Professional Documents
Culture Documents
KASUS 1 2nov2010
Uploaded by
ninanurfitri2830Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
KASUS 1 2nov2010
Uploaded by
ninanurfitri2830Copyright:
Available Formats
Melissa Fellman, RDH, BS
Pharmacology and Periodontal Disease:
Implications and Future Options
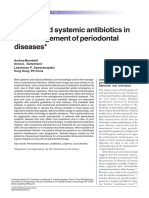
Introduction There are many systemic antibiotics on the market. The most
Periodontal disease is a complex inflammatory disease characterized commonly used include tetracycline, ciprofloxacin, metronidazole and
by bacterial infection, host response and patient behavior. The debride- the penicillins, including amoxicillin and amoxicillin/clavulanate acid
ment of plaque biofilm and adequate home care are essential (Augmentin®). Tetracycline is bacteriostatic, targets both gram
elements of a patient’s periodontal treatment. Antibiotics, antimi- positive and gram negative organisms, and has become bacterial
crobials, herbs, antivirals and vaccines may also be beneficial when resistant. Ciprofloxacin is bactericidal, targets gram negative rods, and
combined with scaling and root planing. There is research both in may cause gastrointestinal discomfort. Amoxicillin and Augmentin are
support of and against the use of supplemental therapy to traditional both bactericidal, with Augmentin targeting a more narrow spectrum
biofilm removal.1 When considering the use of adjunctive therapy it than amoxicillin. Augmentin was developed due to amoxicillin’s bacte-
is always important to do a detailed medical health history with your rial resistance from penicillinase enzyme sensitivity.1
patient to rule out any known contraindications. Of the many systemic antibiotics available, there is no consensus as to
an ideal dose and duration. The choice of antibiotic should be made on
Antibiotics an individual basis. In addition to serious adverse effects, like anaphy-
The physical removal of biofilm has proven to be the most effective lactic shock, microbial resistance is a growing concern.4 Other issues
method for treating periodontal disease. The use of adjunctive antibiotic with oral antibiotic administration are patient adherence and adequate
therapy, either systemic or topical, is controversial. Some studies show absorption from the gastrointestinal tract.
superior results with antibiotic use while others show no clinical differ- Understanding that the periodontal disease process may be initi-
ence. There is a general consensus that antibiotics should not be used ated by bacteria but the individual’s host response was critical to the
as a monotherapy in the treatment of periodontal disease. Antibiotics progression of this disease led to the FDA approval of doxycycline at a
as a stand-alone treatment are ineffective at diminishing intact subgin- sub-antimicrobial dose (20mg twice daily). When administered
gival biofilms.2 at this low dose, doxycycline does not cause the long term side
The American Academy of Periodontology has offered guidelines for effects seen with other systemic antibiotics. Randomized double blind
systemic and topical antibiotic use in treating periodontal disease.3 placebo controlled trials demonstrated reduction in probing depths,
These guidelines suggest that aggressive types of periodontitis and improvement in clinical attachment levels and decreased bleeding on
acute periodontal infections should be treated with systemic anti- probing when used as an adjunct with scaling and root planing.5
biotics while chronic infections should be treated with topical therapy.
A recent review evaluating non-surgical chemotherapeutic strategies
Antibiotic therapy is generally used as a follow up treatment after for the management of periodontal disease determined that “systemic
conventional mechanical therapy. Aggressive periodontitis may use antibiotics reach the periodontal tissues by transuduction across
systemic antibiotics as an adjunctive therapy. serum, then cross the crevicular and junctional epithelia to enter the
gingival sulcus.”1 By the time the systemic antibiotic reaches
Classification of Antibiotic Agents That Can Affect Periodontal Microbes the gingival sulcus it no longer has an adequate concentra-
BACTERICIDAL BACTERIOSTATIC tion to achieve the desired antimicrobial effect. This supports
the fact that the mechanical disruption of biofilm must be
Cephalosporins (Includes Keflex®, Ceclor®) Clindamycin*
included in the treatment of periodontal disease.
