Professional Documents
Culture Documents
COPD Notes
Uploaded by
jisooOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
COPD Notes
Uploaded by
jisooCopyright:
Available Formats
NCLEX Review on COPD The name “blue bloaters” is due
to cyanosis from “hypoxia” and bloating from
Definition: pulmonary disease that causes edema AND increase in lung volume. The
chronic obstruction of airflow from the lungs bloating is from the effects of the lung disease
Keys Point for COPD: on the heart which causes right-sided heart
failure.
Limited Airflow (due to thick and
swollen bronchioles that have
become deformed with excessive
sputum production and this narrows
the airways)
Inability to fully exhale (due to
loss of elasticity of the alveoli sacs
from damage and the sacs start to
develop air pockets)
Irreversible once developed…cases
vary among people from mild to
severe…managed with lifestyle
changes and medications.
Happens gradually….most people
start to notice signs and symptoms
middle-aged and will present with
dyspnea with activity they could
normally tolerate, recurrent lung
infections, chronic cough etc. In chronic bronchitis, the bronchioles become
COPD is a term used as a “catch damaged that leads them to be thick and swollen
all” for diseases that limit airflow and deformed. This is accompanied by more
and cause dyspnea. sputum production. This limits the ability of the
Types of COPD include:
person being able to completely exhale the air
taken in. So, when they take another breath in, it
Emphysema “pink puffers”
Chronic bronchitis “blue bloaters” will increase the air volume even more (because
they have retained air from the previous breath),
Pathophysiology of COPD and this leads to hyperinflation.
Normal breathing: Also, less oxygen is getting into the blood and more
Inhaled oxygen travels down through the carbon dioxide is staying in the blood. This leads to
trachea which splits at the carina into bronchial low blood levels and high carbon dioxide levels.
tubes starting with the primary bronchus then Patients will have cyanosis due to a decreased
into smaller airways called secondary and oxygen level. To compensate, the body increases
tertiary bronchi which divide into bronchioles
RBC production and cause blood to shift elsewhere
and the oxygen goes into the alveolar sacs
which increases pressure in the pulmonary artery
where gas exchange happens. As the alveoli
inflate and deflate with ease, inhaled oxygen leading to pulmonary hypertension. Pulmonary
attaches to the red blood cells and carbon hypertension leads to right-sided heart failure
dioxide enters the respiratory system to be (which is why you will start to see bloating..edema
exhaled. in the abdomen and legs)
In conditions such as emphysema “pink puffers”:
What happens in breathing with COPD?
In conditions such as chronic bronchitis The name comes from hyperventilation (puffing to
“blue bloaters”: breathe) and pink complexion (they maintain a
relatively normal oxygen level due to rapid Anteroposterior diameter increased (barrel
breathing) rather than cyanosis as in chronic chest)….emphysema “pink puffers”
bronchitis. Gets in the Tripod Position during dyspnea (stands
In emphysema, the alveoli sacs lose their ability to leaning forward while supporting body with hands
inflate and deflate due to an inflammatory on knees or an object)
response in the body. So, the sac is unable to Extreme dyspnea
properly deflate and inflate. Inhaled air starts to
get trapped in the sacs and this causes major In turn over time, people with COPD will be
hyperinflation of the lungs because the patient is stimulated to breathe due to low oxygen levels
retaining so much volume. RATHER than high carbon dioxide levels.
Hyperinflation causes the diaphragm to flatten.
The diaphragm plays a huge role in helping the Complications of COPD
patient breathe effortlessly in and out. Therefore, Heart Disease (remember heart and lungs
in order to fully exhale, the patient starts to work together in replenishing the body with
hyperventilate and use accessory muscles to get oxygen)…heart failure
the air out now. This leads to the barrel chest look
Pneumothorax (spontaneous due to
and during inspect it may be noted there is an
forming of air sacs)
INCREASED ANTEROPOSTERIOR DIAMETER.
