mean
Patients in ICUs are predisposed to thirst and scores for thirst distress and thirst intensity were 5.5
dry mouth for a variety of reasons, including mechan- and 6.1 (on a numeric rating scale [NRS] of 1-10),
ical ventilation, receiving nothing by mouth, specific respectively. Dry mouth was reported by 66% of
classes of medication, and certain medical conditions.7 patients. Usual care consisting of oral swabs moist-
Little research has been done ened with ice water and lip moisturizer containing
on nonpharmacological methyl lactate (a derivative of menthol) are provided
Patients receiving interventions to manage to patients upon request at this facility. More than
mechanical ventilation and minimize thirst and half of the patients reported using these interven-
dry mouth in hospitalized tions to relieve thirst and dry mouth.
experience powerless- adults, especially ICU Our aim in this study was to compare the effec-
patients, resulting in a lack tiveness of scheduled use of ice water oral swabs and
ness and frustration of solid evidence for prac- lip moisturizer with menthol with the effectiveness
because of the inability tice. Cold water was the of unscheduled, as-needed use of the same interven-
most common approach, tions (usual care) at relieving thirst intensity, thirst
to satisfy thirst. with a variety of application distress, and dry mouth in ICU patients. We hypoth-
techniques.1,3,8,9 Menthol esized that providing patients with regularly scheduled
was also cited as an intervention for its cooling sen- applications of ice water oral swabs and lip moistur-
sation.10 Puntillo et al1 used a menthol lip moistur- izer with menthol would decrease the patients’ per-
izer as part of an intervention bundle to prevent thirst ception of thirst intensity, thirst distress, and dry
and dry mouth. No evidence-based recommendations mouth more than would providing these interven-
for a standardized frequency of use were reported. tions upon patients’ request.
A thirst intervention bundle consisting of ice water
spray, oral swab wipes, and menthol lip moisturizer Methods
Design, Setting, and Sample
About the Authors We used a quasi-experimental study design with
Michelle VonStein and Cristina Millen are clinical nurses, a convenience sample of patients admitted to 2 medi-
and Deborah Lampo is a nurse manager, WellSpan York cal ICUs at WellSpan York Hospital, York, Pennsyl-
Hospital, York, Pennsylvania. Barbara L. Buchko is direc-
tor, Evidence-Based Practice and Nursing Research, and vania, a 580-bed acute care community teaching
Theodore Bell is a research program manager, WellSpan hospital. One unit provided the scheduled-use inter-
Health, York, Pennsylvania. Anne B. Woods is adjunct vention and the other unit provided usual care to
faculty, Messiah College, Mechanicsburg, Pennsylvania.
patients as needed. Both units provide care for ICU
Corresponding author: Barbara Buchko, Director of patients with a variety of medical diagnoses. The
Evidence-Based Practice and Nursing Research, Well-
Span Health, 1001 S George St, York, PA 17405 (email: study was approved by the appropriate institutional
bbuchko@wellspan.org). review board.
42 AJCC AMERICAN JOURNAL OF CRITICAL CARE, January 2019, Volume 28, No. 1 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 8, 2019
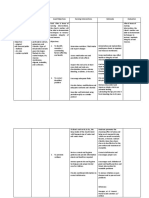
Assessed for eligibility
(n = 296) Excluded (n = 162)
Enrollment
Patients were eligible if they were more than 18 Not meeting inclusion
years old, spoke English, were able to provide informed criteria (n = 77)
consent, had an ICU stay of 12 hours or more, had Nonrandom assignment Declined participation
a score of -1, 0, or +1 on the Richmond Agitation- by unit (n = 85)
Sedation Scale, and had a baseline thirst intensity or (n = 134)
thirst distress score of 3 or greater (on a 0-10 NRS).
Allocation
The exclusion criteria mirrored those of the study of
Puntillo et al1: a history of dementia; open lesions Intervention unit Usual care unit
or desquamation on the mouth or lips; or a medical (n = 79) (n = 55)
condition, such as recent oral surgery, that contrain-
dicated the intervention. We did an a priori power
Follow-up
analysis for a paired t test with an _ of .05, a power Lost to follow-up Lost to follow-up
of 0.80, and an effect size of 0.35 (small-moderate). (n = 17) (n = 14)
The results indicated that 66 patients would be needed
for each group.
Analysis
A total of 296 patients were evaluated for eligi- Analyzed (n = 62) Analyzed (n = 41)
bility from February through September 2017. Of
these patients, 219 met eligibility criteria, and 134
(61%) were enrolled in the study. The Figure is a
Figure Flowchart of participants enrolled in the study.
flowchart of enrollment in the study. A total of 31
participants were lost to follow-up because of trans-
fer from the unit before completion of data collec- menthol. A reminder card was placed at each par-
tion. The 2 groups did not differ significantly (r21 = 0.3; ticipant’s bedside to ensure completion of sched-
P = .59) in the number who were lost to attrition: uled treatments. Clinical staff in the intervention
22% in the intervention group (n = 17) and 26% in unit were provided education about the interven-
the control group (n = 14). The final sample consisted tion and its frequency for participants.
