Professional Documents
Culture Documents
ICD-10-CM Documentation and Coding For Obstetric Procedures: Adviser
Uploaded by
Rocking ChairOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ICD-10-CM Documentation and Coding For Obstetric Procedures: Adviser
Uploaded by
Rocking ChairCopyright:
Available Formats
Reimbursement
ADVISER
ICD-10-CM documentation
and coding for obstetric procedures
With the new system set to take effect in
less than a month, here’s what you need to
know about key changes to obstetric coding
Melanie Witt, RN, CPC, COBGC, MA
T
he countdown is on for the big How to get started
coding switch. Last month I wrote Figuring out where you are now goes a long
about changes in International way toward knowing where you need to be
Classification of Diseases, 10th Revision, when the calendar changes to October 1—
Clinical Modification (ICD-10-CM) codes and the best way to do it is to perform a gap
that will occur in relation to gynecologic analysis. This analysis can be carried out by the
services, but now it’s time to tackle obstetric clinician or a qualified practice staff person. IN THIS
ARTICLE
services. For obstetricians, the changes will To begin, run a report of the distinct
be all about definitions. And documentation obstetric codes you have billed in 2015 How to do a
of obstetric conditions will be more compli- by frequency. Then sort them in numeric gap analysis
cated due to several factors, including the order so that each individual code category
need to report trimester information and is captured for all of the 5th digits (and the
This page
gestational age, use of a placeholder code, code then will be counted as a single code).
more complex guidelines for certain condi- Finally, review 5 medical records for each of Highlights of
tions, chorionicity for multiple gestations, the top 10 reported diagnosis categories and OB coding
and use of a 7th digit to identify the fetus determine whether you could have reported Page 16
with a problem. a more specific ICD-10-CM code.
No one is expecting clinicians to instantly The information you gain will go a long Condition-specific
ILLUSTRATION: MARY ELLEN NIATAS FOR OBG MANAGEMENT
be fluent in code-speak, but in order for the way toward identifying potential weak- coding notations
most specific diagnoses to be reported, the nesses in the documentation, or, if you are
Page 20
clinical documentation must be spot on. currently using an electronic health record
Think of it this way: ICD-10-CM is not requir- (EHR) to look up a code, it will point up any
ing you to document more, it’s requiring you weak points in searching for the right code,
to document more precisely. based on your specific documentation at the
encounter. Remember, practice makes per-
fect…eventually.
Ms. Witt is an independent coding and documentation Well-trained staff can help
consultant and former program manager, department Not only must you, the clinician, learn about
of coding and nomenclature, American Congress of
Obstetricians and Gynecologists. the part your clinical documentation will play
Ms. Witt reports no financial relationships relevant to in providing the most specific information
this article. that will lead to a very specific code, but your
ob g m a n a g e me n t . c om Vol. 27 No. 9 | September 2015 | OBG Management 15
Reimbursement
ADVISER
coding and billing staff will need training as • second: 14 weeks, 0 days to less than
well. They are the ones who should be check- 28 weeks, 0 days
ing your claims for accuracy from October 1 • third: 28 weeks, 0 days until delivery.
forward, as they will know the basic rules Examples of trimester codes include:
about which codes can be billed together, • O25.11 Malnutrition in pregnancy, first
code order, place codes, and so on. In other trimester
words, while you as a clinician should be re- • O14.02 Mild to moderate preeclampsia,
sponsible for picking the more specific code second trimester
in ICD-10-CM, your staff is your backup • O24.013 Preexisting diabetes mellitus,
when you don’t. type 1, in pregnancy, third trimester.
Feedback from your staff on how the However, definitions in ICD-10-CM go
claims are being processed and, perhaps, the beyond this, and these definitions will have
overuse of unspecified codes will keep you to be taken into account to provide sufficient
moving toward the goal of complete and pre- documentation to report the condition.
cise clinical documentation and the report- In ICD-9-CM, a missed abortion and early
ing of diagnoses at the highest level possible hemorrhage in pregnancy occurred prior to
given the documentation. 22 completed weeks, but in ICD-10-CM that
definition changes to prior to 20 completed
weeks.