Risk for Pneumonia
The damage in the sacs cause the body to keep
Cancer (especially lung)
high carbon dioxide levels and low blood oxygen
levels. Inhaled oxygen will not be able to enter into How is COPD Diagnosed?
the sacs for gas exchange and carbon dioxide won’t Spirometry: A test where a patient breathes into a
leave the cells to be exhaled. tube that measure how much volume the lungs can
The body tries to compensate by causing hold during inhalation and how much and fast air
hyperventilation (increasing the respiratory volume is exhaled.
rate…hence puffer) and the patient will have less Measuring the FVC (Forced Vital Capacity):
hypoxemia “pink complexion” than chronic a low reading shows restrictive
bronchitis who have the cyanosis because pink breathing….it measures the largest amount
puffers keep their oxygen level just where it needs of air a person exhales after breathing in
to be from hyperventilation. deeply in one second.
Forced Expiratory Volume: measures how
Signs & Symptoms of COPD much air a person can exhale within one
second. A low reading shows the severity of
Remember: Lung Damage
the disease.
Lack of energy Nursing Interventions for COPD
Unable to tolerate activity (shortness of breath) Monitor Respiratory System:
Nutrition poor (weight loss) due to energy used
breathing especially with emphysema Assess lung sounds (may need suction) and
Gases abnormal (high PCO2 >45 and low PO2 sputum production…obtain a culture if
<90)..respiratory acidosis ordered…at risk for pneumonia
Dry or productive cough constant (productive with Keep oxygen saturation (88%-93%) why
chronic bronchitis) between this range?
Accessory muscle usage during breathing, Patients with COPD are stimulated to
Abnormal lung sounds: diminished, coarse crackles breathe due to LOW OXYGEN SATURATION
(chronic bronchitis) or wheezing rather than high carbon dioxide
Modification of skin color from pink to cyanosis in levels….which is the opposite for people for
lips, mucous membranes, nail beds (“blue healthy lungs. If they are given too much
bloaters”) oxygen it will reduce their need to
breathe…causing hypoventilation and Corticosteroids: decreases inflammation and
carbon dioxide levels will increase to toxic mucous production in airway… given: oral, IV,
levels. inhaled and used in combination with
Given oxygen as prescribed in low amounts bronchodilator like:
1-2 liters
Monitor effort of breathing and teach about Symbicort: combination of steroid and long acting
pursed-lip and diaphragmatic breathing bronchodilator
Pursed-lip breathing: used for when patient Other corticosteroids: Prednisone, Solu-medrol,
starts to get dyspneic. This technique Pulmicort
increases the oxygen level and encourages Side effects: easy bruising, hyperglycemia, risk of
them to breath out longer (remember these infection, bone problems (long term use)
patient don’t fully exhale very well). It is Patient education: rinse mouth after using inhaled
similar to like blowing out a birthday corticosteroids…can develop thrush, use
candle. corticosteroid inhaler AFTER using bronchodilator
Diaphragmatic breathing: uses abdominal inhaler
muscles for breathing rather than accessory Methylxanthines: Theophylline (most commonly
muscles helps make diaphragm stronger given orally) type of bronchodilator used long term
which is weak slows down breathing rate to in patients who have severe COPD
allow breathing to be easier decreases
energy used to breathe used along with Remember: Narrow therapeutic range of
pursued breathing technique 10 to 20 mcg/mL
Administering breathing treatments as Increases risk for digoxin toxicity and
needed: bronchodilators, nebulizer etc. decreases the effects of lithium and Dilantin
Respiratory therapy helps play a role in this Phosphodiestrace-4 inhibitors: “Roflumilast” used
as well (medications are discussed in more for people who have chronic bronchitis and it
detail below) works by decreasing COPD exacerbation…not a
Patient Education for COPD bronchodilator
Side effects: can cause suicidal thoughts
Nutrition needs: eating high calorie, protein
(remember the word “last” in the drug’s
rich meals that are small but frequent and
name…it could be the patient’s last days if
staying hydrated if not
they are not assessed for this side effect)
contraindicated….avoid large heavy meals
and can cause weight loss.