of 103 patients who completed the study: 62 in the Control (Usual Care). Providing ice water oral
intervention group and 41 in the control group. swabs and lip moisturizer with menthol when
Participants who completed the study (n = 103) requested by a patient was the usual care. Study
and those who were lost because of attrition (n = 31) participants within the ICU that provided usual
did not differ significantly in age; sex; ventilator sta- care were notified that they could ask the clinical
tus; or scores for thirst intensity, thirst distress, and staff for ice water oral swabs
dry mouth obtained before the start of the study. and lip moisturizer with men-
thol when needed. The charge
The intervention
Procedures nurse and each participant’s group received hourly
Five research nurses were trained to enroll patients primary nurse in the usual-care
and collect data. These nurses used a researcher- ICU were notified that the par- ice water oral swabs
developed data collection tool to ensure precision ticipant was enrolled in a study. and lip moisturizer
in collection. Potential participants were identified No additional education was
each morning by a research nurse in collaboration provided to the nursing staff with menthol.
with the unit charge nurse. Baseline data were col- because no change in usual care
lected to determine eligibility. Patients who agreed was required. A research nurse returned to the
to participate completed an informed consent form. usual-care unit to evaluate the study participants’
Intervention. The research nurses informed par- thirst intensity, thirst distress, and dry mouth 7 hours
ticipants in the intervention group that clinical staff after enrollment (between 5:30 PM and 6 PM)
members would provide freshly obtained ice water
oral swabs and would apply lip moisturizer with Instruments
menthol every hour with the first application at 10 AM Construct validity of the NRS was established
and the last application at 5 PM. The research nurses through factor analysis.11,12 Concurrent validity was
informed the unit charge nurse and each patient’s evidenced by strong correlations between scores on
primary nurse of the patient’s enrollment in the study. the NRS and scores on a visual analog scale, current
Participants in the intervention group received a pain intensity word scales, and simple descriptive
packet containing 8 swabs and lip moisturizer with scales.11,12 We chose an NRS rather than a visual
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, January 2019, Volume 28, No. 1 43
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 8, 2019
Table 1
Group demographics
Intervention Control groupa
Data Analysis
Characteristic groupa (n = 62) (n = 41) P value
We used IBM SPSS Statistics for Windows, version
Male sex 33 (53) 24 (59) .60 24.0, (IBM Corp) to maintain and analyze data. To
Ventilator status 1 (2) 1 (2) > .99 evaluate differences between the scheduled-use group
10 (16) 6 (15) > .99
and the control group for demographics (sex, venti-
Nothing by mouth status
lator status, and nothing by mouth status), we used
Age, mean (SD), y 60.3 (17.1) 62.8 (11.3) .41
the Pearson r2 test or the Fisher exact test as appropri-
a
Values are No. (%) of patients unless otherwise indicated in first column.
ate. Differences in age between the 2 groups were eval-
uated by using an independent samples t test. The
outcome variables (number of ice water swabs used
Table 2 and number of times lip moisturizer with menthol
Paired samples results for intervention was used), along with scores for thirst intensity, thirst
and control groupsa distress, and dry mouth, were examined to assess
Score, mean (SD)
assumptions for parametric testing. These data violated
Group Outcomes Before After Z P valueb
the assumptions of normality (kurtosis ≥ 1.0; Shapiro
Wilk test < .05), so nonparametric analyses were used.
Intervention Thirst intensity 6.48 (2.45) 3.65 (2.84) -5.10 < .001 The Wilcoxon signed rank test was used to identify dif-
Thirst distress 5.21 (2.95) 2.73 (3.03) -4.57 < .001
ferences in scores before and after the intervention in
Dry mouth 6.63 (2.57) 3.48 (2.84) -5.36 < .001
both the intervention and the control groups. The
Control Thirst intensity 7.10 (2.41) 5.42 (2.87) -3.29 .001 Mann-Whitney test was used to detect significant dif-
Thirst distress 5.83 (3.20) 4.18 (3.40) -2.57 .01
Dry mouth 6.76 (2.95) 5.20 (2.97) -2.66 .008
ferences in the mean use of ice water oral swabs and
lip moisturizer with menthol between the intervention
a
Scores were on a numeric rating scale. and control groups and to detect differences in mean
b
Wilcoxon signed rank test.
difference scores before and after the intervention in
the intervention and control groups for thirst intensity,
Table 3 thirst distress, and dry mouth. Statistical significance
Comparison of mean difference scores for was established as P less than .05.
thirst intensity, thirst distress, and dry moutha
Score Mean Results
Outcomes Group Before After difference P value Sample Characteristics
A total of 103 patients completed the study, 62
Thirst intensity Intervention 6.48 3.65 -2.84 .02
Control 7.10 5.42 -1.68
in the scheduled-use group and 41 in the control
group. The 2 groups did not differ significantly in
Thirst distress Intervention 5.21 2.73 -2.48 .07
sex (P = .60), ventilator status (P > .99), nothing by
Control 5.83 4.18 -1.65
mouth status (P > .99) or age (P = .41; see Table 1).