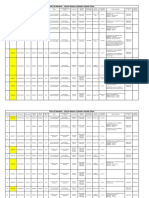
Highlights of ICD-10-CM Additional definitions that may impact
obstetric coding coding:
Given the complexity of obstetric coding, this • preterm labor or delivery: 20 completed
article deals only with the most important weeks to less than 37 completed weeks
changes. It will be up to each clinician to learn • full-term labor or delivery: 37 com-
the rules that surround the diagnostic codes pleted weeks to 40 completed weeks
that you report most frequently. Here again, • postterm pregnancy: more than
For inpatient a trained staff can help by preparing specific 40 completed weeks to 42 completed weeks
admissions, the coding tools for the most frequently used di- • prolonged pregnancy: more than
trimester will be agnoses, including notes about what must be 42 completed weeks.
based on the in the record to report the most specific code. You also will be required to include a
code for gestational age any time you report
gestational age
Trimester, gestational age, an obstetric complication. This and the tri-
at the time of
and timing definitions mester information will change as the preg-
admission, even
The majority of obstetric complication codes nancy advances, so always be sure that the
if the patient is
(these are the codes that start with the letter code selected matches the gestational age on
hospitalized over “O”) and the “Z” codes for supervision of a the flow sheet at the time of the encounter. The
more than normal pregnancy require trimester infor- gestational age code is Z3A.__, with the final
one trimester mation to be valid. In the outpatient setting, 2 digits representing the weeks of gesta-
the trimester will be based on the gestational tion (for instance, from 27 weeks, 0 days to
age at the date of the encounter. For inpatient 27 weeks, 6 days, the final 2 digits will be “27”).
admissions, the trimester will be based on ICD-10-CM also has different conven-
the age at the time of admission; if the patient tions when it comes to timing as it relates to
is hospitalized over more than one trimester, conditions that are present during the epi-
it is the admission trimester that continues to sode in which the patient delivers. When this
be recorded, not the discharge trimester. is the case, an “in childbirth” code must be
Although there are codes that indicate selected instead of assigning the diagnosis
an unspecified trimester, they should be by trimester, if one is available. There also
reported rarely if this information is, in fact, are codes that are specific to “in the puer-
available. Trimesters are defined as: perium,” and these generally will be reported
• first: less than 14 weeks, 0 days after the patient has been discharged after
CONTINUED ON PAGE 18
16 OBG Management | September
January 2015
2015
| Vol.
| Vol.
27 27
No.1
No. 9 o bg manag ement.co m
Reimbursement
ADVISER
CONTINUED FRO M PAGE 16
Most docs still not ready for ICD-10 switch
A majority of physician practices will not be ready when the ICD-10 compliance date rolls
around on October 1, according to a recent survey by the Workgroup for Electronic Data
Interchange (WEDI).
Less than half of physician practices reported that they were ready or would be ready
to implement ICD-10 by the compliance date. Nearly one-quarter of practices indicated they
would not be ready, with the balance identifying their readiness status as “unknown.”
The WEDI survey was conducted in June, prior to the Centers for Medicare and Medicaid
Services’ announcing a 1-year transition period during which Medicare will not deny claims
based solely on the specificity of diagnosis codes, provided they are in the appropriate family
of ICD-10 codes.
Physician practices “may now be working more quickly toward compliance, since the
potential for further delay has been removed,” WEDI wrote in a letter to Health and Human
Services Secretary Sylvia Burwell.
WEDI, formed in 1991 by the HHS and named as an advisory organization to the agency
under HIPAA, warned that if physician practices in particular “do not make a dedicated and
aggressive effort to complete their implementation activities in the time remaining, there is
likely to be disruption to industry claims processing on Oct. 1, 2015.”