Macrolides* (Includes Erythromycin, Macrolides* (Includes Erythromycin,
Azithromycin, Clarithromycin) Azithromycin, Clarithromycin) Topical Antibiotic Therapy
Metronidazole Tetracyclines (Includes Doxycycline, Minocycline)
Topical (local) antibiotic/antimicrobial therapy (LAA) was
Penicillins (Includes Ampicillin, Amoxicillin, the natural progression from systemic administration. It
Augmentin®, Penicillin VK)
was thought that LAAs would solve the risk to benefit ratio
Quinolones (Includes Ciprofloxacin) of systemic antibiotics.5 Although there are some studies
*Bactericidal against some organisms at high blood levels supporting the use of topicals, most fail to demonstrate a
Table modified from: Haveles, E. B. (2011). Applied Pharmacology for the Dental Hygienist. (6th ed.). significant difference between scaling and root planing alone.
Maryland Heights, MO: Mosby Elsevier, p. 77-78.
Continued on Page 10
CDHA Journal – Summer 2010 9
Investigations do show benefits for high risk patients, such as smokers, rinse. This term refers to the adherent qualities of a mouthwash and its
who do not respond to mechanical therapy.6-7 Recent studies have ability to be retained. Saliva has a natural flushing property making it
demonstrated that the use of LAAs resulted in an overall reduction of difficult to maintain an antimicrobial effect. Research shows a signifi-
the bacterial bioburden with reduced cardiovascular event risks.8-9 cant antibacterial effect up to 7 hours after mouthrinses with high a
The first locally administered antibiotic for periodontal disease was substantivity property.11
Actisite®, made up of nonabsorbable fibers filled with tetracycline. First generation antimicrobials include phenolic, sanguinarine, qua-
Although Actisite was found to be effective in many cases, placement ternary compounds. Listerine® and its generics are phenolics which
and patient follow-up for fiber removal were challenging issues.1 A possess the only ADA Seal of Acceptance among the first generation
bioabsorbable local delivery device called PerioChip® was then deve- antimicrobials. Listerine contains 26.9% alcohol, alters the bacterial
loped. It was comprised of 34% chlorhexidine gluconate, about 5mm cell wall, and has 36% gingivitis reduction.1 Cepacol® and Scope®,
round and 1mm thick. It is the only LAA that is not an antibiotic. quaternary ammonium compounds, contain 14% and 18.9% alcohol
Atridox® is a 10% doxycyline hyclate gel and is prepared by mixing respectively, increase bacterial cell wall permeability causing cell lysis,
powder and liquid from two syringes. The antibiotic is administered and reduces gingivitis approximately 15%.1
into the gingival sulcus through a cannula. Absorption lasts up to 21 Second generation antimicrobials include cetylpyridinium chloride
days, while therapeutic drug levels in the gingival crevicular fluid start (CPC) and chlorhexidine (CHX). A commercial name for CPC is Crest®
to decline at 7 days. The most notable drawback is the high level of Pro-Health®, which contains 0.07% CPC. Bacteria cells are killed by
clinician skill needed to deliver this therapy as the material tends to cellular pressure, resulting in a similar efficacy as Listerine. Chlorhexi-
come out of the pocket as the syringe is being pulled out of the sulcus. dine has many commercial products including the availability of a
The majority of the time, more than one site can be treated depending nonalcoholic version by Sunstar Americas, Inc. Peridex® by 3M Espe
on the depth and size of the pockets.1 and Periogard® by Colgate® Professional are two examples of popular
Arestin® is comprised of spheres embedded with 2% minocycline HCl chlorhexidine-based products. Their active ingredient is 0.12%
that is slowly released and holds the therapeutic dose in the gingival chlorhexidine. Cell death results from altered osmotic equilibrium.