Dry mouth Intervention 6.63 3.48 -3.15 .008
Control 6.76 5.20 -1.56
Findings
a
Mann-Whitney test. In the total sample, thirst intensity, thirst dis-
tress, and dry mouth were reported as substantial
analog scale (as used by Puntillo et al1) because symptoms, with mean NRS scores of 6.73 (SD, 2.4),
patients are familiar with the 0 to 10 NRS. Measures 5.46 (SD, 3.1), and 6.68 (SD, 2.7), respectively. Mean
for thirst intensity and thirst distress mirrored those use of ice water oral swabs and lip moisturizer with
used by Puntillo et al.1 Thirst intensity was scored menthol was significantly greater in the intervention
as 0 (no thirst) to 10 (worst possible thirst); thirst group than in the control group: oral swabs, 5.4 vs
distress as 0 (no distress) to 10 (worst possible dis- 1.7 (P < .001); lip moisturizer with menthol, 4.4 vs
tress); and dry mouth as 0 (no dryness) to 10 (worst 0.5 (P < .001). The 2 groups did not differ significantly
possible dryness). Participants who were unable to in the mean preintervention scores obtained within
communicate verbally because of endotracheal intu- 1 hour of the time the study began for thirst inten-
bation were shown a paper copy of the NRS and asked sity (P = .22), thirst distress (P = .22), or dry mouth
to point to the number that corresponded to their (P = .68). Although both the intervention and the
thirst intensity, thirst distress, and dry mouth or to control group had significant decreases in all 3 out-
nod affirmatively when the research nurse pointed comes (Table 2), the magnitude of the differences
to the numbers, as done in an earlier study.1 was greatest in the intervention group (Table 3), with
44 AJCC AMERICAN JOURNAL OF CRITICAL CARE, January 2019, Volume 28, No. 1 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 8, 2019
significant statistical differences for thirst intensity in clarifying thirst distress to participants, a situation
(-2.84 vs -1.68, U = 941.5, Z = -2.24, P = .02) and dry that may have affected the participants’ rating of
mouth (-3.15 vs -1.56, U = 877.5, Z = -2.66, P = .008). thirst distress. In addition, possible underlying dif-
These findings were also clinically significant, with ferences between the 2 units could have inadvertently
medium-effect sizes for thirst intensity (Cohen d = 0.4) confounded the findings. Randomization to groups
and dry mouth (Cohen d = 0.5). was not done; clear separa-
Discussion
tion of the intervention group
and the control group ensured
Thirst intensity, thirst
Thirst and dry mouth are substantial symptoms intervention fidelity. Also, distress, and dry mouth
experienced by patients in ICUs. Our preinterven- some study participants might
tion mean scores for thirst intensity, thirst distress, have received cold water swabs
were reported as
and dry mouth are similar to those reported by Wang rather than ice water swabs; substantial symptoms.
et al,5 who used a visual analog scale to measure we did not require measure-
thirst and dry mouth associated with discomfort in ment of water temperature to confirm use of ice
patients receiving mechanical ventilation. The mean water. Our study was limited to 2 ICUs in a single
value for thirst and dry mouth in their multiple hospital; therefore, our findings cannot be general-
regression analysis was 5.789 (P = .04), indicating ized to other types of acute inpatient units. Our
that these 2 symptoms were significant predictors of study sample had few patients receiving mechanical
discomfort in patients treated with mechanical ven- ventilation. Puntillo et al1 also had few patients
tilation. Wang et al5 recognized thirst and dry receiving mechanical ventilation and suggested
mouth as a problem and recommended further that interventions for thirst intensity, thirst distress,
research for interventions. and dry mouth may be beneficial to these patients.
Puntillo et al1 investigated interventions. Of note, Therefore, additional research is needed to generalize
Puntillo et al1 measured thirst intensity and thirst our interventions for other populations of patients.
distress by using a 0 to 10 NRS as we did but measured
dry mouth by using a dichotomous (yes-no) mea- Conclusions
sure, whereas we used an NRS. Our preintervention Thirst and dry mouth are the result of illness,
findings for thirst intensity and thirst distress scores medications, and other interventions that patients
were higher than those of Puntillo et al1; however, receive in ICUs. These symptoms are uncomfortable
both their study and ours indicated improvement and distressing, but they are not routinely assessed
in each group. Puntillo et al1 found significant or treated. Thirst must compete with a cadre of other
improvement with use of interventions in thirst symptoms that have greater potential to adversely
intensity, thirst distress, and dry mouth, whereas affect patient outcomes. Our findings confirm that
we found significant improvement in thirst inten- thirst intensity, thirst distress, and dry mouth are
sity and dry mouth only. This difference may be common distressing symptoms among patients in
due to participants’ difficulty in understanding the ICUs. Nurses play a pivotal role in the assessment
concept of thirst distress. Data collectors in our and identification of these symptoms. Compared
study reported the need to explain and use various with as-needed interventions, implementation of a
terms for clarification. simple, scheduled protocol
A strength of our study is that the clinical staff to reduce these symptoms
who provided the intervention could readily incor- can increase patient com-
Implementing a simple
porate these practices with hourly rounding, a situa- fort. Scheduled, hourly scheduled protocol to
tion that supports the feasibility of implementing applications of ice cold
these interventions in the clinical setting. Our study water oral swabs and lip reduce symptoms of
has limitations. Because of challenges with staffing
and patient enrollment, the sample did not meet
moisturizer with menthol
are simple interventions
thirst and dry mouth can
the recommended size of 66 for each group as that can easily be incorpo- increase patient comfort.
determined by the a priori power analysis. Although rated with other hourly
power was sufficient to detect a significant difference rounding interventions. These interventions can be
for thirst intensity and dry mouth in both the inter- used to engage patients and patients’ families to
vention and control groups, the lack of statistical participate more actively in the plan of care. Further
significance for thirst distress may be due to a type research with larger sample sizes is needed to gener-
II error related to insufficient power. Variations occurred alize our findings to other populations of patients.