Physician practices may have a lot of catching up to do in a short amount of time be-
cause of inaction taken with each delayed implementation date. Many organizations “did not
take full advantage of this additional time and as indicated in prior surveys, many organiza-
tions stopped or slowed down efforts when a delay was announced,” WEDI noted.
In a separate letter, WEDI called for more transparency regarding the readiness of state
Medicaid agencies to convert to ICD-10, and urged the HHS to appoint an ombudsman for
ICD-10 as soon as possible.
Copyright © 2015 Ob.Gyn. News Digital Network, Frontline Medical Communications. http://www.obgynnews.com/practice-economics
/practice-management/single-article/most-docs-still-not-ready-for-icd-10-switch/11c918da2cfee2c84c068fc638c204c5.html.
For multiple
gestations, several delivery but also would be reported if there is second and third terms mean that it devel-
code categories no “in childbirth” code available at the time oped prior to delivery. For example, code
of delivery. The code categories to which this O90.81, Anemia of the puerperium, refers
require a 7th
concept will apply are: to anemia that develops following delivery,
numeric character
• preexisting hypertension while code O99.03 Anemia complicating the
of 0 or 1 through 9
• diabetes mellitus puerperium, denotes preexisting anemia that
• malnutrition is still present in the postpartum period.
• liver and biliary tract disorders
• subluxation of symphysis (pubis) Multiple gestation coding
• obstetric embolism and the 7th digit
• maternal infectious and parasitic diseases The first thing you will notice here is that
classifiable elsewhere several code categories require a 7th numeric
• other maternal diseases classifiable character of 0 or 1 through 9. This rule will ap-
elsewhere ply to the following categories:
• maternal malignant neoplasms, traumatic • complications specific to multiple gestation
injuries, and abuse classifiable elsewhere. • maternal care for malpresentation of fetus
Taking time to read a code description • maternal care for disproportion
from a search program or drop-down menu • maternal care for known or suspected fetal
also will be important because some codes abnormality and damage
refer to “of the puerperium” versus “com- • maternal care for other fetal problems
plicating the puerperium” or “in the puer- • polyhydramnios
perium.” The first reference means that the • other disorders of amniotic fluid and
condition develops after delivery, while the membranes
CONTINUED ON PAGE 20
18 OBG Management | September 2015 | Vol. 27 No. 9 o bg manag ement.co m
Reimbursement
ADVISER
CONTINUED FRO M PAGE 18
CMS takes steps to ease transition to ICD-10-CM
To help health care providers get “up to speed” on the International Classification of Diseases,
10th Revision, Clinical Modification (ICD-10-CM), which takes effect October 1, 2015, the
Centers for Medicare and Medicaid Services (CMS) has launched a new series for specialists.
A guide tailored to ObGyns is available at http://roadto10.org/example-practice-obgyn. The
guide includes:
• common codes for the specialty, such as excessive, frequent, and irregular menstruation;
disorders of the breast; and inflammation of the vagina and vulva, with corresponding
ICD-9-CM codes
• a primer on changes in clinical documentation that involve new definitions and terminology
and a need for greater specificity
• clinical scenarios to demonstrate key ICD-10-CM concepts, such as a patient with a breast
lump at her annual well-woman exam
• links to other resources, including Webcasts on various topics.
The guide is geared to small ObGyn practices making the switch to the new system.
• preterm labor with preterm delivery unspecified code would be reported in that
• term delivery with preterm labor case. In addition, if there is a continuing
• obstructed labor due to malposition and pregnancy after fetal loss, the cause must
malpresentation of fetus be identified within the code (that is, fetal
• labor and delivery with umbilical cord reduction, fetal demise [and retained], or
complications. spontaneous abortion).