crivicular fluid for 14-21 days. The most notable drawback for Arestin CHX efficacy in the reduction of certain aerobic and anaerobic bacteria
is the delivery dose. The syringe holds pre-set doses that may not has been shown to be as high as 97% after 6 months of use. CHX
be sufficient for every site. This results in the need to reapply in the has 29% gingivitis reduction. The gingivitis reduction percents listed
same pocket. above for both first and second generation antimicrobials are based on
efficacy data published by manufacturers.1
Currently, resorbable antibiotics such as Atridox® and Arestin® are the
topical antibiotics of choice. The American Academy of Periodontology Other antimicrobials include oxygenating, chlorine dioxide, and zinc
(AAP) supports that local adjuncts, when compared with scaling and chloride agents. Peroxyl® is an oxygenating agent with the active
root planing alone, provide limited improvement.10 Locally admin- ingredient of hydrogen peroxide. It has anti-inflammatory properties
istered antibiotics still require a strict health history review to verify as well as a bubbling action to clean and alleviate discomfort. Short
there are no known allergies. Even though these medications are term studies have produced controversial findings. Oxyfresh®, a 1%
applied topically, as opposed to oral administration, the same chlorine dioxide agent, has minimal plaque reduction. It is a stable,
precautions apply. free radical and an oxidant with algicidal, bactericidal, cysticidal,
fungicidal, sporicidal, and viricidal properties. Oxyfresh is primarily
Antibiotic Brand Name Delivery Absorption used for the treatment of halitosis. Breath Rx® is a zinc chloride agent
10% Doxycyline Atridox® Fluid mixed in a 21 days designed to odorize sulfhydryl groups with zinc ions. It claims to be a
syringe, Multisite scientific bad breath treatment specifically designed to help treat the
2% Minocycline Arestin® Solid dose applies 14-21 days causes of bad breath and the symptoms.1
HCl microspheres with a syringe,
Antimicrobial mouth rinses have been linked to several side effects;
Single site
some more serious than others. First generation compounds like
Antiseptics Listerine can cause a burning sensation and bitter taste. Chlorhexidine
can cause supragingival calculus build-up and staining. Research
Unlike topical controlled-released antibiotics, oral rinses do not has demonstrated permanent damage to enamel through erosive pH
penetrate deep into the gingival sulcus. Despite this limitation they do levels and abrasive antimicrobial toothpastes.1 Carcinogenic changes
show benefit when used adjunctively for gingival inflammation. Oral have been linked to the use of oxygenating agents and mouth rinses
rinses are also of great value in post surgical healing. Substantivity is containing alcohol.1
a crucial component when considering the effectiveness of a mouth
10 CDHA Journal Vol. 25 No. 2
Nutraceuticals have been identified as antigenic targets.19 More research is needed in
As antibiotic resistance becomes more of a concern, health care pro- this field before it is widely accepted as an alternative to antibiotic or
viders looking for alternate adjunctive periodontal therapies for their antimicrobial therapy.
patients. Some examples of nutraceuticals include herbal and nutri- Conclusion
tional supplements and the future of this type of therapy is promising. All drug sensitivities and allergies should be reviewed prior to incorpo-
There are approximately 500,000 plant species, with only 1% having rating pharmacological agents into a patient’s treatment regimen. The
been photochemically investigated. Herbal plant extracts have been future is promising in the areas of nutraceuticals and vaccines but more
shown to reduce the level of biofilms influencing the level of bacterial research is needed. The future of public health can be greatly affected
adhesion. This has shown results with the reduction of periodontal by the scientific breakthroughs becoming made in dentistry. Long time
disease. Some herbs such as Coptidis rhizome extract and Hamamelis traditional regimens of antibiotics and antimicrobials have served
virginiana, are used as bactericidal agents against oral bacteria while our profession well and assisted hygienists to achieve optimal patient
others such as cranberry, Polygonum cuspidatum and Mikania are results.
used to inhibit adhesion.12
About the Author
The use of probiotics in the control of periodontal pathogens is emerg-
ing. Probiotics are “live microorganisms, which when administered Melissa Fellman, RDH, BS, is the Program
in adequate amounts confer a health benefit on the host.”13 Simply Coordinator and Evaluation Specialist for the
put, they are healthy bacteria that displace unhealthy or pathogenic Nevada State Oral Health Program. In addi-
bacteria. A reduction in gingivitis and dental plaque has been shown tion, she is an instructor in the dental hygiene
with the administration of L. reuteri Prodentis® gum chewed twice program at Truckee Meadows Community College
daily in patients with moderate to severe gingivitis.14 GUM® PerioBal- (TMCC) in Reno, NV where she teaches pharma-
ance®, marketed by Sunstar Americas, is a once daily lozenge with cology. Melissa is in the process of completing a
L. reuteri Prodentis® that claims a reduction in moderate to severe Master’s degree in public health at the University
plaque and bad breath.15 EvoraPlus™ from Oragenics, Inc. is another of Nevada, Reno where her graduate research includes conducting a
new probiotic for oral health and is used once daily. This supplement dental hygiene needs assessment on HIV outpatients and developing a
contains a combination of three bacterial strains Streptococcus uberis coalition to increase access to dental hygiene care for HIV positive indi-
KJ2, S. oralis KJ3, and S. rattus JH145, and claims a reduction in viduals in northern NV. Melissa can be reached at mfellman@tmcc.edu
periopathogens within the periodontal pocket.16 References
Antivirals 1. Krayer JW, Leite RS, Kirkwood KL. Non-surgical chemotherapeutic treatment
strategies for the management of periodontal diseases. Dent Clin N Am. 2010;
A new area of research when evaluating periodontal disease is the use 54: 13-33.