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, January 2019, Volume 28, No. 1 45
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 8, 2019
ACKNOWLEDGMENTS 6. Kjeldsen C, Hansen M, Jensen K, Holm A, Haahr A, Dreyer
This research was performed at WellSpan York Hospital. P. Patients’ experience of thirst while being conscious and
mechanically ventilated in the intensive care unit. Nurs Crit
Care. 2018;23(2):75-81.
FINANCIAL DISCLOSURES
7. Arai S, Stotts N, Puntillo K. Thirst in critically ill patients:
Funding for this study was provided through a grant from from physiology to sensation. Am J Crit Care. 2013;22(4):
the George L. Laverty Foundation. 328-335.
8. Brunstrom J. Effects of mouth dryness on drinking behav-
REFERENCES ior and beverage acceptability. Physiol Behav. 2002;76(3):
1. Puntillo K, Arai S, Cooper B, Stotts N, Nelson J. A randomized 423-429.
clinical trial of an intervention to relieve thirst and dry 9. Brunstrom J, Macrae A. Effects of temperature and volume
mouth in intensive care unit patients. Intensive Care Med. on measures of mouth dryness, thirst, and stomach full-
2014;40(9):1295-1302. ness in males and females. Appetite. 1997;29(1):31-42.
2. Stotts N, Arai S, Cooper B, Nelson J, Puntillo K. Predictors 10. Eccles R. Role of cold receptors and menthol in thirst, the
of thirst in intensive care unit patients. J Pain Symptom drive to breathe and arousal. Appetite. 2000;34(1):29-35.
Manage. 2015;49(3):530-508. 11. Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA,
3. Puntillo K, Nelson J, Weissman D, et al; Advisory Board of Anderson JA. Studies with pain rating scales. Ann Rheum
the Improving Palliative Care in the ICU (IPAL-ICU) Project. Dis. 1978;37(4):378-381.
Palliative care in the ICU: relief of pain, dyspnea, and thirst— 12. Jensen MP, Karoly P, Braver S. The measurement of clinical
a report from the IPAL-ICU Advisory Board. Intensive Care pain intensity: a comparison of six methods. Pain. 1986;
Med. 2014;40(2):235-248. 27(1):117-126.
4. Puntillo LA, Arai S, Cohen NH, et al. Symptoms experi-
enced by intensive care unit patients at high risk of dying.
Crit Care Med. 2010;38(11):2155-2160.
5. Wang Y, Li H, Zou H, Li Y. Analysis of complaints from To purchase electronic or print reprints, contact American
patients during mechanical ventilation after cardiac sur- Association of Critical-Care Nurses, 101 Columbia, Aliso
gery: a retrospective study. J Cardiothorac Vasc Anesth. Viejo, CA 92656. Phone, (800) 899-1712 or (949) 362-2050
2015;29(4):990-994. (ext 532); fax, (949) 362-2049; email, reprints@aacn.org.
46 AJCC AMERICAN JOURNAL OF CRITICAL CARE, January 2019, Volume 28, No. 1 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 8, 2019
Effect of a Scheduled Nurse Intervention on Thirst and Dry Mouth in Intensive Care
Patients
Michelle VonStein, Barbara L. Buchko, Cristina Millen, Deborah Lampo, Theodore Bell and Anne B.
Woods
Am J Crit Care 2019;28 41-46 10.4037/ajcc2019400
©2019 American Association of Critical-Care Nurses
Published online http://ajcc.aacnjournals.org/
Personal use only. For copyright permission information:
http://ajcc.aacnjournals.org/cgi/external_ref?link_type=PERMISSIONDIRECT
Subscription Information
http://ajcc.aacnjournals.org/subscriptions/
Information for authors
http://ajcc.aacnjournals.org/misc/ifora.xhtml
Submit a manuscript
http://www.editorialmanager.com/ajcc
Email alerts
http://ajcc.aacnjournals.org/subscriptions/etoc.xhtml
The American Journal of Critical Care is an official peer-reviewed journal of the American Association of Critical-Care Nurses
(AACN) published bimonthly by AACN, 101 Columbia, Aliso Viejo, CA 92656. Telephone: (800) 899-1712, (949) 362-2050, ext.
