Professional Documents
Culture Documents
Lower Extremity Presentation
Uploaded by
myokamaltaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lower Extremity Presentation
Uploaded by
myokamaltaCopyright:
Available Formats
A General Review of Lower Extremity Patient Presentation
(From Kids to the Weekend Warrior)
Presented by:
J. Alan Lovejoy, D.C., LCP, FICA
Sponsored by:
This course presents the philosophy and biomechanical approach to the evaluation
and adjustment of the extra-vertebral articulations of the body, with specific focus
on the lower extremities. Patient history, evaluation and analysis will focus on
general patient presentations in a ChiropracTic office. Emphasis is given to the
biomechanical impact on the body as a whole.
4 Part Harmony
The body was created with the innate ability to maintain “Health” and
overcome sickness and disease.
The nervous system controls and coordinates every function in the body
either directly or indirectly including the immune system.
Interference to the nervous system will cause dysfunction within the body.
Subluxations cause nervous interference; therefore, subluxations cause
dysfunction within the body.
Removal of nervous interference will allow the body’s innate ability to
restore health; therefore, correction of the subluxation will remove
interference to the nervous system, thereby, allowing the body to heal.
Where your Attitude goes
Your Energy flows and
That’s what Grows to
Become Manifest in
YOUR LIFE
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 1
Why Adjust Extremities?
A Brief History of Extra-Vertebral Adjusting
Hippocrates
On the Articulations
Written 400 B.C.E
Translated by Francis Adams http://classics.mit.edu/
Wrote mostly of dislocations but did refer to “slight displacement”
(sub-luxated) and fixing these was translated in some cases as
adjusted.
Also wrote of examination; comparing the bad to good.
Modern Day Bonesetter Practice ?
“Old Dad Chiro”
1st instance of DD adjusting a foot; A letter dated Sept. 10, 1896 Nellie
Richardson …adjusted the foot joints to relieve pain on the dorsal part
of her arch. (Keating et.al, 1992)
Referred the bonesetter Sweet adjusting Mrs. Garrison’s foot. (Palmer
& Palmer, 1906,pp.191)
“ The science of the cause of disease and the art of adjusting by hand
all subluxations of the 300 articulations of the skeletal frame.” (Palmer
& Palmer, 1906, Introduction)
Innovators and Techniques
Some Innovators:
Gonstead
States
Charrette
Broome
Faye
Hearon
Mally
Thompson
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 2
Some Techniques:
Gonstead-analysis & adjusting
Diversified
Charette’s Protocols
Activator
Thompson Drop Table
MPI-analysis & adjusting
Certifications:
Hearon-CCEP
Mally
A Few General Considerations:
Always relate back to the spine
Remember, an extremity does not have to be symptomatic.
History is a very important part of your Dx
Do active ROM before doing passive ROM
Take bilateral X-ray views
When adjusting extremities you need to:
Explain what you are doing
Be gentle with passive motion
Be specific with your contact
Be fast with your adjustment
Be sure you are at End Play
Be motivated and positive
Relate everything back to the spine
Be clear with any take home instructions
Optimal?Normal Joint Function
Painless movement of appendages through a complete range of
motion.
Proper distribution of loads across articular tissues
Maintenance of stability during use.
Extremities do NOT have to be symptomatic
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 3
P.A.R.T.S.
Pain and Tenderness: evaluated by
Quality
Location
Intensity
Asymmetry: identified through
Posture
Gait analysis
Static palpation
X-ray
ROM: evaluated through
ROM testing
Kinetic palpation
Stress radiography
Tone, Texture, Temperature: through
Observation
Palpation
Functional assessments
Instrumentation
Special test:
Specific x-rays: MRI,CAT etc.
First Things First
History: localize, characterize, what, when, where, how, why, ADL.
Bare the Area: Skin on Skin
Bilateral observation: deformities, swelling, side to side comparison
Bilateral palpation: side to side comparison
Active ROM: have patient move extremities, do good then bad
Passive ROM: Dr. moves the extremities, do good side then bad
Orthopedics/neurological exams:
X-Rays: 2 views usually AP and Lateral and maybe a comparison
view
Focused Examination of Involved Joints
Inspection: gross swelling, redness, malalignment (fracture ?)
Palpation: warmth, crepitus, tenderness (not pain)
Motion: active, passive, and resisted
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 4
“Cardinal Signs of Inflammation”
S - welling
H - eat
A - ltered Biomechanics
R - edness
P - ain
C-ompress
A Tip on Tape:
Please be sure you know taping techniques
Perform a tape test for allergic reactions
Use appropriate tape for the area, ie. correct tape width, no non-stretch
tape around muscles
Be smooth and overlap by half
Avoid gaps and wrinkles, may cause blisters
Do not wrap too tight or with too many layers, may impair circulation
and neural transmission
After taping Always check for sensation and pulse distal to the taping,
eg. capillary refill.