due to compression on the lungs from the
Short-acting bronchodilators: relaxes the smooth
stomach
muscle of the bronchial tubes and are used in
Avoiding sick people, irritants, hot humid
emergency situations where quick relief is needed
(smothering) or very cold weather
Albuterol (beta 2 agonist) and Atrovent
Stop smoking or being around people who
(anticholinergic)
smoke
Long-acting Bronchodilators: relaxes the smooth
Vaccination up-to-date: annual flu shot and
muscle of the bronchial tubes (same as short-acting
Pneumovax every 5 years because it is very
bronchodilators BUT their effects last longer) used
hard for people with COPD to recover from
over a longer period of time….taken once or twice
illnesses
a day
Pursed lip and diaphragmatic breathing
Beta 2 agonist: salmeterol, anticholinergics:
techniques
Spiriva
Administering medications: be familiar with
Patient education: let them know which
groups, side effects, and patient teaching
drug is short and long-acting, how to use
Medication Regime for COPD inhaler and to use bronchodilator inhaler
Remember the mnemonic: Chronic Pulmonary
Medications Save Lungs
BEFORE steroid inhaler (wait 5 minutes in
between)
WHY? TO OPEN UP THE AIRWAYS SO THE
STEROID CAN GET IN THERE AND DO ITS
JOB
Side effects of beta 2 agonist: increased
heart rate, urinary retention
Side effects of anticholinergic: dry mouth,
blurred vision
You might also like
- Congenital Heart DiseasesDocument14 pagesCongenital Heart DiseasesEulane Ferrer100% (1)
- Fluid and ElectrolyteDocument66 pagesFluid and ElectrolyteMoni Mbumba Meleke100% (1)
- CardiomyopathyDocument2 pagesCardiomyopathyBianca SarmientoNo ratings yet
- Bulimia NervosaDocument13 pagesBulimia Nervosaemlyn_lanonNo ratings yet
- Disturbances in OxygenationDocument10 pagesDisturbances in OxygenationjenrylNo ratings yet
- Drug study nursing considerationsDocument9 pagesDrug study nursing considerationsDaryl TabefrancaNo ratings yet
- Altered Level of ConsciousnessDocument11 pagesAltered Level of ConsciousnessRamji PaudelNo ratings yet
- Week 2 Electrolyte Imbalance Group Work INSTRUCTOR 1 PDFDocument8 pagesWeek 2 Electrolyte Imbalance Group Work INSTRUCTOR 1 PDFMaica LectanaNo ratings yet
- II. Anatomy and PhysiologyDocument16 pagesII. Anatomy and PhysiologyLee Cel100% (1)
- Acute Respiratory Distress Syndrome (ARDS) Causes, Symptoms, TreatmentDocument2 pagesAcute Respiratory Distress Syndrome (ARDS) Causes, Symptoms, Treatmentmanish086No ratings yet
- 3136 - OA - Motivation Among Nurses PDFDocument6 pages3136 - OA - Motivation Among Nurses PDFShahnaz DarNo ratings yet
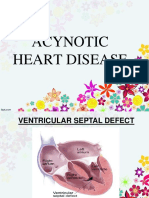
- Acynotic DiseaseDocument55 pagesAcynotic DiseaseTesfamichael AbathunNo ratings yet
- Alexithymia ArticleDocument14 pagesAlexithymia ArticleDomingo MosqueraNo ratings yet
- Antibiotic Prescribing in Primary Care - Therapeutic Guidelines Summary Table 2019Document2 pagesAntibiotic Prescribing in Primary Care - Therapeutic Guidelines Summary Table 2019RL100% (1)
- Fluid Volume Deficit R/T Diarrhea & VomitingDocument4 pagesFluid Volume Deficit R/T Diarrhea & Vomitingjisoo100% (3)