532. Fax: (949) 362-2049. Copyright ©2016 by AACN. All rights reserved.
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 8, 2019
You might also like
- Textbook of Oral Medicine Oral Diagnosis and Oral RadiologyDocument924 pagesTextbook of Oral Medicine Oral Diagnosis and Oral RadiologyAnonymous Bt6favSF4Y90% (67)
- NCP Impaired Oral Mucous MembraneDocument2 pagesNCP Impaired Oral Mucous Membraneklemtot83% (6)
- Oral Manifestation of Systemic DiseaseDocument137 pagesOral Manifestation of Systemic DiseaseJeff Burgess100% (3)
- MFDS Questions ImpDocument8 pagesMFDS Questions ImpalkaNo ratings yet
- HH 2Document6 pagesHH 2LestiNo ratings yet
- Management of Dry Mouth Symptoms After Polysaccharide RinseDocument8 pagesManagement of Dry Mouth Symptoms After Polysaccharide Rinseotoralla1591No ratings yet
- MagicMouthwash For OralMucositis Sol Stanford PDFDocument2 pagesMagicMouthwash For OralMucositis Sol Stanford PDFManuel ArenasNo ratings yet
- Oral Care Reduces Pneumonia in Older Patients in Nursing HomesDocument4 pagesOral Care Reduces Pneumonia in Older Patients in Nursing HomesYasir MahfudNo ratings yet
- Original Article: Dental Research, Dental Clinics, Dental ProspectsDocument8 pagesOriginal Article: Dental Research, Dental Clinics, Dental Prospectsmadhu kakanurNo ratings yet
- Weissman 2011Document5 pagesWeissman 2011gulararezendeNo ratings yet
- Comparing Nasal Irrigation Devices for Pediatric SinusitisDocument6 pagesComparing Nasal Irrigation Devices for Pediatric SinusitisrivanaNo ratings yet
- PneumoniaDocument8 pagesPneumoniaSoffie FitriyahNo ratings yet
- Doxycycline: An Option in The Treatment of Ulcerated Oral Lesions?Document6 pagesDoxycycline: An Option in The Treatment of Ulcerated Oral Lesions?nnNo ratings yet
- Chitsuthipakorn 2021Document12 pagesChitsuthipakorn 2021Diko KoestantyoNo ratings yet
- Oxitard Capsules Improve Oral Submucous Fibrosis SymptomsDocument5 pagesOxitard Capsules Improve Oral Submucous Fibrosis SymptomssevattapillaiNo ratings yet
- Management of Endodontic Emergencies: Chapter OutlineDocument9 pagesManagement of Endodontic Emergencies: Chapter OutlineNur IbrahimNo ratings yet
- Kjped 57 479Document5 pagesKjped 57 479Vincent LivandyNo ratings yet
- 1 s2.0 S009923991500182X MainDocument6 pages1 s2.0 S009923991500182X MainDaniella NúñezNo ratings yet
- Effects of A Standard Versus Comprehensive Oral Care Protocol Among Intubated Neuroscience ICU Patients: Results of A Randomized Controlled TrialDocument13 pagesEffects of A Standard Versus Comprehensive Oral Care Protocol Among Intubated Neuroscience ICU Patients: Results of A Randomized Controlled TrialMohammed Falih HassanNo ratings yet
- Oral Care May Reduce Pneumonia Risk in Tube-Fed ElderlyDocument6 pagesOral Care May Reduce Pneumonia Risk in Tube-Fed ElderlyIvan Ramos GutarraNo ratings yet
- Anesthetic Efficacy of Buccal Infiltration Articaine Versus Lidocaine For Extraction of Primary Molar TeethDocument5 pagesAnesthetic Efficacy of Buccal Infiltration Articaine Versus Lidocaine For Extraction of Primary Molar TeethFabro BianNo ratings yet
- 2887 10028 1 PBDocument5 pages2887 10028 1 PBniratig691No ratings yet
- Clinically Proven Herbal Toothpaste in Sri LankaDocument7 pagesClinically Proven Herbal Toothpaste in Sri LankaYoga ChanNo ratings yet
- Tes MenelanDocument9 pagesTes MenelanAnonymous q1NLY8RNo ratings yet
- FinalprintedarticleDocument9 pagesFinalprintedarticleNia DefinisiNo ratings yet
- Xylitol Nasal Irrigation in The Management of ChronicDocument6 pagesXylitol Nasal Irrigation in The Management of ChronicFlor OMNo ratings yet
- One Stage Full-Mouth Disinfection Improves Periodontitis OutcomesDocument14 pagesOne Stage Full-Mouth Disinfection Improves Periodontitis OutcomesAnita PrastiwiNo ratings yet
- Irrigacion Iodo Vs Agua OxigenadaDocument5 pagesIrrigacion Iodo Vs Agua OxigenadaAlanis BuenrostroNo ratings yet
- Effects of Parentereal Hydration in Terminally Ill Cancer Patients A Preleminary StudyDocument6 pagesEffects of Parentereal Hydration in Terminally Ill Cancer Patients A Preleminary StudyCristian Meza ValladaresNo ratings yet