A 7th character of 0 will be reported if
this is a singleton pregnancy, and the num- Documentation requirements for
Documentation bers 1 through 5 and 9 refer to which fetus of certain conditions
needs to the multiple gestation has the problem. The If you plan on reporting any complication of
state whether number 9 would indicate any fetus that was pregnancy at the time of the encounter, infor-
hypertension is not labeled as 1 to 5. mation about that condition needs to be part
The trick in documentation will be iden- of the antepartum flow sheet comments. If,
preexisting or
tifying the fetus with the problem consis- at the time of the encounter, a condition the
gestational
tently while still recognizing that, in some patient has is not addressed and the entire
cases, such as fetal position, twins may visit involves only routine care, you would re-
switch places. On the other hand, if one fetus port the code for routine supervision of preg-
is small for dates, chances are good that this nancy rather than the complication code.
fetus will remain so during pregnancy when If the complication is again addressed at a
twins are present. later visit, the complication code would be
A code will be denied as invalid without reported again for that visit. The routine su-
this 7th digit, so it will be good practice for pervision code and the complication code
the clinician to document this information at cannot be reported on the record for the
each visit. same encounter under ICD-10-CM rules.
Additional information in regard to Hypertension. Documentation needs to
multiple gestations will be the chorionicity state whether the hypertension is preexisting
of the pregnancy, if known, but there will or gestational. If it is preexisting, it needs to
also be an “unable to determine” and an be identified as essential or secondary. If the
“unspecified” code available if that better fits patient also has hypertensive heart disease
the documentation for the visit. Note, how- or chronic kidney disease, this information
ever, that there is no code for a trichorionic/ should be included, as different codes must
triamniotic pregnancy; therefore, only the be selected.
20 OBG Management | September 2015 | Vol. 27 No. 9 o bg manag ement.co m
Diabetes. The documentation needs to • Abnormal findings on antenatal screening.
state whether it is preexisting or gestational. These would be reported when the ante-
If preexisting, you must document whether natal test is abnormal but you have not yet
it is type 1 or type 2. If it is type 2, you must determined a definitive diagnosis.
report an additional code for long-term in- • Alcohol, drug, and tobacco use during
sulin use, if applicable. The assumption for a pregnancy. If you report any of these codes,
woman with type 1 diabetes is that she is al- you must also report a manifestation code
ways insulin-dependent, so long-term use is for the patient’s condition. If the use is
not reported separately. Note, however, that uncomplicated, you would report that
neither metformin nor glyburide is consid- code instead.
ered insulin and there is no mechanism for • Abuse of the pregnant patient. You can
reporting control with these medications. report sexual, physical, or psychological
If diabetes is gestational, you must indi- abuse, but you also must report a code for
cate whether the patient’s blood glucose level any applicable injury to the patient and
is controlled by diet or insulin. If both, report identify the abuser, if known.
only the insulin. There is no code for the use • Pruritic urticarial papules and plaques
of other medications for the control of gesta- of pregnancy
tional diabetes, so you would have to report • Retained intrauterine contraceptive device
an unspecified code in that case. in pregnancy
Also note that ICD-10-CM differentiates • Maternal care due to uterine scar from other
between an abnormal 1-hour glucose toler- previous surgery. This would mean a surgery
ance test (GTT) and gestational diabetes. other than a previous cesarean delivery.
Unless a 3-specimen or 4-specimen GTT has • Maternal care for (suspected) damage to
been performed and results are abnormal, a the fetus by other medical procedures
diagnosis of gestational diabetes should not • Maternal care for hydrops fetalis
be reported. • Maternal care for viable fetus in abdominal
An additional code outside of the obstet- pregnancy If you report
ric complication chapter is required to denote • Malignant neoplasm complicating sexual, physical,
any manifestations of diabetes. If there are pregnancy or psychological
none, then a diabetes uncomplicated mani- • Failed attempt at vaginal birth after previ- abuse, you must
festation code must be reported. ous cesarean delivery
also report a code
Preterm labor and delivery. Your docu- • Supervision of high-risk pregnancy due to
for any applicable
mentation must clearly indicate whether social problems (for instance, a homeless
injury and identify
the patient has preterm labor with preterm patient)
the abuser, if known
delivery or whether the delivery is term in • Rh incompatibility status (when you lack
addition to the trimester. For instance, if you confirmation of serum antibodies and
document that Mary presents with preterm are giving prophylactic Rho[D] immune
labor at 27 weeks, 2 days and delivers a girl globulin).