Don’t leave on too long, may cause skin to breakdown
Remove slowly and carefully
Do not Tape:
As first aid without assessment
If joint is swollen and painful
If skin sensation is abnormal
Where injury is acute, joint is unstable and/or bleeding is present
If not familiar with taping technique
A bad tape job is Worse than no tape
“When in doubt, Don’t”
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 5
Regarding differential diagnosis:
1) Biomechanical
Rest relieves pain
Activity increases or produces pain
Unilateral and has specific location
Character of pain is sharp or stabbing
History of trauma
2) Organic
Rest stiffens or increases pain
Bilateral, diffuse and broad in location
Character may be deep, dull ache
May not have obvious trauma, but trauma may be reason for
visit
Healing Response:
Inadequate functional recovery of tissue following injury is most
frequently a result of our inability to recognize that the body has its
own, inherent healing mechanisms. The fundamental principles of
healing should be directed at understanding the process of injury and
nature’s healing response to injury. It’s only then we can assist the
remarkable human body with its ability to recover normal function.
Evidence may show a possible protocol, but clinical experience is the
decision maker.
Proprioceptors:
Sensory receptors that respond to joint movement (kinesthesia) and
joint position (joint position sense), but do not typically contribute to
conscious sensation. .
Joint Proprioceptors:
Generally are “non-adapting” resulting in constant firing with
abnormal ligament stress.
Clinically, can get ongoing symptoms due to abnormal joint posture.
Wyke BD, Polack P: Articular Neurology.
JBJS1975;57B:401.
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 6
Improved proprioception with exercise makes physiological sense
Lephart et al, 1996
Nociceptors:
“a continuous tridimensional plexus of unmyelinated nerve fibers that
weaves
(like chicken-wire) in all directions throughout the tissue.”
Wyke B.Neurological Aspects of Pain Therapy. In: Swerdlow M,
Editor. The Therapy of Pain. Philadelphia: JB Lippencott: 1980
Nociceptor activity reflexively activates the sympathetic nervous
system…
Kabell J. Sympathetically maintained pain.In: Willis W.ed.
Hyperalgesia and Allodynia. Raven Press. NY: 1992
Nociceptors:
Fire with harmful or potentially harmful stimuli.
Thermo, mechano, and chemo, sensitive.
Estimated that half of all dorsal afferents are nociceptors.
Facilitation:
Repeated impulses enhance neural activity and reinforce response.
Hypo-mobile joints:
“Restricted joint motion causes an increase in nociceptive axons (A-
delta and C fibers) and a decrease firing of large diameter
mechanoreceptor axons (A-beta fibers).”Hooshmand H. Chronic pain:
reflex sympathetic dystrophy, prevention and management. Boca Raton, FL
CRS Press:1993.
“…..nociceptive input from dysfunctioning joints can cause symptoms
such as sweating, palor, nausea, vomitting, abdominal pain, sinus
congestions, dyspnea, cardiac palpitations, and chest pain that mimics
heart disease.”Nansel D. Szlazak M. Somatic dysfunction and the phenonema
of visceral disease simulation: A probable explanation for the apparent
effectiveness of somatic therapy in patients presumes to be suffering from
visceral disease. J. Manipulative Physiol Ther 1995:118:379-97.
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 7
Increase of nociceptor firing, decreases mechanorecptor firing.
Increase mechanorecptor input, decrease nociceptor at the level of the
spinal cord.
Altered Proprioception of nociceptor firing mechanoreceptor firing.
Adjusting mechanoreceptor input nociceptor firing at the level of
the spinal cord.
What can a Chiropractor do?
Adjust
“Adjustments to decrease nociceptor input to the spinal cord seem to
be an effective way to decrease the hyperexcitable central
state.”Patterson M. The spinal cord: participant in disorder.
J Spinal Manip: 1993:9(3)2-11
Posture affects every part of the musculoskeltal system of the body and
thus merits our consideration. Caillet R.,Soft tissue pain and disability.
Normal Joint Function:
Painless movement of appendages through a complete range of
motion.
Proper distribution of loads across articular tissues.
Maintenance of stability during use.
Documenting
Documenting
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 8
Bone Response to Stress
Wolff's law (1892)
tissue adapts to level of imposed stress
increased stress
hypertrophy (increase strength)
decreased stress
atrophy (decrease strength)
SHAPE REFLECTS FUNCTION
Genetics, Body weight, physical activity, diet, lifestyle
Generic
Stress-Strain Relationship
Bone
Stress-Strain Relationship
Overuse/Repetitive Injury:
Happens when the forces are below the maximal failure load but
applied enough times to result in an accumulation of microtrauma.
Tissue fatigue limits are exceeded and the damage occurs faster than
the body can repair it.
Common in athletes and repetitive work tasks.
Pain, onset and loss of function is gradual and over a period of time.
Loss of function, swelling and pain are not immediately disabling but
may increase to a point of severe loss of function.
The extremities are especially vulnerable to long term micro trauma.
The shoulder, elbow, wrist, knee and ankle are at particular risk.