- A Double-Blind Randomized Controlled Trial of Normal Saline, Lactated Ringer's, and Hypertonic Saline Nasal Irrigation Solution After Endoscopic Sinus SurgeryDocument7 pagesA Double-Blind Randomized Controlled Trial of Normal Saline, Lactated Ringer's, and Hypertonic Saline Nasal Irrigation Solution After Endoscopic Sinus SurgeryYasdika ImamNo ratings yet
- Sample of Journal & Critique PresenationDocument42 pagesSample of Journal & Critique PresenationMonika shankarNo ratings yet
- Joph2019 5491626Document5 pagesJoph2019 5491626rizki agusmaiNo ratings yet
- tratamiento con AINESDocument6 pagestratamiento con AINESCarol Chávez MedinaNo ratings yet
- Anesthesia Onset Time and Injection Pain Between Buffered and Unbuffered Lidocaine Used As Local Anesthetic For Dental Care in ChildrenDocument4 pagesAnesthesia Onset Time and Injection Pain Between Buffered and Unbuffered Lidocaine Used As Local Anesthetic For Dental Care in ChildrenFernando MenesesNo ratings yet
- Clinical Efficacy of Local Delivered Minocycline in The Treatment of Chronic Periodontitis Smoker PatientsDocument5 pagesClinical Efficacy of Local Delivered Minocycline in The Treatment of Chronic Periodontitis Smoker PatientsvivigaitanNo ratings yet
- Tap Water Versus Sterile Normal Saline in Wound Swabbing: A Double-Blind Randomized Controlled TrialDocument8 pagesTap Water Versus Sterile Normal Saline in Wound Swabbing: A Double-Blind Randomized Controlled TrialAnonymous RxjOeoYn9No ratings yet
- Univer Complu Madrid NBF Peri - Implant MucositisDocument10 pagesUniver Complu Madrid NBF Peri - Implant Mucositisjuan perezNo ratings yet
- Referensi 5Document5 pagesReferensi 5RizkaGayoNo ratings yet
- The Effects of Povidone Iodine (PH 4.2) On Patients With Adenoviral ConjunctivitisDocument3 pagesThe Effects of Povidone Iodine (PH 4.2) On Patients With Adenoviral ConjunctivitisShari' Si WahyuNo ratings yet
- Hamre - 2012 - Pulpa Dentis D30 For Acute Reversible Pulpitis A Prospective Cohort Study in Routine Dental PracticeDocument7 pagesHamre - 2012 - Pulpa Dentis D30 For Acute Reversible Pulpitis A Prospective Cohort Study in Routine Dental PracticeMaría Reynel TarazonaNo ratings yet
- Determination of Salivary Levels of Mucin and Amylase in Chronic Periodontitis PacientsDocument7 pagesDetermination of Salivary Levels of Mucin and Amylase in Chronic Periodontitis PacientsOctavian BoaruNo ratings yet
- Avaliacao Quantitativa FuncaooralDocument6 pagesAvaliacao Quantitativa FuncaooralAMELIA PAZ LETELIER AGUIRRENo ratings yet
- Topical Application of Local Anaesthetic Gel VS IcDocument7 pagesTopical Application of Local Anaesthetic Gel VS IcNhấtNo ratings yet
- Effectiveness of buffered and non-buffered local anaesthetic in inferior alveolar nerve block: a randomised studyDocument5 pagesEffectiveness of buffered and non-buffered local anaesthetic in inferior alveolar nerve block: a randomised studykaluaxeniaNo ratings yet
- Oral Care in Ventilation MechanicDocument8 pagesOral Care in Ventilation MechanicRusida LiyaniNo ratings yet
- Çocuklarda Sıvı Tedavisi Ile Pobk Arasındaki IlişkiDocument6 pagesÇocuklarda Sıvı Tedavisi Ile Pobk Arasındaki IlişkiAli ÖzdemirNo ratings yet
- Daily Interruption of Sedation in Patients Receiving Mechanical VentilationDocument10 pagesDaily Interruption of Sedation in Patients Receiving Mechanical VentilationJim LinNo ratings yet
- Management of Dentinehypersensitivity Ef Cacy Ofprofessionally Andself-Administered AgentsDocument47 pagesManagement of Dentinehypersensitivity Ef Cacy Ofprofessionally Andself-Administered AgentsNaoki MezarinaNo ratings yet
- Nursing Care Plan for Oral Mucosa InjuryDocument4 pagesNursing Care Plan for Oral Mucosa InjurySweetie PieNo ratings yet
- Could Patient Controlled Thirst Driven Fluid Administration 2018 British JouDocument7 pagesCould Patient Controlled Thirst Driven Fluid Administration 2018 British JouSeveNNo ratings yet
- Uri 2011Document5 pagesUri 2011anton.neonatusNo ratings yet
- Evaluation of The Efficacy of Dentin Hypersensitivity Treatments-A Systematic Review and Follow Up AnalysisDocument39 pagesEvaluation of The Efficacy of Dentin Hypersensitivity Treatments-A Systematic Review and Follow Up AnalysisNaoki MezarinaNo ratings yet
- Evidencia 2Document3 pagesEvidencia 2Alex MolinaNo ratings yet