at 28 weeks, 6 days, your code will describe
Preterm labor second trimester with preterm
delivery third trimester. However, if Susan Parting words
presents with preterm labor at 30 weeks, ICD-10-CM may seem like the end of the
2 days and is managed until 37 weeks, 1 day, world, but its difficulty is exaggerated. If you
when she delivers a baby boy, your code fail to prepare, you will fail, and money com-
would describe Term delivery with preterm ing in the door may be affected. If you pre-
labor, third trimester. pare with training and practice, you will have
a short learning curve. I wish you all the best.
New coding options If you have specific questions about your
Among the new coding options under practice, don’t hesitate to let us know so they
ICD-10-CM: can be addressed early.
ob g m a n a g e me n t . c om Vol. 27 No. 9 | September 2015 | OBG Management 21
You might also like
- Changing Paradigms Optometric Vision Therapy Is Neuro-ScienceDocument4 pagesChanging Paradigms Optometric Vision Therapy Is Neuro-SciencePierre A. RodulfoNo ratings yet
- Icd 10ebookDocument41 pagesIcd 10ebookPkts Universitas Duta Bangsa100% (3)
- Monitoring Coding Compliance: Richard F. Averill, M.SDocument10 pagesMonitoring Coding Compliance: Richard F. Averill, M.SKiran Devkare100% (1)
- Chapter 6 Coding and Billing Basics PDFDocument33 pagesChapter 6 Coding and Billing Basics PDFamruthkiranbabujiNo ratings yet
- Adeel Khan: Contacts DetailsDocument2 pagesAdeel Khan: Contacts DetailszarartahirNo ratings yet
- Advanced 20 Medical 20 Coding 20 Case 20 Studies 20 Answers 20 KeyDocument4 pagesAdvanced 20 Medical 20 Coding 20 Case 20 Studies 20 Answers 20 KeynerdinaNo ratings yet
- David's CPNE NotesDocument21 pagesDavid's CPNE Notesdbryant0101100% (14)
- Module 3. Topical Outline and ReadingsDocument5 pagesModule 3. Topical Outline and Readingsapi-350882100No ratings yet
- Neonatal Disease Severity Scoring SystemsDocument6 pagesNeonatal Disease Severity Scoring Systemsida ayu agung WijayantiNo ratings yet
- Icd 10Document4 pagesIcd 10Radhika ShahNo ratings yet
- CMA Case ScenarioDocument3 pagesCMA Case ScenarioMitali SharmaNo ratings yet
- Irjet V6i31160Document7 pagesIrjet V6i31160Ananya DhuriaNo ratings yet
- 622 2267 1 PBDocument10 pages622 2267 1 PBNanda FallaNo ratings yet
- Missidentificaton of PatientsDocument5 pagesMissidentificaton of PatientsLuís Filipe Fernandes MendesNo ratings yet
- What Exactly Is Medical CodingDocument4 pagesWhat Exactly Is Medical CodingSusan FNo ratings yet
- Comp9 Unit4b Audio TranscriptDocument9 pagesComp9 Unit4b Audio TranscriptP D SpencerNo ratings yet
- Auditing Guidelines For Success: Why Am I Getting Audited?Document10 pagesAuditing Guidelines For Success: Why Am I Getting Audited?Chris DubuqueNo ratings yet
- Coding For SurgeonDocument379 pagesCoding For SurgeonLiza Fathiariani100% (1)
- Icd 10 Webinar Anatomy and PhsyiologyDocument47 pagesIcd 10 Webinar Anatomy and PhsyiologyJeswin JoseNo ratings yet
- An Expert System Using Nonmonotonic Techniques For Benets Inquiry in The Insurance IndustryDocument7 pagesAn Expert System Using Nonmonotonic Techniques For Benets Inquiry in The Insurance IndustrypostscriptNo ratings yet