The Mechanism/Bio-mechanics of
the Injury
“ The weakest and oldest among us can become some kind of athlete, but
only the strongest can survive as spectators. Only the hardiest can
survive the perils of inertia, inactivity, and immobility.”
Bland and Cooper, 1985 Sem Arthritis Rheum
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 9
Grading Sprain/Strains:
Grade I: stretching or separation of a few ligamentous fibers; exhibits
mild inflammation, edema, tenderness, no function loss.
Grade II: a more significant degree of separation or tearing of
ligamentous fibers; characterized by pain, edema, inflammation,
partial loss of function; possible permanent instability due to scar
tissue formation
Grade III: complete ligamentous tear or disruption; characterized by
edema, inflammation, hemorrhage, complete loss of function; usually
requires surgical intervention
Muscle Grading Chart
Using Modalities
Ice
Laser
Heat
Ultrasound – pulsed/continuous
Electro-Muscle Stim
TENS
Massage
Other
Deconditioning Syndrome
Decreased strength
Decreased endurance
Decreased flexibility
Decreased cardiovascular fitness
Decreased awareness of position sense and kinesthesia
Dr. Malik Slosberg, Validating Chiropractic
Protracted bed rest leads to a catabolic state with general malaise.
There is demineralization of the bone and a 3% loss of muscle strength
per day. Rest, particularly prolonged bed rest may be the most
harmful Tx ever devised and a potent cause of iatrogenic disability.
Waddell, MD.,Spine 1987;12(7):632-644.
1. Muscle atrophy: 1.0 to 1.5% of muscle mass lost per day,
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 10
2. Cardiopulomonary deconditioning (15% loss of aerobic capacity in 10
days)
3. Bone mineral loss with hypercalcemia & hypercalcuria;
4. Risk of thromboembolism,
5. Social side effects such as perception of severe illness,
6. Economic loss due to increased time lost from work.
Bigos, MD., Acute Low Back Problems in Adults. Clinical Practice
Guidelines. December 1994. Potential Harms & Side Effects of Bed
Rest. (p.53)
Fear Avoidance Behavior
Leads to inactivity, immobilization and disuse
May result in tissue impairment, reduced strength and ROM, stiffness
and weakness.
This will result in reduced motor skills, proprioception, balance,
stability and increased risk of more injury resulting in more fear
avoidance.
Dr. Malik Slosberg, Validating Chiropractic
Active Rehabilitation
There is clear evidence that, despite general belief, activity is not
harmful, and active rehabilitation not only restores function, but
also reduces pain. Wadell G:Spine, Vol.12, no. 7 ,1987
Restoring tissue function progressively
PRICE
Modification of activities and education
Modalities: heat, electrical stimulation, ultrasound, etc.
Range of motion exercises
Strength, power, endurance, and specific agility exercises
Functional Disability
Scar tissue formation
Restricted joint motion
Muscular contracture
Fascial shortening
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 11
If a segment is:
Hypo-mobile - Mobilize
Hyper-mobile - Stabilize
Normal/Optimal - Leave alone
Life to a Joint is MOTION Get it moving
Focused Examination of Involved Joints
Inspection: gross swelling, redness, malalignment
Palpation: warmth, crepitus, tenderness (not pain)
Motion: active, passive, and resisted
“Cardinal Signs of Inflammation”
S - welling
H - eat
A - ltered Biomechanics
R - edness
P - ain
This Marvelous Knee
Basic Anatomy & Kinesiology
Femur
Tibia
Patella
First Things First
History: localize, characterize, what, when, where, how, why, ADL.
Bare the Area
Bilateral observation
Bilateral palpation
Active ROM
Passive ROM
Orthopedics/neurological exams
X-Rays: 2 views usually AP and Lateral and maybe a comparison
view
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 12
Focused Examination of Involved Joints
Inspection: gross swelling, redness, malalignment (fracture ?)
Palpation: warmth, crepitus, tenderness (not pain)
Motion: active, passive, and resisted
Ligaments of the Knee
The Knee is considered to be a Two joint structure
1. Patellofemoral 2. Tibiofemoral
modified hinge joint with flexion and extension as the primary motion
with “some” rotation when the knee is flexed
Runners Knee
What is Runner's Knee (Patellofemoral Pain Syndrome)?
The patella does not track vertically in the Trochelar groove, but is
pulled sideways.
This causes the cartilage on the undersurface of the patella, and the
cartilage in the Trochlear Groove to rub abnormally against each other,
producing pain.
If left untreated, the cartilage that is subjected to this excessive rubbing
will become permanently damaged, and begin to deteriorate and break
down.
This condition is known as chondromalacia and can become
permanent, since damaged cartilage cannot usually repair itself.
Runners Knee Presentation
Pain near the knee cap (patella), and below it. The pain is located on
the anterior surface (front) of the knee, not deep within the knee
joint.
You may feel and hear a "grinding" when the knee is flexed and
extended.
Pain after sitting with the knees bent for a time, and then standing
up and walking.
Walking or running downhill, or walking down stairs may produce
knee pain.
Direct pressure on the knee cap may produce pain.