of antivirals. The Epstein-Barr (EBV) virus has been associated with 2. Schaudinn C, Gorur A, Keller D, Sedghizadeh PP, Costerton JW. Periodontitis:
recurrent periodontal disease. Since bacterial disease may be second- an archetypical biofilm disease. JADA. 2009;140: 978-86.
ary to viral infections, antiviral treatment decreases EBV and improves 3. The American Academy of Periodontology (AAP). J. Periodontol. 2004;75: 1553-65.
the periodontal condition.17 The Human Cytomegalovirus (HCMV) has 4. Heitz-Mayfield LJA. Systemic antibiotics in periodontal therapy. Aus Dent J.
also been linked to periodontal disease. The HCMV can cause infections 2009;54(1 Suppl): S96-S101.
in immune-compromised individuals like organ transplant patients or 5. Cortelli JR, Aquino DR, Cortillo SC, Carvalho-Filho J, Roman-Torres CVG, Costa
patients with acquired immune deficiency syndrome (AIDS). Periodon- FO. A double-blinded randomized clinical trial of subgingival minocycline for
chronic periodontitis. J Oral Sci. 2009;50(3): 259-65.
tal lesions can exhibit great amounts of EBV and HCMV. Anti-herpes-
virus chemotherapy can decrease salivary viral loads resulting in the 6. Goodson JM, Gunsolley JC, Grossi SG, Bland PS, Otomo-Corgel J, Doherty F,
Comiskey J. Minocycline HCl microspheres reduce red-complex bacteria in
improvement if secondary bacterial periodontal infections exist.18 periodontal disease therapy. J Periodontol. 2007;78: 1568-79.
Vaccines 7. Machion L, Andia DC, Lecio G, Nociti FH Jr, Casati MZ, Sallum AW, Sallum EA.
Locally delivered doxycylcline as an adjunctive therapy to scaling and root
Vaccine therapy in the fight against periodontal disease is also a new planing in the treatment of smokers: a two-year follow-up. J Periodontol.
and exciting option. As discussed earlier, antibiotic resistance is a 2006;77(4): 606-13.
growing worldwide problem. Vaccines offer a solution to the overuse of 8. D’Aiuto F, Parkar M, Nibali L, Suvan J, Lessem J, Tonetti MS. Periodontal infections
antibiotics in dentistry. Vaccine development is based on the identifica- cause changes in traditional and novel cardiovascular risk factors: results from a
randomized controlled clinical trial. Am Heart J. 2006;151(5): 977-84.
tion of virulence factors that stimulate the induction of salivary
immunoglobulin A antibody response. When used for periodontal
disease, Porphyromonas gingivalis and Aggregatibacter actinobacillus References continued on Page 25
CDHA Journal – Summer 2010 11
CareerCorner
What is the most exciting aspect of your work? Anna Matsuishi Pattison received her
Traveling and teaching hands-on advanced periodontal instrumen- BS degree in Dental Hygiene from the
tation courses around the world. Basic instrumentation skills and University of Southern California and
ultrasonic instrumentation are taught and practiced everywhere but her MS degree in Dental Hygiene from
there are very few teachers or practitioners who have ever been Columbia University. She has been an
able to take an advanced course that focuses on access, adaptation Associate Professor at USC for over 30
and scaling of difficult problem areas such as deep distal or palatal years and has served as Chair of the
pockets, line angles and furcations. When I teach the advanced Department of Dental Hygiene. Ms.
instrumentation course, the rapid improvement and gratitude of Pattison has been a featured speaker
these clinicians is extremely rewarding and renews my resolve to throughout then US, Asia, Europe, Australia and New Zealand. She
keep on traveling and teaching. is currently the Co-Director with her husband, Dr. Gordon Pattison,
of the Pattison Institute which offers lectures and hands-on instru-
What do you believe our profession should know about mentation workshops throughout the U.S. and abroad. In 2005, she
periodontal disease in 2010? received the Pfizer-ADHA Excellence in Dental Hygiene Award and
Regardless of adjunctive antimicrobial therapies such as local the USC School of Dentistry Alumnus of the Year Award. In 2006
delivery antibiotics, subgingival irrigation or lasers, the keystone of she received the California Society of Periodontists Award. In 2009
good periodontal therapy still is, and has always been, thorough she was selected to be inducted into the USC School of Dentistry
debridement of calculus and biofilm. Looking for a fast, easy way Hall of Fame. Anna is currently editor-in-chief of Dimensions of
out and shifting the focus away from meticulous root debridement Dental Hygiene.
is a dangerous path. Dental hygienists, who lose their focus and do
not develop advanced skills, run the risk of losing their positions to
lesser educated individuals.