- Chronic Obstructive Pulmonary DiseaseDocument18 pagesChronic Obstructive Pulmonary DiseaseMaryam BajwaNo ratings yet
- Insulin AdministrationDocument15 pagesInsulin Administrationmec17No ratings yet
- EmphysemaDocument2 pagesEmphysemaGeorley LobridoNo ratings yet
- PSYCHE FINALS: SIGNS OF DEPRESSIONDocument10 pagesPSYCHE FINALS: SIGNS OF DEPRESSIONjisooNo ratings yet
- Icu Equipments BY: Presented Bhupender Kumar MehtoDocument35 pagesIcu Equipments BY: Presented Bhupender Kumar Mehtobhupendermehto012No ratings yet
- Diseases of Poultry A Colour AtlasDocument213 pagesDiseases of Poultry A Colour AtlasShakil Mahmod100% (1)
- Multiple Organ Dysfunction SyndromeDocument4 pagesMultiple Organ Dysfunction SyndromeJenny SisonNo ratings yet
- Patent Ductus ArteriosusDocument5 pagesPatent Ductus ArteriosusAisyahKautsarIlmiNo ratings yet
- Case Press Medical WardDocument29 pagesCase Press Medical WardivanloveschieNo ratings yet
- Acid Base AnswersDocument4 pagesAcid Base Answersapi-232466940No ratings yet
- Polycythemia Vera CompletedDocument5 pagesPolycythemia Vera CompletedSaro BalberanNo ratings yet
- Food Safety Checklist: Personal HygieneDocument3 pagesFood Safety Checklist: Personal Hygienejisoo100% (8)
- Central Venous Access DevicesDocument6 pagesCentral Venous Access DevicesAllan MacacapagalNo ratings yet
- Chronic Kidney DiseaseDocument7 pagesChronic Kidney DiseaseLardel Balbiran LafortezaNo ratings yet
- Cesarean BirthDocument3 pagesCesarean BirthAijem RyanNo ratings yet
- Acute Respiratory Distress Syndrome (ARDS) : MR Sanjay. M. Peerapur, Principal, KLES Institute of Nursing Sciences, HubliDocument22 pagesAcute Respiratory Distress Syndrome (ARDS) : MR Sanjay. M. Peerapur, Principal, KLES Institute of Nursing Sciences, Hublimanish dafdaNo ratings yet
- Blood Transfusion ReactionDocument9 pagesBlood Transfusion ReactionReema Akberali nooraniNo ratings yet
- Nursing Process OverviewDocument11 pagesNursing Process OverviewJoanne CareahNo ratings yet
- EmphysemaDocument40 pagesEmphysemaJulienne Sanchez-SalazarNo ratings yet
- Types of Drug Preparation and AdministrationDocument5 pagesTypes of Drug Preparation and AdministrationZam Pamate100% (1)
- Endokarditis, Miokarditis Perikarditis: Blok KardiovaskularDocument31 pagesEndokarditis, Miokarditis Perikarditis: Blok KardiovaskularTiara RamliNo ratings yet
- First Semester 2020-2021 Study Guide: University of The CordillerasDocument13 pagesFirst Semester 2020-2021 Study Guide: University of The CordillerasJonalyn EtongNo ratings yet
- Pathophysiology ARDSDocument2 pagesPathophysiology ARDSKim AmboyaNo ratings yet
- Antepartum PeriodDocument3 pagesAntepartum PeriodjisooNo ratings yet
- Abg Analysis NotesDocument32 pagesAbg Analysis Notesakheel ahammedNo ratings yet
- Respiratory Failure (1) .Document36 pagesRespiratory Failure (1) .Ibrahim HemdanNo ratings yet
- Acute Respiratory Distress SyndromeDocument17 pagesAcute Respiratory Distress SyndromeSherree Hayes100% (2)