The area around the patella may swell when pain is present.
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 13
Orthopedics:
Patella Grinding – Chondromalacia patella
Apley’s compression – Meniscus
Apley’s distraction – Ligament integrity
McMurray’s – Meniscal tears
Varus and Valgus stress test – Collateral ligaments
Anterior drawers – Anterior cruciate
Posterior drawers – Posterior cruciate
Some Differential Dx’s
Chronic pain – usually due to intra-articular pathology
Meniscal pain – localized at joint space,worse with activity, pain is
most common symptom of tear (49%)
Patellofemoral pain – anterior knee not deep, pain increases walking
down steps etc.
DJD – related to activity and weather
Inflammatory disorders – generally worse in the mornings
Tibiofemoral
There is a gliding type of motion found throughout the range of
motion.
Tibial plateaus are the main load bearing structures. Bone, cartilage
and ligaments share load bearing.
The menisci help in distributing the stresses imposed on the tibial
plateaus.
Menisci
Menisci
The menisci (semilunar cartilages) attach to the tibial plateau via
coronary ligaments.
They provide deeper articular depressions than are supplied by the
tibial surface alone.
They are responsible for load transmission and shock absorption.
Anterior Cruciate Ligament
Primary role: restraint to Anterior tibial displacement
Accepts 75% of the Anterior force at full extension and ~85% at 30
degrees flexion.
Secondary role: is to resist tibial Rotation, especially toward full
extension, and it functions more as a restraint to Internal Rotation.
Also helps to restrain Valgus opening in full extension.
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 14
Mechanism of ACL injury
Most commonly this injury occurs during rapid cutting maneuvers in
sports such as basketball, soccer, football and rugby.
Participation in these sports predisposes the knee to a collision from
the lateral aspect, as occurs in tackling.
Posterior Cruciate Ligament
Primary role: restraint to Posterior translation, especially at 30 and 90
degrees of flexion, sustaining 95% of the restraining force.
Secondary role: to help restrain valgus opening in full extension
Mechanism of PCL injury
PCL injury can have the same positional mechanism of action as ACL
injury, due to the complexity of knee mechanics and muscular and or
lower leg variables (i.e. foot fixed in ski boot, contractile force of
popliteus, hamstrings or other muscles crossing the knee joint at time
of injury).
Collateral ligament injury
Medial collateral ligament is the primary valgus restraint. Injury is
caused by valgus stress to the knee.
In view of its attachment to the medial meniscus, MCL injury is
commonly associated with medial meniscus and ACL injury (unhappy
triad).
The iliotibial band inserts at the superior aspect of the lateral tibia.
It functions to stabilize the pelvis when the knee is in flexion during
weight bearing.
Friction can be produced at the lateral femoral condyle if the knee does
not flex and extend properly.
Most commonly seen in runners
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 15
Iliotibial band
Friction is usually produced at the time of foot strike and produces
local inflammation of he knee joint with mild-severe lateral knee pain.
Usually caused by poor mechanics.
Overuse is commonly a factor, which is why it is seen most frequently
in runners.
Iliotibial band cont.
Pronation of the foot: is the number one abnormality linked to I.T.B.
Syndrome. Pronation causes the tibia to rotate internally and tightens
the I.T.B., causing it to rub with more force against the edge of the
femur.
High or low arches: prevent the arches in the feet from acting as the
natural "shock absorbers" they were designed to be. Thus, the force of
each foot strike (up to 3 times the body's weight) is passed on to the
knee area.
Bow-legs: cause tightening of the soft tissues on the outer aspect of
the leg and knee, forcing the I.T.B. to rub with greater force against the
edge of the femur.
Iliotibial band cont.
Pain occurs on the outside of the knee
Pain is worse on slow straight line running and actually better on fast,
change of direction movements (the opposite to most knee injuries)
Pain gets worse the longer that running goes for
Pain is worse running downhill than uphill or on level ground
Pain can be severe once the band starts rubbing on bare bone. In this
case it is relieved fully by walking with the leg totally straight.
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 16
Ankle and Foot
Basic Anatomy:
26 – 28 Bones and 33 joints
3 cuneiforms (wedge shaped)
the navicular (boat shape)
the cuboid (cube shape)
the talus (ankle bone)
the calcaneus (heel bone)
five metatarsals
two sesmoid?
14 phalanges
Focused Examination of Involved Joints
Inspection: gross swelling, redness, malalignment (fracture ?)
Palpation: warmth, crepitus, tenderness
(not pain)
Motion: active, passive, and resisted
The Arches
Optimal Arch Angle
Indicators for Excessive Pronation
Foot Flare / Toe Out
Posterior/Lateral Heel Wear
Patellar Approximation
Achilles Tendon Bowing
Navicular / Flat Arch
Callouses on 2-3-4 Metatarsal Heads
Positive Navicular Drop Test (PSI)
Grade 4 Psoas, Gluteus Medius, Quadriceps
Foot Type and Lower Extremity Injury
“ Athletes with pronated and supinated feet had significantly more
knee pain than the normal group.”Dahle LK,et al.J Ortho Sports Phys
Ther 1991;14(2):70-4
Muscles in the Foot
“The first line of defense of the arches is ligamentous. The muscles did
not come into play until a force greater than 400 pounds was exerted
and even then many remained inactive.”Basmajian JV et al.The Role
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 17
of Muscles in Arch Support of the Foot: An Electromyographic Study. J
of Bone and Joint Surgery, Vol 45, No 6 September 1963.