Pharmacology references continued from page 11
I have heard some dentists say, “I can teach a monkey to scale.”
9. Tonetti MS, D’Aiuto F, Nibali L, et al. Treatment of periodontitis and endothelial
After 40 years of teaching dental and dental hygiene students, I function. N Engl J Med. 2007;356(9): 911-20.
know that I can teach any student to gross scale with an ultrasonic
10. The American Academy of Periodontology (AAP). J. Periodontol. 2007;71: 125-40.
scaler and place Arestin® in a short period of time. However, I can
11. Tomás I, García-Caballero L , Cousido MC, Limeres J, Álvarez M, Diz P.
only teach a small number of students to be very highly skilled Evaluation of chlorhexidine substantivity on salivary flora by epifluorescence
at advanced periodontal scaling and root planing. Our profession microscopy. J Oral Dis. 2009;16(6): 428-33.
needs to be recognized for special knowledge and exceptional skills 12. Palombo EA. Traditional medicinal plant extracts and natural products with
that are not easily acquired. activity against oral bacteria: potential application in the prevention and
treatment of oral diseases. eCAM. 2009;1-15.
Periodontal disease is not simple and it is not easy to treat
13. Food and Health Agricultural Organization of the United Nations and World
effectively. Excellent treatment requires intensive initial therapy and Health Organization. Guidelines for the evaluation of probiotics in foods. Joint
constant vigilance during a lifetime of maintenance. Hygienists who FAO/WHO Working Group Report on Drafting Guidelines for the Evaluation of
oversimplify periodontal treatment do a great disservice to their Probiotics in Food. 2002. Available from: ftp://ftp.fao.org/es/esn/food/
wgreport2.pdf
patients and to the dental hygiene profession as a whole.
14. Krasse P, Carlsson B, Dahl C, Paulsson A, Nilsson A, Sinkiewicz G. Decreased gum
Please share a memorable experience from your bleeding and reduced gingivitis by the probiotic Lactobacillus reuteri.
professional career. Swed Dent J. 2006;30(2): 55-60.
From 1973 to 1975, I shared an office and taught dental students 15. GUM PerioBalance. A breakthrough in oral healthcare. 2009. Available from:
http://www.periobalance.com/default.aspx.
with Dr. Esther Wilkins at the Tufts School of Dental Medicine in
16. Evoraplus. Healthy gums and teeth. 2009. Available from: http://evoraplus.com/
Boston. What an experience to be able to teach with and assist the index.php?option=com_content&view=section&layout=blog&id=10<emid-57
“Guru” of Dental Hygiene! We worked together so well that we 17. Sunde PT, Olsen I, Enersen M, Grinde B. Patients with severe periodontitis and
developed a deep professional and personal friendship that has subgingival Epstein-Barr virus treated with antiviral therapy. J Clin Vir. 2008;42:
lasted for 37 years. We now lecture together in a continuing educa- 176-8.
tion course that allows us to travel together all over the country. 18. Sahin S, Saygun I, Kubar A, Slots J. Periodontitis lesions are the main source of
salivary cytomegalovirus. Oral Micro Immunol. 2009;24: 340-2.
Dr. Wilkins’ influence on me and almost every other hygienist in the
19. Liu P-F, Zhu W-H, Huang C-M. Vaccines and photodynamic therapies for oral
country has been profound. She continues to inspire me to do my microbial-related disease. Curr Drug Metab. 2009;10(1): 90-4.
best to keep working and contributing to our profession.
CDHA Journal – Summer 2010 25
Copyright of Journal of the California Dental Hygienists' Association is the property of California Dental
Hygienists' Association and its content may not be copied or emailed to multiple sites or posted to a listserv
without the copyright holder's express written permission. However, users may print, download, or email
articles for individual use.