- ORIF Surgery for Bone FracturesDocument24 pagesORIF Surgery for Bone FracturesSusie PadaoanNo ratings yet
- 13.acute Respiratory FailureDocument34 pages13.acute Respiratory Failurekarim hassan100% (1)
- Terminal Performance Objective:: Plan of Activities (Guiwan Health Center)Document5 pagesTerminal Performance Objective:: Plan of Activities (Guiwan Health Center)jisoo100% (2)
- ARDSDocument57 pagesARDSnesjohnvNo ratings yet
- Medical Surgical Nursing Suretech College of NursingDocument18 pagesMedical Surgical Nursing Suretech College of NursingSanket TelangNo ratings yet
- Bronchial AsthmaDocument95 pagesBronchial AsthmaBrian BrownNo ratings yet
- Kidney Transplantation: Group 9 Syazwaniyati Nurulasmira Nur Hamiza Siti NursuhadaDocument12 pagesKidney Transplantation: Group 9 Syazwaniyati Nurulasmira Nur Hamiza Siti NursuhadaSiti Nursuhada binti Mohd AminNo ratings yet
- Right Sided Heart FailureDocument33 pagesRight Sided Heart FailurePaulNo ratings yet
- TracheostomyDocument4 pagesTracheostomyJyothiNo ratings yet
- Testing Placement of Nasogastric Tubes in Infants & ChildrenDocument4 pagesTesting Placement of Nasogastric Tubes in Infants & ChildrenYwagar YwagarNo ratings yet
- Acute Respiratory Distress SyndromeDocument10 pagesAcute Respiratory Distress Syndromealina abu rumiNo ratings yet
- PneumoniaDocument8 pagesPneumoniaNader Smadi100% (2)
- Competency-Based Training in Basic Emergency Obstetric and Newborn Care (BEmONC) Improves Provider's Performance in TanzaniaDocument16 pagesCompetency-Based Training in Basic Emergency Obstetric and Newborn Care (BEmONC) Improves Provider's Performance in TanzaniaJhpiego100% (2)
- Sputum ExamDocument14 pagesSputum ExamJuan MorseNo ratings yet
- Nursing Management-DirectingDocument31 pagesNursing Management-DirectingFrancis Anthony LoslosoNo ratings yet
- Anatomy & PhysiologyDocument9 pagesAnatomy & Physiologyrachael80% (5)
- Septic Shock: Supervisor: DR Ali Haedar, Sp. EM FAHA Dinisa Novaurahmah Nanin Aprilia PutriDocument42 pagesSeptic Shock: Supervisor: DR Ali Haedar, Sp. EM FAHA Dinisa Novaurahmah Nanin Aprilia PutriMutia Larasati AlbarNo ratings yet
- Pathophysiology of Acute CholecystitisDocument2 pagesPathophysiology of Acute CholecystitisKush KhannaNo ratings yet
- Anemia Anemia Describes The Condition in Which The Number of Red Blood Cells in The Blood Is Low. Probability & StatisticsDocument7 pagesAnemia Anemia Describes The Condition in Which The Number of Red Blood Cells in The Blood Is Low. Probability & StatisticsSahara GalayNo ratings yet
- Syndrome of Inappropriate Secretion of Anti Diuretic HormoneDocument39 pagesSyndrome of Inappropriate Secretion of Anti Diuretic Hormonefarmasi_hmNo ratings yet
- Test - Management 443 Chapter 5 - QuizletDocument3 pagesTest - Management 443 Chapter 5 - Quizletايهاب غزالةNo ratings yet
- Arterial Blood Gas (ABG) Analysis: Measuring Acid-Base BalanceDocument8 pagesArterial Blood Gas (ABG) Analysis: Measuring Acid-Base BalanceprecillathoppilNo ratings yet
- Septic ShockDocument16 pagesSeptic ShockGelo JvrNo ratings yet