4 Facts About the Feet
The most common subluxation pattern of the foot is
1. EXCESSIVE PRONATION.
2. Nearly all excessive pronation is BILATERAL but
ASYMMETRICAL.
3. Whatever one arch in the foot does….so do the other two.
4. Most foot subluxations do not create foot
SYMPTOMATOLOGY.
Arch Stability
The highest relative contribution to arch stability was provided by the
plantar fascia, followed by the plantar ligaments and spring ligament.
Plantar fascia was a major factor in maintenance of the medial
longitudinal arch.Huang et al: Biomechanical Evaluation of
Longitudinal Arch Stabilty. Foot & Ankle, Vol. 14, No. 6, July/August
1993
Simple Relationship of Arches-Bones-Muscles
Chronic Foot Strain
Cause - Repeated excessive stress
What Happens?
1. Ligaments exposed to strain elongate and undergo
inflammatory changes
2. If it persists….
ligament degenerates
loses supporting function
DJD develops in joint
Plantar Fascitis
Pain in arch of foot
Continual stress may cause a calcaneal spur
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 18
Fallen arches
Elastic vs. Plastic deformation
Elastic vs. Plastic deformation
Elasticity - property of a material that allows the material to return to
its original shape and size after the removal of the deforming load.
Plasticity – the property of a material to permanently deform when it is
loaded beyond its elastic range.
Plantar Fascitis
Rx: Plantar Fascitis
Adjust
Exercise – marble pick up,
Roll a tennis ball, with slight weight bearing the length of the foot
Orthotics – to support arches, also with a depression in heel
Ultra-sound
Surgery ????
Metatarsalgia
“pain in the forefoot represents the most frequent cause of pain in the
human foot. The most common origin of the disturbance is an
alteration of the fine biomechanics of the forefoot.”Viladot A:
Metatarsalgia Due to Biomechanical Alterations of the Forefoot.
Orthopedic Clincs of No Ameriaca, Vol 4, No 1, Jan 1973.
Metatarsalgia
Usually middle 3 metatarsal heads due to depression of metatarsal
arch caused by strain
Callous formation indicates excessive weight bearing on metatarsal
heads
Pain greatest on weight bearing, feels like “a pebble in shoe”
Pain is constant
Rx: Metatarsalgia
Elevate Mid-metarsal Arch to assist in restoration of normal weight
bearing
Adjust metarsal heads
Use foot orthotics to help restore archs
Use support under the shafts and not under the heads of the
metatarsals
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 19
Morton’s Neuroma
Fibrous swelling of the 4th digital nerve
Usually caused by irritation due to rubbing between the metatarsal
bones ie. Shoes that are too tight and narrow
Patient usually pain free when not wearing shoes (differentiate from
metatarsalgia)
Pain is sharp, severe, stabbing
Rx: Morton’s Neuroma
Adjust metatarsal heads
Eliminate the cause of the stress, properly fitted shoes
If severe surgical intervention may be necessary
A General Review of Lower Extremity Patient Presentation - J. Alan Lovejoy 20
You might also like
- Examining Joints: How To Succeed in Clinical ExaminationsDocument12 pagesExamining Joints: How To Succeed in Clinical ExaminationsimperiallightNo ratings yet
- Neurological ExaminationDocument23 pagesNeurological ExaminationMuhammad Fahmy100% (1)
- MUSCULOSKELETAL PAINDocument20 pagesMUSCULOSKELETAL PAINFatima JamalNo ratings yet
- HEINKING CounterstrainInAcuteInjuries ACOFPDocument60 pagesHEINKING CounterstrainInAcuteInjuries ACOFPRukaphuongNo ratings yet
- Orthopedic: OrthopaedicsDocument11 pagesOrthopedic: OrthopaedicsDrAyyoub AbboodNo ratings yet
- Lower Back Pain - MontaltoDocument5 pagesLower Back Pain - MontaltoElizabeth OxfordNo ratings yet
- Low Back PainDocument100 pagesLow Back Painchandrusai100% (1)
- Low BackDocument7 pagesLow BackMuhammad FahmyNo ratings yet
- ChapmanDocument7 pagesChapmanEdgardo BivimasNo ratings yet
- KneeDocument24 pagesKneeMuhammad Fahmy100% (1)
- 10 Lumbosacral SpineDocument10 pages10 Lumbosacral Spine楊畯凱No ratings yet