You might also like
- Antibiotics in Periodental TreatmentDocument29 pagesAntibiotics in Periodental TreatmentJana AliNo ratings yet
- Non Antibiotic AcneDocument34 pagesNon Antibiotic AcneAdrian SyahNo ratings yet
- Chapter 044Document5 pagesChapter 044borisdevic223No ratings yet
- The Clinical Relevance of Antibiotic ResistanceDocument7 pagesThe Clinical Relevance of Antibiotic ResistanceKadir KUCUKNo ratings yet
- Systemic Anti-Infective Therapy For Periodontal Diseases: Sebastian G. Ciancio - Angelo J. MariottiDocument13 pagesSystemic Anti-Infective Therapy For Periodontal Diseases: Sebastian G. Ciancio - Angelo J. MariottiYessenia SarabiaNo ratings yet
- PharmacologyinEndodontics PDFDocument6 pagesPharmacologyinEndodontics PDFShikhaNo ratings yet
- Tackling Antimicrobial Resistance: Optimizing Use of An Older Antibiotic-AmoxicillinDocument3 pagesTackling Antimicrobial Resistance: Optimizing Use of An Older Antibiotic-AmoxicillinDiian WulaandariNo ratings yet
- Antibiotic Resistance: A Common Challenge in DentistryDocument6 pagesAntibiotic Resistance: A Common Challenge in DentistryIJAR JOURNALNo ratings yet
- Khamlin Hamad Abdal - GroupeaDocument39 pagesKhamlin Hamad Abdal - GroupeaKhamlin NurseNo ratings yet
- Khamlin Hamad Abdal - GroupeaDocument39 pagesKhamlin Hamad Abdal - GroupeaKhamlin NurseNo ratings yet
- Antibiotics Use in DentistryDocument5 pagesAntibiotics Use in DentistryIyad Abou-RabiiNo ratings yet
- Topical Antibiotics in Dermatology: An Update on Uses and ResistanceDocument19 pagesTopical Antibiotics in Dermatology: An Update on Uses and ResistanceFernanda PutriNo ratings yet
- Acne Treatments: Future Trajectories: Review ArticleDocument7 pagesAcne Treatments: Future Trajectories: Review ArticleIsabel Zamora AuzaNo ratings yet
- AntibioticsDocument9 pagesAntibioticsKerlyMurilloMoraNo ratings yet
- Paro OriginalDocument9 pagesParo OriginalClaudia-Andreea ManeaNo ratings yet
- Antimicrobial Therapy in Veterinary MedicineFrom EverandAntimicrobial Therapy in Veterinary MedicineSteeve GiguèreRating: 4 out of 5 stars4/5 (1)
- Antibiotics and Antibiotic ProphylaxisDocument8 pagesAntibiotics and Antibiotic ProphylaxisDani MuñozNo ratings yet
- Systemic Antibiotics in Periodontal Therapy: LJA Heitz-MayfieldDocument6 pagesSystemic Antibiotics in Periodontal Therapy: LJA Heitz-Mayfieldapi-239502672No ratings yet
- anti microbial drugsDocument35 pagesanti microbial drugsUmashankar SharmaNo ratings yet
- Basic Dental PharmacologyDocument152 pagesBasic Dental PharmacologyDr-Mohamed KandeelNo ratings yet
- Oral Antibiotic Treatment Options For Acne Vulgaris: ReviewDocument7 pagesOral Antibiotic Treatment Options For Acne Vulgaris: ReviewvaiyenNo ratings yet
- Role of Antibiotics in EndodonticsDocument45 pagesRole of Antibiotics in EndodonticsAshutosh KumarNo ratings yet
- Chemotherapy Agents in Periodontal Treatment 2Document5 pagesChemotherapy Agents in Periodontal Treatment 2shathaNo ratings yet
- Antibiotics Used in DentistryDocument17 pagesAntibiotics Used in Dentistrymegamarwa50% (2)
- Central academy student project on antibioticsDocument17 pagesCentral academy student project on antibioticsKartikey VermaNo ratings yet
- AntibioticsDocument63 pagesAntibioticsSahin mollickNo ratings yet
- Uso de Antibióticos en EquinoDocument8 pagesUso de Antibióticos en EquinofdfdfdfNo ratings yet
- Wound 2016 0701Document9 pagesWound 2016 0701Ine Marthia DanieNo ratings yet
- StewardshipDocument19 pagesStewardshipJorge David LopezNo ratings yet