- Managing a Patient with Metastatic Breast CancerDocument3 pagesManaging a Patient with Metastatic Breast Cancerjoseph nga'ng'ahNo ratings yet
- PneumoniaDocument71 pagesPneumoniafrancis00090100% (1)
- Case Study ThrombocytopeniaDocument8 pagesCase Study ThrombocytopeniaAmina TariqNo ratings yet
- Chronic Renal FailureDocument28 pagesChronic Renal FailurePatricia Nadine Sarcadio NeffeNo ratings yet
- Core Competencies in Nursing-1Document11 pagesCore Competencies in Nursing-1yakapmNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Copd NotesDocument11 pagesCopd NotesAgnes Jeane EnriquezNo ratings yet
- Gender and Mental HealthDocument20 pagesGender and Mental HealthjisooNo ratings yet
- Basic Concepts On PsychopharmacologyDocument47 pagesBasic Concepts On PsychopharmacologyjisooNo ratings yet
- Social OrganizationDocument8 pagesSocial OrganizationjisooNo ratings yet
- Antibiotics: I - IntroductionDocument8 pagesAntibiotics: I - IntroductionjisooNo ratings yet
- Trematodes: I - IntroductionDocument4 pagesTrematodes: I - IntroductionjisooNo ratings yet
- History of Computers LectureDocument36 pagesHistory of Computers LecturejisooNo ratings yet
- Digital Citizenship: - Digital Life - Sharing On The InternetDocument66 pagesDigital Citizenship: - Digital Life - Sharing On The InternetjisooNo ratings yet
- Discovering Computers 2010 Living in a Digital WorldDocument43 pagesDiscovering Computers 2010 Living in a Digital WorldjisooNo ratings yet
- Nematodes: I - IntroductionDocument3 pagesNematodes: I - IntroductionjisooNo ratings yet
- Computer Basics: There Are Many Types of Computers IncludingDocument25 pagesComputer Basics: There Are Many Types of Computers Includingmountmalai07No ratings yet
- EARLY CHILDHOOD AND GENECOLOGY OF Jose P. RizalDocument15 pagesEARLY CHILDHOOD AND GENECOLOGY OF Jose P. RizaljisooNo ratings yet
- Liver and Billary DisordersDocument16 pagesLiver and Billary DisordersjisooNo ratings yet
- Care of Clients with Maladaptive Patterns of BehaviorDocument556 pagesCare of Clients with Maladaptive Patterns of BehaviorjisooNo ratings yet
- Endocrine DisordersDocument26 pagesEndocrine DisordersjisooNo ratings yet
- NCM 105 Unit 5-Somatoform-Dissociative-Sleep 2Document93 pagesNCM 105 Unit 5-Somatoform-Dissociative-Sleep 2jisooNo ratings yet
- Prenatal, Labor, Delivery and Postpartum CareDocument3 pagesPrenatal, Labor, Delivery and Postpartum Carejisoo100% (1)
- NeuroassessDocument92 pagesNeuroassessjisooNo ratings yet
- Common Health Issues in AdolescenceDocument250 pagesCommon Health Issues in AdolescencejisooNo ratings yet
- Maternal Health: Pregnancy Signs and StagesDocument9 pagesMaternal Health: Pregnancy Signs and StagesjisooNo ratings yet
- PSYCHE FINALS: TRANS 2Document4 pagesPSYCHE FINALS: TRANS 2jisooNo ratings yet
- Cranial Nerve Test Cranial Nerve I: OlfactoryDocument2 pagesCranial Nerve Test Cranial Nerve I: OlfactoryjisooNo ratings yet
- Overview of Child HealthDocument81 pagesOverview of Child HealthSamer FarhanNo ratings yet
- Anatomy Reproductive SystemDocument8 pagesAnatomy Reproductive SystemjisooNo ratings yet