- Conservative Management of Costovertebral SubluxationDocument4 pagesConservative Management of Costovertebral SubluxationDr Franklin Shoenholtz100% (3)
- David Butler Neural Tissue Mobilisation-1Document11 pagesDavid Butler Neural Tissue Mobilisation-1Himani BhondgeNo ratings yet
- Neurological History and ExaminationDocument30 pagesNeurological History and ExaminationMaria Agatha100% (1)
- Weebly Questions Week TwoDocument3 pagesWeebly Questions Week Twoapi-459697337No ratings yet
- Posture Dr. Dr. MY, SP KFR-KDocument67 pagesPosture Dr. Dr. MY, SP KFR-KCikupaNo ratings yet
- Brunnstrom ApproachDocument9 pagesBrunnstrom ApproachavtordajNo ratings yet
- Shoulder Pain-Pemalang 18 Des 22Document65 pagesShoulder Pain-Pemalang 18 Des 22yaang yuliana ciptaNo ratings yet
- Trigger Point Homp. TehranDocument46 pagesTrigger Point Homp. TehranKasra Chehrazy100% (1)
- Danto AAO Convocation2012LectureDocument48 pagesDanto AAO Convocation2012Lecturercastello20No ratings yet
- Spondylosis 32Document3 pagesSpondylosis 32anaab atif ahmedNo ratings yet
- Lab Report Group 6 Nerves and ReflexesDocument5 pagesLab Report Group 6 Nerves and ReflexesKristina Esta50% (2)
- Lecture 1: Lumbar: Indirect ObjectivesDocument11 pagesLecture 1: Lumbar: Indirect ObjectiveseugeniaNo ratings yet
- Classical Disc Herniation by DR Anupreet BassiDocument17 pagesClassical Disc Herniation by DR Anupreet Bassidr_bassiNo ratings yet
- Acute Low Back PainDocument39 pagesAcute Low Back PainSathish KumarNo ratings yet
- ICD-9-CM Code: 724.3 ICF CodesDocument8 pagesICD-9-CM Code: 724.3 ICF CodesGeorgiana MilcoveanuNo ratings yet
- 1 Peripheral Manipulation Lecture OneDocument13 pages1 Peripheral Manipulation Lecture Onebuhlembatha304No ratings yet
- The Musculoskeletal Examination: Colon H - WilsonDocument5 pagesThe Musculoskeletal Examination: Colon H - WilsonAbdullah Bin SaeedNo ratings yet
- Cervico Thoracic Rehab ProgramDocument20 pagesCervico Thoracic Rehab ProgramulaNo ratings yet
- Assessment: The Neurologic Exam: InterviewDocument10 pagesAssessment: The Neurologic Exam: InterviewJun ManNo ratings yet
- Case Presentaion: Souvik Paul BPT 3 Year Nopany Institute of Healthcare StudiesDocument30 pagesCase Presentaion: Souvik Paul BPT 3 Year Nopany Institute of Healthcare StudiesSouvik PaulNo ratings yet
- Physical Examination: Orthopedics: Clinical Case Story 1 (Extremities)Document0 pagesPhysical Examination: Orthopedics: Clinical Case Story 1 (Extremities)Shamini ShanmugalingamNo ratings yet
- Critical Thinking Questions in Anatomy Chapter 1Document2 pagesCritical Thinking Questions in Anatomy Chapter 1NathaliaNo ratings yet
- Biofeedback Psychophysiological Training: What Is PsychophysiologyDocument16 pagesBiofeedback Psychophysiological Training: What Is PsychophysiologyNatasha PereiraNo ratings yet
- Neuro PEDocument36 pagesNeuro PEkhaderbasha2020No ratings yet
- Turocy Strain Counterstrain PATS06Document46 pagesTurocy Strain Counterstrain PATS06Yap Grace K Xiulin100% (2)
- Health Assessment SAS Session 20Document6 pagesHealth Assessment SAS Session 20Maria Jub MangrubanNo ratings yet
- Physical Exam Lecture 2018Document52 pagesPhysical Exam Lecture 2018mazinNo ratings yet
- Sebastian2014 PDFDocument8 pagesSebastian2014 PDFArchita AgarwalNo ratings yet
- AP41 MDocument3 pagesAP41 Monix2000No ratings yet
- Varieties of Spondylolisthesis: (A) Normal, (B) Congenital, (C) Isthmic, (D) Traumatic, (E) Degenerative, and (F) PathologicalDocument5 pagesVarieties of Spondylolisthesis: (A) Normal, (B) Congenital, (C) Isthmic, (D) Traumatic, (E) Degenerative, and (F) PathologicalYashaswi ANo ratings yet
- Neurological exam guide for medical studentsDocument13 pagesNeurological exam guide for medical studentslailatul husna100% (1)
- 6 Browse PNEDocument4 pages6 Browse PNElama4thyearNo ratings yet
- Introduction To Physical Examination AssesmentDocument38 pagesIntroduction To Physical Examination AssesmentnabillaNo ratings yet