- Performance Improvement Article HFM 12-06Document5 pagesPerformance Improvement Article HFM 12-06McKesson CorporationNo ratings yet
- Acccenture Implementing ICD10 To Achieve High PerformanceDocument8 pagesAcccenture Implementing ICD10 To Achieve High PerformanceshyamchepurNo ratings yet
- Apollo Hospitals Customer Experience ManagementDocument31 pagesApollo Hospitals Customer Experience Managementsreeram kNo ratings yet
- The Three Rs of Medical Quality: Reminder, Record and ReviewDocument3 pagesThe Three Rs of Medical Quality: Reminder, Record and ReviewJerlonNo ratings yet
- Mbacc Ebook Full PagesDocument115 pagesMbacc Ebook Full Pagesclaire m cook100% (4)
- 10.1515 - JPM 2022 0014Document9 pages10.1515 - JPM 2022 0014Bianca Maria PricopNo ratings yet
- P1337420617058 - Citraningrum Putri K - TUGAS MANKEP - RKIDocument49 pagesP1337420617058 - Citraningrum Putri K - TUGAS MANKEP - RKIMade Arya KarangNo ratings yet
- Icd-10 Basics Medical PracticesDocument2 pagesIcd-10 Basics Medical PracticesBrandi TadlockNo ratings yet
- Jurnal Ketepatan Kode Ketileng PDFDocument14 pagesJurnal Ketepatan Kode Ketileng PDFDiah Ayu KartikasariNo ratings yet
- 9 Key Radiology Medical Coding Tips For CodersDocument4 pages9 Key Radiology Medical Coding Tips For Codersayesha100% (1)
- Communication and Documentation For An Ambulatory Practice PDFDocument25 pagesCommunication and Documentation For An Ambulatory Practice PDFSanti Galang GuadesNo ratings yet
- Beginning EmploymentDocument6 pagesBeginning EmploymentAnitha SuprionoNo ratings yet
- Principles of ICD 10 Coding PDFDocument473 pagesPrinciples of ICD 10 Coding PDFSheilla Rismadwita100% (9)
- EU Prep Changing Notified Bodies Whitepaper EMERGO PDFDocument9 pagesEU Prep Changing Notified Bodies Whitepaper EMERGO PDFHiral PatelNo ratings yet
- Meng - 2020 - J. - Phys. - Conf. - Ser. - 1601 - 052016Document7 pagesMeng - 2020 - J. - Phys. - Conf. - Ser. - 1601 - 052016Jamal AhmedNo ratings yet
- 4 Coding and Payment Opportunities You Might Be MissingDocument6 pages4 Coding and Payment Opportunities You Might Be MissingariskaNo ratings yet
- Special Requirements of Electronic Medical Record Systems in Obstetrics and GynecologyDocument4 pagesSpecial Requirements of Electronic Medical Record Systems in Obstetrics and GynecologysayansambitNo ratings yet
- Medicare Audit Defense StrategiesDocument24 pagesMedicare Audit Defense StrategiesEdward M RocheNo ratings yet
- Nursing Info Week 5 - Final ProjectDocument9 pagesNursing Info Week 5 - Final Projectapi-458308352No ratings yet
- Beeben Russell, Platinum Biologics, Scott Martin, Marcus RusselDocument1 pageBeeben Russell, Platinum Biologics, Scott Martin, Marcus RusselseenfgNo ratings yet
- 10 Reasons To Own EM Code CheckDocument26 pages10 Reasons To Own EM Code Checkadultmedicalconsultants100% (1)
- Assg Codingcasestudies 20171109 Ah102 - 1Document2 pagesAssg Codingcasestudies 20171109 Ah102 - 1api-430615583No ratings yet
- 2016 May June Aftercare Vs Follow UpDocument3 pages2016 May June Aftercare Vs Follow UpHarsha VipinNo ratings yet
- Article Patient Identification ErrorsDocument4 pagesArticle Patient Identification ErrorssalsabilahnaaNo ratings yet