- Hyaluronic Acid As An Adjunct After Scaling and Root Planing A Prospective Randomized Clinical TrialDocument9 pagesHyaluronic Acid As An Adjunct After Scaling and Root Planing A Prospective Randomized Clinical TrialAdriana Segura DomínguezNo ratings yet
- Journal of Population Therapeutics & Clinical PharmacologyDocument7 pagesJournal of Population Therapeutics & Clinical PharmacologyEka SetyariniNo ratings yet
- A Comparative Study of Effectiveness Between Topical Insulin Versus Normal Saline Dressings in Management of Diabetic Foot UlcersDocument13 pagesA Comparative Study of Effectiveness Between Topical Insulin Versus Normal Saline Dressings in Management of Diabetic Foot UlcersIJAR JOURNALNo ratings yet
- Efficacy of 25% Glucose in Glycerin and Honey in The Management of Primary Atrophic Rhinitis: A Comparative Prospective StudyDocument4 pagesEfficacy of 25% Glucose in Glycerin and Honey in The Management of Primary Atrophic Rhinitis: A Comparative Prospective StudySathiyamoorthy KarunakaranNo ratings yet
- Parirokh 2016Document7 pagesParirokh 2016Fernando MenesesNo ratings yet
- Role of PH of External Auditory Canal in Acute Otitis ExternaDocument6 pagesRole of PH of External Auditory Canal in Acute Otitis ExternaAayush MittalNo ratings yet
- Efficacy-of-a-Moisturizer-for-Pruritus-AccompaniedDocument9 pagesEfficacy-of-a-Moisturizer-for-Pruritus-Accompaniedachi olivNo ratings yet
- General Anaesthesia in The Dental Management of A Child With Cerebral Palsy and Autism: A Case ReportDocument4 pagesGeneral Anaesthesia in The Dental Management of A Child With Cerebral Palsy and Autism: A Case Reportulum777No ratings yet
- Pone 0145837Document16 pagesPone 0145837Raluca ChisciucNo ratings yet
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- Reliabilityand Validityof Research InstrumentsDocument9 pagesReliabilityand Validityof Research InstrumentsMeylindha Ekawati Biono PutriNo ratings yet
- Analisis Ulangan Umum Semester II Tahun 2014 - 2015Document36 pagesAnalisis Ulangan Umum Semester II Tahun 2014 - 2015Meylindha Ekawati Biono PutriNo ratings yet
- Kawati Biono Putri., S.KepDocument1 pageKawati Biono Putri., S.KepMeylindha Ekawati Biono PutriNo ratings yet
- Reliabilityand Validityof Research InstrumentsDocument9 pagesReliabilityand Validityof Research InstrumentsMeylindha Ekawati Biono PutriNo ratings yet
- Slow Deep Breathing and Lavender Aromatherapy for Post-Caesarean Section PainDocument8 pagesSlow Deep Breathing and Lavender Aromatherapy for Post-Caesarean Section PaineviNo ratings yet
- Contoh CV ProfesionalDocument2 pagesContoh CV ProfesionalElyani AdityaNo ratings yet
- Clinical Scores For Dyspnoea Severity in Children: A Prospective Validation StudyDocument11 pagesClinical Scores For Dyspnoea Severity in Children: A Prospective Validation StudyMeylindha Ekawati Biono PutriNo ratings yet
- HHS Public Access: PICU Nurses' Pain Assessments and Intervention Choices For Virtual Human and Written VignettesDocument21 pagesHHS Public Access: PICU Nurses' Pain Assessments and Intervention Choices For Virtual Human and Written VignettesMeylindha Ekawati Biono PutriNo ratings yet
- The Effects of Position On Gastric Residual Volume of Premature Infants in NICUDocument6 pagesThe Effects of Position On Gastric Residual Volume of Premature Infants in NICUMeylindha Ekawati Biono PutriNo ratings yet
- Published Sandeep STM JNSPDocument5 pagesPublished Sandeep STM JNSPMeylindha Ekawati Biono PutriNo ratings yet
- Contoh CV ProfesionalDocument1 pageContoh CV ProfesionalMeylindha Ekawati Biono PutriNo ratings yet
- Daftar Pustaka: 9454332/penderita - Stroke.di - Yogyakarta.Meningkat. Dua - Kali.LipatDocument4 pagesDaftar Pustaka: 9454332/penderita - Stroke.di - Yogyakarta.Meningkat. Dua - Kali.LipatMeylindha Ekawati Biono PutriNo ratings yet
- Gynecologic Oncology: Nozomi Donoyama, Toyomi Satoh, Tetsutaro Hamano, Norio Ohkoshi, Mamiko OnukiDocument8 pagesGynecologic Oncology: Nozomi Donoyama, Toyomi Satoh, Tetsutaro Hamano, Norio Ohkoshi, Mamiko OnukiMeylindha Ekawati Biono PutriNo ratings yet
- Archives of Psychiatric Nursing: Funda Kavak, Mine EkinciDocument7 pagesArchives of Psychiatric Nursing: Funda Kavak, Mine EkinciMeylindha Ekawati Biono PutriNo ratings yet
- 197 377 1 SMDocument29 pages197 377 1 SMMeylindha Ekawati Biono PutriNo ratings yet