- Introductory Lecture, Neurological Examination: General OverviewDocument8 pagesIntroductory Lecture, Neurological Examination: General OverviewmustafaNo ratings yet
- Tandem Spinal StenosisDocument4 pagesTandem Spinal StenosisikhwanNo ratings yet
- Boehnke - Dorsal Scapular Nerve SyndromeDocument7 pagesBoehnke - Dorsal Scapular Nerve Syndromekeeley_holderNo ratings yet
- Ortho AssessmentDocument91 pagesOrtho AssessmentMfxMazprofxNo ratings yet
- Supervised Clinical Practice-III: AssignmentDocument12 pagesSupervised Clinical Practice-III: Assignmentzainab siddiqueNo ratings yet
- Review of Literature: Presenting By: Monika S. Kulkarni 1 Year MPT Department of Orthopaedic Manual TherapyDocument44 pagesReview of Literature: Presenting By: Monika S. Kulkarni 1 Year MPT Department of Orthopaedic Manual TherapyANKITA SHETTYNo ratings yet
- Ak History - 4 PageDocument4 pagesAk History - 4 Pagejuliano.clj7836No ratings yet
- Clinical Decision Making in Evaluation of Shoulder DysfunctionDocument27 pagesClinical Decision Making in Evaluation of Shoulder DysfunctionSanjanaa ZadNo ratings yet
- Ot StrokeDocument44 pagesOt StrokeDebora Astried F SipayungNo ratings yet
- Clinical Examination of The Wrist PDFDocument11 pagesClinical Examination of The Wrist PDFAdosotoNo ratings yet
- Appendix: Field Neurological AssessmentDocument10 pagesAppendix: Field Neurological AssessmentLeon LellaNo ratings yet
- Paces 6 - Cns - Lower LimbDocument18 pagesPaces 6 - Cns - Lower LimbDrShamshad Khan100% (1)
- The Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaFrom EverandThe Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaNo ratings yet
- Total Reflexology: The Reflex Points for Physical, Emotional, and Psychological HealingFrom EverandTotal Reflexology: The Reflex Points for Physical, Emotional, and Psychological HealingRating: 2.5 out of 5 stars2.5/5 (2)
- The Basics: A Comprehensive Outline of Nursing School ContentFrom EverandThe Basics: A Comprehensive Outline of Nursing School ContentRating: 5 out of 5 stars5/5 (3)
- Core Fluency Thesaurus by Kev Nair, 2nd Edition - 203pDocument203 pagesCore Fluency Thesaurus by Kev Nair, 2nd Edition - 203pLeo King90% (10)
- Kev Nair-The Complete Fluency WordsDocument65 pagesKev Nair-The Complete Fluency Wordsmyokamalta89% (9)
- TautDocument22 pagesTautmyokamaltaNo ratings yet
- SDSG Radiographic Measuremnt ManualDocument120 pagesSDSG Radiographic Measuremnt ManualYuliana Wiralestari100% (2)
- Principles of Functional ExerciseDocument290 pagesPrinciples of Functional ExercisePedro ManéNo ratings yet
- Causes and Tests of Upper Cervical Spine PainDocument22 pagesCauses and Tests of Upper Cervical Spine PainiikemNo ratings yet
- Cox Technique Herniated Disc TreatmentDocument9 pagesCox Technique Herniated Disc TreatmentmyokamaltaNo ratings yet
- DisplacementDocument10 pagesDisplacementmyokamaltaNo ratings yet
- WelnessDocument153 pagesWelnessmyokamaltaNo ratings yet
- Anterior Subluxation of The Cervical Spine:: Hyperflexion SprainDocument8 pagesAnterior Subluxation of The Cervical Spine:: Hyperflexion SprainmyokamaltaNo ratings yet
- Radiology of Lumbar Spine by Jeff Berger DODocument180 pagesRadiology of Lumbar Spine by Jeff Berger DOmyokamalta100% (1)
- Radiology Reference Guide PDFDocument24 pagesRadiology Reference Guide PDFmyokamaltaNo ratings yet
- Deadly Secrets of Dim MakDocument16 pagesDeadly Secrets of Dim MakDeclan Max Brohan92% (49)
- Hypnotic Seduction Techniques: WorkbookDocument18 pagesHypnotic Seduction Techniques: WorkbookmdmoloyNo ratings yet
- Learn How To MassageDocument21 pagesLearn How To MassageEskay100% (29)
- Martial Arts - Pressure Points - Military Hand To Hand Combat GuideDocument27 pagesMartial Arts - Pressure Points - Military Hand To Hand Combat GuidemyokamaltaNo ratings yet
- Wing Chung - History, Philosophy, Dim Mak, Proper Breathing, and Dummy TechniquesDocument151 pagesWing Chung - History, Philosophy, Dim Mak, Proper Breathing, and Dummy Techniquesanon-2674100% (33)