- Drug Safety Surveillance Using De-Identified EMR and Claims Data: Issues and ChallengesDocument4 pagesDrug Safety Surveillance Using De-Identified EMR and Claims Data: Issues and ChallengesRitesh KumarNo ratings yet
- 34 CueDocument6 pages34 Cuejim912No ratings yet
- Medical Coding 101: Boost Your CareerDocument19 pagesMedical Coding 101: Boost Your CareerSupercoder67% (3)
- Medicare Audit Defense StrategiesDocument24 pagesMedicare Audit Defense StrategiesEdward M RocheNo ratings yet
- Nejmp 1215594Document4 pagesNejmp 1215594Cj AlmazanNo ratings yet
- A Meta-Embedding-Based Ensemble Approach For ICD Coding PredictionDocument13 pagesA Meta-Embedding-Based Ensemble Approach For ICD Coding PredictionTudor MicuNo ratings yet
- What Exactly Is Medical CodingDocument5 pagesWhat Exactly Is Medical CodingSnehaNo ratings yet
- ICD 10MythsandFacts11Document4 pagesICD 10MythsandFacts11Dhsc01No ratings yet
- Practice Management IntergrationDocument5 pagesPractice Management Intergrationthe mad king readerNo ratings yet
- Sop Clinical PathwayDocument7 pagesSop Clinical Pathwaypmkp rsud subangNo ratings yet
- Standardized Nursing TerminologyDocument5 pagesStandardized Nursing TerminologyDaniel WainainaNo ratings yet
- NASKAH PUBLIKASI 1,5 (Bahasa Inggris)Document15 pagesNASKAH PUBLIKASI 1,5 (Bahasa Inggris)yuyunNo ratings yet
- Medical BillingDocument229 pagesMedical BillingMohammad Apzar100% (6)
- A few minutes to improve Risk documentation Accuracy even when you know nothing about Medicare Risk AdjustmentFrom EverandA few minutes to improve Risk documentation Accuracy even when you know nothing about Medicare Risk AdjustmentNo ratings yet
- Battaglia Lubchenco1967Document5 pagesBattaglia Lubchenco1967Franco Darío Della FontanaNo ratings yet
- Daftar PustakaDocument1 pageDaftar PustakaRocking ChairNo ratings yet
- Fluconazole Resistance in Candida Albicans: A Review of MechanismsDocument9 pagesFluconazole Resistance in Candida Albicans: A Review of MechanismsRocking ChairNo ratings yet
- ESGO Cervical-Cancer A6 PDFDocument48 pagesESGO Cervical-Cancer A6 PDFRocking ChairNo ratings yet
- Cotton Buyers Guide 2017Document48 pagesCotton Buyers Guide 2017Rocking ChairNo ratings yet
- Cotton Buyers Guide 2017Document48 pagesCotton Buyers Guide 2017Rocking ChairNo ratings yet
- Fluconazole Resistance in Candida Albicans: A Review of MechanismsDocument9 pagesFluconazole Resistance in Candida Albicans: A Review of MechanismsRocking ChairNo ratings yet
- Education and Attitudes Towards The EnvironmentDocument24 pagesEducation and Attitudes Towards The EnvironmentRocking ChairNo ratings yet
- Fiche 54 - Plaquette MASTER - Sciences Du VivantDocument2 pagesFiche 54 - Plaquette MASTER - Sciences Du VivantRocking ChairNo ratings yet
- Master Program - Cardiovascular Science - Göttingen - Registration FormDocument2 pagesMaster Program - Cardiovascular Science - Göttingen - Registration FormRocking ChairNo ratings yet
- Application Form For Master Program CARDIOVASCULAR SCIENCE: Emillyasari@student - Uns.ac - IdDocument1 pageApplication Form For Master Program CARDIOVASCULAR SCIENCE: Emillyasari@student - Uns.ac - IdRocking ChairNo ratings yet