- WhoDocument1 pageWhoMeylindha Ekawati Biono PutriNo ratings yet
- 2015-03-28 - 10-04-09-Ambm 17Document5 pages2015-03-28 - 10-04-09-Ambm 17Meylindha Ekawati Biono PutriNo ratings yet
- 46 HalpinDocument3 pages46 HalpinMeylindha Ekawati Biono PutriNo ratings yet
- 1 PBDocument7 pages1 PBDelly AwalliaNo ratings yet
- Food ChemistryDocument6 pagesFood ChemistryMeylindha Ekawati Biono PutriNo ratings yet
- Assets Documents Reports Clinical Guidelines in Dentistry For Diabetes 2015Document62 pagesAssets Documents Reports Clinical Guidelines in Dentistry For Diabetes 2015PragatiNo ratings yet
- Case Report: Prosthodontic Management of Xerostomic Patient: A Technical ModificationDocument7 pagesCase Report: Prosthodontic Management of Xerostomic Patient: A Technical ModificationLisa Purnia CahyaniNo ratings yet
- Oral Healthcare For The Elderly in Malaysia PDFDocument58 pagesOral Healthcare For The Elderly in Malaysia PDFEr LindaNo ratings yet
- Nursing Care in RadiotherapyDocument26 pagesNursing Care in Radiotherapyحسام جبار مجيد100% (1)
- GIT Biochem PDFDocument46 pagesGIT Biochem PDFMohammad ShafiqNo ratings yet
- Oral Manifestations of Connective Tissue DiseasesDocument34 pagesOral Manifestations of Connective Tissue DiseasesFatin Nabihah Jamil67% (3)
- Contoh CJRDocument16 pagesContoh CJRmmerry743No ratings yet
- Diabetes Mellitus and Prosthodontic Care Chanchal Katariya & Dr. SangeethaDocument3 pagesDiabetes Mellitus and Prosthodontic Care Chanchal Katariya & Dr. SangeethaArushi AgarwalNo ratings yet
- Saliva's potential as a non-invasive diagnostic toolDocument9 pagesSaliva's potential as a non-invasive diagnostic toolSabiran GibranNo ratings yet
- Ecologia de Lactobacilus en La Cavidad BucalDocument11 pagesEcologia de Lactobacilus en La Cavidad BucalLucy Esther Calvo PerniaNo ratings yet
- Artificial Saliva For Therapeutic Management of Xerostomia: A Structured ReviewDocument5 pagesArtificial Saliva For Therapeutic Management of Xerostomia: A Structured ReviewAlexander KevinNo ratings yet
- Estimation of Salivary GlucoseDocument10 pagesEstimation of Salivary GlucoseSuganya MurugaiahNo ratings yet
- The Correlation Between Occurrence of Dental Caries and Oral Health-Related Quality of Life On Elderly Population in Yogyakarta Special RegionDocument10 pagesThe Correlation Between Occurrence of Dental Caries and Oral Health-Related Quality of Life On Elderly Population in Yogyakarta Special RegionClaypella MaskNo ratings yet
- What Is Dry MouthDocument1 pageWhat Is Dry Mouthالعمري العمريNo ratings yet
- Sjogren Syndrome: Schirmer TestDocument2 pagesSjogren Syndrome: Schirmer TestRiena Austine Leonor NarcillaNo ratings yet
- Oral and dental infections and disordersDocument59 pagesOral and dental infections and disordersHendra PranotogomoNo ratings yet
- BL NurBio Activity 11 - Analysis of Saliva (Revised 07.05.20)Document4 pagesBL NurBio Activity 11 - Analysis of Saliva (Revised 07.05.20)Diana CoralineNo ratings yet
- Sarmiento vs. ECC GR No. 65680, May 11, 1988Document3 pagesSarmiento vs. ECC GR No. 65680, May 11, 1988Winnie Ann Daquil LomosadNo ratings yet
- Pros Tho Don Tic Considerations in Diabetes MellitusDocument16 pagesPros Tho Don Tic Considerations in Diabetes MellitusDrPrachi AgrawalNo ratings yet
- Oral Dysfunction in Patients With Head and Neck.10Document14 pagesOral Dysfunction in Patients With Head and Neck.10Yeni PuspitasariNo ratings yet
- Saliva: DR - Deepshikha Soni Mds 1 YearDocument90 pagesSaliva: DR - Deepshikha Soni Mds 1 Yeardisha 146jandialNo ratings yet
- Connective Tissue DisordersDocument35 pagesConnective Tissue DisordersAHMED KHALIDNo ratings yet
- Japanese Dental Science Review: Yumiko Kawashita, Sakiko Soutome, Masahiro Umeda, Toshiyuki SaitoDocument6 pagesJapanese Dental Science Review: Yumiko Kawashita, Sakiko Soutome, Masahiro Umeda, Toshiyuki SaitoYeni PuspitasariNo ratings yet
- Throat PowerpointDocument29 pagesThroat Powerpointminci sensei100% (8)
- 2 Saliva PhysiologyDocument20 pages2 Saliva PhysiologyvelangniNo ratings yet
- Treatment of Sjögren's Syndrome - Constitutional and Non-Sicca Organ-Based Manifestations - UpToDateDocument31 pagesTreatment of Sjögren's Syndrome - Constitutional and Non-Sicca Organ-Based Manifestations - UpToDateGabriel Fernandez FigueroaNo ratings yet