- 00C PrefaceDocument2 pages00C PrefaceJessica AdvínculaNo ratings yet
- AAE Position StatementDocument5 pagesAAE Position StatementCarlos San MartinNo ratings yet
- Clinical Microbiology and InfectionDocument3 pagesClinical Microbiology and InfectionRaphaela BarretoNo ratings yet
- Antimicrobials: Access and Sustainable Eff Ectiveness 2: SeriesDocument12 pagesAntimicrobials: Access and Sustainable Eff Ectiveness 2: SeriesBrenda Cáceres MejíaNo ratings yet
- CrossmDocument9 pagesCrossmAnida HasnaNo ratings yet
- G AntibioticTherapyDocument3 pagesG AntibioticTherapyJacoboGonzálezNo ratings yet
- Host Modulation Sameeksha 2022Document120 pagesHost Modulation Sameeksha 2022satyaki vermaNo ratings yet
- BP AntibiotictherapyDocument4 pagesBP AntibiotictherapyDebasmita Datta GuptaNo ratings yet
- AntibioticDocument25 pagesAntibioticgzmrc6sfrnNo ratings yet
- Tài Liệu Về Các Kháng Sinh 2Document15 pagesTài Liệu Về Các Kháng Sinh 2tuannguyen010700No ratings yet
- Day 2 General Microbiology 12-1-2021Document150 pagesDay 2 General Microbiology 12-1-2021ShriefElghazalyNo ratings yet
- Ramesh Amitha Local Drug Delivery in PeriodontalDocument6 pagesRamesh Amitha Local Drug Delivery in Periodontalsobhan hajianNo ratings yet
- Topical and Systemic Antibiotics in The Management of Periodontal DiseasesDocument12 pagesTopical and Systemic Antibiotics in The Management of Periodontal DiseasesxdxdxdxdNo ratings yet
- Chemistry Project DraftDocument9 pagesChemistry Project DraftSamrat BanerjeeNo ratings yet
- Prepared by The: Antibiotic Guidelines 3 Edition 2011Document82 pagesPrepared by The: Antibiotic Guidelines 3 Edition 2011araNo ratings yet
- 2016 ChemBiol Antibiotics A New HopeDocument8 pages2016 ChemBiol Antibiotics A New HopeIgnacio Pérez-VictoriaNo ratings yet
- Best Antibiotics for Managing Dental InfectionsDocument5 pagesBest Antibiotics for Managing Dental InfectionsNurfidini AzmiNo ratings yet
- Antifungal Stewardship - What We Need To KnowDocument7 pagesAntifungal Stewardship - What We Need To KnowAkbar SaleemNo ratings yet
- Trat AntimicobDocument6 pagesTrat AntimicobAlex MihaelaNo ratings yet
- Adverse Drug Interactions in Dermatology: Cation Binding and CYP Enzyme InductionDocument8 pagesAdverse Drug Interactions in Dermatology: Cation Binding and CYP Enzyme InductionkuronohanaNo ratings yet
- ID 6-Antimicrobial Policy 2022 Student EditionDocument30 pagesID 6-Antimicrobial Policy 2022 Student Edition白羽マイリフNo ratings yet
- Novel Pyrazole Analogues as Antimicrobial AgentsDocument11 pagesNovel Pyrazole Analogues as Antimicrobial AgentsWalid EbaiedNo ratings yet
- Drug CombinationsDocument15 pagesDrug CombinationsntnquynhproNo ratings yet
- Antibiotic in Obstetric and GynecologyDocument36 pagesAntibiotic in Obstetric and GynecologyDrAbdi YusufNo ratings yet
- Antibiotic Stewardship in Critical Care: Ian Johnson MBCHB Frca and Victoria Banks Mbbs BSC Frca Fficm EdicDocument6 pagesAntibiotic Stewardship in Critical Care: Ian Johnson MBCHB Frca and Victoria Banks Mbbs BSC Frca Fficm EdicRavi KumarNo ratings yet
- Journal Reading - One Health's Importance in Helping to Better Control Antimicrobial ResistanceDocument49 pagesJournal Reading - One Health's Importance in Helping to Better Control Antimicrobial ResistanceLoudry Amsal EGNo ratings yet
- Henson 2019Document5 pagesHenson 2019Edimar Joshua FrialaNo ratings yet