- What Is Lateral Collateral Ligament Sprain?Document9 pagesWhat Is Lateral Collateral Ligament Sprain?mochamad ilham kurniaNo ratings yet
- Parotid Gland: LocationDocument111 pagesParotid Gland: LocationFarah FarahNo ratings yet
- USM Student Research on Conservative Meniscus RehabilitationDocument2 pagesUSM Student Research on Conservative Meniscus RehabilitationShahroz Khan100% (1)
- Things To Read: A. Trauma: Fractures and DislocationsDocument4 pagesThings To Read: A. Trauma: Fractures and DislocationsHanien YeeNo ratings yet
- 18 MSK Arm and HandDocument27 pages18 MSK Arm and HandNTRisforthinkersNo ratings yet
- Workout Program: Shortcut To SizeDocument11 pagesWorkout Program: Shortcut To SizeAhmed Hamza100% (1)
- The Complete Guide To Fixing Your Caveman Posture! The Postural Analysis: Side PostureDocument6 pagesThe Complete Guide To Fixing Your Caveman Posture! The Postural Analysis: Side PostureYouRuggedManlyTypeNo ratings yet
- Bursitis-Tendonitis-Dr - Amit PatelDocument52 pagesBursitis-Tendonitis-Dr - Amit PatelAmitNo ratings yet
- Rafii Khairuddin Mahfuzh-1810301069-Pr Manipulasi Upper-DikonversiDocument5 pagesRafii Khairuddin Mahfuzh-1810301069-Pr Manipulasi Upper-Dikonversiraden ayu putri suryaniNo ratings yet
- Joint Structure and Function A Comprehensive Analysis Fifth Edition PDFDocument41 pagesJoint Structure and Function A Comprehensive Analysis Fifth Edition PDFrandy.beard30194% (33)
- Muscles of Upper LimbDocument21 pagesMuscles of Upper Limbمحمد علىNo ratings yet
- Dermatome Map OverviewDocument1 pageDermatome Map Overviewngwinda90100% (1)
- Emilio Aguinaldo College: Assessing ReflexesDocument3 pagesEmilio Aguinaldo College: Assessing ReflexesMarijo DolojolNo ratings yet
- A Person Is Performing Slow Arm Curls With A 10-Kg Weight As - QuizletDocument5 pagesA Person Is Performing Slow Arm Curls With A 10-Kg Weight As - Quizlet刘洋No ratings yet
- TACFIT26 Exercise ManualDocument90 pagesTACFIT26 Exercise ManualEndika Sa Go94% (17)
- Ankle Fractures in Adults - UpToDateDocument50 pagesAnkle Fractures in Adults - UpToDateJose LuceroNo ratings yet
- Maitland ShoulderDocument91 pagesMaitland ShoulderAyesha Sameen100% (1)
- Ue RomDocument5 pagesUe Romnacole78No ratings yet
- BIO34A Exercise 9Document3 pagesBIO34A Exercise 9Patrick IntongNo ratings yet
- TC3HP - Técnica QuirúrgicaDocument84 pagesTC3HP - Técnica QuirúrgicaRafael RecioNo ratings yet
- Biomecanica Rodilla en ArtroplastiasDocument7 pagesBiomecanica Rodilla en ArtroplastiasManuel Azael Rodríguez CigalaNo ratings yet
- Etacarpals: Modifiers For MetacarpalsDocument4 pagesEtacarpals: Modifiers For MetacarpalsGabriela Ballestero ContrerasNo ratings yet
- Variasi Tendon Otot Palmaris Longus: Artikel PenelitianDocument4 pagesVariasi Tendon Otot Palmaris Longus: Artikel PenelitianHesti RiniNo ratings yet
- PT Lab 2/7 Head and Neck FocusDocument2 pagesPT Lab 2/7 Head and Neck FocusNeo Derrick Adrian MartinezNo ratings yet
- Shoulder Dystocia - StatPearls - NCBI BookshelfDocument7 pagesShoulder Dystocia - StatPearls - NCBI Bookshelfjennie JeanNo ratings yet
- Knee Anatomy and InjuriesDocument120 pagesKnee Anatomy and Injurieserfan mohammadi100% (2)
- Dry Needling - From Award Winnin - Harbir Singh M.Ost MedDocument141 pagesDry Needling - From Award Winnin - Harbir Singh M.Ost MedMarcos Tadeu Ferreira100% (1)
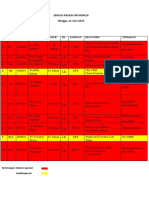
- Sensus Pasien Orthopedi Minggu, 21 JULI 2019: No Bed No - RM Nama Umur JK Jaminan Diagnosis TindakanDocument3 pagesSensus Pasien Orthopedi Minggu, 21 JULI 2019: No Bed No - RM Nama Umur JK Jaminan Diagnosis TindakanWa JulianiNo ratings yet
- Physiotherapist's Pocketbook Essential Facts at Your Fingertips THIRD EDITION. THIRDDocument434 pagesPhysiotherapist's Pocketbook Essential Facts at Your Fingertips THIRD EDITION. THIRDAyesha Abbasi100% (3)
- Bickerstaff Neurological ExaminationDocument73 pagesBickerstaff Neurological ExaminationHisham Elkilaney67% (6)