- Gastroentritis Study of Illness ConditionDocument2 pagesGastroentritis Study of Illness ConditionjisooNo ratings yet
- DR Natsir SPPD KR Painful JointDocument41 pagesDR Natsir SPPD KR Painful JointSITI BINTA MASYKURINNo ratings yet
- Hemartrosis PPT EnglishDocument27 pagesHemartrosis PPT EnglishAri SamadNo ratings yet
- Pathology of Diabetic Ketoacidosis - Romeo Rivera Jr.Document1 pagePathology of Diabetic Ketoacidosis - Romeo Rivera Jr.romeo riveraNo ratings yet
- Childhood Disorders & SchizophreniaDocument25 pagesChildhood Disorders & SchizophreniaMaJoy OrdoñezNo ratings yet
- GLIMITAB M-1/GLIMITAB M-2 Tablets: CompositionDocument6 pagesGLIMITAB M-1/GLIMITAB M-2 Tablets: Compositiongaurav7augNo ratings yet
- Background: Historical NoteDocument8 pagesBackground: Historical NoteEvan Folamauk0% (1)
- Medical-Surgical Nursing Care: Caring For Clients With Diabetes MellitusDocument90 pagesMedical-Surgical Nursing Care: Caring For Clients With Diabetes MellitusJonalynCollodChewacheoNo ratings yet
- Diet Analysis ProjectDocument7 pagesDiet Analysis ProjectBrittany DiamondGurl ColbertNo ratings yet
- Long Cases ADocument24 pagesLong Cases Amieraf mesfinNo ratings yet
- Muscular Dystrophy-Olivia (Autosaved)Document14 pagesMuscular Dystrophy-Olivia (Autosaved)Aaron James GrayNo ratings yet
- Inake Forms AJD Complete Nov 07 - Rev 09072009Document19 pagesInake Forms AJD Complete Nov 07 - Rev 09072009adruckerNo ratings yet
- Human Osteology at Wharram PercyDocument2 pagesHuman Osteology at Wharram PercyMichael Lovejoy100% (1)
- مهم للمزاولةDocument13 pagesمهم للمزاولةbelal nurseNo ratings yet
- CARDIOVASCULAR EXAM GUIDEDocument30 pagesCARDIOVASCULAR EXAM GUIDEsnowlover boyNo ratings yet
- F 2433 CMED Saxagliptin A Selective DPP 4 Inhibitor For The Treatment of Type 2 D.PDF 3311Document12 pagesF 2433 CMED Saxagliptin A Selective DPP 4 Inhibitor For The Treatment of Type 2 D.PDF 3311Ridha Surya NugrahaNo ratings yet
- Adjectives 2Document3 pagesAdjectives 2arlindo machavaNo ratings yet
- rnpedia-mcn-pnle-naDocument30 pagesrnpedia-mcn-pnle-naFrances Sofia DuranNo ratings yet
- Effectiveness of Orange Peelings As Insect Repellent: Mark Anthony Paul Borabo Jonard Estrallado Raff QuillosDocument4 pagesEffectiveness of Orange Peelings As Insect Repellent: Mark Anthony Paul Borabo Jonard Estrallado Raff QuillosAoki kazeNo ratings yet
- Nutritional Strategies in Acute PancreatitisDocument19 pagesNutritional Strategies in Acute PancreatitisSyed Irfan ArifNo ratings yet
- Portal Hypertension Pathogenesis and Diagnosis PDFDocument15 pagesPortal Hypertension Pathogenesis and Diagnosis PDFLizeth GirónNo ratings yet
- Integumentary PT AssessmentDocument12 pagesIntegumentary PT AssessmentkumaninaNo ratings yet
- Reviews: Microbiome-Based TherapeuticsDocument16 pagesReviews: Microbiome-Based TherapeuticsMyM ConstructoresNo ratings yet
- Pinyin Dictionary M To e A5c1Document237 pagesPinyin Dictionary M To e A5c1Zianaly JeffryNo ratings yet
- 21-Day Water Fast Detox Project ReportDocument12 pages21-Day Water Fast Detox Project ReportJayanth Bv100% (1)