- Comparative Efficacy of Amoxicillin Clavulanate and Clindamycin in Management of Resistant Orofacial Infection. Randomized Clinical TrialDocument7 pagesComparative Efficacy of Amoxicillin Clavulanate and Clindamycin in Management of Resistant Orofacial Infection. Randomized Clinical TrialInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Avent Et Al-2011-Internal Medicine JournalDocument9 pagesAvent Et Al-2011-Internal Medicine JournalAgil Wahyu WicaksonoNo ratings yet
- EBSCO Metadata 2023 04 19Document68 pagesEBSCO Metadata 2023 04 19psychologistnsmNo ratings yet
- Medsurg Cardio Ana&PhysioDocument6 pagesMedsurg Cardio Ana&Physiorabsibala80% (10)
- Atlas de Oncologia Clinica PDFDocument512 pagesAtlas de Oncologia Clinica PDFAlfonso Carlos Gutierrez MartinezNo ratings yet
- Lupin Project CompatibleDocument97 pagesLupin Project CompatibleNitish SinghNo ratings yet
- Program CraiovaDocument9 pagesProgram Craiovaonix2000No ratings yet
- Worksheets EBMDocument19 pagesWorksheets EBMRizki IrwansyahNo ratings yet
- Angel EssenceDocument23 pagesAngel EssenceShivani Manchanda50% (2)
- Nutrition in The Critically Ill PatientDocument13 pagesNutrition in The Critically Ill PatientnainazahraNo ratings yet
- How To Grow Medicinal MarijuanaDocument9 pagesHow To Grow Medicinal MarijuanaRoy HarperNo ratings yet
- Panic DisorderDocument60 pagesPanic Disordergrinakis100% (1)
- Caries Predication, Risk Assessment and Treatment PlanningDocument74 pagesCaries Predication, Risk Assessment and Treatment PlanningmohammadNo ratings yet
- Self-motivation quiz tipsDocument1 pageSelf-motivation quiz tipsRose D GuzmanNo ratings yet
- ESC Guidelines for Diagnosis and Treatment of Acute and Chronic Heart FailureDocument61 pagesESC Guidelines for Diagnosis and Treatment of Acute and Chronic Heart FailureSurya ArhNo ratings yet
- Cognitive-Behavioral Therapy For Adult ADHD - An Integrative Psychosocial and Medical Approach (PDFDrive) PDFDocument253 pagesCognitive-Behavioral Therapy For Adult ADHD - An Integrative Psychosocial and Medical Approach (PDFDrive) PDFRaúl BonillaNo ratings yet
- Nurse Practitioner VS Physical TherapistsDocument5 pagesNurse Practitioner VS Physical Therapistspdet1No ratings yet
- Sigmund Freud's TheoryDocument22 pagesSigmund Freud's TheoryGil Mark B TOmas100% (2)
- Essential medicines certificateDocument2 pagesEssential medicines certificateAnji KaringuNo ratings yet
- Acute Intestinal Failure.11Document6 pagesAcute Intestinal Failure.11albimar239512No ratings yet
- GuidlinesDocument10 pagesGuidlinesbubuvulpeaNo ratings yet
- Acute Gingival InfectionsDocument35 pagesAcute Gingival InfectionsAhmed Tawfig GamalNo ratings yet
- Kasabach Merritt SyndromeDocument33 pagesKasabach Merritt SyndromeAndrew Arnold David VillanuevaNo ratings yet
- Tgwellness Massage g10pdfDocument71 pagesTgwellness Massage g10pdfStephenNo ratings yet
- Letty KuanDocument1 pageLetty KuanchrizthineeNo ratings yet
- ESMRDocument23 pagesESMRbiogene_bdNo ratings yet
- NICE Infection Control GuidelinesDocument702 pagesNICE Infection Control Guidelinesyewha550No ratings yet
- Modulo 200Document2 pagesModulo 200suso73No ratings yet
- Accidental Intravenous Infusion of Air: A Concise ReviewDocument5 pagesAccidental Intravenous Infusion of Air: A Concise ReviewSiswand BIn Mohd AliNo ratings yet
- Foreign Qualification Recognition GuideDocument2 pagesForeign Qualification Recognition Guidesatishg99No ratings yet
- Cheat Sheet (AutoRecovered)Document2 pagesCheat Sheet (AutoRecovered)Garry LeeNo ratings yet
- Dr. Smith's ECG Blog - "Shark Fin" - A Deadly ECG Sign That You Must Know! PDFDocument7 pagesDr. Smith's ECG Blog - "Shark Fin" - A Deadly ECG Sign That You Must Know! PDFZACHARIAH MANKIRNo ratings yet