- BackgroundDocument1 pageBackgroundRocking ChairNo ratings yet
- Prof Ram Charan Awards Brochure2020 PDFDocument5 pagesProf Ram Charan Awards Brochure2020 PDFSubindu HalderNo ratings yet
- Jfif 1.02Document9 pagesJfif 1.02Berry Hoekstra100% (1)
- Budgetary ControlsDocument2 pagesBudgetary Controlssiva_lordNo ratings yet
- Os PPT-1Document12 pagesOs PPT-1Dhanush MudigereNo ratings yet
- April 26, 2019 Strathmore TimesDocument16 pagesApril 26, 2019 Strathmore TimesStrathmore Times100% (1)
- Tigo Pesa Account StatementDocument7 pagesTigo Pesa Account StatementPeter Ngicur Carthemi100% (1)
- 2nd Pornhub Awards - WikipediaaDocument13 pages2nd Pornhub Awards - WikipediaaParam SinghNo ratings yet
- Inside Animator PDFDocument484 pagesInside Animator PDFdonkey slapNo ratings yet
- 17BCE0552 Java DA1 PDFDocument10 pages17BCE0552 Java DA1 PDFABHIMAYU JENANo ratings yet
- Numerical Methods Chapter 10 SummaryDocument8 pagesNumerical Methods Chapter 10 SummarynedumpillilNo ratings yet
- Disaster Management Plan 2018Document255 pagesDisaster Management Plan 2018sifoisbspNo ratings yet
- Rubber Chemical Resistance Chart V001MAR17Document27 pagesRubber Chemical Resistance Chart V001MAR17Deepak patilNo ratings yet
- ServiceDocument47 pagesServiceMarko KoširNo ratings yet
- Service and Maintenance Manual: Models 600A 600AJDocument342 pagesService and Maintenance Manual: Models 600A 600AJHari Hara SuthanNo ratings yet
- Propiedades Grado 50 A572Document2 pagesPropiedades Grado 50 A572daniel moreno jassoNo ratings yet
- Honda Wave Parts Manual enDocument61 pagesHonda Wave Parts Manual enMurat Kaykun86% (94)
- Simply Put - ENT EAR LECTURE NOTESDocument48 pagesSimply Put - ENT EAR LECTURE NOTESCedric KyekyeNo ratings yet
- Olympics Notes by Yousuf Jalal - PDF Version 1Document13 pagesOlympics Notes by Yousuf Jalal - PDF Version 1saad jahangirNo ratings yet
- STAT455 Assignment 1 - Part ADocument2 pagesSTAT455 Assignment 1 - Part AAndyNo ratings yet
- En dx300lc 5 Brochure PDFDocument24 pagesEn dx300lc 5 Brochure PDFsaroniNo ratings yet
- Case StudyDocument2 pagesCase StudyBunga Larangan73% (11)
- Gas Dehydration (ENGINEERING DESIGN GUIDELINE)Document23 pagesGas Dehydration (ENGINEERING DESIGN GUIDELINE)Tu Dang TrongNo ratings yet
- The Impact of School Facilities On The Learning EnvironmentDocument174 pagesThe Impact of School Facilities On The Learning EnvironmentEnrry Sebastian71% (31)
- Astera Data Integration BootcampDocument4 pagesAstera Data Integration BootcampTalha MehtabNo ratings yet
- Sentinel 2 Products Specification DocumentDocument510 pagesSentinel 2 Products Specification DocumentSherly BhengeNo ratings yet
- Exercises 6 Workshops 9001 - WBP1Document1 pageExercises 6 Workshops 9001 - WBP1rameshqcNo ratings yet
- Decision Maths 1 AlgorithmsDocument7 pagesDecision Maths 1 AlgorithmsNurul HafiqahNo ratings yet
- CMC Ready ReckonerxlsxDocument3 pagesCMC Ready ReckonerxlsxShalaniNo ratings yet
- House Rules For Jforce: Penalties (First Offence/Minor Offense) Penalties (First Offence/Major Offence)Document4 pagesHouse Rules For Jforce: Penalties (First Offence/Minor Offense) Penalties (First Offence/Major Offence)Raphael Eyitayor TyNo ratings yet